X-ray examination takes a leading place in identifying kidney and ureteral stones. The most common method is survey urography.” With its help, you can determine the size and shape of the stone, as well as approximately its location.
A survey urogram should cover the entire kidney area
and urinary tract on both sides. Not all stones cast a shadow in a survey photo. The chemical composition of stones, their size and location are extremely diverse. G_^salads and phosphates contain elements with a large atomic mass and give an intense shadow._ In 10% of cases, stones are visible on a survey x-ray (urate, cystine^ and xanthine stones), since their density in relation to x-rays approaches soft tissue density (X-ray negative stones). With an abnormality of the urinary tract, the shadow of a stone on a survey image can be detected outside the usual location of the kidneys and ureters.
It should be borne in mind that a shadow suspicious for a kidney or ureteral calculus may belong to a foreign body, a calcified lymph node, a gall bladder stone, etc.
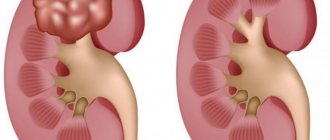
In the projection of the small pelvis, rounded shadows are often visible - 1/phleboliths, similar to stone. Their distinctive feature is regularly round, clear contours and enlightenment in the center. Based on survey urography, a diagnosis of coral-shaped kidney stones is made, which are a cast of the pyelocaliceal system and give a dense shadow in the area of projection of the kidneys (Fig. 1G), with the exception of X-ray negative stones. In children, especially younger children, it is not always possible to achieve good quality radiographs, which is due to severe flatulence and restless behavior during the examination.
After a survey image of the urinary tract, excretory urolithiasis should be performed. Based on its data, it is possible to determine whether the shadow visible on the survey image refers to the urinary tract. Excretory urography allows you to identify the anatomical and functional position of the kidneys, determine the type of pelvis (intrarenal or extrarenal) and the localization of the stone (in the pelvis, calyx or ureter). In cases where a stone disrupts the outflow of urine, excretory urograms reveal changes in the pyelocaliceal system (hydrocalicosis, pyeloectasia). Usually, the images show a shadow of the stone against the background of a radiopaque substance (Fig. 99). If the stone occludes the ureter, then the radiopaque substance is located above the stone in the non-dilated ureter as “pointing” to the stone.
and an X-ray-negative stone against the background of a radiopaque substance, a filling defect corresponding to the calculus is visible. As a rule, excretory urography gives a complete picture of the functional capacity of the kidney, however, after an attack of renal colic, the kidney is in a state of blockade and temporarily does not function. When examining the “4Sh1k-national ability of such a kidney,” there is great help I provide isotope research methods. They make it possible to establish that in most cases, a blocked, “silent” kidney retains its functional capacity and that there are no irreversible changes in the caudal apparatus. Previous Next
www.urologi.ru
Tactics for renal colic
If a patient with renal colic has previously been diagnosed with an X-ray positive stone, then a plain X-ray of the abdomen is performed to clarify the size and location of the stone and select the optimal treatment tactics.
Patients with an unclear clinical picture, who have no history of urolithiasis or have been identified with X-ray negative urinary stones, undergo spiral computed tomography (CT) without contrast or excretory urography. Ultrasound examination (ultrasound) is informative for kidney stones, but does not always reveal ureteral stones.
If the patient has both kidneys, his condition is stable, there are no signs of infection, the obstruction of the urinary tract is incomplete and does not threaten renal failure, you can limit yourself to analgesics (it is often necessary to use narcotic analgesics). Otherwise, urgent urine diversion is indicated by installing a stent in the ureter or percutaneous nephrostomy. In case of infection, antibiotics are immediately prescribed. The need for surgical treatment is determined by the size of the stone. With conservative treatment, stones up to 4 mm in size pass away on their own in 90% of cases, and stones in size of 6 mm or more pass away on their own in only 10% of cases. If the pain persists or after 3-4 weeks of conservative measures the stone does not move or pass away, surgical treatment is indicated.
Urolithiasis (continued...)
An increase in calcium levels (hypercalcemia), a decrease in the level of phosphorus and magnesium in the blood serum are signs of impaired metabolism, which are considered as risk factors for recurrent stone formation and require the exclusion of the renal form of primary hyperparathyroidism.
An increase in the level of uric acid (hyperuricemia) in the blood serum is observed with urate nephrolithiasis. Hyperuricemia and hyperuricuria (hyperuricosuria) indicate impaired synthesis of uric acid, which occurs with uric acid diathesis, gout and renal failure.
Hyperphosphaturia may be a manifestation of phosphate diathesis, congenital or acquired as a result of primary diseases of the stomach or central nervous system. More often, phosphaturia is false (pH 7.0 and higher), which depends on alkali-forming bacteria (Proteus).
A study of hormone levels (calcitonin and parathyroid hormone) is carried out in the diagnosis of hyperparathyroidism, especially in patients with staghorn, bilateral and recurrent stones with elevated serum calcium levels.
Zimnitsky's test is an assessment of the functional state of the kidneys based on the dynamics of urine density (normally 1005-1025) during the day in 8 portions of urine. The test is the most physiological. A decrease in the relative density of urine and monotony of indicators indicate renal dysfunction.
Bacteriological examination (culture) of urine makes it possible to identify the microflora of urine and determine the titer of bacteriuria. Bacteriological urine cultures with determination of the sensitivity of microflora to antibacterial drugs make it possible to carry out etiotropic treatment of pyelonephritis, which is one of the causes of recurrent stone formation.
Radiation diagnostics
Ultrasound examination makes it possible to assess the size, position and mobility of the kidneys, the size of the parenchyma, determine the presence and degree of dilatation of the pyelocaliceal system, the localization of the stone(s) and determine its linear dimensions. The ultrasound picture of a kidney stone is characterized by the presence of a hyperechoic area with an acoustic shadow (“track”) distal to it.
Survey radiography is indicated for the purpose of detecting and localizing radiopositive (radiopaque) shadows suspicious for stones in the projection of the kidneys, ureters and bladder.
Stones may be x-ray positive
(radio-opaque),
radio-negative
(radio-opaque) or low-contrast, which depends on the chemical composition (primarily the presence and amount of the calcium component) of urinary stones. Stones consisting of calcium oxalates and calcium phosphates are clearly visible on radiographs.
Stones consisting of uric acid and its salts (urates) are not visible on plain radiographs. The “invisibility” of a stone in a survey image may be due not only to its chemical composition, but also to poor image quality, projection of the stone onto the skeletal bones, and other reasons (ascites, obesity, etc.).
Kidney and ureteral stones often have to be differentiated from calcified lymph nodes and phleboliths in the pelvic area, gall bladder stones, stool shadows, and intestinal foreign bodies. Excretory urography helps to clarify the nature and localization of the shadow.
Indications for excretory urography are: a stone (ultrasound and survey X-ray data), the size of which does not allow for spontaneous passage, an X-ray negative stone, ureterohydronephrosis, bilateral nephrolithiasis, relapse of the disease, any pathological changes in the opposite kidney with unilateral nephrolithiasis, doubts about the genesis of renal colic etc.
It is recommended to carry it out in a pain-free period (outside of renal colic). With complete occlusion of the ureter by a stone, a radiopaque substance is located above the stone in the dilated ureter, as if indicating the stone (Lichtenberg's sign).
In the case of an X-ray negative kidney or ureteral stone, a filling defect corresponding to the stone is determined against the background of a radiopaque substance.
Additional X-ray examinations:
retrograde (ascending) ureteropyelography, and in the presence of nephrostomy drainage, antegrade pyelography are performed according to indications. Indications for performing retrograde ureteropyelography are doubts regarding the diagnosis of urolithiasis or if the stone is X-ray negative.
Computed tomography details the features of the angio-architectonics and anatomical and functional state of the kidneys and urinary tract, clarifies the localization of the stone (stones) and their structural density (densitometry), identifies possible anomalies of the urinary tract, as well as concomitant diseases of the abdominal organs, etc.
Modern and most informative methods for studying patients with urolithiasis are SCT and MSCT with the possibility of three-dimensional image reconstruction and virtual endoscopy, which detail the size, location and structural density of stones, the anatomical and functional state of the upper urinary tract, which determines the choice of treatment method. Modern types of CT detect stones of any location and X-ray positivity.
Magnetic resonance urography allows you to determine the level of obstruction of the urinary tract by a stone without contrast in patients with renal colic and with intolerance to a radiocontrast agent.
Complications.
The most common and serious complication of urolithiasis is acute obstructive pyelonephritis, in the event of which all therapeutic measures should be aimed at stopping the inflammatory process. Chronic calculous pyelonephritis is observed in a significant number of patients (90-98%), and its latent course periodically passes into the active phase in almost 2/3 of patients.
The persisting impaired passage of urine against the background of a chronic inflammatory process leads to the development of kidney shrinkage (nephrosclerosis), which is accompanied by a decrease in the functional state of the kidney, and the possible development of nephrogenic arterial hypertension. The most serious complication of urolithiasis is the development of acute and chronic renal failure (ARF and CRF).
Treatment.
Complex treatment of patients with urolithiasis should pursue the following goals: to relieve pain and especially an attack of renal colic, to promote the passage of small stones, to remove stones that, due to their size or for other reasons, cannot pass on their own, and to prevent recurrent stone formation.
Drug treatment
- Antispasmodics and antispasmodic analgesics
used as symptomatic therapy aimed at eliminating an attack of renal colic. Antispasmodic analgesics improve the passage of small stones and reduce tissue swelling during prolonged standing of the stone. The most commonly used drugs are no-shla (drotaverine) and baralgin.
- Herbal preparations
(canephron, cystone, cystenal, phytolysin) are prescribed to patients with urolithiasis, taking into account their diuretic, anti-inflammatory and antispasmodic effects.
- Preparations for dissolving (litholysis) of urinary stones.
Urate stones are subject to medicinal litholysis.
Taking into account that urate stones occur against the background of a decrease in urine pH (pH 5.0-5.5), then to dissolve them it is necessary to increase the urine pH (pH 6.2-6.8), which is achieved by taking citrate mixtures (blemaren , uralite U).
Therapy with citrate mixtures is carried out for 1 to 6 months, while the dissolution of stones is possible after 2-3 months.
- Medicines aimed at correcting biochemical changes in the blood and urine.
To correct purine metabolism, a drug that reduces the formation of uric acid is used - allopurinol (milurite), which inhibits the enzyme xanthine oxidase, which reduces the formation of uric acid, lowers its content in the blood serum, thereby preventing deposition in the kidneys and tissues. Indications for use are urate urolithiasis and other types of urolithiasis occurring with hyperuricemia.
- Antibacterial and non-steroidal anti-inflammatory drugs
used for the treatment of acute or chronic calculous pyelonephritis. The most commonly recommended are fluoroquinolones (ofloxacin, ciprofloxacin), cephalosporins (cefuroxime, cefazolin, ceftriaxone), aminoglycosides (gentamicin, amikacin, neomycin), carbapenems (thienam), etc.Antibacterial therapy in patients with urolithiasis is possible only with preserved urine outflow, taking into account the possibility of developing bacteriotoxic shock.
External shock wave lithotripsy. The first session of external shock wave lithotripsy (ESWL or ESWL) was performed in 1980 by Professor Ch. Chaussy (Germany).
Over the past years, due to its high efficiency and low invasiveness, it has become widely used and is the method of choice in the treatment of patients with urolithiasis.
Modern lithotripters are based on three main principles of shock wave generation: electromagnetic, electrohydraulic and piezoceramic. X-ray or ultrasonic control is used to direct a shock wave at the stone.
The effectiveness of remote lithotripsy is determined by the location, size and structural density of the stone, the anatomical and functional state of the upper urinary tract, the technical characteristics of the lithotripter, etc.
Optimal for extracorporeal lithotripsy are kidney stones up to 1.5-2.5 cm in size and ureteral stones up to 0.0-1.5 cm in size.
Open surgical interventions. Expansion of clinical indications for extracorporeal lithotripsy, percutaneous nephrolithotripsy, improvement of ureteroscopy and contact ureterolithotripsy techniques have changed the approach to the treatment of patients with urolithiasis - currently the percentage of “traditional” surgical interventions is no more than 5-15%.
Kidney surgeries in patients with urolithiasis can be organ-sapping (nephrectomy) or organ-preserving (pyelolithotomy, partial nephrectomy, nephrolithotomy).
Organ-preserving operations are the main ones in surgical treatment. Ureterolithotomy is used to remove stones from the ureter.
Currently, laparoscopic and retroperitoneal procedures
surgery (pyelolithotomy, ureterolithotomy) for patients with urolithiasis, which is considered as an alternative to open surgery for large kidney stones as the main method of treatment, and when remote or contact crushing is ineffective.
Prevention.
Therapeutic measures for urolithiasis should consist not only of removing the stone, but also of carrying out the necessary preventive treatment in order to prevent recurrent stone formation.
Relapses of the disease, depending on one or another form of urolithiasis, occur in 10-40% of patients.
The variety of causes and clinical forms of urolithiasis makes prevention a complex task, which should be individualized as much as possible depending on the clinical form of the disease, the chemical composition of urinary stones, etc.
Preventive treatment is based on dietary recommendations, correction of biochemical changes, medicinal litholysis (according to indications), etc. Comprehensive monitoring includes general and biochemical blood and urine tests, ultrasound of the urinary system, X-ray examination, etc.
The nature of nutrition is one of the significant risk factors for the development of urolithiasis, and therefore diet therapy, adequate maintenance of water balance, etc. play an important role. Dietary recommendations should take into account the results of a chemical analysis of the removed stone and be aimed at correcting biochemical changes.
Source: https://www.eurolab.ua/encyclopedia/Urology.patient/3022/?page=2
Radiation diagnostics
Radiation diagnostics is one of the most important stages of the examination. With its help, you can determine the number, size and location of stones, identify anatomical defects of the urinary tract, and assess kidney function. Research is carried out before treatment is prescribed.
More than 90% of urinary stones are radiopositive (that is, visible on X-ray). Calcium phosphate and calcium oxalate stones are best visible. All patients with urolithiasis first undergo a plain X-ray of the abdomen (kidneys—ureters—bladder). Studies using X-ray contrast agents are carried out later, since these substances can mask even a large stone.
From a survey image of the abdomen, one can determine the number, size and location of stones, and suggest their composition (based on X-ray positivity). Sometimes urinary stones are not visible on a plain X-ray due to the bone structures (sacrum, transverse processes of the vertebrae). In such cases, radiography in oblique or posterior direct projection is useful. Small, hard-to-see stones can be detected using CT.
Kidney ultrasound
This method helps to identify hydronephrosis and stones of the pyelocaliceal system, to assess the condition of the kidney parenchyma against the background of urinary tract obstruction. Ultrasound can detect X-ray negative stones. The middle and lower third of the ureter are poorly visible due to the accumulation of gas in the intestine and the projection onto the pelvic bones. Ultrasound can be used to exclude other causes of acute abdominal pain, as well as to monitor patients with recurrent urolithiasis (in this case, it replaces radiography and avoids unnecessary radiation exposure).
The method is especially valuable in the presence of X-ray negative filling defects in the renal pelvis or ureter. In addition, CT can detect anatomical defects, urinary tract obstruction and diseases accompanied by acute abdominal pain.
Spiral CT without contrast is now considered the best method for examining patients with acute flank pain. This method is fast, economical and more sensitive than radiography and ultrasound, allowing the detection of urinary stones of any composition. It can help identify other signs of stone obstruction in the urinary tract. In addition, spiral CT is useful in diagnosing causes of acute flank and abdominal pain such as appendicitis and diverticulitis.
Causes of stones
Coral stones are salt deposits that form in the collecting system (PUS) of the kidneys. The formation of stones occurs under the glomerular region in the renal tubules. When salts of uric, oxalic or phosphoric acid crystallize, deposits in different parts of the pelvis merge. The result is a large stone resembling sea coral.
The key cause of stone formation is a violation of protein and mineral metabolism. All patients with nephrolithiasis have proteinuria (protein in the urine). Protein molecules play the role of matrices on which acid salts are deposited. Over time, coral-like deposits fill the entire CLS.
Nephrologists and urologists identify factors that provoke nephrolithiasis:
- unbalanced diet;
- abuse of salty foods;
- dehydration;
- urogenital infections;
- non-compliance with drinking regime;
- deficiency of retinol and vitamin D;
- hyperfunction of the parathyroid glands;
- spinal cord injuries;
- peptic ulcer;
- alcohol abuse;
- osteoporosis;
- chronic kidney inflammation;
- sedentary lifestyle;
- abnormal structure of the urinary organs;
- tumors in the ureters, ureter;
- bone injuries.
In most cases, staghorn stones form in the right kidney.
In 15% of patients, bilateral nephrolithiasis is detected. Nephrolithiasis is a disease that is caused by many factors. But in 85% of cases, a shift in urine pH to the acidic or alkaline side is associated with metabolic and endocrine disorders. Coral stones are large in size. They almost completely occupy the calyces and pelvis, which leads to severe impairment of renal function.
Treatment and prevention
There are several general recommendations for the treatment of urolithiasis, regardless of its cause. Increase fluid intake so that diuresis (urine volume) exceeds 2 liters per day. A diet low in oxalates and sodium is prescribed (this reduces the excretion of oxalates and calcium).
After 3-4 months the patient is examined again. If, with the help of diet and plenty of fluids, it was possible to eliminate the factors contributing to the formation of urinary stones, this treatment is continued, examining daily urine every 6 months. If these measures are unsuccessful, drug treatment is prescribed.
Indications for surgical treatment are persistent pain, urinary tract obstruction, staghorn stones (even asymptomatic ones). In addition, such treatment is indicated for patients who cannot be allowed to develop renal colic (for example, pilots) or infection (patients who have undergone transplantation or endoprosthetics). Treatment planning and choice of method depend on the composition, location and size of the stone, kidney function and anatomical features of the urinary tract.
General information
Urolithiasis (UCD) is a common urological disease, manifested by the formation of stones in various parts of the urinary system, most often in the kidneys and bladder.
There is often a tendency to a severe relapsing course. Urolithiasis can occur at any age, but most often affects people 25-50 years old. In children and elderly patients with urolithiasis, bladder stones are more likely to form, while middle-aged and young people mainly suffer from stones in the kidneys and ureters. There has been an increase in the incidence of urolithiasis, which is believed to be associated with an increase in the influence of unfavorable environmental factors.
Urolithiasis disease
Laboratory research
The primary stage of research after examining the patient will be laboratory tests. Their results provide the doctor with information about the functional functioning of the kidneys and determine the presence of a pathological process. Laboratory methods are safe and highly accurate. The result can be obtained in a fairly short period of time.
Return to contents
General urine analysis
One of the first things patients suspect of renal pathology is a urine test. It does not require preliminary preparation or financial investment. Based on its results, you can immediately find out about a problem in the functioning of the kidneys. The patient must submit:
- morning urine analysis;
- 24-hour urine analysis.
The main indicator is red blood cells in the urine. An increased content of red blood cells accompanies not only urolithiasis. But the doctor, having studied the history of the disease, comparing it with the results of the analysis, can easily make a presumptive diagnosis. In addition to red blood cells, salt crystals, proteins, and bacteria are detected in the urine. If you have kidney stones, their number will be overestimated. Studying the chemical composition of salts will tell you about the type of stone.
Return to contents
Blood tests
More often, a general blood test in patients shows normal results, but it must be taken. During an exacerbation, an increase in leukocytes is observed. Their percentage shifts to the left and this indicates the development of the inflammatory process. In addition, pay attention to changes in ESR and the manifestation of anemia. Based on these indicators, we can conclude that renal function is impaired.
Return to contents
Factors that provoke the appearance of cholelithiasis
Stones (scientifically called concretions) in the bladder and bile ducts, as a rule, are formed as a result of a violation of the normal composition of bile, or more precisely, a change in the quantitative proportions of its constituent components.
The result of this disruption is the precipitation of solid components of this enzyme (the so-called biliary sludge), which over time increase in size and turn into stones. Often this pathology develops due to increased cholesterol content in bile (this bile is called lithogenic).
An increase in the concentration of cholesterol in bile can be caused by a number of negative factors:
- excessive consumption of cholesterol-rich foods;
- a decrease in the amount of bile acids in the bile resulting from dysfunction of hepatocyte cells (bile secretion decreases);
- reducing the concentration of phospholipids, which prevent the formation of sediments;
- violations of the bile outflow of bile, leading to stagnation of this liver secretion in the gallbladder;
- obesity (in women, this disease can be provoked by female hormones - estrogens, and frequent childbirth);
- surgical interventions (for example, removal of the lower lobe of the ileum, vagotomy, etc.);
- the presence of concomitant diseases (for example, diabetes mellitus, hemolytic anemia, liver cirrhosis, Crohn's disease, Caroli syndrome, and so on).
The causes of bile stagnation in this organ can be divided into mechanical and functional.
The first reason for the occurrence of a stagnant process is associated with the presence of some obstacle in the path of bile outflow (for example, during adhesions, swelling of the walls of the gallbladder, in cases of a tumor, kinking or narrowing of the bile duct, enlarged lymph nodes, and so on).
Functional disorders are associated with deterioration of bile duct motility (so-called dyskinesia). Also, the reasons that provoke stone formation in this organ can be infections or inflammations in the biliary system itself (liver + gallbladder), autoimmune diseases and various types of allergies.
The risk of gallstones increases with a sedentary lifestyle, during fasting to lose weight, during pregnancy, as well as with injuries, endocrine diseases, liver pathologies, and so on.
Chemical analysis of stones
An important point in examining patients is the chemical analysis of kidney stones. Using information about the composition of a kidney stone, one can trace the history of the development of the disease: metabolic disorders, the inflammatory process, and even changes in the chemical structure of medications in the tissues of the body. Chemical analysis can only be done in a special laboratory.
A kidney stone is a deposit that does not dissolve. More often, deposits form mineral salts: phosphates, oxalates, urates, cystine. Deposits can settle not only in the kidney, but also in any part of the urinary system. The size of the stone ranges from 1 mm to several centimeters. Oxalates and urates are perfectly tracked on x-rays.
The structure, contours of the stone and urinary tract, their shape can be tracked using survey urography.
Return to contents
Features and symptoms
Coral stone impairs the flow of urine from the kidney, which leads to dangerous consequences. For a long time, nephrolithiasis occurs latently or is accompanied by nonspecific symptoms - moderate lower back pain, deterioration of health, drowsiness. The symptomatic picture largely depends on the size of the stones, their shape and location.
Characteristic signs of coral nephrolithiasis include:
- hematuria (blood in urine);
- decreased urine formation;
- dull back pain;
- headache;
- chronic fatigue;
- moderate increase in temperature;
- cloudy urine;
- flatulence;
- insomnia.
The movement of coral stones in the kidneys leads to damage to the central joint, which causes hematuria.
Its severity depends on the degree of injury to the renal structures. Due to the deterioration of urine outflow, the pressure inside the kidney increases, which leads to colic. If the disease is complicated by renal failure, the following symptoms are added:
- anuria (lack of urine);
- feverish condition;
- decreased appetite;
- constant nausea.
The accumulation of metabolic products in the body leads to poisoning and a decrease in immune strength. Therefore, people with kidney stones complain of frequent exacerbations of chronic infections.
Instrumental diagnostics
X-ray diagnostic methods
Survey X-ray
Diagnosis of urolithiasis is based on the medical history, physiological disorders, and the passage of stones in the urine. Doctors obtain important information using X-ray examinations. Stones larger than 3 mm, consisting of oxalates, are visible on x-rays. Stones of other composition are difficult to identify; they do not transmit x-rays. There is no visible shadow from them in the survey photographs.
This is a routine examination of the kidney using x-rays. Contrast agents are not used. No preparation is needed to use an x-ray, so it is used in emergency situations. Sometimes the results are inaccurate, so it is recommended to perform a bowel cleanse before the examination.
Return to contents
Excretory urography
Diagnosis of kidney stones is carried out using plain radiography, with intravenous administration of a contrast agent. Once in the body, the contrast is released by the kidneys after some time, which makes it possible to clearly recognize stones, determine the presence of pathologies and check the functioning of the kidneys. This type of urography requires more than just bowel preparation. An analysis is required to determine allergic reactions to the contrast agent.
Return to contents
Retrograde pyelography
This method will show a clear image of the anatomical condition of the kidney and urinary tract. The method is carried out using a catheterization cytoscope. Through a catheter inserted into the kidney, contrast liquid is injected gradually, under low pressure. After contrast is administered and the catheter is removed, a picture is taken. Using the method, you can obtain a clear image of the renal pelvis and the entire length of the ureter.
Process description
The procedure is permitted only after the feasibility of the method has been established and contraindications have been taken into account. A study is being conducted in a hospital. The service is paid, but its price is not very high. The following drugs can be used for diagnosis: Urografin, Fortrans.
Preliminary activities
Preparation for kidney urography using a contrast agent involves donating blood for analysis. Biochemical indicators of biological fluid are required. The diagnostic results will help to exclude allergies, underlying and chronic diseases, and insufficient kidney function. You also need to meet the following requirements:
- Cleansing diet. A few days before the examination, all foods that increase gas formation in the intestines are excluded from the menu.
- Additionally, to cleanse the body, the patient takes activated carbon or another sorbent for 2-3 days.
- A person will need anti-anxiety medications if they feel anxious about the procedure or have an overstimulated nervous system.
- You can eat on the day of urography only in the morning, but the food should be easy to digest. The evening before you are allowed to take a laxative. In the morning you need to give an enema.
- If you have an allergic reaction, you must undergo a course of therapy with antihistamines.
- To avoid consequences in the form of receiving incorrect data, the radiologist recommends removing all metal objects.
Attention! You need to prepare for the procedure carefully, since the result of urography largely depends on this. You can find out how it is carried out from your doctor, he will give a complete description of the process.
Methodology
There is no need to be afraid of this procedure, since the administration of the medicine will not hurt. All activities last no more than 1.5 hours. It is carried out strictly according to the instructions and in a medical office. The patient is in a supine position, although in some cases he can stand.
Before the study, the patient must undergo a drug sensitivity test. The following tools are used in the specialist’s work: “Vizipak”, “Cardiotrust”, “Urografin”. The product in the ampoule must meet the following requirements: be harmless to the kidneys, not participate in metabolic processes. It is important that the drug cannot accumulate in body tissues. Also, a good medicine provides high-quality contrast. The doctor calculates the dosage, and he must do this as accurately as possible. It depends on the type of drug used, as well as on the body weight of the person being studied.
The introduction algorithm is simple. In the medical center, the patient must be positioned on a table. He shouldn't move. A puncture is made in the vessel, after which the medicine is gradually introduced into the venous bed. If this is done dropwise, then the amount of substance used should be doubled. When the product enters the body, a person may feel a slight burning sensation on the hand.
In the video you can see in detail how the diagnosis is carried out. After the procedure begins, the specialist takes two or three pictures within 10 minutes. If the patient is elderly, then the first photos can be obtained only after 13-14 minutes.
Upon completion of the study, the doctor is obliged to check the patient’s well-being. If everything is in order, then after a few hours he is sent home.
Performing the procedure in children
If it is necessary to perform urography in children, how such a diagnosis is made, the doctor must explain to the parents. It is allowed even for an infant, boy or girl. A child needs to prepare for it in the same way as an adult. For work, the specialist chooses gentle drugs. They are administered intramuscularly or parenterally (into the intestines). This will prevent rapid absorption of the contrast agent and the development of a chemical burn or phlebitis. Contraindications to the use of the procedure are the same as for adults.
Attention! You should not agree to urography if your baby has diathesis, liver damage or decompensated heart failure.
Modern equipment makes it possible to carry out diagnostics quickly and safely, even when the child is only a month old. If the baby is too active, then the manipulation can be performed under general anesthesia.
Differential diagnosis for identifying kidney stones
The diagnostic methods described above can determine the presence of any type of kidney stone without much difficulty. As a rule, urolithiasis does not need to be differentiated from other diseases. The only case when differential diagnosis may be necessary is acute renal colic. In this case, it is important to differentiate colic from an attack of appendicitis, cholecystitis, pancreatitis and even a perforated ulcer.
The basis for making a correct diagnosis is considered to be knowledge of the clinical symptoms of those pathologies with which renal colic is differentiated. Attention is focused on the location of pain, disturbances in urination, and changes in the physical characteristics of urine. There are pathologies of the pelvic organs and abdominal cavity, the symptoms of which are similar to the signs of urolithiasis. A thorough medical history and laboratory tests allow you to make the correct diagnosis and prescribe the correct treatment.
In the section on the question Small kidney stones. What are the effective diagnostic methods? asked by the author Andrey Semenchenko, the best answer is it is necessary to undergo tests, undergo an ultrasound and excretory urography - a contrast agent is injected into a vein, which is secreted by the kidneys, and a series of X-rays are taken. The method allows you to evaluate the entire anatomy of the genitourinary system and detect stones in all parts of the genitourinary system. However, there are so-called X-ray negative stones, which allow X-rays to pass through them and therefore are not visible on photographs. You need to find out which kidney stones are oxalates, phosphates or urates. Excess phosphate causes gout. If phosphates are found in the urine, you need to forget about dairy products and “press” on meat, fish and flour. Excess oxalates “saturate” the muscles and make them prone to spasms. Limit the consumption of greens, including sorrel, spinach, parsley, beets, tomatoes, radishes and carrots, beans, lentils, gooseberries, cranberries and red currants, strong tea, coffee and ascorbic acid. Drink herbal tea for a month, break for 2 weeks, and then repeat. Tea: 1 tbsp. l. Mix corn silk, bearberry leaves, hernia grass and knotweed. 1 tbsp. l. collection in 1 cup of boiling water, leave for 45 minutes. , strain, drink ¼ cup 4 r. per day, an hour after meals. If there is an excess of urates, avoid liver and other offal, meat broths and fried meat, as well as mushrooms, canned food, baked goods, chocolate, coffee, ice cream. There is such herbal tea “Saxifrage” (link...). When a person drinks it, the stones gradually dissolve, so getting rid of the stones is gentle and painless. Moreover, dissolution occurs faster if you drink tea while wearing the Information Matrix (link...). But the most important thing is that the Information Matrix gives excellent results in the presence of cysts; they resolve and simply disappear, and in a fairly short period of time. What methods of treatment at home can I also recommend, write
Kidney stones
The kidneys act as a filter for the blood , purifying it from waste products of the body, forming urine. In addition, the kidneys play the role of a regulator of electrolytes necessary for the functioning of the body. Urine, formed in the tubular system of the kidneys, passes through the entire urinary system, starting from the collecting system, then through the ureters to the bladder, which is the reservoir of urine. When the bladder is sufficiently full, the urge to urinate arises and urine passes out through the urethra.
In some people, crystalline chemicals in the urine precipitate, forming sand or kidney stones. At the initial stages, kidney stones are small in size, sometimes even smaller than a grain of sand, but gradually they can increase and occupy almost the entire renal pelvis (coral stones).
Urolithiasis is a concept that refers to the formation of stones in all parts of the urinary system, while nephrolithiasis refers to the development of kidney stones, and ureterolithiasis refers to stones in the ureters. It is not so much the size of the stone that matters, but its location, and whether it leads to obstruction and disruption of the outflow of urine.
If the stone is localized in the kidney, then it rarely leads to problems, however, if it migrates from the kidney to the ureter, then symptoms arise that prompt patients to consult a doctor. While the kidneys continue to function and produce urine, pressure increases above the obstruction, causing increased pressure in the collecting system. This pressure is what causes kidney stone pain. In addition, increased pelvicalyceal pressure helps push the stone along the ureter. If the stone passes into the bladder, then all symptoms of ureteral obstruction by the kidney stone are resolved.
Causes of kidney stones
There is no consensus on the cause of kidney stones.
Heredity. Some people are more susceptible to forming kidney stones, which suggests that heredity may play a role. Most kidney stones are made of calcium, and hypercalciuria (high levels of calcium in the urine) is a risk factor. A predisposition to high levels of calcium in the urine can be passed on from generation to generation. Some rare inherited diseases also predispose some people to form kidney stones. Examples of such diseases include people with renal tubular acidosis, people with disorders of the metabolism of various chemicals, which may include cystine (an amino acid), oxalates, (a type of crystal), uric acid (for gout).
Geographical position. Among the causes of kidney stones, geographic predisposition is distinguished. Where a person lives may predispose him or her to the formation of kidney stones. There are regions where the risk of stone formation is increased. Hot, dry climates combined with low fluid intake can leave people relatively dehydrated, causing urine to become concentrated and increasing the risk of kidney stones.
Diet. There is ambivalence regarding the effect of diet on the formation of kidney stones. If you are predisposed to stone formation, it is believed that a diet rich in calcium may increase the risk of stone formation. If there is no predisposition to stone formation, then the diet will probably not affect the development of kidney stones.
Some medications. Patients taking diuretics (or diuretics) and those who consume excess amounts of calcium-containing antacids may experience increased calcium levels in their urine, potentially increasing the risk of stone formation. Taking excess amounts of vitamins A and D also increases calcium levels in the urine. Patients with HIV who take the antiviral drug Indinavir (Crixivan) may develop indinavir-related kidney stones. Other commonly prescribed drugs associated with an increased risk of stone formation include the antibiotics ceftriaxone and ciprofloxacin.
Some diseases. Some chronic diseases associated with an increased risk of kidney stones include cystic fibrosis, renal tubular acidosis, and inflammatory bowel disease.
Symptoms of kidney stones
In the presence of obstruction of the ureters by a stone, a cramping (wavy) pain syndrome occurs as a result of attempts to remove the obstruction. This wave-like pattern of pain is called renal colic. The pain syndrome in renal colic differs in its cramping nature from the pain syndrome that accompanies diseases such as acute appendicitis, pancreatitis, cholecystitis. With these diseases, any movement of the body increases the pain, so the patient tries to lie in a forced position without changing body position (unlike renal colic, the patient cannot find a “place for himself”).
Renal colic is the occurrence of pain accompanying the passage of a stone through the ureter. The pain is intense and appears suddenly. The pain may wax and wane, but the nature of the pain, as a rule, is very pronounced and is caused by a spasmodic mechanism. Pain in renal colic is usually localized along the lateral surface of the abdomen or in the lumbar region on the affected side, radiating to the groin area. In men with renal colic, pain may be felt in the testicles or scrotum on the affected side. During renal colic, the patient cannot find a comfortable position, writhes in pain and even walks from corner to corner.
Renal colic is often accompanied by nausea, vomiting, and excessive sweating.
Hematuria (blood in the urine) may be visible (macroscopic) or invisible (microscopic). Blood in the urine appears as a result of stone irritation of the mucous membrane of the kidney or ureter. However, blood in the urine (hematuria) is not always a significant indicator of kidney stones. The presence of blood in the urine requires the exclusion of other pathologies of the urinary system, such as kidney or bladder infections, trauma, or a tumor process. Examining your urine under a microscope (urinalysis) can detect blood (the presence of red blood cells) even if there is no blood in the urine when viewed with the naked eye. Sometimes, if a kidney stone has caused a complete obstruction, blood may not be found in the urine because there is no flow of urine and therefore no blood.
Diagnosis of kidney stones
The classic presentation of renal colic, associated with blood in the urine, supports the diagnosis of kidney stones. Many other diseases can wear the mask of renal colic, and therefore the doctor will need a number of diagnostic methods to confirm the diagnosis. Particular attention should be paid in old age, since the picture of the disease can be erased due to a reduced pain sensitivity threshold. So, the doctor needs to rule out a rupture of an abdominal aortic aneurysm (an abnormal expansion of the main blood vessels that supply blood to the entire body from the heart), which is the cause of sharp and unbearable pain.
Clinical examination for kidney stones may reveal nothing other than painful (or tender) palpation of the lateral abdominal region or the costovertebral angle on the affected side. A physical examination is usually performed to rule out dangerous diseases. The doctor may palpate the abdomen and may detect a high-intensity pulsating area, which may indicate the presence of an abdominal aortic aneurysm. By auscultating (listening through a phonendoscope) the abdomen, the doctor may detect a noise made by abnormal blood flow in the dilated part of the abdominal aorta (aortic aneurysm). Pain on palpation in the right hypochondrium may indicate gallbladder disease. Soreness in the groin areas may be associated with acute appendicitis, diverticulitis, inflammation of the ovaries or appendages (in women). Examination of the scrotal organs will rule out or confirm the presence of testicular torsion.
Symptomatic relief of kidney stones is important, so symptomatic treatment may be offered, aimed at eliminating pain and nausea, even before a diagnosis is made.
A urinalysis for kidney stones can reveal the presence of blood in the urine (hematuria). In addition, a general urine test can reveal signs of infection of the genitourinary system (leukocyturia, bacteriuria), which can be a complication of kidney stones.
A general blood test for kidney stones is usually within standard values. But in the presence of complications of kidney stones, such as infection, a blood test may reveal leukocyturia, a shift in the leukocyte formula, and an increase in ESR (erythrocyte sedimentation rate).
Instrumental methods for studying kidney stones include kidney ultrasound, kidney CT, and plain radiography of the abdominal cavity.
All patients with kidney stones undergo a renal ultrasound. Kidney ultrasound is an effective method in diagnosing kidney stones. Ultrasound of the kidneys can reveal signs of hydronephrosis caused by a stone localized at the mouth of the renal pelvis.
In the case of X-ray negative (stones invisible on X-ray) stones of the genitourinary system (urate, cystine stones), the stones are clearly visualized by ultrasound of the kidneys.
Plain radiography of the abdominal cavity (also known as plain urography) can detect kidney stones, their location, size, and shape in some patients. In some rare cases, survey urography allows one to assess the dynamics of urolithiasis (stone growth, or, conversely, its passage) without the use of other diagnostic methods. Abdominal x-rays reveal x-ray-positive kidney stones (calcium-containing (calcium) stones), which make up 85 percent of all genitourinary stones. Urate, indinavir-induced and cystine kidney stones are not detected by X-ray (called X-ray negative), so additional diagnostic methods may be required. Thus, the presence of appropriate symptoms and no kidney stones detected on abdominal x-ray does not mean that there are no kidney stones.
Non-contrast-enhanced renal CT is the most sensitive method for diagnosing kidney stones. All X-ray positive and even X-ray negative (except for indinavir-induced) stones of the urinary system are well visualized on CT scan of the kidneys. CT clearly demonstrates the anatomy of the kidneys, ureters, bladder, visualizes the stone, helps in diagnosing its location, size, shape, and whether the stone leads to dilation of the ureter or inflammation of the kidneys. In addition, CT allows you to diagnose other pathologies and carry out differential diagnosis with acute renal colic (abdominal aneurysm, acute appendicitis, acute cholecystitis, pancreatitis and others). There are disadvantages of renal CT, which include the following: it is not used to assess individual renal functions; indinavir-induced stones are not visualized; relatively expensive research.
Treatment of kidney stones
Outpatient treatment of kidney stones
Preventing kidney stones is always preferable to treating kidney stones. Adequate hydration dilutes the urine (reducing its concentration), thereby preventing the formation of kidney stones.
Those patients who have never experienced renal colic cannot assess the severity of symptoms. Renal colic may be accompanied by nausea, vomiting, and the patient, as a rule, cannot cope with the symptoms on his own, so it is necessary to call an ambulance team.
With a confirmed diagnosis of kidney stones, the patient can monitor therapy on an outpatient basis (at home). Most kidney stones are capable of passing (if they are large enough to migrate), so treatment should be aimed at eliminating possible symptoms. Patients should take sufficient fluid (at least 2 liters). As for medications, the patient can take non-steroidal anti-inflammatory drugs (NSAIDs), which have anti-inflammatory and analgesic effects. It is also important to remember that it is important to consult a doctor before taking any drug.
You should tell your doctor if symptoms of kidney stones are accompanied by fever. This may indicate an infection, which may require emergency medical attention and may also require intervention in the form of kidney stone removal.
Drug treatment of kidney stones (renal colic)
Renal colic is a condition requiring emergency medical attention. In case of emergency medical care, intravenous drip administration of the drug diluted in physical solution is used. Painkillers, antispasmodics, NSAIDs, and antiemetics can be used as the main drug. Physic solution in sufficient quantity is used as hydration.
If, during therapy, pain persists (uncontrollable, untreatable), nausea, and persistent vomiting, then this patient with a kidney stone requires hospital treatment. The patient also needs hospitalization if the kidney stone is complicated by infection.
At the outpatient stage, to relieve possible symptoms of kidney stones, the doctor may recommend painkillers, NSAIDs as an anti-inflammatory treatment, antiemetics in the form of tablets or suppositories. In some cases, patients may be prescribed tamsulosin (a drug used for prostate cancer), which can help the stone pass from the ureter into the bladder.
Some kidney stones, due to their size and location, are not able to migrate; their removal requires the help of a doctor. If the stone is localized in the upper third of the ureter, near the kidney, and is large, then the doctor may need external shock wave lithotripsy, in which a shock wave is focused on the stone, and energy sent through the tissue into the stone causes it to oscillate asynchronously, which ultimately leads to fragmentation (division into small parts). As a result, small fragments are passed out in the urine. This method has many advantages over invasive surgery, the main one being that stones are crushed remotely (at a distance) under the influence of waves of a certain intensity.
If there are contraindications to external shock wave lithotripsy (size more than 2 cm, localization of the stone in the lower segment of the kidney, excess weight of the patient), ureteroscopy is performed, through which contact ureterolithotripsy is performed. The urologist passes a ureteroscope (a thin metal tube with a camera, a light guide and an additional working lumen) through the urethra, bladder and into the ureter to the stone, then, if the size of the stone allows it to be removed with forceps, then the stone is captured and removed. If the stone is large, ureterolithotripsy is performed. After removing stone fragments, a stent (hollow tube) is installed in the ureter for some time, ensuring normal outflow of urine and also improving the passage of microscopic stone fragments.
Complications of kidney stones
Since most patients have two kidneys, temporary obstruction of one kidney due to a migrated kidney stone does not lead to significant changes. If the patient has a single kidney, then obstruction by a stone may require emergency medical attention. If a kidney remains obstructed for a long period of time, it may stop functioning.
The addition of infection to kidney stone obstruction is another emergency situation. When urine is infected and does not drain, the infection can spread throughout the body (sepsis). Fever (increased body temperature) is a significant symptom of this complication. A urine test can reveal the presence of infection, and the doctor will insert a stent or remove the obstruction using a ureteroscope as an emergency measure.
Treatment results and observation for urolithiasis
During the treatment of urolithiasis (kidney stones), the patient may feel the passage of a stone or its fragment through the ureter and its exit with a stream of urine. Sometimes the doctor may recommend monitoring this moment in order to subsequently remove the stone and study its composition in the laboratory. But the stone can be so small that it simply cannot be seen. In most cases, stones have a calcium composition, but there are kidney stones of a different nature. The feasibility of clarifying the nature of kidney stones is necessary to prevent further stone formation by prescribing drugs for prophylactic purposes.
The doctor, having prescribed treatment aimed at eliminating kidney stones, also recommends drinking plenty of fluids (at least 2 liters of fluid), which facilitates the passage of fragments of kidney stones with urine flowing out.
It must be remembered that if pain syndrome characteristic of renal colic, nausea, vomiting, or fever appears, you should immediately consult a doctor or call an ambulance.
Prevention of kidney stones
Currently, the formation of kidney stones and renal colic probably cannot be prevented, but the risk of developing urolithiasis can be minimized by avoiding dehydration. Hydration (drinking enough fluids) helps dilute the urine, reducing its concentration, thereby minimizing the risk of kidney stones.
Nowadays, there are drugs for the treatment of urolithiasis for various types of stones. Compliance in taking medications (compliance with the regimen, duration of treatment, adherence to doctor’s recommendations) can reduce the risk of kidney stones and prevent episodes of renal colic.
Prognosis for kidney stones
The prognosis for kidney stones is favorable, especially if you follow all the recommendations of your doctor. But it must be remembered that if urolithiasis has been diagnosed (and the stone has been removed surgically or passed away on its own), then the likelihood of the formation of another stone exists. Since the hereditary factor plays a role in the etiology of urolithiasis, there is a possibility of developing kidney stones in subsequent generations.
SIGN UP FOR A CONSULTATION by phone +7 (812) 951 - 7 - 951
Share link:
Classification
The most common types of kidney stones are mixed. But even in this case, some mineral predominates in the structure of the stone. Based on their chemical composition, the following types of stones are distinguished:
- oxalate (oxalic acid salts);
- urates (salts of uric acid);
- phosphate (salts of phosphoric acid);
- carbonate (salts of carbonic acid);
- protein (a mixture of several amino acids);
- cystine (compound of the amino acid cystine);
- cholesterol
These are the most common types of kidney stones. However, there are also rare types of stones:
- xanthine (xanthine – ammonium urate);
- struvite (a mixture of calcium and magnesium ammonium salts).
Xanthines in the urine appear due to genetic defects in enzyme metabolism, which happens very rarely. Struvite occurs against the background of infection with the active participation of bacteria producing a special enzyme in stone formation.
Depending on the size of the stones, the following types are possible:
- microliths with a size of up to 10 mm;
- macrolites with a size of more than 1 cm;
- coral-shaped stone more than 15 cm.
The size plays a significant role in the choice of treatment. You can try to remove microlites in the kidneys at home; when identifying macrolites, it is better not to use traditional medicine methods. In addition to size, other factors must be taken into account. Depending on the type of kidney stones, further treatment tactics are determined.
Prevention
In 87% of cases, the course of coral nephrolithiasis is favorable. When the stones are removed, kidney function is completely restored. To avoid relapses, be sure to eat right and treat endocrine diseases in a timely manner. To prevent recurrent stone formation, you should:
- control body weight;
- to live an active lifestyle;
- give up alcohol;
- drink up to 3 liters of fluid per day;
- stop relapses of urological diseases.
By following a diet, the likelihood of developing kidney stones is reduced by 45-50%.
Patients with a predisposition to nephrolithiasis are recommended to be examined by a nephrologist at least 1-2 times a year. Timely diagnosis and therapy eliminates the need for surgery and kidney removal.
Reasons for education
Congenital or acquired metabolic problems that provoke disturbances in mineral metabolism include the following conditions:
- diseases of purine metabolism, in which there is an accumulation of urates in the urine (uraturia);
- endocrine diseases that contribute to impaired metabolism of calcium, magnesium, phosphorus and their excretion of calcium salts through the kidneys (oxaluria, phosphaturia);
- disorders of carbohydrate and protein metabolism with increased release of amino acids into the urine (aminoaciduria, cystinuria);
- pathology of lipid metabolism with increased cholesterol in the blood and urine.
Infection and accompanying chronic inflammation play a significant role in urolithiasis. Bacteria can become a framework or basis for a future calculus. Or infection may play a major role in the formation of a stone with a characteristic chemical composition.
Causes
Currently, the causes and mechanism of development of urolithiasis have not yet been fully studied. Modern urology has many theories that explain the individual stages of stone formation, but so far it has not been possible to combine these theories and fill in the missing gaps in a single picture of the development of urolithiasis. There are three groups of predisposing factors that increase the risk of developing urolithiasis.
- External factors. The likelihood of developing urolithiasis increases if a person leads a sedentary lifestyle, which leads to disruption of phosphorus-calcium metabolism. The occurrence of urolithiasis can be triggered by dietary habits (excess protein, sour and spicy foods that increase the acidity of urine), water properties (water with a high content of calcium salts), lack of B vitamins and vitamin A, harmful working conditions, taking a number of drugs (large quantities ascorbic acid, sulfonamides).
- Local internal factors. Urolithiasis most often occurs in the presence of abnormalities in the development of the urinary system (single kidney, narrowing of the urinary tract, horseshoe kidney), inflammatory diseases of the urinary tract.
- General internal factors. The risk of urolithiasis increases with chronic gastrointestinal diseases, prolonged immobility due to illness or injury, dehydration due to poisoning and infectious diseases, metabolic disorders due to a deficiency of certain enzymes.
Men are more likely to suffer from urolithiasis, but women more often develop severe forms of urolithiasis with the formation of staghorn stones, which can occupy the entire kidney cavity.