Causes of chronic pyelonephritis
The immediate cause of inflammation in the kidneys is infection. As in the acute form of the disease, the main pathogens in pyelonephritis are opportunistic microorganisms: Escherichia coli (E. coli - 80% of cases), Klebsiella (3-6% of cases), various strains of saprophytic Staphylococcus (less than 3% of cases), Proteus, enterobacter, enterococci. However, in acute pyelonephritis, the treatment allows you to quickly eradicate the pathogen from the urinary tract with the help of antibacterial drugs without serious consequences. Chronic pyelonephritis, in contrast to acute pyelonephritis, is difficult to treat and consists of alternating exacerbations, leading to even greater damage to the kidney tissue. In some cases, the pathogen cannot be identified.
For a long time it was unknown why acute pyelonephritis passes without a trace in some patients, while in others it is accompanied by constant exacerbations. The leading role was played by the hypothesis that the main factor in the development of chronic pyelonephritis was a decrease in immunity. Low reactivity of the body does not allow you to effectively fight infection.
It is currently believed that abnormal urine flow (vesicoureteral reflux) plays a major role in the development of the disease. The bladder and its hyperreactivity (dysfunction), chronic foci of infection (chronic prostatitis, chronic cystitis, urethritis), congenital anomalies of the urinary tract create additional conditions for the infection to spread upward through the ureters to the kidney. Normally, the vesicoureteral valve prevents this by preventing urine from entering the bladder into the upper excretory system. However, some people have congenital valve insufficiency. As a result, the risk of ascending kidney infection increases sharply, which leads to frequent exacerbations of chronic pyelonephritis. Possible bilateral or unilateral lesions.
Additional predisposing factors are considered:
- gender and age of the patient (in sexually active men and especially women, chronic pyelonephritis is diagnosed more often);
- pregnancy (leads to difficulty in the outflow of urine and decreased tone of the urinary tract);
- virulence of the infectious agent;
- genetic predisposition to the disease;
- the presence of factors that impair the outflow of urine (prostate adenoma, neurogenic bladder, ureteral strictures).
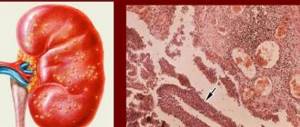
When infected urine enters the kidney, inflammation occurs. In this case, the affected part of the kidney tissue dies, and processes of death of nephrons, which are the structural and functional units of the organ, occur in it. Inflammation resolves by replacing necrotic areas with connective tissue. With each repeated attack, the number of lost nephrons increases, as does the severity of fibrosclerotic changes. Over time, kidney function begins to suffer from this, since the remaining part of the nephrons is not enough to effectively remove toxins and metabolic products. Sclerotic processes disrupt microcirculation and blood circulation in the kidney tissue. In response to hypoperfusion, the renin-angiotensin system is activated, leading to renal hypertension.
During fibrosclerotic processes in the renal tissues, the synthesis of erythropoietin (one of the kidney hormones), which stimulates hematopoiesis, suffers. For this reason, already deeply developed pyelonephritis is often accompanied by anemia.
The outcome of the above processes is chronic renal failure, which always ends in death without treatment with dialysis or kidney transplantation.
Causes
Etiological factors of the disease are divided into the following categories:
- Primary (endogenous);
- Secondary (exogenous).
Exogenous causes of pathology:
Causative agents of intestinal infection
- Dysbacteriosis and intestinal infections;
- Gastrointestinal disorders;
- Enterobiasis and helminthic infestations;
- Chronic respiratory and viral infections;
- Hypothermia;
- Poor nutrition;
- Use of nephrotic drugs;
- Organic and functional intestinal disorders;
- Inflammatory changes in the ENT organs.
Endogenous etiological factors of chronic pyelonephritis:
- Developmental defects (acquired and congenital), formed due to poor heredity or exposure to occupational hazards;
- Intrauterine infections, fetal hypoxia, gestosis in pregnant women, prematurity;
- Constitutional diathesis;
- Intrauterine pathology of the nervous system, urinary tract dyskinesia, bladder dysfunction, enuresis.
Endogenous causes of the disease: diabetes mellitus, hormonal imbalance, metabolic diseases, renal failure and a number of other nosological forms lead to impaired renal functionality.
Classification of chronic pyelonephritis
The clinical classification of chronic pyelonephritis, adopted in the CIS countries, distinguishes the following forms of the disease:
- latent;
- recurrent;
- hypertensive;
- anemic;
- azotemic.
This division is conditional, since one patient may experience several leading syndromes. According to the course, chronic pyelonephritis is distinguished in the phase of exacerbation or remission. By localization - one-sided or two-sided.
The presence of complications - anemia, hypertension, chronic renal failure - suggests a complicated form of the disease. If there are disturbances in the outflow of urine from the diseased kidney during an exacerbation, abscesses may form. Renal shrinkage or total nephrosclerosis is the result of a long-term disease.
Course of the disease
The course of chronic kidney inflammation has 2 stages: exacerbations and remission.
The active course of the pathological process is characterized by the presence of bacteria and leukocytes in urine.
At the same time, a febrile syndrome occurs.
Against the background of complete clinical and laboratory remission (no symptoms for more than 6 months), changes in the blood and urine may not be detected.
According to the flow, the following forms of the disease are distinguished:
- Latent;
- Recurrent.
The latent stage is the onset of the disease, in which only urinary syndrome may appear. The recurrent course is manifested by remission and exacerbation. The last phase is characterized by the following symptoms:
- General intoxication;
- Pain syndrome;
- Urinary changes.
Symptoms of chronic pyelonephritis
The symptoms of chronic pyelonephritis during an exacerbation are similar to the clinical picture of the acute form of the disease with minor differences. Often the disease is disguised as other inflammatory processes of the urinary tract: cystitis, urethritis, attack of urolithiasis.
Only a detailed study reveals chronic pyelonephritis. Symptoms that occur during exacerbation can be divided into local and general.
Local:
- pain in the lower back and abdomen that occurs at rest;
- polyuria at the onset of the disease and oliguria when renal failure occurs;
- nocturia;
- dysuric phenomena (pain, burning during urination, increased urge to urinate).
Are common:
- weakness, fatigue;
- nausea, vomiting;
- lack of appetite;
- fever, slight increase in temperature, low-grade fever, chills;
- skin itching, headaches, change in skin color.
Itching, skin discoloration, anemia, and arterial hypertension occur in the presence of nephrosclerosis and chronic renal failure.
Often the disease is asymptomatic. The only way to identify the disease is to conduct a general urine test and a urine test according to Nechiporenko, Addis-Kakovsky. Unfortunately, clinical urine testing is often neglected by both doctors and patients. Asymptomatic bacteriuria and pyuria in such patients are the only signs to suspect chronic pyelonephritis. Symptoms of renal failure in such patients, arising against the background of apparent health, are the basis for a detailed examination that reveals the disease.
Medical therapy
It is necessary to treat the disease comprehensively, with the calculation of an individual algorithm of actions. Therapeutic tactics depend on the origin of the disease and the general condition of the patient. In this case, the characteristics of his body and accompanying pathologies are taken into account.
Standard treatment therapy includes:
- compliance with the drinking regime,
- following a diet
- drug effects,
- traditional medicine.
It is impossible to completely cure the chronic form of the disease. Properly selected treatment tactics and compliance with the doctor’s basic recommendations speed up the process of remission. During the period of exacerbation, the patient should be under the supervision of specialists in a hospital setting.
Drug effects
Drug therapy is based on the use of a wide range of drugs. To eliminate the pathogen, antibiotics and uroseptics are prescribed. Drugs are selected taking into account the individual characteristics of the human body. Most medications are highly toxic.
The main groups of antibiotics used include:
- penicillin series (Amoxicillin and Azlocillin). They have a wide spectrum of action,
- 2nd and 3rd generation cephalosporins (Suprax and Cedex). Taken by injection only in a hospital setting,
- fluoroquinolones (Ciprofloxacin and Norfloxacin). They are highly effective against most pathogens of infectious diseases,
- sulfonamide drugs (Biseptol). They eliminate infections and are used after testing the sensitivity of the microorganism.
In case of acute onset of the disease, it is advisable to use nitrofurans (Furadonin and Furamag) and hydroxyquinolines (Nitroxoline). The duration of therapy is determined by the doctor individually. The average duration of drug exposure is 14 days, this period can vary depending on the severity of the inflammatory process.
Surgery
Surgical intervention is appropriate in acute cases of the disease. The operation is performed when the functional purpose of an organ is lost, with the impossibility of its restoration. The main indications include: death of organ cells, replacement of healthy tissue with scar tissue and the development of complications.
The following types of surgical intervention are distinguished:
- resection (removal of part of an organ),
- nephrectomy (removal of the entire kidney or a separate part of it),
- nephroureterectomy (removal of malignant neoplasms).
The outcome of surgical intervention depends on the degree of organ damage. Before the operation, the patient must undergo preparatory measures in order to avoid complications during the operation. The person undergoes laboratory and instrumental tests, avoids taking medications and maintains proper nutrition.
Traditional treatment
Treatment with traditional methods must have scientific and medical justification. Therapy using non-traditional methods has a supportive effect on the body. It cannot be used as the main treatment strategy.
The main components of traditional methods are detoxification and herbal medicine. To speed up the elimination of pathogenic agents from the body, it is advisable to increase the amount of fluid consumed. For an adult, the norm is 3 liters. It is permissible to drink not only clean water, but also juices and fruit drinks. If the body temperature is elevated and there are signs of poisoning, it is advisable to take Regidron solution.
Herbal medicine is based on the use of medicinal herbs, in particular, bearberry, birch leaves, licorice, cornflower and corn silk. Additionally, Rosehip fruits are used (they have a diuretic effect) and Horsetail.
Laboratory research methods
Clinical urine analysis and its modifications according to Nechiporenko and Addis-Kakovsky are of leading importance in inflammatory kidney diseases. A general urine test, according to most doctors, does not have sufficient sensitivity for reliable diagnosis.
Urinalysis on Addis-Kakovsky is a microscopic examination of 24-hour urine sediment. The method allows for differential diagnosis between pyelonephritis and glomerulonephritis. It is quite difficult to differentiate these pathologies. The principle of the method is to collect 24-hour urine, followed by centrifugation and microscopy of the sediment. The predominance of leukocytes over erythrocytes indicates pyelonephritis, the predominance of erythrocytes indicates glomerulonephritis. Urine during collection should be stored at a temperature of + 8 degrees Celsius.
Urinalysis according to Nechiporenko allows you to detect low-grade inflammation in the kidneys. To do this, the average portion of morning urine is centrifuged, 1 ml of sediment is pipetted to the Goryaev chamber (used when calculating the leukoformula), for further counting of red blood cells, leukocytes and casts. More than 2000 leukocytes in men and more than 4000 in women in 1 ml of sediment indicates latent inflammation.
A urine test for leukocyte esterase (an enzyme found in leukocytes) is a modern method for diagnosing inflammatory diseases of the kidneys and urinary tract. Most leukocytes in the urine are destroyed, which is why they are not detected during analysis. However, leukocyte esterase is not degraded by the death of leukocytes and can be detected during analysis. Its presence in the urine is a marker of inflammation.
Urine culture with determination of sensitivity to antibiotics makes it possible to identify the pathogen and carry out treatment more effectively.
Diet for kidney disease
A diet for chronic kidney pyelonephritis is prescribed to correct metabolic disorders in the kidney tissue. In case of active disease, table No. 5 is recommended (according to Pevzner):
- Limiting salt;
- Increased drinking regime;
- Elimination of essential oils, fatty, spicy and fried foods
During convalescence, restriction of coffee, garlic, onions and spicy foods is required. A rich fluid regime is also recommended.
Prevention
Prevention of chronic pyelonephritis includes a set of procedures aimed at preventing infection of the kidney tissue. One of its main features is daily hygiene of the genitals.
Did you know that untreated inflammatory kidney diseases can lead to purulent and necrotic damage? Acute pyelonephritis: symptoms, pathogenesis, diet - you will learn what drug and surgical treatment is and how not to start the disease. It is very important to follow the recommendations for proper nutrition when treating pyelonephritis. This article is all about diets for various inflammatory diseases.
Instrumental diagnosis of chronic pyelonephritis
Ultrasound and excretory urography are mainly used to diagnose chronic pyelonephritis.
Characteristic signs of the disease on sonography are the following changes:
- reduction in kidney size, asymmetry compared to the intact side;
- atrophy and thinning of the medulla;
- compensatory hypertrophy of a healthy kidney or intact areas on the affected side;
- thinning and expansion of the pyelocaliceal system.
Excretory urography reveals similar changes in addition to signs of impaired urinary outflow. With severe vesicoureteral reflux, they lead to significant dilation of the ureters, which is an unfavorable sign. The effectiveness of conservative treatment in such patients is significantly reduced.
Radioisotope scanning is a sensitive method for detecting damage to the kidney parenchyma and foci of sclerosis. Defects in radiopharmaceutical accumulation correspond to areas replaced by connective tissue. The method allows you to estimate the amount of damage.
Diagnostics: modern methods
Laboratory analysis for chronic kidney pyelonephritis is carried out at the following intervals:
- In the remission stage - 2 times a year;
- In case of exacerbation - 1 time per week;
- When subsiding - once every 2 weeks;
- Intercurrent course - at the end and beginning of the disease.
Clinical and laboratory testing for chronic kidney inflammation also requires a biochemical blood test for C-reactive protein, fibrinogen, urea, and protein fractions:
- During remission - 2 times in 6 months;
- In case of exacerbation - once every 2 weeks;
- When it subsides - once every 2-3 weeks.
Urine tests are of great importance in diagnosing inflammation of the renal pyelocaliceal system . They are carried out at the following intervals:
- During remission – once every 3-4 months;
- During the acute stage – once every 1-2 weeks;
- If active – 1 time in 5 days;
- Intercurrent flow - single analysis.
Proteins in biochemical blood analysis
To determine the concentration ability of urine, tests according to Amburge and Nechiporenko are performed:
- During remission – once every six months;
- In case of exacerbation - severe leukocyturia;
- When it subsides - once every 10 days.
To determine the causative agent of inflammatory changes in the renal tissue, it is necessary to carry out an antibiogram and cultural cultures:
- During treatment - once;
- Before starting therapy - once;
- During remission - only if there are bacteria in the urine.
Determination of biochemical substances in urine (lipids, peroxide, ethanolamine, calcium salts, cystine, urates, oxalates, protein):
- In remission - according to indications;
- In the subsiding stage - with metabolic disorders;
- At maximum activity - once.
Determination of creatinine clearance and glomerular filtration rate
To determine the functional state of the kidneys, the following laboratory tests are performed:
- The Zimnitsky test determines the concentration properties of urine. It is carried out annually during remission;
- Determination of urea;
- Determination of creatinine clearance;
- Assessment of diuresis;
- Accounting for the volume and rhythm of urination.
Clinical and instrumental studies in chronic pyelonephritis:
- Ultrasound examination in a standing and lying position with a filled bladder. Repeated experiments once every 6 months. A pelvic ultrasound is performed at least once annually;
- Daily blood pressure monitoring to select therapy;
- Excretory urography (contrast study);
- Vaccination cystography – according to indications.
Are you worried about the frequent urge to urinate? The causes and symptoms of frequent urination may vary depending on the type of disease. Let's consider different forms of the disease - urgent, stressful and mixed. Read about inflammatory kidney diseases here.
And here you will learn about how the excretory urography procedure is performed. In what cases should this examination be carried out and are there any contraindications?
Treatment of chronic pyelonephritis
The basis of treatment of chronic pyelonephritis is antibacterial therapy. Drugs are selected taking into account the patient’s sensitivity to antibiotics, which increases the effectiveness of treatment.
Penicillin and cephalosporin drugs are used as first line. They have a pronounced bactericidal effect against gram-negative bacteria, most often causing chronic pyelonephritis. Treatment is carried out for 7-9 days and does not stop even with rapid improvement of the condition. Rational and correct antibacterial therapy prevents the development of drug resistance.
Fluoroquinolones (levofloxacin, ofloxacin) are an alternative to beta-lactams, are also excreted primarily by the kidneys, and have a bactericidal effect against a wide range of microbes. Uroseptics (furadonin, furagin, nitroxoline) can be used in combination with antibiotics. It is necessary to take into account the synergism of the prescribed drugs. Combinations of beta-lactams with macrolides and aminoglycosides should not be prescribed.
The choice of antibiotic should take into account the degree of kidney damage, since nephrotoxic drugs can impair the function of the excretory organs.
Experts believe that the presence of severe vesicoureteral reflux explains the low effectiveness of treatment and relapses. For this reason, surgical methods of therapy are also used. Surgical intervention on the urinary tract improves the prognosis and allows chronic pyelonephritis to be eliminated once and for all. Treatment in this way is carried out in patients with reflux of 4-5 degrees of severity with pronounced dilation of the ureters. In domestic practice, plastic surgery of the ureters and vesicoureteral segment is used.
In advanced cases, in the presence of severe nephrosclerosis, the kidney turns into a source of infection and loses its function. Antibacterial therapy does not make sense. Nephrectomy eliminates the risk of damage to the intact kidney.
Classification by patient groups
In addition to the traditional classification, doctors divide patients into groups. In each case, pyelonephritis is caused by its own causes and requires different treatment. Depending on the nature of the disease, the following groups of patients are distinguished:
Children, including newborns
To newborns, the disease is transmitted from the mother. Contributes to the disease - congenital reflux. In children, the disease can begin after suffering from a sore throat, influenza, ARVI, measles and other diseases.
Aged people
In old age, this disease is diagnosed more often in men than in women. This is due to impaired urodynamics due to prostate adenoma.
Pregnant women
Most often, the disease affects pregnant women, starting in the second trimester, when the uterus enlarges and puts more and more pressure on the kidneys and ureters. During pregnancy, the mother's immunity is weakened in order to bear a healthy child. This reduces resistance to pathogens.
Patients with diabetes mellitus
A quarter of patients with diabetes suffer from pyelonephritis. This is due to decreased immunity. The environment resulting from the disease is an excellent place for bacteria to multiply. Pyelonephritis in diabetics most often occurs hidden.
Treatment and prevention
In acute cases, hospital treatment is necessary. Patients are prescribed bed rest, drinking plenty of fluids, they should avoid hypothermia, and empty their bladder on time. The doctor prescribes antibiotics. Herbal preparations are also used for treatment. It is necessary to regularly visit a doctor, take urine and blood tests, so as not to miss the first symptoms of the disease. Be sure to reduce your salt intake. It is recommended to avoid spicy, fatty and fried foods.
To prevent the disease, it is necessary to eliminate possible sources of infection, consume sufficient amounts of vitamins, and perform an ultrasound of the kidneys and bladder.
Forecast
The prognosis largely depends on timely diagnosis and treatment. In such cases, it is generally possible to achieve remission. Failures are caused by the presence of urinary tract blocks (urolithiasis, strictures, chronic prostatitis), multidrug-resistant infection (nosocomial infection often leads to chronic pyelonephritis and is associated with instrumental studies of the urinary tract), severe vesicoureteral reflux.
Chronic renal failure is observed in 2% of patients with chronic pyelonephritis. In 8-10% of cases, the disease is complicated by severe anemia and hypertension.
Acute pyelonephritis
Lasts less than six months. The inflammatory process begins suddenly in the kidneys. Body temperature rises greatly. The person begins to shiver, nausea, vomiting, a feeling of weakness, and aching pain in the lumbar region appear. Intoxication of the body has a pronounced character. In the first stages of the disease, the content of nitrogen compounds in the blood exceeds the norm. Red blood cells, pus, protein are detected in the urine; the number of bacteria exceeds the norm. If you sharply touch the patient in the lumbar region, pain will appear (Pasternatsky's symptom).
Primary acute pyelonephritis
Occurs during the normal structure of the urinary system due to the penetration of pathogenic microbes into the kidneys. It is not complicated by disturbances in the functioning of other organs.
It is divided into serous, purulent and necrotizing papillitis. Purulent is divided into apostematous pyelonephritis, kidney carbuncle, kidney abscess.
Manifested by high fever, chills, severe sweating, nausea, vomiting, and a feeling of weakness. A dark coating appears on the tongue. The pulse rises.
Secondary acute pyelonephritis
It develops as a result of existing disturbances in the functioning of the body. Because of this, the kidneys are unable to resist the action of bacteria. The disease is associated with problems in the functioning of other organs. The cause of the disease is also anomalies in the structure of the urinary system.
Local symptoms are pronounced, making the disease easier to recognize and not to be confused with others. Often, abnormalities in the structure of the urinary tract are caused by urolithiasis. In women they occur during pregnancy. In men - due to prostate adenoma.
Diagnostics
The diagnosis of chronic pyelonephritis is made based on an analysis of complaints, the dynamics of their development, and symptoms. Without fail, the doctor checks Pasternatsky’s symptom - painful sensations when tapping in the kidney area, and pain when palpating the lower back is also characteristic.
Diagnosis of chronic pyelonephritis includes laboratory and instrumental examinations. Latent pyelonephritis is detected only by pathological changes in the urine.
In a general urine test for the disease, the following changes are determined:
- pyuria (presence of pus);
- bacteriuria;
- moderate amount of protein;
- microhematuria (admixture of blood).
Diagnosis of chronic pyelonephritis involves performing specific urine tests, for example, according to Nechiporenko or Addis-Kakovsky, which confirm the inflammatory process.
The latent course of pyelonephritis is revealed by special diagnostic tests - minimal doses of hormones are administered according to the scheme, then the number of active leukocytes in the urine is counted.
A general and biochemical blood test is performed. The following instrumental studies are prescribed:
- Ultrasound;
- excretory urography - to clarify the causes of urodynamic disturbances;
- angiography - shows a decrease in the number of arteries and their narrowing.
Prevention
Prevention of chronic pyelonephritis involves timely treatment of acute inflammation of the urinary tract.
If a person has suffered acute kidney inflammation, it is necessary to undergo an annual medical examination, even in the absence of signs of the disease. The development of chronic pyelonephritis can be prevented by promptly eliminating urogenital infections.
The following preventive measures are also needed:
- elimination of any infectious foci in the body;
- passing a general urine test 2 times a year;
- timely treatment of diseases leading to urinary tract obstruction.
To prevent chronicity, you need to follow a daily routine, eat well, and avoid overwork and stress. It is important to prevent hypothermia of the feet.
Chronic kidney pyelonephritis is a dangerous pathology that often occurs hidden and can lead to irreparable, life-threatening consequences. Therefore, when identifying any disease of the urinary system, it is so important to carefully follow all medical recommendations and be prepared for persistent and long-term treatment.
Author: Olga Shchepina, doctor, especially for Nefrologiya.pro
Treatment
The main medications for chronic pyelonephritis are antibiotics. Treatment of chronic pyelonephritis differs little from the treatment of the acute form, but is carried out regularly in courses. A regimen of 10-14 days of antibiotics per month is often used.
If signs of exacerbation occur, aggressive antimicrobial therapy is prescribed. The drugs are changed every 10 days under the control of urine tests.
New generation cephalosporins are now widely used: for example, Cefodox. The advantage of the medicine is that it can be taken orally, 1 tablet per day. Penicillin drugs, aminoglycosides, and fluoroquinolones are often used.
For treatment to be effective, the patient must maintain an active drinking regime - drink at least 2.5-3 liters of water per day.
The disease takes a long time to treat, using various means:
- uroseptics (Palin, 5-NOK);
- antispasmodics (No-shpa);
- diuretics (Furosemide);
- vascular agents (Nikospan);
- vitamins (Ascorbic acid, Milgamma);
- means for the prevention of dysbacteriosis (Lactobacterin).
Treatment of chronic pyelonephritis in women is always agreed with a gynecologist, since the presence of a urogenital infection is possible.
Surgical intervention is performed when conservative measures are ineffective - elimination of a stone or tumor, removal of a renal abscess. In advanced cases, the kidney is removed.