Forms of glomerulonephritis in children
Doctors distinguish two types of this disease - chronic and acute glomerulonephritis in children.
They differ not only in the nature of their course, but also in other characteristics, namely:
- An acute illness almost always occurs as a result of a recent infectious disease. Its symptoms are always pronounced, and the baby’s general well-being deteriorates quite sharply. If this disease is detected in a timely manner, it can be eliminated without much difficulty;
- the chronic variant is also called “diffuse”. It is a severe and dangerous inflammatory process in the kidneys, which over time causes the death of the kidney glomeruli. In the vast majority of cases, the chronic form of the disease occurs as a result of an untreated acute form. The symptoms of this disease can be erased and resemble hypertension. This form of the disease must be treated in a hospital setting for a long time. Fortunately, this type is quite rare among children - in approximately 2% of cases, a child with glomerulonephritis is diagnosed with its chronic stage.
Treatment
Treatment of glomerulonephritis in children has one feature - the disease is much easier to tolerate than in adults.
Treatment of glomerulonephritis in children has one feature - the disease is much easier to tolerate than in adults. The treatment regimen is as follows:
- The child must remain in bed until the main symptoms of the disease disappear. This usually takes several weeks.
- Antibacterial therapy with the prescription of penicillin and macrolide drugs is mandatory.
- To facilitate the removal of fluid from the body, medications with a diuretic effect are prescribed.
- If, within seven days after the start of treatment, the child’s pale yellow skin tone, the smell of urine from the mouth does not disappear, and an increased level of toxic substances in the blood is observed, then hemodialysis is required using an artificial kidney machine.
- With glomerulonephritis, children must follow a diet that includes carbohydrate days. During treatment, the child should not be given meat (only chicken is allowed), fish (only low-fat lean fish is allowed), seasonings, smoked meats, meat broths, and marinades. It is healthy to eat vegetable and fruit dishes, vegetarian soups, natural juices, dairy products and foods rich in potassium. It is better to eat food 3-5 times a day.
Attention: you need to reconsider your child’s drinking regime. The daily volume of fluid can be no more than 0.5 liters greater than the total amount of urine excreted.
After the illness, the child must be registered with a pediatrician and pediatric nephrologist for another five years. In case of relapse of the disease, lifelong dispensary registration is required. Vaccination is usually contraindicated for such children. A sanatorium stay is useful for disease prevention.
Causes of acute glomerulonephritis in children
The main cause of acute glomerulonephritis is an infection that has entered the child’s body, mainly streptococcal. As a rule, this disease develops in a child approximately 2-3 weeks after suffering from influenza, sore throat, scarlet fever, pharyngitis, laryngitis, tonsillitis, as well as some viral infections of the respiratory tract. In rare cases, glomerulonephritis turns out to be a complication after measles or chickenpox.
Meanwhile, this is the main reason, but far from the only one. In fact, even the formation of a small abscess on a child’s skin or simple hypothermia can cause the development of this disease.
PATHOGENESIS
There are immunologically determined and immunologically non-determined variants of the disease.
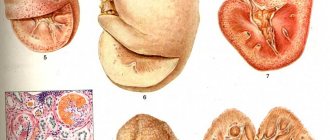
Immunologically caused can be of immunocomplex or, less commonly, autoantibody origin. Most forms of primary chronic glomerulonephritis are classified as immune complex glomerulopathies. Their pathogenesis resembles that of acute glomerulonephritis (see section “Acute glomerulonephritis”). The involvement of immunological processes in minimal change glomerulonephritis is a matter of debate. Examination of the glomeruli by immunohistochemical method does not reveal specific changes in this variant of the disease. Electron microscopy reveals a reduction in small processes of podocytes, indicating metabolic changes in the cells. Pathology of podocytes leads to disruption of the integrity of the glomerular filter. As a result, excess proteins and lipids penetrate into the primary urine and, being reabsorbed, accumulate in the tubular epithelium. Protein and fatty degeneration of tubular cells develops, clearly visible under light microscopy, which in the past gave rise to calling the pathological process “lipid nephrosis.”
Main symptoms and methods of treatment of acute glomerulonephritis
The signs of this disease almost always appear very clearly, so it is incredibly difficult to miss this disease.
As a rule, in the acute phase the disease is accompanied by the following symptoms:
- general weakness, including muscle weakness;
- increased fatigue, inability to perform usual activities, excessive drowsiness;
- strong thirst;
- a gradual decrease in urine output during the day;
- change in color of discharge;
- noticeable swelling that starts from the face and spreads to the lumbar region and lower extremities;
- headache;
- nausea and vomiting;
- blurred vision;
- simultaneous increase in upper and lower blood pressure. This symptom may indicate a possible transition of the disease to the chronic stage. If the situation does not return to normal within 3-4 months, and hypertension persists, despite all the measures taken, most likely, acute glomerulonephritis was followed by complications, and this disease took a chronic form.
Acute glomerulonephritis can provoke other complications, namely:
- acute renal or heart failure;
- intracerebral hemorrhage;
- preeclampsia or eclampsia;
- cerebral edema.
That is why, in order to prevent the development of such complications, treatment of this disease should begin immediately after the first signs of the disease are detected. As a rule, if the child himself does not complain to his parents about changes in his condition, mom and dad begin to suspect something is wrong based on the change in the color of the baby’s urine.
Causes of glomerulonephritis
There are immune and non-immune glomerulonephritis .
Congenital and hereditary kidney diseases, accompanied by damage to the glomeruli, can only be conditionally classified as glomerulopathies, since they involve genetically determined damage not only to the glomeruli, but also to the tubules, renal parenchyma and renal vessels. Glomerulonephritis can develop at any age, but most often it occurs between 7 and 12 years of age.
Hereditary nephritis is most often inherited according to the dominant type linked to the X chromosome, which does not exclude another type of inheritance.
The following variants of hereditary nephritis are distinguished:
- Alport syndrome
- hematuria syndrome without hearing loss
The first includes damage to the kidneys, eyes, and auditory nerve. Kidney damage manifests itself in the form of microhematuria, proteinuria and cylindruria are possible. Urinary syndrome increases in adolescence and in adults. The prognosis is often unfavorable. Deafness is observed in half of the boys with hereditary nephritis.
Hematuria syndrome without hearing loss is manifested by microhematuria, occurs in children of both sexes, the prognosis in most cases is favorable.
Adequate assessment of the clinical manifestations of hereditary nephritis is of great importance, since their timely distinction from acquired glomerulonephritis allows one to correctly determine the amount of necessary therapy.
Recently, it has become common to distinguish primary glomerulonephritis, which develops several weeks after exposure of the kidney tissue to infectious, allergic and other factors. Secondary or systemic glomerulonephritis occurs with rheumatism, hemorrhagic vasculitis, periarteritis nodosa, cryoglobulinemia, etc.
Primary glomerulonephritis is a polyetiological disease. Often the cause of the disease is a streptococcal or staphylococcal infection. A major role in the development of the disease has been proven for viruses (cytomegalovirus, herpes virus, HBs-Ag). The role of sunlight, hypothermia, chemicals and medicinal substances remains controversial.
Symptoms
The disease usually occurs acutely in children. The following symptoms are characteristic of glomerulonephritis:
- Pain in the lumbar area.
- Swelling of the face, especially in the eyelid area.
- Hypertension.
- Reducing the daily amount of urine excreted.
- Urine takes on a dark rusty color.
- Headache.
The state of health deteriorates sharply and rapidly. The most dangerous is the rapidly progressing form of acute glomerulonephritis. Then the following manifestations are added to the general symptoms:
- Presence of flakes in urine.
- The appearance of blood clots in urine.
- The presence of a large number of protein bodies in the urine.
It happens that the pathology occurs hidden. Then most of the signs described above are not observed in the child. The disease can only be recognized during a preventive examination and testing.
Prevention
Preventive measures: adequate and relevant treatment of ARVI, influenza, and other respiratory tract infections; completely eliminate allergens from the diet, adhere to sleep and nutrition regimens; avoid purulent lesions on the skin. As such, there is no prevention of chronic glomerulonephritis, only constant observation. As you can see, glomerulonephritis is a very severe and serious disease that can serve as a trigger for the development of many complications. Therefore, in no case should you self-medicate, and at the first discomfort you should consult a doctor and follow all his recommendations.
General information
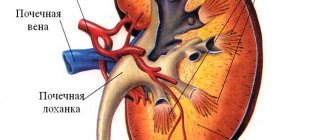
Before you get acquainted with the causes of glomerulonephritis, you should familiarize yourself with the functions of the kidneys and the mechanism of their work. The main functions of the kidneys are to remove protein breakdown products, toxic foreign compounds, and excess organic and inorganic particles from the body. The kidneys are also involved in the formation of blood and are responsible for blood pressure levels.
A nephron is a structural unit of the kidney that consists of tubules and glomeruli in the kidneys. When these same glomeruli are damaged, the process of purifying the blood from harmful substances is disrupted. Red blood cells, as well as protein, begin to leak into the urine along with salts. When diagnosing glomerulonephritis in children, large protein losses are observed and in a situation where red blood cells are reduced, there is a risk of anemia.
Glomerulonephritis occurs quite often, moreover, it occupies the second “prize” position among kidney pathologies, sacrificing only to diseases of the urinary system. It most often affects children aged 2−12 years. In young children under 2 years of age, this disease is rarely diagnosed. Among girls, the diagnosis is confirmed two times less often than among boys. Glomerulonephritis is especially dangerous for children, as there is a risk of kidney failure and a chance of disability at an early age.
Causes
It is possible to identify the cause of this pathology in children in 80-90%, but in the case of a chronic form, only in 5-10%. This percentage difference is due to the fact that the main causes of glomerulonephritis are infections.
Enterococci - pathogens
These can be bacteria (nephritogenic strains of group A hemolytic streptococcus, enterococci, pneumococci, staphylococci), parasites (toxoplasma, the causative agent of malaria), viruses (measles, chickenpox, rubella, hepatitis B), fungi, such as candida. Sometimes the development of the acute form can be triggered by non-infectious factors, such as a vaccine, foreign protein, serum, drugs, pollen, toxins.
The development of the acute form can be facilitated by a sore throat, pharyngitis, scarlet fever, pneumonia, impetigo, streptoderma and other diseases caused by streptococcal bacillus.
Chronic glomerulonephritis in children develops as a consequence of an untimely treated inflammatory process.
The main cause of the development of glomerulonephritis is the genetic component of the determined immune response to antigens inherent in each individual organism.
As a result of this response, specific immune complexes are formed, which damage weak capillaries in the renal glomeruli. Such damage, in turn, leads to disturbances in microcirculation, and further to inflammatory and degenerative changes in the kidney.
Often, glomerulonephritis develops with connective tissue diseases. In addition, the disease can develop in the presence of a hereditarily determined anomaly, for example, T-cell dysfunction or with a hereditary deficiency of the C7 and C6 fractions of complement and antithrombin.
Children may be at risk for developing glomerulonephritis if they have a family history, are carriers of nephritic strains of group A streptococcal infection, have an increased sensitivity to streptococci, or have a focal chronic infection on the skin or nasopharynx.
For the development of glomerulonephritis from a latent streptococcal infection, it is enough to overcool the body and develop ARVI.
The course of the disease in children can be influenced by physiological features. Thus, in children, the course of glomerulonephritis can be complicated by the functional immaturity of the kidney, as well as the peculiar reactivity of the body (changes in immunopathological reactions).
If a child has a chronic sore throat, a smear should be taken for a strep throat infection. After all, there is a high probability of complications in the form of glomerulonephritis.
Diagnostics
The disease can be diagnosed using the following tests:
- biochemical urine analysis and Nechiporenko analysis (for the presence of protein in urine);
- a blood test that will show an increase in ESR, anemia, a decrease in protein, an increase in globulins, a decrease in albumin;
- immunological testing, it will detect the presence of antibodies to streptococcus;
- biopsy.
Additionally, the doctor may prescribe:
- Ultrasound of the kidneys;
- puncture biopsy;
- computed tomography;
- chest x-ray;
- X-ray of the kidneys.
The patient is examined by an otolaryngologist, dentist, ophthalmologist and geneticist to identify the causes of the infection.