Author of the article
Arthur Viniaminovich Artemyev
Urologist, gynecologist, practicing specialist
Articles written
64
Contact the author
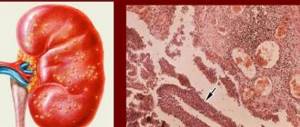
Acute glomerulonephritis is a kidney pathology that affects the structural parts of the nephrons. The disease most often develops in children between 2 and 10 years of age, with boys and men more susceptible to the disease.
Problems begin with the body's immune reaction to an allergy or with the occurrence of an infection; sometimes the disease occurs 1-2 weeks after a sore throat. High humidity and constantly low ambient temperature provoke a chronic nature of the disease.
The main effect is on the glomerular apparatus, renal corpuscles, with often occurring deviations in the structure of the tissue. The main danger is that the disease in some cases proceeds without noticeable external changes.
Pathogenesis of acute glomerulonephritis
The disease is reflected in the official medical classifier under the ICD 10 code and has its own characteristic signs and specific development.
The pathology manifests itself spontaneously, progresses quickly, but most often can be completely cured. Less commonly, complications arise that become chronic.
The patient’s priority problems are associated with the entry of b-hemolytic streptococcus into the body; its antigens come into contact with the immune system and force the production of antibodies, which are necessary to combat harmful microflora. However, streptococcal antibodies, adapting to the structure of their normal counterparts, gradually replace them and attack not only pathogenic microorganisms, but also healthy organs, thereby provoking the occurrence of foci of inflammation, gradually affecting the entire capillary system.
It turns out that streptococcus itself does not disrupt the functioning of the kidneys; everything happens due to the improper functioning of antibodies that destroy kidney tissue. Pathogenesis can also proceed differently: after excessive antigenic stimulation, the immune system experiences overload, which leads to damage to the renal glomeruli.
Important! Acute post-streptococcal glomerulonephritis is considered the most dangerous.
Symptoms
The classic picture of pathology is represented by three syndromes (symptom complexes):
- renal (kidney);
- extrarenal - hypertensive and edematous.
The development of the disease begins after one or two weeks after the action of one or another etiological factor - an infectious disease, hypersensitivity reaction and other provocateurs.
- The earliest sign of the acute form is the appearance of edema. In half of the situations, swelling is significant. The localization of swelling is in the face, it is more pronounced in the morning, and in the daytime the ankles and legs swell. Edema syndrome can develop to conditions such as hydroperitoneum, hydropericardium, hydrothorax, and widespread edema (anasarca). Visually noticeable swelling is not a mandatory symptom, but fluid retention is confirmed by an increase in body weight.
- Hypertension manifests itself moderately: in approximately 2⁄3 patients the pressure level is no more than 160/100 mmHg. Art. But you need to understand that prolonged persistent hypertension in the future gives a negative prognosis. In the case of acute damage to the glomeruli, hypertension is combined with a decrease (heart rate less than 60 beats per minute). It lasts for one or two weeks.
- When hypovolemia develops acutely, progression of left ventricular failure cannot be ruled out. Clinically, this is expressed in the form of pulmonary edema and cardiac asthma.
- Inflammation of the glomerular apparatus can be accompanied by pain of varying intensity. More often symmetrical pain occurs in the lumbar region. They arise as a result of overstretching of the kidney capsules and disturbances in urodynamic processes.
- The urinary syndrome of this pathology involves the early manifestation of oliguria, and in other situations, anuria. At the same time, there is pronounced thirst.
- The relative density of urine increases, and cylinders of hyaline and granular types begin to appear in it. Erythrocyturia (micro- or macrohematuria) and proteinuria are noted. In the case of gross hematuria, urine becomes the color of “meat slop.” Hematuria and proteinuria are especially intense on the first day of disease progression.
Quite often, cerebral disorders progress, which arise due to swelling of the brain. The list of manifestations includes:
- headache;
- vomiting and nausea;
- deterioration of visual function;
- the appearance of a “veil” before the eyes;
- deterioration of auditory perception;
- disturbances of psychomotor excitability.
The most severe manifestation of cerebral syndrome is eclampsia (angiospastic encephalopathy). It includes tonic-clonic convulsions, disturbances of consciousness, cyanosis of the facial and cervical area, swelling of the neck veins, decreased pulse rate and other symptoms.
In rare situations, the pathology progresses in a monosidromic form, which includes isolated urinary syndrome. There is no swelling and acceptable blood pressure levels are maintained.
How the disease progresses: causes, symptoms, stages of development
In addition to streptococcal infection, there are other prerequisites due to which the normal functioning of the kidneys is disrupted and subacute or acute form of glomerulonephritis is formed.
Other reasons include the following:
- genetic predisposition;
- viruses;
- joint diseases;
- respiratory problems;
- constant use of alcohol;
- parasitic infestations;
- oncology;
- frequent hypothermia;
- late toxicosis during pregnancy;
- allergy;
- poor quality vaccination;
- stress and overexertion.
Methodological guidelines of the department / Nephrology / 02 Acute and chronic glomerulonephritis
9
heart disease, shortness of breath during exercise, decreased vision) or edema syndrome (decreased urine output, the appearance of edema of varying severity). Changes in the color of urine are rarely noted by patients.
During a physical examination, depending on the severity of arterial hypertension, a lateral displacement of the left border of the heart is noted, the apical impulse is strengthened and also displaced, an accent of the second tone is heard in the second intercostal space to the right of the sternum, and a systolic murmur may also be heard. Blood pressure fluctuates within a wide range; its increase can be stable or transient. Swelling with CGN is not detected in all patients and is localized on the face, lower extremities or throughout the body. In cases where CGN is part of some other disease, corresponding signs can be identified (for example, infective endocarditis, SLE, etc.).
When examining urine, proteinuria is typical for patients with CGN, which can vary depending on the clinical variant of the disease (in this regard, it is extremely important to determine the protein content in daily urine). The dynamics of urinary sediment is characteristic: hematuria is expressed to varying degrees and rarely reaches the level of gross hematuria. Cylindruria is detected, as a rule, in patients with great constancy.
When examining blood during an exacerbation of glomerulonephritis in some patients, acute-phase indicators are recorded (increased ESR, hyper-γ-globulinemia, increased fibrinogen content, appearance of SRV). In a biochemical blood test, the limits of fluctuations in individual indicators (cholesterol, triglycerides, total protein and its fractions) are very significant and are determined by the clinical variant of CGN. The level of nitrogenous wastes (creatinine, urea, total nitrogen), as well as the amount of glomerular filtration, depend on the functional state of the kidneys.
X-ray examination of patients with arterial hypertension reveals an enlargement of the left ventricle, and if it persists for a long time, an expansion of the ascending aorta due to the development of atherosclerosis. An ECG in the presence of arterial hypertension shows left ventricular hypertrophy syndrome, expressed to varying degrees. When examining the fundus, vascular changes caused by arterial hypertension are detected.
Classification of CGN: the issue of classification is complex. In world practice, the classification is based on the complete morphological picture of GN, which requires a mandatory puncture biopsy of the kidney. This approach is quite legitimate, but for Russia, where only a few nephrological centers perform kidney biopsies and, moreover, not all of these centers have qualified (nephrologically) morphologists, it often turns out to be unacceptable. Therefore, the clinical classification is put to the fore, in which the following variants of GN are highlighted (slightly modified classification by E.M. Tareev): latent, hematuric, nephrotic, hypertensive and mixed.
Clinical variants of CGN:
Latent GN is the most common form of chronic GN, manifested only by changes in urine (proteinuria up to 3 g/day, slight erythrocyturia), sometimes slightly increased blood pressure. The course is usually slowly progressive, the prognosis is better with isolated proteinuria, worse with a combination of proteinuria with erythrocyturia, 10-year survival rate is 85-70%.
Hematuric GN makes up 6-8% of cases of chronic GN, manifests itself as constant hematuria, sometimes with episodes of gross hematuria, the course is quite favorable.
no. One of the forms of hematuric GN is IgA nephropathy.
Nephrotic GN (10-20% of cases of chronic GN) occurs, as the name suggests, with nephrotic syndrome (proteinuria above 3.5 g/day, hypoproteinemia, edema, hypercholesterolemia). Nephrotic syndrome is usually recurrent in nature, less often it has a persistent course with gradual addition of arterial
Diagnosis of the disease
Before making an accurate diagnosis, the doctor interviews, examines the patient and conducts additional examination.
Priority methods:
- A general urine test is prescribed, color and composition are assessed. Based on these data, the presence or absence of the inflammatory process is determined. If the amount of protein deviates from the norm, observation is carried out for a week with repeated tests over time. The color of urine is usually cloudy;
- a serological blood test is performed to detect an increase in the titer of streptococcal antibodies;
- Ultrasound;
- kidney biopsy.
In acute glomerulonephritis, urine has a pink to red color or the appearance of burgundy meat streaks.
If the symptoms appear 1-3 weeks after the infection enters the body, we are talking about an acute course of the disease; if the interval is calculated in days, this is a chronic case.
Multicomponent treatment regimens for the disease
Treatment of glomerulonephritis is carried out using three regimens:
- Ponticelli scheme - in this case, pulse therapy is carried out with Prednisolone 1 thousand mg per day. It is carried out for 3 days, after which the remaining 27 days are 30 mg per day. Prednisolone must be changed periodically with a cytostatic agent. Then, over the next month, Chlorambucil 0.2 mg.
- Steinberg's scheme - it involves the following procedure: once a month for a year, intravenously administer drugs such as Cyclophosphamide 1 thousand mg. Then, for two years you need to take the drug once every 3 months, and for the next two years - once every 6 months.
- Four-component scheme. Prednisolone 30 mg per day for 60 days. Gradually it is necessary to give the body a rest. Cytostatic is prescribed until target remission. Heparin 5 thousand units. 4 times a day for a month. Gradually replace with Asperin. Dipyridamole 400 mg. This method is perfect for rapidly progressing glomerulonephritis.
Therapy is quite a complex process for many forms. As a result, people who are still carrying out their work activities develop disabilities. It is very important to monitor the patient during recovery and while in the clinic.
Treatment of acute glomerulonephritis
Both forms of the disease: acute and chronic are treated in the same way according to the standard regimen, using complex therapy.
It is directed:
- to stop the rate of development of renal failure;
- restoration of normal kidney function.
There are 4 approaches to treating the disease:
- etiotropic treatment - antibiotics of the penicillin group are prescribed in the form of injections;
- pathogenetic – concerns the mechanism of treatment;
- the use of glucocorticoids to relieve inflammation and suppress pathologies of the immune system;
- cytostatics - if the body does not sufficiently accept glucocorticoids or there are individual characteristics in which serious side effects occur when taking the latter.
Acute glomerulonephritis in children clinical guidelines
In children, treatment is carried out with similar drugs, but without the use of hormones; the difference lies in the dosage and the choice of more gentle drugs. Whenever possible, doctors try to make do with minimal use of medications, paying more attention to folk remedies and diets.
ethnoscience
Treatment of the disease occurs in several stages. In parallel with drug therapy, treatment with folk remedies is recommended. The folk remedy is used during the recovery period or for chronic glomerulonephritis. With the help of herbal medicine, patients can achieve the following effects:
- diuretic;
- anti-inflammatory;
- anticoagulant;
- antiallergic.
According to the recommendations of doctors, therapy using traditional medicine involves the correct selection of the combination and dosage of natural phytocomponents.
The result will be the necessary tonic and diuretic effect. Herbal treatment helps reduce the burden of drugs on the human body. Source
Diet
Acute glomerulonephritis is a serious diagnosis, which, in addition to drug therapy, requires support from proper nutrition. Doctors recommend reducing salt and liquid intake as much as possible and adhering to a special list of products from diet No. 7A.
| It is forbidden | Can |
| Alcohol | Poultry and lean beef |
| Spicy seasonings and products | Vegetable soups, steamed vegetables |
| Canned foods | Fruits |
| Strong tea/coffee | Herbal tea (medicinal pharmacy) |
| Concentrated meat/fish broths | Cottage cheese, fermented milk products |
| Roast | Lean fish |
| Egg whites |
Important! All food should be either boiled or steamed. Doctors note that dogwood helps to cope well with the disease.
Glomerulonephritis and pregnancy
Mostly pregnant women experience glomerulonephritis in its acute form. The causes that provoke this disease are the same factors that accompany the standard forms of its course, while the main reason in pregnant women is the development of the disease against the background of a chronic infection of the ENT organs and throat, which were not cured before pregnancy.
As the main method for determining the possibility of diagnosing glomerulonephritis during pregnancy, a general urine test is used, the results of which, if the disease is relevant, determine the presence of an increased level of protein in its content. A blood test can determine in this case an increased content of red blood cells.
Glomerulonephritis, in combination with complications accompanying it (for example, in the form of high blood pressure), often significantly complicates the course of pregnancy. Taking this into account, some cases require (albeit extremely rarely) termination of pregnancy, designed to save the life of a mother with a current diagnosis of glomerulonephritis. When treating this disease during pregnancy, the following actions are taken into account:
- the use of antibiotics acceptable during pregnancy, used to suppress infection;
- determining appropriate therapy to eliminate swelling and stabilize high blood pressure;
- implementation of appropriate measures aimed at maintaining the inherent functions of the kidneys until their complete restoration.
Recommendations
Acute glomerulonephritis is a common phenomenon that requires a long time and certain conditions for treatment. Doctors often say that any disease is easier to prevent, and therefore it is better to carry out treatment at the initial stage or avoid it altogether by observing preventive measures.
Clinical recommendations for prevention:
- promptly identify and treat common acute respiratory viral infections, etc.
- engage in intensive allergy treatment;
- carefully monitor the body’s reaction after all vaccinations;
- monitor the quality of food;
- eliminate bad habits;
- do not overcool;
- to live an active lifestyle.
Drug therapy
Now we can talk about what medications need to be taken to eliminate symptoms and treat glomerulonephritis in adults.
As a rule, doctors prescribe the following medications:
- Wobenzym. An immunomodulatory and anti-inflammatory agent, which is based on enzymes (protein molecules) of animal and plant origin. Taking this drug is aimed at reducing the number of immune complexes in the body, normalizing the permeability of vascular walls and regulating the adhesion of blood cells.
- "Canephron N". This is a herbal medicine, a diuretic of plant origin. It has several effects at once - antimicrobial, diuretic, anti-inflammatory and antispasmodic.
- "Metypred." A glucocorticosteroid of synthetic origin that has immunosuppressive, antiallergic and anti-inflammatory effects. The drug also reduces the amount of globulins in plasma, increases albumin synthesis in the kidneys and liver, normalizes carbohydrate metabolism, and increases the resistance of the cell membrane to various damaging factors.
Of course, this is not the entire list of drugs indicated for use. However, it should be noted that therapy can only be prescribed by a nephrologist, who is involved in the treatment of glomerulonephritis.
The doctor’s clinical recommendations are based on diagnostic results and therefore do not raise doubts. But self-medication and the decision to prescribe any medications on your own can be fraught with complications and the emergence of other health problems.
Causes
Pathogenesis
In typical cases, acute glomerulonephritis occurs cyclically with a successive change of three periods and is manifested by nephritic syndrome, including extrarenal (edema, increased blood pressure, changes in the heart and central nervous system) and renal (oliguria, hematuria, proteinuria, cylindruria) symptoms.
After about 1.5 - 2 months. (sometimes later) urine parameters return to normal. A period of complete clinical and laboratory remission begins. However, complete recovery, taking into account the involution of morphological changes in the kidneys, occurs much later - after 12 years. If individual clinical symptoms persist for more than 6 months, they speak of a protracted course of acute glomerulonephritis; the duration of symptoms for more than 1 year indicates a transition to chronic nephritis.
The most common complication is eclampsia (angiospastic encephalopathy), caused by cerebral vasospasm and edema. Eclampsia is manifested by tonic-clonic convulsions that occur after a short period of precursors (headache, nausea, vomiting, visual impairment). The attack resembles an epileptic seizure and is always accompanied by an increase in blood pressure. During a seizure, there is no consciousness, the skin and mucous membranes become cyanotic, breathing becomes uneven, wheezing, foam appears at the mouth, and involuntary urination occurs. The attack lasts several minutes, sometimes a series of attacks is observed. In the absence of timely adequate treatment, death from hemorrhage in the brain is possible.
Acute cardiovascular failure in children occurs rarely. The symptoms with which it is characterized: a sharp increase in the size of the liver, an increase in peripheral edema and the clinical picture of pulmonary edema (usually it causes the death of the patient).
Disease history
Glomerulonephritis is a disease that affects two kidneys at once. Most often this disease is autoimmune in origin . When the disease appears, the glomeruli and tissues in the kidneys are damaged.
This means that the organs can no longer function in the correct mode, which leads to disturbances throughout the body.
The function of the kidneys is to filter blood and form urine, but when one of its elements becomes inflamed, then a malfunction occurs that is felt throughout the human body.
Most often, the disease occurs in people under the age of forty. In terms of frequency, this disease ranks third among all diseases affecting the kidneys. According to statistics, men are three times more likely to suffer from glomerulonephritis than women.
In children, the disease occurs frequently and in many cases leads to disability if treatment is not started in time. In advanced cases, the disease leads to kidney failure.
Therefore, it is important to pay attention to the main symptoms in time and urgently take measures to contact a qualified specialist.
Experts say that in recent years the number of people exposed to this disease has been growing and this is explained by the fact that the environmental situation around the world is worsening, and the population’s immunity is decreasing , which in most cases comes from an unhealthy lifestyle and poor nutrition.
If you do not pay attention to the symptoms in time and do not start treatment, then diffuse glomerulonephritis can lead to the following complications:
- acute heart failure (in cases less than three percent);
- intracerebral hemorrhage;
- visual impairment;
- chronic diffuse glomeruloneritis;
- eclampsia or preeclampsia;
- acute renal failure (observed in approximately one percent of such cases).
About pathogenesis (development process)
Let's turn to anatomy. Special structural units – nephrons – help the kidneys provide the main urinary function. The structure of nephrons is represented by tubules, capsule and glomerulus (glomerulus). When glomeruli are damaged by pathological agents, inflammation—glomerulonephritis—occurs.
The human immune system responds to the introduction of foreign substances by producing antibodies. In the process of struggle between aggressors-antigens and defenders-antibodies, the structure of the capillary network of the renal glomeruli suffers. As a result, the blood supply to the kidneys is disrupted, leading to a general malfunction of the urinary apparatus.
The inflammatory process can affect from 80 to 100% of the glomerular system. The picture of the disease is reflected in clinical signs.