Author of the article
Anatoly Shishigin
Reading time: 4 minutes
AA
The drug Euphyllin refers to drugs that normalize heart rate and respiratory function. Often doctors prescribe it as a diuretic, which is determined in each case by a specialist based on medical history and the severity of the disease. Doctors strongly do not recommend using medications on your own, so as not to complicate the disease.
Action and composition of the drug
Eufillin is a popular drug whose pharmacological action is based on the work of aminophylline, the active component of the drug. This substance, in turn, is a mixture consisting of four parts theophylline and one part ethylenediamine.
Theophylline translated from Greek and Latin means tea leaf.
Eufillin is a popular bronchodilator
Theophylline is a natural alkaloid found in tea tree, Paraguayan holly, and cocoa fruit . When this substance enters the female body:
- relaxes bronchial muscles;
- improves lung ventilation through stimulation of diaphragm contractions, which ultimately leads to blood saturation with oxygen;
- reduces the tone of blood vessels, increasing their lumen, resulting in: improved blood circulation in the myocardium;
- cardiac activity is stimulated;
- blood pressure decreases;
The second component of aminophylline, ethylenediamine, promotes the rapid dissolution and absorption of theophylline, and also enhances the relaxation of smooth muscles.
Thus, Eufillin has a complex effect on the body of a pregnant woman, not only relieving edema, but also reducing high blood pressure, as well as improving heart function.
Direct assignments
It is recommended to use "Eufillin" for the following pathological conditions:
The drug is prescribed to relieve bronchospasm.
- chronic inflammatory disease of the respiratory tract;
- bronchospasm;
- cerebrovascular accidents;
- cardiovascular pathologies characterized by circulatory insufficiency and congestion;
- cerebral ischemia;
- hypertonic disease;
- pulmonary edema;
- initial stage of stroke;
- as a diuretic for arterial hypertension.
Eufillin is often prescribed to pregnant women to relieve swelling of the extremities caused by sodium salts.
Is it possible for expectant mothers to take Eufillin?
Manufacturers in the annotation for the drug warn that the active substance can penetrate the placental barrier and accumulate in the child’s plasma. In addition, the use of aminophylline in late gestation often results in potentially harmful concentrations of theophylline in the blood of the newborn.
Reviews from doctors regarding the use of Eufillin during pregnancy are contradictory
Many doctors are against prescribing Eufillin to pregnant women, considering it an outdated and potentially harmful drug. As an argument, they cite the fact that the diuretic effect of the drug can disrupt the water-salt balance, and this is just as dangerous for the expectant mother’s body as edema.
However, doctors of the “old school” continue to recommend the medication, citing many years of experience in its use in obstetric and gynecological practice. Indeed, with severe gestosis, Eufillin is able to quickly help a woman, eliminating the dangerous condition.
Thus, before prescribing the drug, the doctor assesses all possible risks and threats, takes into account the severity of symptoms, the trimester of pregnancy (the first trimester is prescribed extremely rarely), as well as the health status of the expectant mother and child.
If Eufillin was nevertheless prescribed, certain rules must be followed:
- It is better to take medication treatment in a hospital, since it is necessary to regularly examine the woman and the fetus;
- the drug cannot be used for a long time (usually symptomatic therapy for swelling is indicated for expectant mothers);
- It is worth minimizing the dosage (as much as possible).
The American Food and Drug Administration has assigned aminophylline, the active substance of Euphyllin, category C. It follows that animal experiments have established a negative effect of the drug on the embryo. And yet, the likely benefits of using the medication for serious indications justify the numerous risks.
Mechanism of action of Eufillin
The product belongs to the group of xanthines (methylxanthine derivatives), soluble in water and has a positive effect on the cleansing function of the kidneys (glomerular filtration). By dilating the vessels of the glomeruli of the kidneys, the drug activates blood flow, which leads to an increase in the formation of the first urine.
At the same time, the rate of passage of urine through the renal tubules increases, which leads to a decrease in its reabsorption (reabsorption). Ultimately, urine production increases. Application options:
- oral (inside);
- parenteral;
- rectally in microenemas (for children).
Combined with release forms:
- tablets 0.15 g;
- injections into the muscle and into the vein, based on this 24% and 2.4% solutions.
Intravenous administration is practiced in severe cases. In less pointed ones - tablets or intramuscularly. Eufillin diuretic tablets are prescribed in a variety of dosages depending on the severity of the condition and the weight of the patient. It is recommended to take on a full stomach with plenty of water. Very often, Eufillin is prescribed during pregnancy to relieve swelling of the legs and arms caused by sodium salts. Very often when herbal remedies are ineffective.
Often this is a short-term course, extremely rarely – long-term, up to a month.
Side effects or who is at risk?
With rapid drip or intramuscular administration, the patient may experience complications. But pills can also make you feel worse. Side effects include:
Persons with heart rhythm disturbances (paroxysmal tachycardia, extrasystole), coronary insufficiency, epilepsy, or low blood pressure should not take the drug as a diuretic. Since Eufillin is a moderate diuretic, it is easy to replace.
The drug is not prescribed to children under 14 years of age.
In what cases is medication prescribed?
In the annotation for the drug you can find both standard indications that apply to all categories of patients, and those relating only to the gestation period. Thus, the use of the drug is permissible when:
- attacks of bronchial spasm;
- bronchial asthma;
- pulmonary emphysema (pathological expansion of bronchioles, which is accompanied by oxygen starvation of the lung tissue);
- pulmonary obstruction;
- increased blood pressure in the vessels of the pulmonary circulation;
- impaired cerebral circulation;
- gestosis (late toxicosis), accompanied by: severe edema;
- high blood pressure;
- high protein content in urine;
There is no need to consider Eufillin a universal “drug for edema.” In most cases, they do not pose a serious danger to a woman. The drug is usually prescribed for late toxicosis that develops in the second and third trimesters of pregnancy, when the upper half of the body swells, protein appears in the urine, and blood pressure rises.
Late toxicosis in expectant mothers - video
Hangover symptoms and complications
The consequences can be unpleasant and harmful to health:
- Pathological dysfunctions of internal organs.
- Fainting, possible seizures.
- Visual and auditory illusions - including the development of delirium tremens, when a person begins to experience hallucinations.
- Deterioration of orientation in space and time.
- Suicide attempts are possible.
- Young people experience a predominance of anxiety, while older people experience worsening mood and panic attacks.
- Exhaustion.
- Dehydration.
- Severe hyperthermia.
Contraindications and possible side effects
Eufillin is a serious medicine, which once again confirms the impressive list of restrictions and prohibitions. The medication has absolute and relative contraindications for use.
Absolute and relative contraindications to taking Eufillin - table
| Absolute contraindications | Relative contraindications |
|
|
Undesirable consequences from the use of tablets and solution
The list of undesirable consequences and their severity largely depend on what dosage form is prescribed to the expectant mother - tablets or liquid (solution for injection).
- When taking tablets, the following adverse reactions may occur:
- sleep problems;
- anxiety;
- increased heart rate;
- lowering blood sugar levels.
- The result of injection therapy can be:
- migraine;
- severe anxiety, irritation;
- insomnia;
- arrhythmia;
- disorders of the cardiovascular system (arrhythmia, heart pain, hypotension);
- dyspeptic disorders (vomiting, burning in the chest, epigastric pain, decreased appetite);
- low glucose levels in the body;
- skin rashes;
- increased urination.
When using Euphyllin in the third trimester, an increased heart rate in the fetus and a high concentration of theophylline in the blood plasma of a newborn baby are possible.
Drug interactions
It is extremely important to tell your doctor if you are taking other medications, since Eufillin tends to interact with medications.
- The simultaneous use of Eufillin with glucocorticosteroids increases the severity of undesirable consequences from the latter.
- Sorbents and antidiarrheals reduce the absorption of Eufillin.
- The effect of the drug is enhanced by the use of macrolide antibiotics, as well as medications containing human interferon.
- Eufillin affects the effectiveness of diuretics and beta-agonists (often prescribed for asthma).
In addition, the drug cannot be combined with glucose and ascorbic acid.
During therapy with Eufillin, you should refrain from consuming products that contain caffeine (coffee, chocolate, black or green tea).
Features of the use of the drug Eufillin
During treatment with Eufillin, drinking strong tea, alcohol and coffee is prohibited. There are also significant restrictions when interacting with other drugs. So, if the drug is safe to combine with vitamin complexes and dietary supplements, then combined use with other medications requires prior consultation with a specialist.
Use with glucocorticoid, mineralocorticoid drugs, as well as with medications that affect the central nervous system, entails increased side effects of the latter. A similar fate awaits lithium salts, since their effect in the body will also be weakened during treatment with Eufillin.
In addition, Eufillin is not used in conjunction with xanthine derivatives, and it enhances the activity of diuretics and sympathomimetics, but reduces the effect of α-adrenergic receptors. In the “duet” with phenobarbital, rifampicin, aminoglutethimide, phenytoin, isoniazid, sulfinpyrazone, carbamazepine and moracizine, the effectiveness of Eufillin decreases, requiring adjustment of its dose.
Complex treatment with antibiotics of the group lincomycin, cimetidine, macrolides, propranolol, isoprenaline, oral contraceptives, ethanol, disulfiram, allopurinol, enoxacin, recombinant interferon-α, fluoroquinolones, ticlopidine, methotrexate, propafenone, mexiletine, thiabendazole and verapamil, the intensity of action may rise that implies a reduction in the dose of Eufillin. Prescribe with caution with anticoagulants.
Instructions for use
Intravenous administration (drips)
Most often, during the period of bearing a child, Eufillin is prescribed in the form of intravenous injections (using a dropper), which are carried out in a hospital setting.
Before use, the drug is diluted with isotonic sodium solution. The drug is administered extremely slowly (the infusion rate usually does not exceed 30–50 drops per minute), while monitoring the blood pressure and heart rate of the woman and child.
Use of tablet form
Eufillin in tablet form is taken after meals to avoid stomach problems. Take the medicine with clean boiled water.
The medical manual for the drug does not indicate the specifics of using the drug during gestation, so the duration of therapy and dosage in each case are determined individually. The treatment regimen depends on the severity of symptoms and characteristics of the body.
Inhalation therapy
Inhalations with Eufillin are a controversial procedure
Inhalation with a solution of the drug is another example of the use of Eufillin for off-label purposes. Therefore, the attitude towards them on the part of medical workers is ambiguous:
- Some experts recommend breathing a diluted solution of the drug through a nebulizer during attacks of obstructive bronchitis. It is believed that such procedures expand and cleanse the bronchi and improve breathing.
- Others deny this method of therapy, since the therapeutic effect is detected only when the drug penetrates the systemic bloodstream. Contact of the active component with the bronchial mucosa does not have any significant effect.
In any case, taking Eufillin on your own is strictly prohibited.
Hangover symptoms and complications
Symptoms depend on the severity of alcohol dependence and are divided as follows.
First degree
It develops during the transformation of the first phase of alcohol dependence into the second, which is typical for short-term binge drinking:
- The predominance of asthenic symptoms (depression, depression, fear, etc.).
- Autonomic disorders.
- Poor heartbeat.
- Diarrhea.
- Dry mouth.
- Excessive sweating.
Second phase
Characteristic of stage II of alcohol dependence, when binge drinking lasts more than three, up to 10 days:
- Autonomic manifestations are accompanied by neurological disorders.
- Disturbances in the functioning of internal organs with corresponding symptoms.
- Hyperemia of the whites of the eyes and epidermis.
- Tachycardia.
- Pressure surges.
- Vomiting, nausea.
- Feeling of heaviness in the head, foggy consciousness.
- Gait disturbances.
- Muscle tone is reduced.
- Trembling, tremor of eyelids, hands, tongue.
Third degree
The symptoms of a hangover develop against the background of the transition of pathological addiction from stage II to stage III, when binge drinking continues for more than 10 days:
- Preservation of somatic and vegetative manifestations, but they become secondary.
- Clinical manifestations are determined by disturbances in the patient’s mental state.
- Aggressive attitude towards others.
- High irritability.
- Sad, depressed mood.
- Anxiety followed by feelings of guilt.
- Nightmares.
- Sleep disorders.
Manifestations of a hangover can have different colors, the predominance and severity of which depend on the condition of the patient’s internal organs and the degree of alcoholism. Hangover syndrome in the later stages of addiction is accompanied by an irresistible craving for alcohol.
How to replace Eufillin
In pharmacy chains you can find only one synonymous drug - Aminophylline-Eskom. In addition, Eufillin has analogs that also belong to the group of bronchodilators, but contain other active ingredients. These include:
- Theophylline (in the form of tablets and rectal suppositories);
- Diprophylline (tablet and injection forms);
- Theobromine;
- Teofedrine-N;
- Theotard.
Since Eufillin is most often prescribed to pregnant women for gestosis, high blood pressure and edema, the drug can be replaced with medications aimed specifically at combating these pathological conditions.
Medicines substitutes for Eufillin for expectant mothers - table
| Name | Dosage forms | Active ingredients | Indications | Contraindications | Features of use during gestation |
| Theotard | capsules | theophylline |
|
| Not recommended in the third trimester due to the possibility of weakening labor. |
| Canephron N |
|
|
|
| Prescribed by a doctor after carefully weighing the possible risks. |
| Chime |
| dipyridamole |
|
| Allowed during gestation, but in the later stages it is taken with caution. |
| Askorutin | pills |
|
|
| Prohibited in the first trimester, allowed for use in later periods. |
| Verapamil |
| verapamil hydrochloride |
|
| The instructions do not recommend taking the drug during gestation, however, many years of practice have shown the effectiveness of the drug during pregnancy. |
Analogs of Eufillin - gallery
Theotard is a bronchodilator
Curantil is a drug that dilates the coronary vessels
Verapamil is often prescribed for gestosis
Canephron N is used to get rid of edema
Ascorutin is prescribed for gestosis and high blood pressure
Vengerovsky / 40-41 Diuretics
LECTURE
40
DIURETICS (GENERAL CHARACTERISTICS, XANTHINES, CARBONAN HYDRASE INHIBITORS, OSMOTIC DIURETICS)
Diuretics, having a direct effect on the functional state of nephrons, increase natriuresis and diuresis. They are used to treat edema, arterial hypertension, and accelerate the elimination of poisons in case of poisoning.
Retention of salts and water in the body with increased tissue hydration, the formation of edema and fluid accumulation in the cavities accompanies many diseases of the kidneys, liver, cardiovascular failure, and hormonal dysfunctions. Salts and water quickly move from the vascular bed into the interstitial fluid and then into the cells (the total surface of the capillaries is 20,000 m2).
Not all drugs that increase diuresis belong to the group of diuretics. For example, drugs that improve blood supply to the kidneys as a result of increased heart contractions (cardiac glycosides) and dilation of the renal artery (vasodilators) have a diuretic effect. They are used to eliminate edema in heart failure.
The kidneys contain about 1 million nephrons, where filtration, reabsorption and secretion occur.
In vascular glomeruli
blood plasma is filtered through the membranes of capillaries and nephron capsules at a rate of 120 ml/min. Almost all blood plasma passes through the membrane pores, with the exception of proteins with large molecular weights, substances associated with proteins, and lipids.
In the proximal convoluted tubule
65% of the ultrafiltrate is reabsorbed -
Na \ K\Ca2 ' (
70%) returns to the blood.
MD 2 '
(20-25%). HCO3. phosphates (80%), amino acids, glucose, vitamins, water is absorbed along the osmotic gradient. Primary urine in the final section of the proximal tubules resembles a simple sodium chloride solution, isoosmotic to the interstitial fluid and blood plasma. In the middle segment of the proximal tubules there are systems for the secretion of organic acids (uric, lara-aminohippuric acids, diuretics, antibiotics of the p-lactam group). Organic bases (creatinine, choline, novocainamide) are secreted in the initial and middle segments.
In the descending limb of the nephron loop
Water is reabsorbed along an osmotic gradient into the hyperosmotic medulla of the kidney. Primary urine becomes hyperosmotic.
In the thin segment of the ascending limb of the loop
Na \ Cl ~
are reabsorbed .
In the thick segment of the ascending limb of the loop
Na \ \
C1, Ca2 * (
20%),
Md2 * (70-75%) are reabsorbed Primary urine first becomes isoosmotic, and then, as it moves along the ascending limb and absorbs ions, it becomes hypoosmotic. In this case, the interstitial fluid of the medulla becomes hyperosmotic, which is necessary for the reabsorption of water in the descending limb. In total, 25% of primary urine is reabsorbed in the nephron loop.
In the distal convoluted tubules
Na , Ca 2+
and
C1
are reabsorbed without water entering the blood,
K*
and
H
. Primary urine retains the hypoosmotic state that arose in the ascending limb of the loop.
Hormones participate in the reabsorption of ions in the distal convoluted tubules:
• The mineralocorticoid aldosterone increases Na+ reabsorption and stimulates K^
and
N' \
'
Parathyroidin increases the reabsorption of
Ca 2+
through the channels of the apical membrane and with the participation of
Na , Ca 2+
of the basolateral membrane.
In the collecting ducts,
under the influence of vasopressin (antidiuretic hormone), water is reabsorbed into the hyperosmotic environment of the medulla of the kidney, aldosterone-dependent
Na
K
and
H
secretion
Md 2+
is absorbed . The urine becomes hyperosmotic.
Urine formation is regulated by tubular-glomerular feedback.
With an increase in the concentration
of NaCI in
primary urine, the macula densa receptors are irritated, which stimulates the secretion of adenosine. This mediator, by narrowing the afferent arteriole of the glomeruli, limits filtration.
The following membranes are distinguished in nephrocytes:
• Apical (lumenal) membrane
-
facing the lumen of the tubules to the primary urine;
• basement membrane
- facing the interstitial fluid;
• Lateral membranes
-
create intercellular gaps.
TYPES OF SUBSTANCE TRANSPORT IN THE KIDNEY
7. Passive diffusion
• Filtration of water through cell pores and intercellular cracks into a medium with a higher osmotic pressure;
• Simple diffusion of lipophilic substances along a concentration gradient;
• Diffusion of ions through specific channels along an electrochemical gradient;
• Facilitated diffusion (uniport) along an electrochemical gradient with the participation of carrier proteins;
• Symport (cotransport) - facilitated diffusion of a cation and anion in one direction with the participation of a common carrier protein (sym-porter);
• Antiport (countertransport) - facilitated diffusion of ions with the same charge in opposite directions with the participation of a common carrier protein (antiporter). The symport and antiport systems function in the apical and basal membranes of nephrocytes. During the symport process of Na
passes through the apical membrane along an electrochemical gradient and, neutralizing the negative charge inside the cells, creates conditions for the entry of C/- and HCO3.” Then the anions flow along an electrochemical gradient through the basement membrane into the interstitial fluid, reducing its positive charge, which facilitates the release of Na\
Antiport requires a decrease in the positive charge of primary urine after Na
into nephrocytes through the apical membrane.
This forms an electrochemical gradient for the release of H2
into the lumen of the tubules.
of HCO^~
occurs along an electrochemical gradient into the interstitial fluid, associated with the entry into nephrocytes C/ - (Fig. 40.1).
2.
Active diffusion in the basement membrane of nephrocytes
• Removal of 3 Na
against the electrochemical gradient into the interstitial fluid in exchange for the return
of 2K^
with the participation of
Na /K
-ATPase;
• Ca 2
and
MD 2
with the participation, respectively, of calcium-dependent
my ATPase and magnesium-dependent ATPase.
Basement membrane pumps create an electrochemical gradient for passive diffusion of ions across the apical membrane of nephrocytes. The formation of energy in the renal cortex is ensured by oxidative phosphorylation (the kidneys consume 10% of the oxygen entering the body); In the medulla, energy is supplied by anaerobic glycolysis.
Diuretics enhance the filtration of primary urine in the glomeruli and reduce the reabsorption of ions and water in the tubules. Inhibition of tubular reabsorption most effectively increases diuresis:
• Without changing reabsorption, the volume of secondary urine can be doubled (from 1.5 to 3 l), if the volume of ultrafiltrate also doubles (from 150 to 300 l), this is not feasible due to limited blood circulation;
• Secondary urine volume doubles when water reabsorption decreases by only 1%.
CLASSIFICATION OF DIURETICS
By the nature of the diuretic effect
• Hydrouretics that cause predominantly water diuresis are osmotic diuretics;
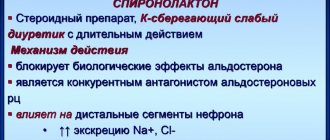
• Saluretics that primarily inhibit the reabsorption of ions are carbonic anhydrase inhibitors, potent diuretics, thiazides, thiazide-like and potassium-sparing diuretics.
According to the localization of the diuretic effect in the nephron
• Diuretics. predominantly increasing glomerular filtration - dimethylxanthines;
• Diuretics that inhibit reabsorption
- in the proximal convoluted tubules - carbonic anhydrase inhibitors;
- in the nephron loop - osmotic diuretics;
- in the thick segment of the ascending limb of the nephron loop - potent diuretics (inhibitors of Na ^- K ^-2 CI ~ symport)',
- in the distal convoluted tubules - thiazides, thiazide-like diuretics (inhibitors of Na ^-CI ' )}
-
in
the distal convoluted tubules and collecting ducts - potassium-sparing diuretics.
Na + is indicated in parentheses )
- Strong diuretics - potent diuretics (15-25%);
- Medium strength diuretics - osmotic diuretics (5-8%), thiazides, thiazide-like diuretics (5-10%);
- Weak diuretics - dimethylxanthines, carbonic anhydrase inhibitors, potassium-sparing diuretics (3-5%).
According to the speed of onset and duration of diuretic action
- Diuretics that cause a rapid and short-term diuretic effect - osmotic and potent diuretics;
• Diuretics of medium speed and duration of action - dimethylxanthines, carbonic anhydrase inhibitors. thiazides, potassium-sparing diuretics (triamterene, amiloride);
• Diuretics with delayed and prolonged diuretic effect - thiazide-like diuretics. potassium-sparing diuretics (spironolactone).
By
their effect on the acid-base balance of the blood
• Diuretics that cause severe metabolic acidosis are carbonic anhydrase inhibitors. ammonium chloride;
• Diuretics. causing moderate metabolic acidosis. - potassium-sparing diuretics;
• Diuretics that cause mild metabolic alkalosis. - potent diuretics. thiazides, thiazide-like diuretics.
Lo
influence on the excretion of potassium ions
• Strong kaliuretics (diuresis/kaliuresis = 1/1) - carbonic anhydrase inhibitors. thiazides;
• Moderate kaliuretics (diuresis/kaliuresis = 1/0.75) are potent diuretics. thiazide-like diuretics;
• Small kaliuretics (diuresis/kaliuresis = 1/0.25) - osmotic diuretics;
• Potassium-sparing diuretics.
By influence on the excretion of calcium ions
• Diuretics. increasing Ca^ excretion. - potent diuretics;
• Diuretics that reduce Ca2 excretion - thiazides, thiazide-like diuretics.
The effect of diuretics on the excretion of ions, uric acid and renal hemodynamics is presented in Tables 40.1 and 40.2.
DIURETICS,
INCREASING FILTRATION IN Glomeruli
Dimethylxanthines
Dimethylxanthines include:
• THEOPHYLLINE
- 1,3-dimethylxanthine;
• EUPHYLLINE
(AMINOPHYLLINE} -
soluble theophylline. 80% theophylline + 20% ethylenediamine;
• THEOBROMINE
- 3,7-dimethylxanthine.
Theophylline drug, aminophylline, is used as a diuretic. Theophylline, by blocking A1 adenosine receptors, eliminates their inhibitory effect on the activity of adenylate cyclase and the synthesis of cAMP. In large doses, theophylline inhibits phosphodiesterase and delays the inactivation of cyclic nucleotides. Thus, when aminophylline is used in cells, the level of cAMP increases.
Eufillin has a weak diuretic effect (increases Na
up to 3-5%):
• Increases blood supply to the kidneys (increases cardiac activity and dilates the renal artery);
• Stimulates glomerular filtration (increases renal blood flow, dilates the afferent arteriole to a greater extent than the efferent arteriole);
• Reduces the contact of nephrocytes with urine, accelerating its movement through the tubules;
• Inhibits the reabsorption of water in the descending limb of the nephron loop (promotes the removal of ions and urea from the renal medulla through dilated vessels into the bloodstream, which reduces the osmotic gradient between primary urine and interstitial fluid);
• Suppresses Na
Na ^- HCO ^'
symport in the basement membrane).
Eufillin is taken orally, injected into muscles and veins for left ventricular failure, arterial hypertension, cerebrovascular accidents, and is also combined with diuretics that worsen renal blood flow. The diuretic effect develops after 15-30 minutes and lasts 2-3 hours.
The side effects of aminophylline when taken orally are dyspeptic disorders, when injected into muscles - local soreness, and when quickly infused into a vein - dizziness, headache, palpitations. nausea, vomiting, convulsions, arterial hypotension. Sensitization to ethylenediamine causes exfoliative dermatitis and fever.
The use of aminophylline is contraindicated in cases of significant arterial hypotension. paroxysmal tachycardia, extrasystole, angina pectoris, myocardial infarction, epilepsy.
DIURETICS INHIBITED REABSORPTION IN THE PROXIMAL CONVOLVED TUBE
Carbonic anhydrase inhibitors
DIACARB
(ACETAZOLAMIDE,
DIAMOX, FONURIT) with the help of a sulfonamide group inhibits the zinc-containing active center of carbonic anhydrase of various tissues. Unlike antimicrobial sulfonamides, in diacarb the sulfonamide group is attached not to the aromatic ring, but to the thiadiazine heterocycle.
Carbonic anhydrase accelerates the hydration and dehydration reactions of carbonic acid by 1000 times. Carbonic anhydrase isoenzyme II functions in the brush border of the apical membrane of the proximal tubules, and isoenzyme IV is located in the cytoplasm.
Na reabsorption
with the participation of carbonic anhydrase occurs in several stages:
Na enters the cells
in exchange for the release of
H^\
• Carbonic acid is formed in the urine:
• Brush border carbonic anhydrase catalyzes the dehydration of carbonic acid to release carbon dioxide:
• Carbon dioxide as a lipophilic substance is reabsorbed into nephrocytes and in their cytoplasm, with the participation of the cytoplasmic isoenzyme carbonic anhydrase, adds water:
• Carbonic acid in cells dissociates into ions:
• H^
exit into primary urine by antiport with N;
• Anions HCO3~
are excreted into the blood through the basement membrane by symport with
Na + .
The urine reaction becomes acidic, and an alkaline buffer enters the blood to maintain acid-base balance.
When carbonic anhydrase is blocked with diacarb, the dehydration of carbonic acid in primary urine and its formation in the cytoplasm of nephrocytes are disrupted, therefore the reabsorption of Na ^,
HCO3 -
and the release of
H^
into The urine reaction shifts to the alkaline side (pH = 8.0).
Diacarb increases Na
up to 3-5%,
K^
- up to 70%,
HCO 3 ' -
up to 35%, significantly increases the excretion of phosphates (poorly reabsorbed disubstituted phosphates are formed in alkaline urine), weakly stimulates the excretion of C/-, does not affect the excretion of
Ca 2 ^ , Md 2 ^,
with long-term use, it disrupts the secretion of uric acid and impairs blood flow in the kidneys.
Diacarb has a weak diuretic effect, since the reabsorption of Na
compensatory increases in the ascending limb of the loop, distal convoluted tubules and the beginning of the collecting ducts.
A small portion of bicarbonate is reabsorbed without the participation of carbonic anhydrase. NaHCO ,
increasing the negative electrical potential on the apical membrane of the distal nephron, stimulating K secretion
Diacarb increases HCO excretion"
more than C/ Bicarbonate resources are gradually depleted, which causes metabolic hyperchloremic acidosis. After a few days of therapy, addiction occurs due to hyperchloremic acidosis and increased tubular-glomerular feedback.
Diacarb blocks carbonic anhydrase in addition to the kidneys and in other tissues:
• In the ciliary (ciliary) body of the eyeball, it inhibits the secretion of intraocular fluid;
• In the pia mater, it suppresses the production of cerebrospinal fluid (intracranial pressure and neuronal excitability are reduced);
• In the parietal cells of the gastric glands, the formation of hydrochloric acid is disrupted.
Diacarb is well absorbed from the intestine. The diuretic effect occurs after 2 hours, reaches a maximum after 6 hours and lasts 12 hours. The drug is excreted from the body unchanged by the kidneys. The half-life period is 6-9 hours.
Diacarb is prescribed in courses of 3-5 days with a break of 2-3 days to replenish alkaline blood reserves and eliminate hypokalemia.
Currently, Diacarb is used for course treatment of glaucoma and relief of glaucomatous crisis, treatment of hydrocephalus, absence seizures in epilepsy, and acute mountain sickness. It is also prescribed for cardiopulmonary failure, pulmonary emphysema, for the correction of hypochloremic alkalosis, hyperkalemia and hyperphosphatemia. Diacarb. creating an alkaline reaction in urine, can be used to dissolve cystine kidney stones and treat mild poisoning with acid drugs - salicylates. barbiturates (in an alkaline environment, organic acids dissociate, lose their solubility in lipids and the ability to be reabsorbed by simple diffusion).
Side effects of Diacarb are as follows:
• Severe hypokalemia;
• Hyperchloremic acidosis;
• Formation of kidney stones from calcium phosphate and calcium citrate:
• Reducing the acidity of gastric juice;
• Allergic reactions, agranulocytosis.
Hypokalemia is manifested by drowsiness, disorientation, paresthesia, paralytic ileus, nephropathy, and cardiac arrhythmia. To correct it, limit the consumption of table salt (2-2.5 g per day); prescribe a diet enriched with potassium; use potassium preparations (panangin, asparkam) or angiotensin-converting enzyme inhibitors. In case of severe hyperchloremic acidosis, sodium bicarbonate is injected into a vein.
Diacarb is contraindicated in severe respiratory failure, uremia, diabetes mellitus, adrenal insufficiency, hypokalemia, a tendency to acidosis, and in the first 3 months of pregnancy. In patients with liver cirrhosis, diacarb therapy increases hypokalemia and creates the risk of hepatic encephalopathy (ammonia reabsorption increases).
A carbonic anhydrase inhibitor has been created for local action on the eye with open-angle glaucoma - DORZOLAMIDE.
It suppresses the production of intraocular fluid by 50% 2 hours after use in eye drops. The duration of the hypotensive effect is 12 hours. Addiction to dorzolamide does not develop over a year of constant use. Side effects are a short-term burning sensation in the eye (in 80% of people), a feeling of bitterness in the mouth (in 15%), allergic conjunctivitis, superficial punctate keratitis, increased contrast sensitivity. Resorptive toxic effects occur less frequently - headache, fatigue, epidermal necrolysis, agranulocytosis, aplastic anemia. Contraindicated in case of intolerance to sulfonamides, liver and kidney diseases, pregnancy, lactation.
DIURETICS INHIBITED REABSORPTION IN THE NEPHRON LOOP
Osmotic diuretics
Osmotic diuretics are highly polar substances (mannitol, urea, isosorbide, glycerol). Several drugs are used in medical practice:
• MANNITOL
(MANNITOL)
• UREA
(Urea)
Hexahydric alcohol mannitol does not penetrate histohematic barriers (with the exception of the glomerular filter), urea has a weak ability to enter the interstitial fluid.
When mannitol and urea are administered into a vein, the osmotic pressure of the blood increases significantly, which causes the transfer of water from the cells into the blood. The circulating blood volume (CBV) initially increases, but then decreases as the diuretic effect develops. Osmotic diuretics reduce blood viscosity and stimulate the secretion of atrial (atrial) natriuretic peptide.
The hydrouretic mannitol is used as a diuretic. It improves blood supply to the kidneys by stimulating the formation of vasodilating factors - prostaglandin E2 and prostacyclin in the endothelium of the renal artery. It is well filtered in the glomeruli, but as a polar substance it is not reabsorbed. Increases the osmotic pressure of primary urine, promotes the removal of ions and urea from the medulla of the kidneys into the bloodstream. As a result of these effects, the osmotic gradient necessary for the reabsorption of water from the descending limb of the nephron loop is eliminated. The ascending limb receives diluted urine with a low concentration of NaCI ,
which reduces the gradient of ion reabsorption.
Mannitol increases Na
up to 5-8%, moderately increases the excretion of
K*,
Ca2^
Md 2 ^,
C/-, HCO3″ and phosphates, variably changes the acid-base balance of the blood - causes both acidosis and alkalosis;
Mannitol is injected into a vein in the form of 10-20% solutions. Diuresis increases after 15-20 minutes and remains at an elevated level for 4-5 hours. The half-life of mannitol is 0.25-1.7 hours.
Mannitol is used as a dehydrating and diuretic for the following indications:
• Acute attack of glaucoma and preparation of patients with glaucoma for surgery;
• Brain edema in patients with an intact blood-brain barrier (reduces intracranial pressure by 60-80%, reduces edema-swelling of neurons, stabilizes lysosomes, suppresses lipid peroxidation);
• Acute necrosis of the renal tubules during shock, infections, hemolytic reaction and intoxication (improves blood supply to the kidneys and filtration, removes detritus from the tubules, reduces the concentration of nephrotoxins in primary urine, counteracts the swelling of nephrocytes);
• Prevention of renal ischemia during operations with artificial circulation;
• The need for hemodilution and forced diuresis in case of poisoning (before the onset of anuria).
An overdose of osmotic diuretics is accompanied by severe dehydration, arterial hypotension, thrombosis, thirst, dyspeptic disorders and hallucinations. In case of traumatic cerebral edema, diuretics, penetrating the damaged blood-brain barrier, attract water with them.
Urea has an irritating effect on the veins, creating the danger of thrombophlebitis. When urea gets under the skin, necrosis develops.
Osmotic diuretics are contraindicated for pulmonary edema in patients with heart failure, as they increase blood volume, venous and arterial pressure, pressure in the pulmonary circulation and, as a result, preload and afterload on the heart. Osmotic diuretics are not prescribed in the stage of anuria with renal failure, cerebral edema with a damaged blood-brain barrier, or intracranial bleeding. Urea is contraindicated in uremia and liver failure.
DIURETICS INHIBITED REABSORPTION IN THE NEPHRON LOOP
Potent diuretics (
Na ^ -KCI )
Potent diuretics have a powerful and short-lived diuretic effect . Information on medicines is presented in Table 41.1.
Potent diuretics are organic acids. Furosemide, bufenox, xipamide, pyretanide and torasemide have a sulfonamide group, ethacrynic acid is a prodrug derived from dichlorophenoxyacetic acid. The active compound is formed after the binding of the methylene group of ethacrynic acid to the sulfhydryl group of cysteine.
Potent diuretics are secreted in the proximal convoluted tubules, enter the primary urine and, with its flow, reach the thick segment of the ascending limb of the nephron loop. Here in the apical membrane of nephrocytes they inhibit the symport of Na ^- K ^-2 CI ~,
blocking the C/- binding site on the symporter protein.
E increases
and prostacyclin from arachidonic acid in fat depots.
These metabolites dilate the renal artery and improve blood supply to the kidneys. In nephrocytes, diuretics inactivate Na /K
-ATPase of the basement membrane, microsomal Ca2-dependent ATPase. adenylate cyclase, phosphodiesterase, prostaglandin dehydrogenase, disrupt tissue respiration. Ethacrynic acid weakens the effect of vasopressin (antidiuretic hormone) in the collecting ducts.
sodium excretion increases
(15-25%),
K, H , Ca 2 ^ Md 2 CI -.
Agents with a sulfonamide group, by inhibiting carbonic anhydrase in the proximal convoluted tubule, increase the excretion of
HCO 3
and phosphates.
In the lumen of the ascending limb of the loop, the positive potential normally caused by the cyclic transport of potassium ions decreases. This stimulates the excretion of magnesium and calcium ions. Severe hypomagnesemia develops. The loss of calcium is compensated by its reabsorption in the distal convoluted tubules. Excessive secretion of potassium and hydrogen ions occurs in the distal tubules and collecting ducts in response to large amounts of NaCI
and water.
Potent diuretics cause metabolic hypochloremic alkalosis, as they increase secretion into the urine /-/+, stimulate the excretion of Cl ,
than the removal of
HCO 3 .
The diuretic effect of furosemide and xipamide persists when glomerular filtration decreases to 5-10 ml/min; other drugs are effective when glomerular filtration is at least 30 ml/min. Potent diuretics weaken tubular-glomerular feedback by preventing the entry of NaCI
into
macula densa cells.
Strong diuretics dilate arteries and veins. Dilation of the arteries causes hypotension. Venous deposition of blood reduces pre-load on the heart. Extracellular water is removed from tissues through dilated veins into the blood.
As is known, an increase in blood volume and Na* content in the blood is necessary in the initial period of congestive heart failure to maintain cardiac output and sufficient blood supply to organs. With an increase in diastolic blood volume and pressure in the left ventricle, heart contractions increase according to the Frank-Starling mechanism. Subsequently, as the disease progresses, myogenic dilatation and weakening of heart contractions occur. Diuretics increase venous deposition of blood (already in the first 10 minutes after injection into a vein), reduce the volume of blood volume and filling pressure of the left ventricle with blood (preload). Thus, they create conditions for restoring the Frank-Starling mechanism and enhancing the contractile function of the myocardium. Diuretic therapy in small doses is combined with limiting table salt in the diet to 1-3 g per day. When using drugs in large doses, limiting sodium chloride intake can cause dehydration and hypochloremic alkalosis.
Reviews from women
Accepted. They prescribed it to me. Because of these side effects, at the end of November I could only sleep half-sitting and next to the open window. But in a week I lost three kilograms. After that, the doctor canceled it. If a gynecologist prescribes it, it means there is a need.
Kisa_myau.ru
https://deti.mail.ru/forum/v_ozhidanii_chuda/beremennost/jeufillin_pri_beremennosti_uzhasnyj_uzhas/
I took Eufillin for edema. However, they also placed IVs with something, I don’t remember. Within 3-4 days the swelling went away and never came back. This was about 35 weeks ago. It was August-September, and I ate a lot of watermelons and melons. Normally, the kidneys should have excreted the fluid themselves, but apparently something in the body failed. Before 33 weeks, I gained 5 kg in total, and then in 2 weeks I gained almost 4. They put me in storage - they treated me, and after 5 days I was discharged. Apparently, it was necessary to help the body a little. So Eufillin definitely helps with edema.
Pipuh
https://www.babyplan.ru/blog/56965/entry-173839-eufillin-ot-otekov#ixzz4LFHHdgQu
I was also prescribed Eufillin for edema + Brusniver 4 times a day. Helps. The doctor immediately told me - don’t read the instructions, they are outdated (I’ll say right away that I trust the doctor, this is not a mossy woman from the LCD, but a practicing clinical doctor).
Underkne
https://www.babyplan.ru/blog/56965/entry-173839-eufillin-ot-otekov#ixzz4LFHkxLD8
I took Eufillin during my first pregnancy - it made me feel terrible, I couldn’t stand at all, my blood pressure dropped significantly. I lasted only one day, then quit - in my opinion, there were too many side effects, and it’s not clear what is more: benefit or harm.
listic
https://2006–2009.littleone.ru/archive/index.php/t-443101.html
Compatibility
Alcohol enhances the absorption of the drug.
It is important to know that the pharmaceutical drug "Eufillin", which has a diuretic effect, is incompatible with acid solutions. It should also be taken into account that when taken simultaneously with antibacterial agents, the healing effects of aminophylline may be enhanced. It is worth considering that ethyl found in alcohol, as well as nicotine, which is abused by smokers, can accelerate the absorption of drugs and activate the metabolic process.
Analogs
If for some reason it is not possible to eliminate swelling with Eufillin, it can be replaced with the following medications:
- Diprophylline;
- Theophylline;
- Neophylline;
- Teopek.
Can women who are expecting the birth of a child take this medicine? The drug Eufillin is a powerful and very effective remedy against edema during pregnancy, however, it has a wide range of contraindications and possible side effects, so it should only be taken under the supervision of a physician.
When can a doctor prescribe Eufillin to a pregnant woman?
The indications according to which Eufillin is prescribed to a pregnant woman are not specified in the instructions. But despite this, this medication has practically become an integral part of therapeutic therapy in the fight against pathological swelling during gestation.
It is worth noting that in the first three months of bearing a baby, doctors do not prescribe Eufillin, since it is during this period that the baby’s organ systems are being formed.
Starting from the second trimester of pregnancy, when active growth of the fetus begins and the uterus puts pressure on all the blood vessels and organs of the peritoneum, stagnation of fluid in the body is observed. This is primarily due to the fact that the blood cannot circulate normally and ensure the normal functioning of all organs, and the liver cannot cope with the double load. As a result of fluid stagnation, the expectant mother experiences swelling.
As a rule, swelling of the legs is regarded as a normal condition for a pregnant woman at the end of the second and third trimester. Moreover, it does not require any treatment. But if the area of edema extends above the waist, and is accompanied by headaches, increased blood pressure, and the presence of protein in the urine, then we are talking about gestosis.
Pathological swelling during pregnancy is fraught with:
- fetal hypoxia;
- placental insufficiency and circulatory disorders in the umbilical cord;
- miscarriage or the onset of premature labor;
- intoxication of the fetus and the development of intrauterine infection;
- intoxication of the mother's body.
Determining swelling on your own without the use of special devices and tests will not be difficult for any expectant mother. To do this, you need to hold your finger on the surface of the body for 20 seconds. If a depression remains at the point of pressure, then we can talk about edema. When swelling occurs, it becomes difficult for a pregnant woman to put on her previously familiar shoes and clothes; the elastic bands dig into the body. This is especially observed in the afternoon and late evening after physical activity.
When else can a doctor prescribe the drug to an expectant mother:
- with heart failure;
- in case of circulatory disorders in the vessels of the brain;
- in case of kidney dysfunction;
- for bronchial asthma. In this case, the drug is prescribed in combination with other medications.
Personally, while carrying the baby, I did not have severe swelling, much less problems with excess weight. But still, slight swelling was observed. In order not to aggravate the situation with new complications that develop as a result of fluid stagnation in the body, I stopped eating pickles and also limited the amount of fluid. But this does not mean that I completely gave up drinking. Before pregnancy, as a rule, I drank 2.5 liters of water per day during pregnancy - 1.5 - 2 liters. Moreover, she did not drink a whole glass at a time, but divided this volume into 3-4 doses. I tried to drink in small sips. And as it turned out, this way you can cope with thirst much more effectively. Moreover, there is enough information on the Internet that a woman who suffers from edema should completely give up liquids. This is a misconception that is not supported by medical facts. If the body requires, especially two, then it should receive it, but in reasonable quantities. At first, I even tried to drink kidney diuretic teas, of course, after consulting with a gynecologist, but I didn’t see much result from using them.