The article discusses the procalcitonin test, the interpretation of which allows for early diagnosis of severe bacterial infection or sepsis. Procalcitonin is directly involved in the formation of the systemic inflammatory response of the human body to infection. The method is classified as express diagnostics with high diagnostic value. Since the value of the indicator increases at the early stage of infection, when other proteins are still within acceptable values.
Procalcitonin test – what is it?
Procalcitonin is a precursor to the hormone calcitonin, which is necessary to maintain calcium metabolism in the human body. The prohormone is secreted by the thyroid gland and is represented by 116 amino acids. In a healthy person, the amount of procalcitonin in the blood is extremely small; the prohormone is found in trace amounts in the test material.
The procalcitonin test is prescribed for the following diseases:
- sepsis and septic shock;
- severe forms of infectious and purulent processes;
- puerperal fevers;
- acute pancreatitis (for differential diagnosis between sterile and infected inflammatory processes);
- generalized bacterial infections in an adult or newborn;
- secondary bacterial infection due to viral infections or autoimmune pathologies.
The study is of particular value after complex surgical interventions after extensive injuries and fractures, 3rd - 4th degree burns and in cardiovascular pathologies. It allows you to exclude the fact of bacterial infection or diagnose it in time and select the appropriate treatment. Repeated testing is recommended when monitoring the effectiveness of selected antibiotics to treat bacterial infections.
Features of the procalcitonin test
It has been noted that pathogens stimulate the production of procalcitonin in the human body. Procalcitonin production begins to increase in the first 2 to 4 hours after bacterial infection. This indicator reaches its peak values 12 hours after infection. Its half-life varies from 20 to 26 hours.
Important: during a viral infection, the value of procalcitonin does not increase. Therefore, it is not performed if a viral infection is suspected.
The advantage of the test is that the value of procalcitonin during a bacterial infection changes much faster than other proteins. Symptoms of inflammation and extensive bacterial infection:
- a decrease in body temperature by less than 36°C or an increase to 38°C or more degrees;
- pulse of 90 beats per minute or more;
- a sharp increase in the number of leukocytes in the blood and the level of ESR;
- The patient's breathing rate increases to 20 times per minute or more.
There was a direct correlation between the degree of increase in the indicator and the severity of the patient’s condition.
Pericardial calcification
In constrictive pericarditis, a thick, calcified lining replaces the normal lining around the heart, or pericardium. This leads to the fact that the lower chambers of the heart begin to fill with blood worse.
Symptoms
Symptoms of pericardial calcification resemble those of heart failure. They usually begin to appear when constrictive pericarditis develops.
These symptoms include the following:
- fatigue;
- shortness of breath during exercise;
- shortness of breath when lying down;
- shortness of breath when bending forward.
It is also important to note that pericardial calcification may not cause symptoms at all.
Causes
One of the main causes of pericardial calcification is pericarditis. Pericarditis in medical practice is called inflammation of the pericardium, which quite often develops for unknown reasons.
Major heart surgery can provoke the development of constrictive pericarditis, and sometimes this condition develops as a result of viral infections in the pericardium.
Other causes of pericardial calcification include the following:
- injuries;
- radiation (radiation) therapy;
- connective tissue diseases;
- malignant formations.
Treatment
If there are no symptoms of pericardial calcification, no treatment is required.
Some patients with pericardial calcification also have underlying inflammation. In such cases, anti-inflammatory drugs such as colchicine, as well as corticosteroids and non-steroidal anti-inflammatory drugs (NSAIDs), can help.
For some patients with pericardial calcification, doctors offer a surgical procedure called pericardiectomy, which involves removing part of the pericardium.
Preparing for analysis
To obtain the most reliable laboratory test results, you should follow the basic rules of preanalytical preparation. Before visiting the laboratory, adult patients must abstain from food for at least 8 hours and from alcoholic beverages for 1 day. Infants under 1 year of age should not be fed for 30-40 minutes before taking biomaterial. Children from 1 to 5 years old are recommended to refrain from eating for 2-3 hours.
It is important to drink plenty of clean and still water. This rule is of particular importance for young patients. Because the venipuncture procedure is extremely unpleasant for them. Drinking plenty of fluid will make it easier to collect venous blood. If the child is not given water to drink before the test, the blood will flow into the test tube drop by drop. This will significantly increase the time of venipuncture and increase the risk of hemolysis of red blood cells. Carrying out research with biomaterial with destroyed red blood cells is impossible and requires mandatory re-sampling of blood.
You should limit any type of stress before the test. Children should be calmed and distracted as much as possible. It is not recommended to take venous blood from crying children, as this may lead to unreliable test results. Adult patients need to sit quietly in the laboratory department for 15-20 minutes before venipuncture.
The minimum interval between smoking and blood collection should be 30 minutes, optimal – 3 hours.
How to donate urine
To measure calcium in the blood, there are two types of tests. The total Ca assay calculates both the free and bound forms. The ionized calcium test measures only the free form of this substance. To measure it, the doctor prescribes a biochemical test of blood and urine.
A blood test is taken from a vein. If a urine calcium test is done, a 24-hour collection is examined, although urine collected over a different, shorter period may also be examined.
Studying urine collected during the day is more preferable than analyzing urine collected at one time, due to the fact that all processes in the body occur cyclically. This means that at one time the substance is excreted by the kidneys in larger quantities, at other times in smaller quantities. Daily collection allows you to identify the average value, which will allow the attending physician to perform a more accurate analysis.
To collect urine in 24 hours, you need to do the following. After waking up in the morning, empty your bladder into the toilet. This urine is not used for analysis. In this case, you need to note the time. Over the next 24 hours, drain all urine into a prepared container. When 24 hours have passed, you need to wait for the next urination and empty your bladder into a container. This is the last portion of urine. After this, the container with the 24-hour urine sample should be delivered to the laboratory or placed in the refrigerator for storage if immediate delivery is not possible.
Interpretation of the procalcitonin test
The norm of the procalcitonin test for children and adults is identical, it is 0 – 0.064 ng/ml. Deviations from the norm to a greater extent are a sign of the development of bacterial inflammation.
It is not advisable to try to decipher laboratory test results on your own. When interpreting the procalcitonin test, the doctor takes into account the clinical picture of the pathology, the addition of secondary infections and concomitant diseases. No less significant is the antibacterial therapy used, its duration and types of antibiotics.
In newborn babies, the level of prohormone is increased. Peak values are observed at 24–36 hours of life. What the specialist must take into account when interpreting. The laboratory criterion reaches normal values on days 4–5, when repeated testing is carried out if necessary.
It should be emphasized that the value of the indicator is influenced by some medications. Medicines that suppress the immune system temporarily increase the level of prohormone in the blood. Therefore, if the patient is taking medications, they should be reported to the laboratory department employee.
When is a test ordered?
Your doctor will order blood and urine calcium tests as part of your general physical examination. In many patients, symptoms of its increased or decreased levels in the blood do not appear until they reach impressive levels.
A low Ca level is indicated by cramps in the abdomen, muscle spasms, and tingling sensations in the fingers. If it increases, the following symptoms appear:
- Fatigue.
- Feeling weak.
- Loss of appetite.
- Nausea.
- Vomit.
- Constipation.
- Stomach ache.
- Frequent urge to urinate.
- Intense thirst.
The attending physician can give the patient a referral for calcium tests if he has symptoms of diseases of the parathyroid glands, thyroid gland, food is not absorbed or digested, or the patient is not eating well. It is necessary to monitor the level of the mineral during treatment of diseases associated with calcium imbalance to assess the effectiveness of treatment. This also applies to patients who take Ca or vitamin D supplements.
It is necessary to regularly take a calcium test if you have kidney disease (often low, especially with kidney failure) or after an organ transplant. Analysis is prescribed for diseases of the skeletal system and neurological diseases.
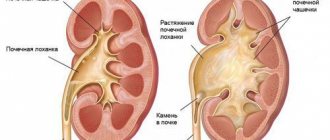
Ca tests are prescribed to confirm the diagnosis of urolithiasis. In this case, the patient experiences symptoms such as sharp pain in the back or side in the kidney area, which can progress to the lower abdomen. Blood may appear in urine due to urolithiasis (hematuria). Monitoring the amount of calcium should be carried out if the patient has breast, lung, head, or neck cancer. Testing is also prescribed for kidney cancer and multiple myeloma.
Sepsis is the cause of increased procalcitonin
Sepsis is a systemic inflammatory reaction of the human body in response to an infectious infection. From a medical point of view, this condition is considered severe. It is accompanied by the penetration of pathogenic microorganisms into the blood, which should normally be sterile. It should be emphasized that the inflammatory process in sepsis is localized throughout the body, and not in individual organs.
A special case is neonatal sepsis, when newborn children are infected. Signs of sepsis in children:
- the child refuses to breastfeed;
- there is a high fever;
- bloating;
- restlessness, moodiness, or sudden drowsiness;
- vomiting and diarrhea;
- blood may appear in the stool (with infectious enterocolitis);
- sudden weight loss;
- changes in the color and elasticity of the skin;
- formation of suppuration in the umbilical cord area.
Neonatal sepsis occurs in the presence of infectious diseases in the mother, infection of the amnion and during childbirth in non-sterile conditions, infection with a staphylococcal infection in the first weeks of life, etc.
Treatment of sepsis should be carried out immediately in a clinic setting. Effective antibacterial drugs are selected for patients, procedures are carried out to detoxify the body from bacterial toxins and replenish fluid losses.
A decrease in procalcitonin levels indicates the effectiveness of the chosen treatment methods.
Changes in the properties of urine and the appearance of flaky discharge in it
Have you been trying to cure your KIDNEYS for many years?
Head of the Institute of Nephrology: “You will be amazed at how easy it is to heal your kidneys just by taking it every day...
Read more "
A sign of human health is clear urine, its homogeneous structure and the absence of white discharge. If the internal organs function normally, then there should be no foreign formations in the waste product of the body. In women during the menstrual cycle, the presence of blood in the urine is considered a completely natural phenomenon, and tests are not performed at this time.
Representatives of both sexes need to know: if white flakes suddenly appear in the urine, this is a reason to sound the alarm, because such formations may indicate impaired metabolism, excess protein, and the presence of inflammatory processes in the body.
Changes in diet. Infection
Only a doctor can answer the question of why the color, structure, and density of urine changes after a thorough diagnosis of the patient. The most harmless option is a sudden change in your daily diet. White flakes can be observed in those who suddenly switched to a vegetarian diet or sharply increased the amount of protein foods. A similar phenomenon is often found among children whom adults, with good intentions, feed with high-calorie, heavy protein foods, which the child’s body simply cannot cope with; as a result, proteins are not absorbed.
Any sudden change in regime, diet, or amount of food is stressful for the body. It often turns out to be unable to efficiently process unusual products. Precipitates form from the remains of unprocessed substances, and they settle in flakes in the liquid. This phenomenon usually does not last long, however, you need to contact medical specialists, and first of all, a gastroenterologist.
The protein gives the flakes a white tint. Its excess in waste products, including urine, clearly signals: inflammatory processes are underway in the body. It is the increased amount of protein that indicates that a person has
- cystitis,
- urethritis,
- pyelonephritis.
Urethritis is similar in symptoms to cystitis and pyelonephritis: during the listed ailments, urine is characterized by white discharge present in it.
These pathologies in men and women can occur simultaneously or act as a provoking factor in relation to other infectious diseases. In such cases, sediment in the urine is present in the form of white flakes and admixtures of pus, and when urinating, the person experiences
- discomfort,
- pain and
- burning.
The listed symptoms in women are usually accompanied by pain in the vaginal area; Urethritis in the fairer sex develops more dynamically. This is due to the fact that the female genital organs are closer to the urethra, and the ureters are wider than those of men.
Violation of water-salt metabolism. Pregnancy
White flakes may indicate impaired water-salt metabolism or the onset of diabetes. In the first case, they often appear in children who do not receive the required amount of fluid (most often in the hot season). And again, there is a nuance here: when there is an excess of salty and fatty foods in a child’s diet, the structure of the urine fluid is also disrupted, it becomes cloudy, darker in color and has a sharp, unusual smell. Precipitates form in it, because the liquid contains substances that have not been processed by internal organs, including the kidneys.
However, parents should not lose their vigilance in the summer, remembering that the symptoms of impaired water-salt metabolism and pyelonephritis are similar. These include
- white sediments in urine,
- increased body temperature,
- headache,
- vomiting
- gastrointestinal disorder.
When a child’s urine changes its usual characteristics, you should immediately consult a doctor. Acute forms of pyelonephritis quickly enough, in the absence of proper treatment, pass into the chronic stage, causing severe complications in the functioning of internal organs.
In pregnant women, flakes in the urine are considered either normal or pathological. Forming in the vagina and getting into the urine from there, they can be a sign of increased protein in the body, but they can also act as a manifestation of gynecological inflammatory diseases. In this case, the expectant mother is prescribed additional tests that will help identify the cause of changes in the urine.
When a person’s immunity decreases, urine is one of the first to signal this. It may also indicate the onset of diabetes. However, if this disease occurs against the background of urethritis, cystitis, or pyelonephritis, this symptom will confirm the presence of abnormalities in the endocrine system, as well as a decrease in the body’s resistance to infectious diseases.
Formation of flakes in urine in men
Pyelonephritis and cystitis are considered to be “female” diseases, because in men they are less common, occur much more easily and with fewer complications. Representatives of the stronger sex, like women, also experience the formation of flakes in their urine. This phenomenon, first of all, indicates problems with the prostate gland, whose functioning is instantly disrupted under the influence of any inflammatory processes.
The urine becomes cloudy due to an increased number of white blood cells. If the functioning of the urinary tract is impaired due to the appearance of sand and stones in it, blood clots will also be present in the urine. In the latter case, it acquires a brownish-reddish tint. Changes in it are accompanied by pain symptoms not only when urinating, but also during physical activity or being at rest.
If these pathologies develop against the background of urethritis, not only white sediments appear in the fluid, but also purulent discharge.
As for the latter, their shape and size often depend on the nature and extent of damage to the internal organs. If the urethra is inflamed, an increased number of leukocytes is observed, the discharge can become thread-like in nature, settle and, at the initial stage of the disease, make the liquid turbid. In any of the inflammatory diseases, the urine has a sharp, putrid odor that is not typical for it. In diabetes mellitus, its smell resembles a flower.
White flakes can indicate the presence of malignant tumors in the genitourinary system. Prostate adenoma may not make itself felt with pronounced symptoms at first, and only darkened urine that has changed its structure will help identify it. Kidney injuries in women and men are accompanied by similar changes in urine. White flakes may indicate the beginning of decomposition of kidney tissue - renal fatty degeneration. If your urine characteristics change, you should immediately contact medical specialists and under no circumstances self-medicate.
Other reasons for the increase
If sepsis is excluded, the patient must undergo additional diagnostics and establish the cause of the increase in prohormone in the blood. Possible reasons for changes in the value of the laboratory indicator under consideration include:
- pneumonia;
- bronchitis;
- meningitis;
- peritonitis;
- pancreatitis.
With fungal and parasitic infestations, a procalcitonin test may show positive results with a high level of prohormone. To establish a diagnosis, the patient is additionally prescribed: a clinical blood test with a leukocyte formula, a general urine test and a test for the level of C-reactive protein.
Why does the body need calcium?
Calcium (Ca) is essential for the human body. Thanks to it, muscles, nerves and heart function correctly, blood clots normally, bones are formed, compacted and maintained healthy.
99% of calcium is found in bone tissue, while the remainder circulates in the blood. Its quantity is strictly controlled by the body. If there is not enough Ca in the body (insufficient intake from food, increased excretion in urine or feces), the element is extracted from bone tissue to maintain its normal level in the blood.
Half of the calcium that circulates in the blood is contained in “free” form, that is, it takes part in metabolic processes. The remaining half is reserved for participation in reactions with protein albumin and anions, which also include phosphates, and does not take part in metabolism.
The body loses some Ca every day: it is filtered in the kidneys and excreted in the urine. Measuring the amount of calcium in the urine helps determine the amount of the mineral being filtered out by the kidneys. This allows you to make a diagnosis or monitor the patient's condition.
Reduced level
The most common cause of low calcium is a low level of protein in the blood, primarily albumin. This may be the result of liver disease or malnutrition, which may occur due to alcoholism or other diseases. Reduced albumin levels are common in patients with acute illness. But it must be borne in mind that with a reduced number of proteins, only bound calcium decreases, while the free form remains normal, and Ca exchange proceeds normally.
Urinalysis for phosphorus
Phosphorus is one of the most important microelements. It is part of cell membrane proteins, high-energy molecules, bone matrix, nucleic acids and other compounds. Phosphorus levels in the body are regulated through a complex interaction between vitamin D and parathyroid hormone. Some diseases are accompanied by leaching of phosphates. To determine the degree of loss, a urine test for phosphorus is prescribed.
The study is recommended for:
- diseases of the kidneys, skeletal system, thyroid glands,
- long-term immobilization after fractures,
- Fanconi syndrome,
- rickets in children
- familial hypophosphatemia,
- non-renal acidosis,
- treatment with vitamin D,
- predisposition to the formation of urinary stones,
- acromegaly,
- tuberculosis and other infectious diseases,
- hypo- and hyperparathyroidism,
- suspected metastatic bone lesions.
A urine test for phosphorus as part of a biochemical study is prescribed to exclude or confirm the presence of pathologies of the endocrine, bone and urinary systems of the body.
Reasons for the appearance of phosphate salts
There are several factors for phosphate getting into the urine in adults and children:
- incorrect lifestyle and diet (vegetarian menu, some diets);
- abuse of foods high in phosphorus (dairy products, seafood, whole grain cereals, mineral water);
- metabolic disease;
- lack of fat-soluble vitamins;
- pregnancy (changes in hormonal levels and taste preferences);
- dehydration due to vomiting and diarrhea;
- poisoning with chemicals containing phosphorus.
Amorphous phosphates in the urine of a child under 5 years of age usually indicate immaturity of the digestive system and mechanisms for regulating metabolic processes.
Phosphates and other salts in urine can be a sign of various diseases:
- genetic disorder - phosphate diabetes;
- Fanconi disease;
- urolithiasis (stones in different parts of the urinary system);
- chronic kidney failure;
- renal tubular acidosis or congenital anomaly;
- hyperfunction of the thyroid and parathyroid glands.
Often the amount of phosphates in the urine increases with inflammatory and infectious diseases of the genitourinary system:
- cystitis;
- pyelonephritis;
- urethritis;
- prostatitis.
Free Form CA Study
A total calcium test is the most commonly performed test when it is necessary to check the content of this element in the body. In most cases, the analysis fairly accurately reflects the presence of free calcium in the blood, since the ratio between free and bound forms in the body has clearly established proportions. If tests reveal that there is increased calcium in the urine, this is considered a signal of a health problem. Additional tests are performed to find the cause.
Sometimes it is necessary to test for ionized Ca. This test is used for critically ill patients who have received a blood transfusion or are receiving intravenous nutrition.
Patients who have undergone major operations, as well as patients with low levels of protein (albumin) in the blood, need analysis. An ionized calcium test is also prescribed if patients experience numbness in the tissues around the mouth, in the feet, hands, and muscle spasms in these areas.
Strong fluctuations in ionized calcium can cause slow heartbeats, spasms and titanic muscle convulsions, provoke loss of consciousness and even coma. In critically ill patients, it may be very important to monitor the condition using calcium ion tests. This is necessary to prevent complications and increases the chances of treatment success.
The total test measures both free and bound calcium. But because bound Ca is highly dependent on blood protein levels, total level results can be skewed if protein levels are abnormal. Therefore, when protein levels are abnormal, more accurate methods of measuring free calcium through ion testing must be used.
If Ca deviates from the norm, an analysis is often prescribed for parathyroid hormones and vitamin D, which are responsible for maintaining calcium in the blood at the required level, so their deviation indicates a developing problem. Testing for urine calcium and phosphorus and/or magnesium will help determine if other abnormalities exist. Measuring the balance between these substances is just as important as changes in the concentration of these elements in the blood.
How to test urine for phosphorus?
To obtain reliable test results, it is important to test urine for phosphorus in accordance with all rules. When preparing, follow these guidelines:
- in consultation with your doctor, temporarily stop taking diuretics, glucocorticoids, parathyroid hormone, asparagine, vitamin D, antacids;
- do not undergo examination immediately after cystoscopy and during menstruation;
- Avoid alcohol and carbohydrate-rich foods per day.
Since the removal of phosphorus from the body occurs unevenly, the morning urine sample is not suitable for analysis. The study requires 24-hour urine. To do this, the first portion is poured out, after which the urine is collected within 24 hours in a large, clean container. Then the contents are mixed, 50 milliliters are poured into a sterile plastic container and delivered to the laboratory. Do not forget to indicate the volume of biomaterial per day.
The results must be interpreted by a doctor. An increased content of phosphorus in daily urine is often observed with:
- prolonged immobility - for example, after fractures or surgical treatment,
- rickets in young children,
- damage to the renal tubules,
- predisposition to nephrolithiasis,
- leukemia.
Hypophosphaturia occurs with prolonged fasting, tuberculosis, enterocolitis, hypothyroidism, and acute infectious diseases.
You can always take urine tests for phosphorus at INTELmed Solntsevo. Based on the results of laboratory tests, the specialist will clarify the diagnosis and draw up a treatment plan. Contact us - we will help!
Norm
The concentration of phosphorus in urine varies with age. The lowest value is in infants, and this is understandable, since they have neither teeth nor a well-developed, ossified skeleton, which contains a large amount of hydroxyapatite. That's why:
- in children under one year old, the limit of phosphates in daily urine should not exceed 15 mmol;
- in a four-year-old child – no more than 25 mmol;
- from 4 to 7 years of age, this limit is 30 mmol per day;
- in adolescents under 14 years of age - no more than 40 millimoles per day;
- a person over 14 years of age, and into old age, usually has a constant concentration of phosphates in the urine, which does not go beyond 13 to 42 mmol in daily urine.
General symptoms of phosphaturia
The following signs are taken into account:
- the urine is turbid, small flakes appear that easily precipitate;
- a person may experience pain in the abdomen, frequent urge to visit the toilet;
- in the lumbar region, unilateral pain, a feeling of heaviness, which often occurs during physical activity;
- flatulence increases;
- nausea and vomiting, intestinal colic are likely;
- blood pressure jumps.
But the listed signs are characteristic of an advanced state. In the initial stage, phosphaturia practically does not cause symptoms. And an overestimated concentration of chemical compounds can only be determined during an examination for another reason.