Renal failure is a syndrome of disturbances in the functional activity of an organ, as a result of which water, electrolyte, nitrogen and other types of metabolism suffer. The only method of saving human life in this pathology is kidney replacement therapy.
Renal replacement therapy includes a series of medical procedures, carried out in a complex manner, used to fully support the lost functions of the organ as a result of incurable pathologies.
Hemodialysis
The essence of the procedure is to purify the blood using medical equipment called an “artificial kidney”. Using the method, the necessary results are achieved:
- Toxins are removed from the blood.
- Urea is removed.
- Electrolyte balance is stabilized.
- Blood pressure is normalized.
- The acid-base balance is restored.
The procedures are carried out on an outpatient basis; a three-time weekly procedure in a medical center, which requires 4 hours, provides the patient with satisfactory well-being, a familiar lifestyle, and the opportunity to work.
Hemodialysis is carried out according to a specific scheme (at home and in a hospital)
Blood hemodialysis can also be performed at home. You need to purchase an “artificial kidney” device and learn how to use it, having mastered the operating rules. The high price of the device does not allow large-scale blood purification at home.
Peritoneal dialysis
An alternative to hemodialysis is peritoneal dialysis, the essence of which is as follows:
- A catheter is inserted into the abdominal wall.
- Every 6 hours, dialysate in a volume of 2 liters is poured through a catheter.
- When the dialysate administration is completed, the catheter is closed, which allows the patient to continue with his usual activities for 6 hours.
- After 6 hours, the fluid is drained and a new portion of dialysate is poured into the abdominal cavity.
Advantages and disadvantages of the method
Peritoneal dialysis has some significant advantages over hemodialysis. Peritoneal dialysis does not have to be performed in a hospital setting; fluid is excreted very slowly. Cardiac stress is significantly reduced and heparin is not required.
Artificial kidney - what is it?
The disadvantages of peritoneal dialysis are: low overall efficiency, the risk of protein loss, the impossibility of predicting the degree of removal of dissolved substances, and the risk of developing peritonitis.
The list also includes the manifestation of ventilation disorders as a result of decreased diaphragmatic mobility and jumps in blood glucose levels.
Improvement of the peritoneal dialysis method, including the use of flexible catheters, and the ability to choose different types of solution give a chance to become competitive among other types of RRT.
Renal replacement therapy: indications, types and methods, drugs and devices
If kidney function is impaired, doctors prescribe renal replacement therapy to patients. There are clearly defined indications for such a prescription and they may relate not only to urological diseases.
Renal replacement therapy - what is it?
Renal replacement therapy is a complex of treatment measures that implies full support of kidney functionality in case of irreversible pathological processes.
This set of measures involves placing the patient in a medical institution, but usually the length of his stay in the hospital does not differ in length.
Those patients who are indicated for continuous renal replacement therapy periodically visit clinics (according to the schedule established by the attending physician) and receive the necessary treatment.
Indications for use
The type of therapy under consideration is prescribed in the case of diagnosing irreversible pathological changes in the kidneys that have led to their dysfunction.
Indications for use in this case are:
- acute renal failure occurring in a severe stage;
- chronic renal failure;
- surgical removal of one or two kidneys;
- disruption of the functionality of one kidney - only if the remaining kidney cannot cope with its work.
An absolute indication for renal replacement therapy is uremia, a condition characterized by poisoning by protein metabolism products, which is always associated with impaired renal function.
If uremia occurs at an early stage, then doctors try to restore the patient’s health with drug therapy, but in the case of seizures, coagulopathy, encephalopathy and pericarditis (complications against the background of rapidly progressing uremia), there is no doubt that only renal replacement therapy can save the patient’s life.
Another kidney disease, which in a certain case involves the therapy in question, is azotemia. A patient with this diagnosis will be diagnosed with an increased content of nitrogen compounds in the blood, and this figure of 30 m/mol or higher is a direct indication for renal replacement therapy.
In addition to kidney diseases, this type of therapy can be prescribed for acidosis, pulmonary edema, hyperkalemia, sepsis, congestive heart failure and while taking highly toxic drugs.
Please note: renal replacement therapy is prescribed on a strictly individual basis. A specific disease is not always an absolute indication - it all depends on the severity of its course, the general condition of the patient, and indicators of laboratory and instrumental studies. Doctors are extremely careful when prescribing renal replacement therapy early.
This type of therapy can be carried out using several different methods.
Kidney transplant
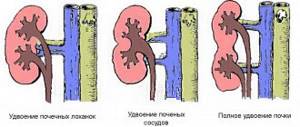
Kidney transplantation is used as a surgical method for treating diseases of the organ if there is no other method other than transplantation. Renal transplantation has the highest survival rate among RRT methods. Indications for transplantation are chronic renal failure resulting from severe diseases or congenital pathologies.
Material for transplantation can be taken from a living person or from a deceased person.
When preparing for transplantation, compatibility should be checked:
- blood groups,
- genetic materials
- correspondence between the ages of the patient and the donor.
Practice shows that donors are often close relatives. A kidney transplant does not pose any risk to the donor.
Contraindications
To prevent rejection of the donor kidney after surgery, it is necessary to refuse transplantation in the following cases:
- if immunological incompatibility is observed;
- the presence of malignant growth of the kidney or other organs, with the exception of asymptomatic, effectively treated tumors;
- if there is an infection in the body;
- exacerbation of coronary heart disease, peptic ulcer, diabetes mellitus;
- presence of mental disorders.
Consequence of organ implantation
It takes 3-5 days for the donor kidney to start functioning normally. Symptoms of kidney failure may take several weeks to disappear.
The doctor prescribes hormonal drugs to prevent transplanted organ rejection
To avoid rejection of the transplanted organ, the patient is administered immunosuppressive medications at the end of the operation. Cytostatics and steroids (Azathioprine, Prednisolone, Cyclosporine) prevent immune cells from perceiving the implant as a foreign body.
The effect of these drugs has a negative side: when the immune system is suppressed, the possibility of infections opens up, which is fraught with the occurrence of various diseases. It is mandatory to follow a diet in the postoperative period that does not allow eating spicy, salty, smoked, fatty, or sweet foods.
Nephrology services use all 3 methods of renal replacement therapy. Timely seeking medical help and the correct choice of replacement therapy can save the patient’s life.
Renal replacement therapy
The possibility of artificially replacing kidney function through dialysis appeared in the 60s of the 20th century. This treatment is now routine for kidney failure.
At the same time, the metabolic and endocrine functions of the kidneys are not replaced, but the biochemical parameters of the plasma (uremic toxins, electrolytes and acid-base state) are maintained at acceptable levels. Additionally, dialysis can remove fluid from the bloodstream (ultrafiltration) to maintain euvolemia.
The main side effects of dialysis are related to hemodynamic disturbances due to fluid removal or extracorporeal circulation, as well as reactions between the blood and components of the dialysis system (biological incompatibility).
The original method of renal replacement therapy was hemodialysis, which remains the most common form of this treatment. Many other techniques have also been developed, especially for patients with acute renal failure who are not receiving chronic renal replacement therapy.
Renal replacement therapy for acute renal failure
There is an individual approach to prescribing renal replacement therapy, taking into account various aspects of the patient's condition. The following indications are recommended.
Increased urea and creatinine. It is undesirable to achieve urea > 30 mmol/l (180 mg/dl), and creatinine > 600 µmol/l.
At lower levels of these metabolites, a progressive disturbance of biochemical parameters can be considered an indication for dialysis, especially with little or no urine production.
There is a trend towards earlier initiation of dialysis in acute renal failure. But there are studies regarding very early initiation of dialysis for oliguria.
Hemodialysis
Hemodialysis or filtration requires access to the bloodstream. This may include arteriovenous fistulas, temporary or semi-permanent central venous catheterization, or arteriovenous shunts (eg, Scribner shunt). Extracorporeal circulation requires the use of anticoagulants, usually heparin
Successful transplantation prolongs life in end-stage chronic renal failure. Long-term use of immunosuppressive therapy is required with associated health risks.
Indications for hemodialysis
Hyperkalemia. Dangerous calcium level >6 mmol/l. Elevated potassium levels can be quickly reduced medically, but dialysis is often required for definitive control.
Metabolic acidosis. Often accompanied by hyperkalemia, leading to a further increase in potassium levels.
Hypervolemia and pulmonary edema. In patients with constant urine production, it can be controlled by careful fluid balance and diuretics, but in patients with oliguria, anuria (dialysis) may be an indication for renal replacement therapy.
Uremic pericarditis/uremic encephalopathy. Signs of severe untreated kidney failure; uncharacteristic of acute renal failure, there are strict indications for starting renal replacement therapy.
The main options for renal replacement therapy for acute renal failure are hemodialysis, high-volume hemofiltration, continuous arteriovenous or venovenous hemofiltration, and peritoneal dialysis.
Intermittent hemodialysis
This technique provides the highest rate of removal of small solutes. In patients with acute renal failure and elevated plasma urea who have not previously undergone dialysis due to the risk of confusion and convulsions due to cerebral edema (dialysis imbalance), hemodialysis should be started gradually.
Typically, partial dialysis sessions (1 hour) are performed at the beginning. Subsequently, patients with acute renal failure with stable hemodynamics can receive hemodialysis for 3-4 hours every other day or, in case of severe metabolic disorders, for 2-3 hours every day.
When carrying out short dialysis sessions, as well as in cases of blood clotting disorders, the use of anticoagulants can be avoided.
Hemofiltration
Hemofiltration can be either intermittent, in which 15-30 liters of plasma ultrafiltrate is exchanged for replacement fluid in 3-5 hours (high-volume hemofiltration), or continuous, in which 1-2 liters of filtrate are replaced per hour (equivalent to GFR 15-30 ml /min); higher filtration rates may be used for sepsis and multiple organ failure. With constant arteriovenous hemofiltration, the driving force of extracorporeal circulation is the difference in arterial and venous pressure. With this treatment, filtration failure and thrombus formation in the filter often occur, leading to a decrease in its effectiveness. Continuous venovenous hemofiltration occurs using a pump, providing reliable extracorporeal circulation. In this case, the same clotting problems occur as with hemodialysis, but they may be more severe and require longer or permanent anticoagulant therapy.
Intermittent hemodiafiltration
This technique combines conventional hemodialysis with a good rate of excretion of small solutes and high ultrafiltration capacity of hemofiltration.
Peritoneal dialysis
This technique is rarely used in acute renal failure because it is less effective than hemodialysis and rarely provides rapid biochemical control. It requires an intact abdominal cavity and is not feasible after recent abdominal surgery
Renal replacement therapy for chronic renal failure
If progressive chronic renal failure is diagnosed, preparation for renal replacement therapy should begin at least 12 months before the expected start date. This includes psychological and social support, assessment of home conditions and discussion of treatment options.
The main problems are represented by the choice between hemodialysis and peritoneal dialysis, as well as the decision regarding referral for kidney transplantation.
Due to the historically high incidence of viral transmission during dialysis, all patients should be pre-screened for hepatitis B, hepatitis C and HIV, and vaccinated against hepatitis B in the absence of specific immunity.
In the UK, among patients starting dialysis, 70% receive hemodialysis and 30% receive peritoneal dialysis. Mortality studies show that 78% of patients survive 1 year (87% of patients survive 90 days of treatment) and 45% of patients survive 5 years.
Mortality varies by age; In patients over 75 years of age, the 5-year survival rate is 15%, and among patients under 45 years of age, 83% survive 5 years.
Comorbid conditions such as diabetes mellitus (30% 5-year survival rate) and generalized vascular disease (34% 5-year survival rate) also influence the prognosis of these patients.
Intermittent hemodialysis
Intermittent hemodialysis is the standard blood purification treatment in ESRD. Hemodialysis is started in the presence of severe symptoms of renal failure, but before the development of serious complications, usually when creatinine is 600-800 µmol/l.
Hemodialysis requires vascular access; it is necessary to form an arteriovenous fistula, usually on the forearm. Formation of a fistula must be carried out when the patient reaches stage IV of kidney disease.
After 4-6 weeks, increased pressure in the vein coming from the fistula leads to its expansion and thickening of the vascular wall (arterialization). After this, a needle with a large hole can be left in the vein for hemodialysis sessions.
Thus, in patients with advanced kidney disease, where hemodialysis may be required in the future, preservation of arm veins is very important. If such access is not possible, central venous catheterization with plastic cannulas can be used for short-term access.
Hemodialysis sessions are usually carried out for 3-5 hours 3 times a week. Most patients note an improvement in their well-being in the first 6 weeks of treatment. After each session, a decrease in urea and creatinine occurs, but they do not return to normal. Some patients may receive treatment at home. Most young patients without comorbidities survive on hemodialysis for more than 20 years.
Continuous ambulatory peritoneal dialysis
Continuous ambulatory peritoneal dialysis (CAPD) is a form of long-term dialysis in which an indwelling silicone catheter is inserted into the peritoneal cavity. Two liters of sterile isotonic dialysis fluid is injected into the peritoneal cavity and left there for approximately 6 hours.
During this time, metabolic products diffuse through the capillaries of the peritoneum into the dialysis fluid along a concentration gradient. The spent fluid is then removed and fresh dialysis fluid is introduced.
The injected fluid is hyperosmolar due to glucose; this results in partial removal of fluid from the patient's body during each cycle (ultrafiltration). The cycle is repeated 4 times a day, during which time the patient is mobile and able to carry out daily activities normally.
CAPD is especially useful for young children, as well as for older patients with cardiovascular instability. Its long-term use may be limited to episodes of bacterial peritonitis and peritoneal injury, but patients can be treated successfully for more than 10 years.
Currently, the use of automated peritoneal dialysis is not widespread. This procedure is similar to CAPD. It is carried out using a mechanical device that exchanges liquid throughout the night without causing difficulty for the patient. A one-time exchange can also be carried out during the day.
Contraindications for kidney transplantation
Absolute
Active tumor: Most tumors require at least 2 years of sustained remission before transplantation.
Active vasculitis or a disease with autoimmune damage to the BMK, with positive serological reactions, at least a year of remission is recommended before transplantation.
Severe coronary heart disease.
Severe occlusion of the aorta and iliac vessels.
Renal replacement therapy in the elderly
Quality of life: Age alone is not a barrier to a good quality of life with renal replacement therapy.
Cardiovascular disease: Its severity can make dialysis difficult. Older adults are more sensitive to changes in fluid balance and are prone to hypotension during dialysis, with rebound hypertension 1 between dialysis sessions. An ischemic heart cannot cope with hypervolemia, and pulmonary edema easily develops.
Treatment conditions: Older patients should only undergo hemodialysis in a hospital and require more medical and nursing time.
Survival on dialysis: It is difficult to predict the life expectancy of an individual patient, but it correlates with age, functional ability and comorbidities.
Withdrawal from dialysis: A common cause of death in older patients is comorbidities.
Transplantation: For most patients, barriers to transplantation include the relatively high risk of surgery and immunosuppression, as well as limited organ function.
Conservative therapy: i.e. treatment without dialysis but with adequate support may be a popular choice when the risk of dialysis-related complications worsening the prognosis is high
Kidney transplants can be taken from cadavers and living donors. The selection of a donor for a particular recipient strictly depends on immunological factors, with tissue incompatibility being the main reason for refusal.
Compatibility with ABO (blood group) antigens is important, as well as the degree of matching of the major histocompatibility complex (MHC), which affects the frequency of rejection.
The main cells involved in graft rejection are T cells; The presence of cytotoxic antibodies, which may be present in the body before transplantation (sensitization), is also important.
Before transplantation, cytotoxic tests are performed for these antibodies, as well as cross-tests for the compatibility of T and B cells (donor lymphocytes are mixed with the patient’s serum). Positive results predict early rejection.
The article was prepared and edited by: surgeon I.B. Pigovich.
Source: https://surgeryzone.net/info/informaciya-po-nefrologii/zamestitelnaya-pochechnaya-terapiya.html