What is prostatitis in men
- How does prostatitis occur in a husband?
- Why are different forms of prostatitis dangerous?
- Prostatitis by form of occurrence
- How to overcome different types of prostatitis
According to the simplest definition, prostatitis is a urological disease, which is inflammation of the prostate (prostate gland) and its swelling. In fact, the question of what prostatitis is in men and the dangers of bringing your body to such a state is quite serious. Almost half of the planet's population (of course, representatives of the stronger sex) aged 20-50 years are familiar with prostatitis quite closely, and from 30 to 50 years the probability of getting sick for each man increases by 20%. And if you consider that this disease has become considerably “younger” in recent decades, interest in this problem is completely justified.
How does prostatitis occur in a husband?
It should be noted right away: when the first symptoms of the disease appear, most men are embarrassed to see a doctor. Even in the modern world, it is not uncommon for a wife to come to the hospital with a lot of questions: “It seems that my husband has prostatitis. What should we do? How to treat it? How to live further? And specialists have to explain the intricacies of how the male body works, sometimes even deliberately frightening the anxious wife in order to force her to literally “drive” her man to the urologist.
It seems strange that modern men - even the most successful, intelligent and educated - doctors still have to give lectures on the topic “What is prostatitis.” For many representatives of the stronger sex, who nevertheless decide to seek help, when certain symptoms of an illness appear, the fact of their vulnerability is a surprise. But an examination by a urologist should become a common tradition from a certain age, so that your own body does not turn out to be a time bomb.
But before we define what prostatitis is in men, it is worth talking about what the prostate gland is. This muscular organ is found only in the male body; it is located in the pelvic area, above the urethra and in close proximity to the vas deferens. The prostate produces a special secretion, which is a component of sperm, due to which it performs the following functions:
- ensures optimal sperm activity and motility;
- supports the stability of the genitourinary system in the fight against infections;
- regulates healthy erection process;
- stimulates testosterone production;
- “coordinates” the activity of the pituitary gland;
- controls normal urination.
Since the scope of activity of the prostate gland is quite wide, prostatitis is dangerous because it provokes a lot of different problems associated with the malfunction of this organ.
Inflammation affecting the prostate provokes its increase in size, during which:
- the ureters are compressed (as a result - problems with urination);
- secretory functions change (consequences - frequent infections, hormonal imbalances, decreased sexual strength, infertility).
Why are different forms of prostatitis dangerous?
Experts identify various signs by which prostatitis in men is classified. So, according to the form of the disease, it can be:
The acute form of inflammation is provoked by damage to prostate tissue by infection, which is a consequence of the pathogenic activity of microorganisms (bacteria, protozoa, fungi). In a normal state of health, these creatures are a familiar part of the body's microflora, however, sometimes a colony of neutral inhabitants increases abnormally and provokes acute inflammation of the prostate gland. This happens when certain factors coincide:
- decreased immunity;
- the presence of concomitant chronic infections;
- existing pathologies of internal organs;
- hormonal imbalances;
- recent surgery.
Acute prostatitis develops rapidly and is usually accompanied by the following symptoms:
- urinary problems (difficulty, frequent urge, sometimes delay);
- sharp pain in areas of the lower body (from the groin and anus to the lower back and legs);
- pain syndrome accompanying the processes of erection, urination, defecation;
- problems with erection (also failures of ejaculation);
- feelings of general malaise.
Although death from even the acute form of prostatitis is unlikely, this condition can only be treated in a hospital setting under the supervision of specialists so that the inflammation does not become chronic or lead to even more serious complications. A complete cure is possible, but only with timely initiation of therapy - this is important to remember for those who, instead of seeing a doctor, wonder whether prostatitis can go away on its own.
A chronic form of inflammation of the prostate gland can develop against the background of tissue damage by microorganisms or due to other phenomena:
- stagnation of blood or prostate secretion;
- age-related changes;
- autoimmune reaction.
The development of chronic lesions can occur against the background of certain risk factors, including:
- transmission of infections of the reproductive system;
- weakened immune system;
- maintaining a sedentary lifestyle;
- frequent stressful situations;
- poor nutrition, causing problems with bowel movements;
- injuries of the pelvic organs (damage to the prostate gland);
- frequent hypothermia (or isolated, but prolonged);
- bad habits.
Chronic inflammation can be asymptomatic - in this form, although the process is clearly occurring, the pathogenic environment is not detected in the tests being studied. However, in most cases, the “chronic” is a lesion that developed from an acute form that did not receive sufficient treatment.
With chronic prostatitis, the following symptoms appear:
- difficulty urinating;
- unpleasant sensations (even mild pain) in the perineal area;
- sharp pain and burning in the groin;
- decreased sex drive;
- general state of weakness, apathy, nervousness.
What is dangerous about chronic prostatitis is that with it, stages of remission are interspersed with stages of exacerbation, which are painful and can cause serious harm without the control of the attending physician. In addition, this form of the disease, if not treated in time, provokes a lot of complications, including:
- adenoma;
- infertility;
- vesiculitis;
- inflammation of the testicles;
- pyelonephritis;
- prostate cancer;
- cystitis.
Considering that the consequences of the development of these complications range from harm to health to the danger of death, the answer to the question of whether such a disease is dangerous seems obvious.
Prostatitis by form of occurrence
In addition to distribution according to the form of its course, prostate disease is classified according to the types of pathogens that provoke it. Separately, it is immediately necessary to distinguish the asymptomatic form, which develops without noticeable clinical manifestations and without the influence of microbes, viruses, and bacteria. Treatment of asymptomatic (non-bacterial) prostatitis is often not even required - it is enough to relieve inflammation and eliminate the phenomena that initially caused the problem.
Unlike non-bacterial lesions, infectious prostatitis occurs:
- bacterial (the causative agents are staphylococcus, streptococcus, Escherichia coli and Pseudomonas aeruginosa bacteria);
- viral (develops after entry into the body of herpes viruses, human papilloma, influenza, cytomegalovirus);
- mycoplasma (the culprits of development are intracellular organisms mycoplasma);
- gonorrheal (caused by gonococci);
- chlamydial (development occurs under the influence of intracellular organisms chlamydia);
- Trichomonas (pathogens are protozoa called Trichomonas);
- tuberculosis (cause of inflammation - Koch bacillus);
- fungal (occurs under the influence of candida fungi against the background of a weakened immune system).
Treatment of pyelonephritis
Patients need:
- adhere to the drinking regime;
- in case of acute form of the disease or in case of exacerbation of the chronic form, observe bed rest for 3 days;
- the diet includes the consumption of lean meat, stale bread, vegetable soups, and dairy products. You will need to exclude alcohol, smoked foods, meat or fish broth, sweets, and spices.
Medicines prescribed include antibacterial drugs (cephalosporins, fluoroquinolones), anti-inflammatory drugs (Diclofenac), and multivitamins. After receiving the results of antibacterial sensitivity tests, the doctor may change the antibiotic.
Herbal medicine: decoction of St. John's wort, chamomile, horsetail, rose hips, etc.
For chronic pyelonephritis, courses of physiotherapy are prescribed: galvanization, electrophoresis, ultrasound. Spa treatment is indicated.
With the development of uncontrolled sepsis, at the stage of kidney shrinkage, surgical intervention is performed - kidney removal (nephrectomy).
Slide captions:
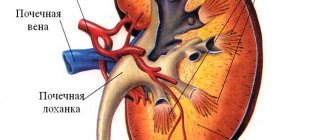
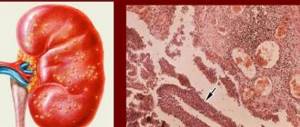
Pyelonephritis is a nonspecific inflammatory process with predominant damage to the renal tubular system, predominantly of bacterial etiology, characterized by damage to the renal pelvis, calyces and renal parenchyma. Pyelonephritis is dangerous because it often occurs asymptomatically, without disturbing a person’s well-being, so some patients treat their problem lightly. The most common of the nonspecific inflammatory diseases of the upper urinary tract, accounting for about 2/3 of all urological diseases, is acute and chronic pyelonephritis.
Pyelonephritis can be acute or chronic. begins suddenly, temperature rises sharply to 39-40°C, weakness, headache, profuse sweating, possible nausea and vomiting. pain in the lower back, as a rule, on one side, is dull in nature. Urination in the uncomplicated form of pyelonephritis is not impaired. Pasternatsky's positive symptom is a consequence of untreated acute pyelonephritis General weakness, lack of appetite, frequent urination Dull aching pain in the lower back Skin is pale, dry.
Etiology and pathogenesis Escherichia coli Proteus Enterococci Pseudomonas aeruginosa Staphylococci Penetration of the pathogen into the kidney in acute pyelonephritis most often occurs hematogenously from any source of infection in the body due to the development of bacteremia. Less commonly, the infection enters the kidney via the urinogenic route from the lower urinary tract (urethra, bladder) along the wall of the ureter (in this case, the disease begins with the development of urethritis or cystitis
Causes: urolithiasis, frequent attacks of renal colic, decreased general immunity of the body, diabetes mellitus, chronic inflammatory diseases and hypothermia, the presence of salts or kidney stones
Complications Acute renal failure Chronic renal failure Paranephritis Urosepsis
Diagnostics Laboratory research methods General blood test (general inflammatory changes: leukocytosis, accelerated ESR, with severe inflammation - anemia. Biochemical blood test (increased levels of urea, creatine) Urinalysis General urinalysis (leukocyturia, erythrocyturia) Bacteriological examination of urine is used to accurately determine the pathogen and its sensitivity to antibiotics
Instrumental research methods: ultrasound examination. X-ray research methods: - survey and excretory urography. An overview image may reveal an increase in the size of the kidney, bulging of its contour (in case of carbuncle and abscess - retrograde pyeloureterography is performed in the absence of kidney function on excretory urograms or if for some reason excretory urography cannot be performed (the patient’s serious condition, the presence of acute or chronic renal failure).
Treatment Antibacterial therapy, infusion-detoxification, anti-inflammatory therapy, physiotherapy. Functional-passive kidney exercises (20 ml of furosemide are prescribed 1-2 times a week). catheterization of the ureter on the affected side in order to restore the outflow of urine from the affected kidney.
prevention To prevent the occurrence of pyelonephritis, it is necessary to: consume a sufficient amount of fluid to ensure normal urine outflow; do not hold urination for a long time if there is an urge; promptly and completely treat any infectious diseases; avoid hypothermia; observe the rules of personal hygiene; lead a healthy lifestyle, regularly conduct courses of restorative therapy: moderate physical activity, hardening, a balanced diet, and the diet must include fruits, vegetables, and herbs; Take multivitamins periodically; men suffering from prostatitis need to regularly monitor the health of the urinary system; Pregnant women are advised to have their urine tested more often.
Symptoms of pyelonephritis
Here are the typical symptoms:
- dull paroxysmal intense pain in the lumbar region from the affected kidney;
- increase in body temperature up to 40 degrees;
- chills;
- weakness; anemia;
- lack of appetite;
- frequent urination;
- tachycardia;
- 10% of patients have urine mixed with blood;
- cloudy urine;
- nausea, vomiting.
Symptoms of pyelonephritis in children
- increase in body temperature up to 40 degrees;
- weakness;
- refusal of food;
- regurgitation in infants;
- poor sleep;
- urinary incontinence;
- tension when urinating;
- frequent urination in small portions of urine;
- cloudy urine.
Content
Completed by: student of the 504th group of the pediatric faculty Vasilyeva V.G.
"Pregnancy and pyelonephritis"
Pyelonephritis is an infectious and inflammatory process that is accompanied by damage to the interstitial tissue of the kidneys, the tubular apparatus and the walls of the renal collecting system.
ClassificationLopatkin.N.A.1974
Primary (develops without the presence of concomitant urological pathology) Secondary (Develops against the background of an existing pathology.)
Gestational pyelonephritis Pyelonephritis that occurred for the first time during pregnancy, childbirth or the early postpartum period………………
Pathogens
Gram+ Gram- Staphylococcus Enterococci Group D and B Streptococci Escherichia coli Klebsiella Proteus CMV + herpesvirus Own flora
Physiological changes
decreased tone (hypotension) and motility (dyskinesia, hypokinesia) of the pelvis and ureters under the influence of estradiol, other estrogens and progesterone, the concentration of which increases significantly; hemodynamic disorders in the kidney, pyelocaliceal system and ureters (hypoxia) associated with hormonal changes and the above urodynamic disorders;