Pyelonephritis is an inflammatory lesion of the pyelocaliceal apparatus of the kidneys, in which the clinical picture includes pain, signs of general intoxication, and urination disorders.
In 80% of cases, the diagnosed pathology is infectious in nature. In the absence of proper treatment, the acute form of pyelonephritis becomes chronic, requiring long-term complex therapy.
For chronic pyelonephritis, clinical recommendations are a kind of guideline for urological doctors. They help create an integrated approach to the diagnosis, treatment and prevention of this pathological condition.
Taking into account world statistics, at least 20% of the world's population suffers from a chronic form of pyelonephritis. This condition can be of a primary or secondary nature.
Primary chronic pyelonephritis develops as an independent disease, under the influence of internal or external negative factors. Secondary chronic pyelonephritis is a consequence of incorrectly treated or undertreated acute inflammatory process in the kidney area.
Description and forms
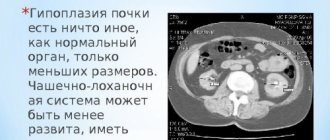
Pyelonephritis is an inflammatory disease that affects the renal tissue and pyelocaliceal system (PCS). The cause of the disease is the development of an infection that successively affects the parenchyma, then the calyx and pelvis of the organ. Infection can also develop simultaneously in the parenchyma and the CLS.
In the vast majority of cases, the causative agents are Escherichia coli, streptococcus, staphylococcus, and less commonly Klebsiella, Enterobacter, Enterococcus and others.
Depending on the effect on the process of urination, inflammation can be primary and secondary. In the primary form, urodynamic disturbances are not observed. In the Tuesday form, the process of formation and excretion of urine is disrupted. The causes of the latter type can be pathologies of the formation of the organs of the urinary system, urolithiasis, inflammatory diseases of the genitourinary organs, benign and malignant tumor formations.
Depending on the location of the inflammatory process in the kidneys, the disease can be unilateral (left- or right-sided) or bilateral.
Depending on the form of manifestation, pyelonephritis occurs acutely and chronically. The first develops rapidly as a result of the proliferation of bacterial flora in the organ. The chronic form is manifested by a long course of symptoms of acute pyelonephritis or its multiple relapses during the year.
Recommendations for adults
The types of infectious diseases in adults are identical to those for children, while preventive measures are aimed at normalizing kidney function and preventing relapses.
The types of infectious diseases in adults are identical to children, while preventive measures are aimed at normalizing kidney function and preventing relapses. If acute or chronic pyelonephritis develops, the following recommendations must be followed:
- hygiene of the external genitalia: proper washing in women (from front to back due to the anatomical proximity of the exit channels and the possibility of infection, infection with ascending pyelonephritis);
- maintaining optimal body temperature balance: warm feet, warm clothes, but without excessive overheating;
- no hypothermia;
- timely emptying of the bladder;
- maintaining a physical activity regime without overload: normal activity is only beneficial, as it normalizes metabolic processes and restores the body’s water balance;
- swimming at a water temperature below +21 C is prohibited, overheating in the bathhouse/sauna is prohibited, taking a contrast shower is prohibited;
- compliance with diet therapy with abstinence from alcohol, spicy and fatty foods (basic detailed nutritional recommendations will be given by a specialist observing the patient);
- compliance with the drinking regime in sufficient quantities (but only without the presence of cardiovascular and other pathologies);
- fasting no more than once a week for 1-2 days with the use of immunostimulating agents (consultation with a doctor is required in advance, as active protein breakdown occurs and waste products are removed by the kidneys, which is not always useful for inflammatory processes in the filtration organs);
- compliance with therapeutic methods of treatment after suffering from seasonal colds (drugs indicated for complete cure should be taken in full course);
- Avoid working in hot workshops that involve inhaling gasoline fumes, heavy metal salts and heavy physical exertion.
Important! Chronic pyelonephritis allows for treatment at home with normal body temperature, absence of nausea, vomiting, acute local or widespread pain. Therapeutic drugs in the form of antibiotics and uroseptics are used in full, the diet and regimen are followed.
As a rule, the course of therapy lasts no more than 14-21 days. In acute cases of pathology, the patient must be hospitalized and be kept in bed. It’s a good idea to take herbal remedies once every six months to prevent exacerbations. The type and volume of the course will be determined by the attending doctor.
Diagnostics
Pyelonephritis is accompanied by a feeling of pain in the lower back, fever and changes in the physicochemical properties of urine. In some cases, with inflammation of the kidneys, feelings of fatigue and weakness, headaches, disorders of the digestive tract, and thirst may be present. Pyelonephritis in children is accompanied by increased excitability, tearfulness and irritability.
During diagnostic measures, the doctor must determine what led to the development of the inflammatory process in the kidneys. For this purpose, a survey is conducted to determine the presence of chronic diseases, inflammatory diseases of the urinary system in the past, anomalies in the structure of the organs of the urinary system and disorders in the functioning of the endocrine system, and immunodeficiency.
Recommendations from pediatric nephrologists and urologists
Consultation with pediatric specialists is necessary at the first signs of leukocyturia or primary dysuritic disorders.
The prevalence of pyelonephritis in children is more than 18%. The frequency of manifestation of the pathology depends on the age and gender of the patient; children in the first year of life are most often affected. For infants, UTI is one of the most severe infectious pathologies, observed in 10-15% of cases.
Symptoms of drug-induced kidney damage and treatment
Important! Until the age of 3 months, UTIs are more common in boys, then the pathology more often develops in girls. After the first illness, the risk of relapse increases with a frequency: in girls from 30% within 12 months after the first episode, in boys 15-20% within 12 months after the first episode.
Consultation with pediatric specialists is necessary at the first signs of leukocyturia or primary dysuritic disorders (inability to urinate with a clear desire, pain during urination, decreased volume of daily urine, change in smell, color of urine, etc.). The cause of the pathology may be local inflammation of the genitals or the presence of phimosis.
Important! In acute forms of the disease, children may not experience damage to the upper respiratory tract even during nephropathic fever. In the first 12 months of a child’s life, an ultrasound examination of the kidneys and bladder is mandatory to eliminate the threat of developing pathology.
Primary prevention of childhood pyelonephritis according to the clinical recommendations of specialists includes the following points:
- regular (do not tolerate) emptying the bladder and bowels;
- compliance with the drinking regime;
- body hygiene.
Rehabilitation activities for children include:
Causes of prolapsed kidney: symptoms and treatment
- regular examinations if episodes of infection recur;
- in the first 90 days after an exacerbation of chronic pyelonephritis or during the course of acute pathology, collecting clinical urine samples once every 10 days, for 3 years once a month, then once a quarter;
- analysis of urine culture for leukocyturia is carried out with unmotivated rises in temperature;
- Ultrasound of the kidneys once a year;
- instrumental examination once every 2 years.
The prognosis for complete cure for pyelonephritis in children is positive. Active diagnosis and early treatment reduces the risk of focal organ shrinkage to 10-12% (in the presence of relapses and refluxes); cicatricial changes do not exceed 24% in children and 13% in children under 14 years of age.
Treatment recommendations
Treatment should be aimed at eliminating the source of the disease, preventing complications and relapses.
In acute primary pyelonephritis, treatment is carried out on an outpatient basis using antibacterial agents. Treatment in a hospital setting is carried out according to indications or in the absence of effect from the drugs used.
Hospitalization is necessary for patients with secondary inflammation, which can lead to serious complications as a result of poisoning the body with toxic compounds.
Gestational pyelonephritis in pregnant women - tips and recommendations on News4Health.ru
Urology (Latin urina - urine, logos - science) is a field of medicine that diagnoses and treats diseases of the kidneys, bladder and urinary tract. In urology, nephrology is additionally distinguished, which more narrowly specializes in kidney pathology. Previously, urology also dealt with diseases of the male reproductive system. Nowadays, this direction in medicine has become a separate science - andrology. And although a urologist still often combines the functions of an andrologist, these two specializations are gradually being separated. Also in urology there are such narrow areas as urogynecology, pediatric urology, geriatric urology, oncourology, phthisiurology.
The development of diseases in urology is often facilitated by such unfavorable factors as hypothermia, infections, STDs, addiction to alcohol, abuse of spices, spicy and smoked foods. Diagnostics in urology is based on the use of a complex of radiological, tomographic, endoscopic, ultrasound, laboratory, electrophysiological, urodynamic studies, and diagnostic operations.
The priority area of urology is the treatment of pathologies of the urinary organs, urinary excretion and the associated reproductive system in men and women. Practical assistance in urology is provided by urologists, nephrologists, urologists-andrologists, urogynecologists, and urological oncologists.
Urology is largely a surgical field, but it also uses conservative treatment methods. Treatment of acute and chronic inflammatory diseases (cystitis, pyelonephritis, glomerulonephritis, urethritis), and urolithiasis is carried out through courses of drug treatment. Medicines used in urology include: antibacterial, anti-inflammatory, antispasmodics, corticosteroids, diuretics, antihypertensives, anticoagulants and antiplatelet agents. For cystitis and urethritis, drug therapy in urology is often combined with physiotherapy and local treatment (bladder lavage, urethral dilation, etc.)
In urology, many diseases and developmental anomalies of the urinary system require surgical treatment. Modern development of technology and medical instruments allows surgeons to perform operations using less traumatic methods and with a lower risk of complications. For example, various methods of crushing stones (lithotripsy) make it possible to remove them with minimal risk of damage to the urinary tract. And thanks to a special shock wave apparatus, it became possible to destroy stones without surgical intervention - remote lithotripsy.
Today, endoscopic surgical interventions are most common in urology. These are so-called transurethral operations, which are performed through the urethra using an endoscope. They allow removal of stones, cysts and neoplasms of the ureters, bladder, and urethra using an endosurgical method and do not require an incision of the skin and underlying tissues for surgical access.
With the help of endoscopes in urology, laparoscopic and retroperitoneoscopic operations are performed, during which interventions are carried out under video control through mini-incisions in the anterior abdominal wall or in the lumbar region. In this way, kidney resection, removal of neoplasms, stones, cysts of the kidneys and ureters, and operations to form anastomoses are performed.
In urology, most previously developed surgical operations are now performed using a laparoscope and microsurgical instruments. The use of a surgical microscope and microsurgical instruments in urology allows the surgeon to perform the operation more accurately, with less damage to healthy tissue and restoration of even small blood vessels and nerve bundles. All this helps to reduce blood loss during surgery, significantly reduce the likelihood of developing postoperative complications, and speed up the patient’s recovery.
Urological care in Moscow
The direction of urology in Moscow is represented by specialized departments of multidisciplinary clinics and specialized centers. Urology in Moscow offers consultations with leading specialists with extensive practical experience, an attentive approach to each client, examination using modern diagnostic equipment, and the use of traditional and unique methods for treating urological diseases.
Contacting a urology clinic in Moscow is recommended for pain in the abdomen or lower back, frequent and painful urination, the appearance of blood or pus in the urine, changes in the color of urine, increased body temperature, and deterioration in general well-being. In addition, preventive annual examinations by specialists in the field of urology in Moscow should be the norm for men and women who monitor their health.
Urology in Moscow deals with the treatment of urethritis, cystitis, pyelonephritis, glomerulonephritis, urolithiasis, renal failure, urinary incontinence, urinary fistulas, urethral strictures, nephroptosis, kidney cysts, developmental anomalies and tumor lesions of the urinary system. Urology in Moscow works closely with andrology, gynecology, venereology, sexology, and oncology. Many urology clinics in Moscow offer comprehensive urological programs for men's and women's health, which make it possible to prevent or promptly detect many diseases of the genitourinary tract.
The consequences of diseases in urology can be catastrophically dangerous, so treatment of urological diseases must be addressed at the earliest stages. Urology clinics in Moscow work to solve all problems that arise in a timely manner and in the shortest possible time. Modern urology in Moscow continues to improve diagnostic methods and treatment methods, taking into account new advances in the field of medical technology and pharmacology. But we must not forget that in urology, as in other areas of medicine, the effectiveness of treatment largely depends on the disease itself, the timeliness of its treatment, the presence of concomitant pathology and the psychological mood of the patient. Adequate adjustment of prescriptions during treatment, correct surgical technique, and patient compliance with all recommendations of the attending physician are important for successful treatment in urology.
Specialists in the field of urology in Moscow warn: advanced cases of urological diseases, as well as diseases complicated by self-medication, may require lengthy and expensive correction and are not always completely curable, despite the use of the most modern techniques.
The main methods of treating pyelonephritis during pregnancy
Treatment of inflammatory diseases in the pelvicalyceal system is a rather lengthy and labor-intensive process, which is largely complicated by the fact that most standard medications are prohibited from being taken during pregnancy. Strong emphasis is placed on traditional medicine and herbal medicine. Changing your eating style and drinking regime also has a beneficial effect on a woman’s health.
Important principles of treatment for pyelonephritis during pregnancy:
- reduction of pain syndrome;
- normalization of blood pressure;
- stimulation of immune system cell activity;
- removing excess fluid from the body;
- restoration of water-salt and acid-base balance;
- no negative effect on the fetus;
- destruction of the bacterial pathogen that provoked the infection.
Medications to treat illness
During pregnancy, the mother's body perceives many substances as foreign components. They can also seriously affect the development of a small person, disrupting the maturation of his organs and tissues. Most often, the nervous, endocrine, and respiratory systems suffer from the use of medications, and external deformities and deformations of the facial skull also appear.
In the practice of the author of this article, there were clinical cases where women independently prescribed and discontinued antimicrobial drugs. Unfortunately, in the vast majority of cases, children were born with serious impairments of hearing, vision, and smell; there was a deep cleft palate or non-closure of holes in the atrial septum, which led to disruption of normal blood flow.
The best way to combat the causative agents of pyelonephritis are antibiotics: they kill pathogenic microflora, preventing further reproduction and development of the microbe in the body's cells. When using these groups of drugs there is no toxic effect on the baby:
- Penicillinins: Benzylpenicillin sodium and potassium salt, Bicillin-1, Bicillin-5, Oxacillin, Ampicillin, Ampiox, Flemoxin, Dicloxacillin, Azlocillin.
- Cephalosporins: Cephalexin, Cefazolin, Cefaclor, Cefuroxime, Cefpirome, Cefepime, Cephobid, Rocefin, Fortum, Claforan, Ceclor, Vercef, Keflex, Zinnat, Zinacef.
- Macrolides: Erythromycin, Roxithromycin, Clarithromycin, Midecamycin, Macropen, Klacid, Rulide, Oleandomycin phosphate, Lincomycin.
Other groups of drugs used to treat the disease:
- Herbal remedies that gently remove excess fluid, toxins and waste from the body. These include Canephron, Cyston, Phytolysin, and pharmaceutically prepared kidney preparations.
- Antihypertensive drugs are used to reduce arterial hypertension and reduce blood pressure to normal levels. In obstetrics and gynecology, Verapamil, Diltiazem, Labetalol, Norvasc, Captopril, Enalapril are used.
- Stimulants of the immune system help activate the body's internal reserves and direct the forces of cells to fight the infectious agent. The most commonly used are Timalin, Timogen, Taktivin, Cycloferon and human immunoglobulin preparations.
- Diuretics should include Urea, Mannitol, Triamterene, Indapamide, as well as any mineral waters and fruit and vegetable juices.
Photo gallery: antibiotics and other drugs used to treat pyelonephritis
Ampicillin is well tolerated during pregnancy
Ceftriaxone must be dissolved in novocaine
Erythromycin helps remove microorganisms
Canephron has anti-inflammatory, antispasmodic, antiseptic and diuretic effects
Captopril is used to treat hypertension
Indapamide removes excess water from the body and lowers blood pressure
Dietary recommendations for pyelonephritis
The nutritional culture of pregnant women is a separate science, the basics of which must be learned at school for expectant mothers. It is worth noting that if the renal pyelocaliceal system is inflamed, you will have to give up your usual eating style. All dishes must be baked, boiled or stewed: fried, smoked and dried delicacies must be excluded from the diet. The number of meals during the day is at least five: breakfast, lunch, dinner, several hearty and healthy snacks. It is also necessary to maintain a drinking regime, drinking at least two liters of clean water per day.
Possible breakfast options:
- porridge with water or milk (rice, oatmeal, rolled oatmeal, buckwheat, millet) with the addition of berries, honey or nuts;
- cottage cheese of at least five percent fat content with sour cream;
- plain yogurt and bread with cheese and butter.
Recommended lunch menu:
- soup (pea, chicken, mushroom, solyanka, borscht, cabbage soup, cream, cheese, puree) with several slices of whole grain bread;
- stewed vegetables in their own juice;
- fish, meat plate.
What to eat for dinner:
- durum pasta with goulash;
- boiled potatoes with chicken breast;
- baked vegetables or turkey stew;
- salmon with buckwheat porridge.
Recommended snack foods:
- yogurt, cottage cheese, kefir, fermented baked milk;
- fresh fruits;
- nuts;
- muesli;
- bitter chocolate.
What is strictly prohibited to consume during pyelonephritis:
- chips, crackers;
- fast food;
- carbonated drinks;
- any alcohol;
- semi-finished products;
- custard noodles;
- industrial sweets;
- black coffee.
Photo gallery: products not recommended for consumption
Fast food is bad for your metabolism
Coffee increases blood pressure
Chips contain a lot of salt
Traditional medicine as an aid
It has long been known that natural recipes are used by women all over the world in order to alleviate their current condition and not harm the baby. Many people deliberately refuse to take traditional medications, completely replacing them with various teas and decoctions. This behavior is not correct, since all traditional medicine helps only to get rid of clinical symptoms, but is practically unable to affect the life cycle of the bacterium that causes pyelonephritis.
The main advantages of natural remedies:
- cheapness;
- ease of preparation and use;
- the ability to assemble the ingredients yourself;
- minimal harm to the health of mother and child;
- good effect from use.
The disadvantages include:
- the possibility of allergic reactions;
- individual intolerance during pregnancy;
- rapid loss of effect upon cessation of use.
Traditional medicine recipes that help cope with the manifestations of pyelonephritis during pregnancy:
- Take three large carrots and two beets and use a juicer to make juice. Dilute 200 ml of juice with 100 ml of hot water and drink on an empty stomach. Beets and carrots not only contain a large amount of vitamins, but also have a pronounced stimulating effect on the immune system of the human body, forcing it to fight bacteria. This juice must be consumed within two months.
- Brew three sachets of chamomile in a half-liter mug of boiling water. After cooling, drink the solution in small sips. The procedure is best carried out at a time when you do not plan to be away from home for a long time: chamomile has a mild diuretic effect, removes harmful toxic substances and waste from the body.
- Place 200 grams of crushed burdock leaves in a saucepan with a liter of hot water and cook over low heat, stirring clockwise. Once the liquid has cooled, divide it into three equal portions to drink throughout the day. Burdock leaves do an excellent job of treating inflammatory processes.
Photo gallery: traditional medicine for pyelonephritis
Beets and carrots contain many useful substances
Chamomile stimulates urination
Burdock relieves inflammation
Video: competent therapy for kidney inflammation during pregnancy
Treatment
- Immediate prescription of antibacterial drugs.
- Focus on the sensitivity of microorganisms (1b, A).
- Timely detection and correction of urodynamic disorders.
- Long-term antimicrobial prophylaxis for VUR and recurrent UTI (2a, B).
- Control of bowel function.
- Reduce the dose of the antibacterial drug depending on creatinine clearance.
In hospitalized patients, especially in infants who find it difficult to give the drug orally, antibacterial therapy is usually started with the parenteral route of administration of the drug in the first three days, followed by switching to oral administration. In the absence of severe intoxication and the child’s ability to receive the drug through the mouth, oral administration of the drug is possible from the first day (2a, B).
Aminoglycosides can be used as reserve drugs, as well as for combination therapy for urosepsis (amikacin 20 mg/kg per day once a day, tobramycin 5 mg/kg per day 3 times a day, gentamicin 5–7.5 mg /kg per day 3 times a day), carbapenems.
For pseudomonas infection - ticarcillin/clavulanate (250 mg/kg per day) or ceftazidime (100 mg/kg per day) + tobramycin (6 mg/kg per day); in particularly refractory cases - fluoroquinolones.
The effectiveness of treatment is assessed after 24–48 hours based on clinical signs and urine test results. If treatment is ineffective, anatomical defects or a kidney abscess should be suspected.
Spectrum of antibacterial drugs used to treat urinary tract infections in outpatients . It should be remembered that if the clearance of endogenous creatinine decreases to less than 50 ml/min, the dose of the drug is halved!
- Amoxicillin + Clavulanic acid – 50 mg/kg per day (amoxicillin) – 3 times a day
- Cefixime – 8 mg/kg per day – 2 times a day
- Cefuroxime axetil – 50–75 mg/kg per day – 2 times a day
- Ceftibuten – 9 mg/kg per day – 1 time per day
- Co-trimoxazole – 10 mg/kg per day (according to sulfamethoxazole) – 2–4 times a day
- Furazidin – 3–5 mg/kg per day – 3–4 times a day
Antibacterial drugs for parenteral use . It should be remembered that when the glomerular filtration rate decreases to less than 50 ml/min, the dose of the drug is halved!
- Amoxicillin + Clavulanic acid – 90 mg/kg per day – 3 times a day
- Ceftriaxone – 50–80 mg/kg per day – once a day
- Cefotaxime – 150 mg/kg per day – 4 times a day
- Cefazolin – 50 mg/kg per day – 3 times a day
Drugs used for long-term antimicrobial prophylaxis.
- Furazidine – 1 mg/kg – Once at night
- Co-trimoxazole – 2 mg/kg (according to sulfamethoxazole) – Once at night
- Amoxicillin + Clavulanic acid – 10 mg/kg – Once at night
Antibacterial therapy for 7–10 days usually eliminates the infection, regardless of its location. With longer courses, flora resistance is developed. In children with cystitis, antibiotics for 3–5 days are sufficient (Ib, A). Antibiotic therapy lasting less than 3 days is not recommended (1a, A).
Prevention
- Regular emptying of the bladder and bowels.
- Adequate fluid intake.
- Hygiene of the external genitalia.
Indications for preventive treatment (2a, B):
- the presence of vesicoureteral reflux of 2–5 degrees;
- recurrent urinary tract infection;
- severe anomalies in the development of the urinary tract before surgical correction.
The duration of prophylaxis is selected individually: usually at least 6 months. Drugs used for long-term antimicrobial prophylaxis are listed above. Additionally, herbal medicine with a bactericidal effect, for example the drug Canephron N (D), can be used.
Gestational pyelonephritis: diagnosis, prevention, treatment
The term urinary tract infection refers to the presence of any microorganisms in the urinary tract that are normally sterile. Traditionally, they are divided depending on the localization of the infectious-inflammatory process: in the bladder - cystitis, kidneys - pyelonephritis or only in the urine - bacteriuria, as well as the presence or absence of clinical manifestations - symptomatic and asymptomatic urinary tract infections [9,12,17, 18,20]. The most common kidney disease (especially in pregnant women) is pyelonephritis, occurring in 6–10% of cases. This is a nonspecific inflammatory process that involves the interstitial tissue and the renal pyelocaliceal system. This inflammation can occur during pregnancy, childbirth or the postpartum period. Its occurrence is facilitated by compression of the ureters by the growing uterus, the presence of foci of infection in the body (tonsillitis, caries, furunculosis, etc.), hormonal changes characteristic of pregnancy. Under the influence of progesterone produced by the placenta, relaxation of the smooth muscles of the intestines, bladder and ureters is observed. In this case, there is a tendency to constipation and a significant slowdown in the passage of urine due to expansion, lengthening, curvature of the ureters with kinks and looping, and an increase in the cavity of the pelvis. The urodynamics of the upper urinary tract and blood circulation in the kidneys are disrupted. Under these conditions, a favorable background is created for the spread of infection ascending from the urethra and bladder through the subepithelial layer of tissue into the renal pelvis. At the same time, dysuria, dysfunction of the bladder, an increase in its volume as a result of decreased tone, impairs the evacuation of urine from the upper urinary tract, which contributes to its retention and the development of inflammation in the kidneys. The pathological process develops in the interstitial tissue of the kidney and ends with its sclerosis, compression of the renal tubules, and the concentrating ability of the kidneys is early impaired. Against this background, renal hypertension may develop, which is observed in 20% of pregnant women with pyelonephritis. In the malignant course of arterial hypertension, renal failure may develop. Infection of the ureteral wall disrupts its peristalsis, leading to urinary stasis. Infection in the renal pelvis contributes to the formation of stones that injure the epithelium of the urinary tract. A vicious circle is formed - during pregnancy, urine evacuation decreases, promoting the development of infection, and urinary tract infection aggravates the stasis and severity of the pathological process [10,11,14,16,19]. Pyelonephritis has an adverse effect on the course of pregnancy and the condition of the fetus, manifested in a significant frequency of threatened miscarriage, premature birth, placental insufficiency, fetal hypoxia, intrauterine infection, gestosis and a complicated course of the adaptation period in the newborn [5,10,15,18,19 ]. In addition, progressive pregnancy can provoke exacerbation of pyelonephritis, increased frequency of attacks of renal colic, and worsens the function of the only kidney in women who have undergone nephrectomy. There are three degrees of risk for pyelonephritis, depending on the presence or absence of hypertension, azotemia, duration of kidney disease and the severity of kidney damage [11]: I degree – acute pyelonephritis that occurred during pregnancy; II degree – chronic uncomplicated pyelonephritis that existed before pregnancy; III degree – pyelonephritis with hypertension, chronic renal failure, pyelonephritis of a single kidney. In women with kidney disease throughout pregnancy, starting from the early stages, careful monitoring of the functional state of the kidneys and the course of pregnancy is necessary. With risk degree I, pregnancy and childbirth proceed, as a rule, safely. Complications such as anemia, threat of miscarriage, and late toxicosis occur with approximately the same frequency as in healthy pregnant women. However, intrauterine infection of the fetus can often occur. With risk degree II, there is a significant frequency of complications - 20–50% (spontaneous abortion, premature birth, fetal malnutrition, late toxicosis, increased perinatal mortality), and the course of pyelonephritis worsens. Tactics are individual. If renal function is preserved, there is no hypertensive syndrome, and there are no toxicoses, then pregnancy can be maintained, even if there were multiple exacerbations of the disease, ureteral catheterization, or kidney surgery during pregnancy. With risk degree III, as a rule, pregnancy is contraindicated, since severe forms of late toxicosis develop and renal failure progresses. With pyelonephritis of a single kidney, pregnancy is permissible only if it is in good functional condition. At the slightest deterioration in kidney function, urgent termination of pregnancy is indicated, regardless of gestational age. There are the following classifications of pyelonephritis: – Based on the duration of the inflammatory process, it is divided into acute or chronic (recurrent). Acute pyelonephritis is an acute exudative inflammation of the kidney and pelvis tissue with severe fever, intoxication, pain, and impaired renal function. Chronic - progressive inflammation of the tissue and tubules of the kidney, causing destructive changes in the pyelocaliceal system and wrinkling of the kidney; characterized by a long latent or recurrent course; – According to the clinical course, serous or purulent pyelonephritis is distinguished. Serous occurs at low-grade or even normal temperature, without symptoms of intoxication. It is recognized mainly by laboratory signs. Purulent is divided into a diffuse purulent (non-destructive) form - cured by conservative methods and a focal purulent form (apostematous nephritis, carbuncle and kidney abscess) - surgical treatment. The causative agents of pyelonephritis in pregnant women are often opportunistic microorganisms. In case of pyelonephritis, microorganisms of the group of enterobacteria (Escherichia coli, Proteus, Klebsiella) are determined predominantly (in approximately 70–80% of patients) in urine culture, less often – enterococcus, Pseudomonas aeruginosa. Along with the listed pathogens, urinary tract infections can be caused by candida, chlamydia, ureaplasma, mycoplasma and viruses. When examining patients, a monoculture of the pathogen is rarely isolated in the urine. As a rule, associations of microorganisms are found. Infection of the kidney most often occurs via an ascending route from the lower urinary tract or hematogenous - when there is an extrarenal focus in the body. Predisposing factors to the occurrence of pyelonephritis in the gestational period are disturbances in the urodynamics of the urinary tract and blood circulation in the kidneys. Starting from the early stages of pregnancy, 80% of healthy women experience functional changes in the urinary tract, manifested by impaired tone and contractile activity, hypotension, hypokinesia, dilatation of the pyelocaliceal system and ureters. Against this background, vesicoureteral and renal pelvic refluxes develop, as a result of which intrapelvic pressure increases, leading to the penetration of urine, microbes, and toxins into the kidney tissue, which predisposes to the development of acute pyelonephritis. In addition, the prerequisites for the development of the inflammatory process in the kidneys are created by abnormalities in the development of the urinary tract, stones, tumors, kinks of the ureter, etc. Most often, pyelonephritis occurs in 22–28 weeks of pregnancy. Acute pyelonephritis in pregnant and postpartum women is characterized by a sudden onset, high body temperature, chills, severe intoxication with the presence of characteristic local symptoms: pain in the lumbar region, corresponding to the side of the lesion, radiating to the upper abdomen, groin area, labia, thigh. The most severe course of pyelonephritis occurs when combined with other diseases of the urinary system: nephrolithiasis, developmental anomalies, nephroptosis, with pyelonephritis of a single kidney. With combined pathology, frequent relapses, severe forms of toxicosis and deterioration in the functional state of the kidneys are observed. In modern conditions, latent forms of chronic pyelonephritis predominate, accompanied by repeated relapses during pregnancy. Its signs may include asymptomatic bacteriuria and pyuria. Diagnosis of pyelonephritis is based on medical history, clinical picture of the disease, laboratory tests, ultrasound, chromocystoscopy, and x-ray methods. In recent years, magnetic resonance imaging has been the most significant in the diagnosis of diseases of the urinary system. The advantages of magnetic resonance imaging are: it is an objective method of medical visualization of all systems and organs for various diseases; non-invasiveness, safety of use and high diagnostic informativeness; the ability to visualize not only the structures of various organs, but also their relationships with adjacent tissues, obtaining information about their blood supply; Possibility of use in pregnant women. Recommended laboratory tests for pyelonephritis: 1) Hemogram: acute pyelonephritis - leukocytosis with band shift of neutrophils, hypochromic anemia; biochemical indicators – hypoproteinemia, dysproteinemia, moderate increase in the concentration of urea and creatinine; 2) General urine analysis: acute pyelonephritis – pyuria, bacteriuria, proteinuria less than 1 g/l, microhematuria; chronic pyelonephritis – unstable bacteriuria, leukocytes more than 10–15 in the field of view; 3) Urinalysis according to Nechiporenko: with pyelonephritis there is a sharp increase in the content of leukocytes; 4) Bacteriological examination of urine: identification of the pathogen, determination of the degree of microbial colonization (for pyelonephritis?? 105 CFU/ml) and sensitivity of the isolated microflora to antibiotics; 5) To study kidney function, the Zimnitsky test (for chronic pyelonephritis - isohyposthenuria, nocturia) and the Rehberg test are used; 6) Ultrasound of the kidneys allows you to determine the size of the kidneys, the thickness of the cortical layer, the size of the pyelocaliceal complex, to identify anatomical and functional disorders of the upper urinary tract (developmental anomalies, tumors, stones, hydronephrosis, etc.); 7) Among additional research methods, chromocystoscopy can be used, which allows you to clarify the localization of the process and contrast urography, which is performed before surgery on the urinary tract for a more accurate diagnosis of the localization of the inflammatory process and the degree of kidney damage; The criteria for prescribing magnetic resonance imaging are: the presence of anomalies of the urinary organs; frequent exacerbations of infectious and inflammatory kidney diseases during pregnancy; suspicion of the formation of severe complications in the form of a carbuncle, apostematous nephritis; the need to assess the functional state of the kidneys. MRI signs of an acute inflammatory process - swelling of the perinephric tissue, deformation and expansion of the pyelocaliceal system. MRI signs of a chronic inflammatory process - decreased differentiation of the cortex and medulla. thinning of the renal cortex. Acute pyelonephritis (exacerbation of chronic) in pregnant and postpartum women does not always have a clear clinical picture. Often, the clinical picture of acute pyelonephritis can simulate the picture of acute appendicitis, cholecystitis, influenza, etc., which can lead to diagnostic and tactical errors. Pyelonephritis in postpartum women can be regarded as a postpartum infectious disease. Basic principles of treatment for acute gestational pyelonephritis: timely antibacterial therapy (empirical and etiotropic), long-term treatment with herbal uroseptics, if necessary, restoration of impaired urine passage (catheterization, ureteral stenting, percutaneous puncture nephrostomy). The complex also provides: infusion, detoxification, sedative, desensitizing, symptomatic therapy, vitamin therapy, etc. If traditional therapy is ineffective, efferent detoxification methods can be used. In addition, careful monitoring of the course of pregnancy, the condition of the fetus, and prevention of hypoxia and fetal malnutrition are carried out. When treating patients in the first trimester of pregnancy, i.e. During the period of organogenesis, to prevent a damaging effect on the embryo, only low-toxic natural and semi-synthetic penicillins, which inhibit the growth of many gram-negative and gram-positive bacteria, and plant uroseptics are used. In the II and III trimesters of pregnancy, i.e. when fetal organogenesis is completed and the placenta begins to function, performing a barrier function in relation to some antibacterial and anti-inflammatory drugs, the range of antibacterial drugs can be expanded: natural and semi-synthetic penicillins, cephalosporins, macrolides; nitrofurans can be used as the second stage of treatment. In the postpartum period, in addition to this therapy, fluoroquinolones can be used. In this case, during the period of antibacterial therapy you should refrain from breastfeeding. Antibacterial therapy for pyelonephritis lasts 7–10 days, depending on the severity of the disease: for the first 5 days, parenteral administration of drugs is carried out, then treatment is carried out with oral forms of drugs until clinical and laboratory parameters are normalized. Antibacterial drugs of choice are: amoxicillin/clavulanate (1.2 g IV), ampicillin (0.5–1.0 g IM, IV), ampicillin/sulbactam (1.5–3.0 g IV /m, i.v.), carbenicillin (1.0 g i.m.), cephalosporins of various generations (1.0 g i.v.), etc. Of particular importance in the prevention and treatment of urinary tract infections, and, in particular, gestational pyelonephritis, is given to herbal uroseptics. Currently, there has been a clear increase in interest in the problems of herbal medicine - treatment with herbal medicines. Herbal medicine has a long history and today the effectiveness of the use of medicinal plants has been proven not only experimentally, but also using scientifically based methods at the molecular and cellular levels. In certain situations, extracts of medicinal plants are not inferior in effectiveness to chemical substances and even surpass them. The clinical significance of herbal medicines is evidenced by the fact that many of the largest pharmacological enterprises that produced synthetic drugs are mastering the production of products based on medicinal plants. Modern herbal preparations are produced using high technology and undergo multi-stage quality control. One of the new generation herbal medicines, widely used in urology, obstetrics, gynecology, etc. is Canephron N. This is a combination drug that includes centaury herb (Centaurium umbellatum), lovage root (Levisticum officinale) and rosemary leaves (Rosmarinus officinale). The substances included in the drug have an antiseptic, antispasmodic, anti-inflammatory effect on the organs of the urinary system, reduce the permeability of the capillaries of the kidneys, have a diuretic effect, improve kidney function, and enhance the effect of antibacterial therapy (Table 1). Various types of action of Canephron N are due to the essential oils, phenolcarbolic acids, phthalides, and bitternesses included in its composition. For example, the diuretic effect of the drug is due to the combination of various points of application of its components. Essential oils dilate the blood vessels of the kidneys, which improves the blood supply to the renal epithelium, and also influence the processes of reabsorption by the cells of the renal tubules. This manifests itself mainly in a decrease in the reabsorption of sodium ions and the corresponding amount of water. The diuretic effect of phenol carbonic acids is explained by the osmotic effect: when they enter the lumen of the renal tubules, they create high osmotic pressure (these substances are not subject to reabsorption); at the same time, the reabsorption of water and sodium ions is significantly reduced. Thus, an increase in water excretion occurs without disturbing the ion balance (potassium-saving effect). The antispasmodic effect is due to the flavonoid component of the drug. Phthalides (lovage) and rosemary oil have a similar effect. Phenolcarboxylic acids have weak antispasmodic properties. The anti-inflammatory effect is mainly due to the presence of rosmarinic acid, which blocks the nonspecific activation of complement and lipoxygenase with subsequent inhibition of leukotriene synthesis. Like other phenolic compounds, rosemary acid shows an antioxidant effect and interrupts free radical chain reactions. All medicinal plants that make up the Kanefron N contain substances that have a wide antimicrobial spectrum of action: phenolcarboard acids affect bacterial protein; Essential oils destroy the cytoplasmic membrane of bacteria and reduce the activity of aerobic respiration, which leads to a decrease in the release of the energy necessary for the synthesis of various organic compounds; Flavons, flavonoids and flavonols are able to contact the proteins of the cell wall and destroy cell membranes of bacteria. This ensures the activity of the drug even with microflora resistant to synthetic agents. The advantage of Kanefron N is also a combination of antimicrobial and anti -inflammatory effects, which is especially valuable in chronic processes in the urinary tract. In addition, the release of organic phenolcarbon acids and their glucuronidized and sulfate metabolites in urine leads to a change in its acidity, which counteracts the growth of bacteria. In addition to the listed properties, the elimination of bacteria from the urinary tract is facilitated by the following factors: bioflavonoids slow down bacterial hyaluronidase and thereby limit the spread of bacteria in tissues; The diuretic effect prevents adhesion of microorganisms. It was established that Kanefron N enhances the excretion of uric acid salts. This side of action is only partly associated with the diuretic effect and is quite specific. Strengthening the release of uric acid prevents the loss in the urinary tract of crystals, the growth of existing stones and the formation of new ones. It was also noted that this drug is enclosing the urine if it is sharply acidic, and supports the value of the pH within 6.2–6.8, which also prevents the formation of urate stones. The pharmacologically proven effect of Kanefron N on the tubular apparatus of the kidney clearly shows that the release of protein in the urine of previously transferred pathological processes that damage the tubular apparatus is significantly reduced. At the FSU "NC AGIP named after IN AND. Kulakova Rosmedtekhnologii ”There is experience in the use of kanephron n in pregnant women with high infectious risk (asymptomatic bacteriuria, pyelonephritis, anomalies in the development of urinary tract, etc.) [3.4,6–8]. If the asymptomatic bacteriuria is detected in the amount of 104–5-5 CFU/ml, a course of treatment with Kanephron H is 2 dragees 3 times a day for 3 weeks, followed by a control microbiological examination of urine. In the absence of the effect of therapy or the presence of higher concentrations of bacteria, as well as in the treatment of gestational or exacerbation of chronic pyelonephritis, antibacterial drugs are prescribed in combination with catneaphron and in the same dosages in order to potentiate the effect. After the cessation of antibacterial therapy, it is necessary to continue taking Kanefron N 2 dragees 3 times a day for 2-3 weeks. In the future, for the prevention of complications, it is necessary to take Kanefron N 2 Drage 3 times a day, within a week 1 time per month before the delivery period. In addition, given the positive effect of the drug on the filtration function of the kidneys, taking the drug in the same mode after delivery for 6 months. The cure of pyelonephritis are: the disappearance of the clinical manifestations of the disease, a positive dynamics in ultrasound examination of the kidneys and the lack of pathological changes in the urine with a threefold study within 8-10 days. Thus, pyelonephritis is a formidable complication, which requires a thorough examination and comprehensive treatment. Timely prevention, diagnosis and treatment can significantly reduce the frequency of pregnancy complications and improve perinatal outcomes.
Traditionally, they are divided depending on the localization of the infectious-inflammatory process: in the bladder - cystitis, kidneys - pyelonephritis or only in the urine - bacteriuria, as well as the presence or absence of clinical manifestations - symptomatic and asymptomatic urinary tract infections [9,12,17, 18,20]. The most common kidney disease (especially in pregnant women) is pyelonephritis, occurring in 6–10% of cases. This is a nonspecific inflammatory process that involves the interstitial tissue and the renal pyelocaliceal system. This inflammation can occur during pregnancy, childbirth or the postpartum period. Its occurrence is facilitated by compression of the ureters by the growing uterus, the presence of foci of infection in the body (tonsillitis, caries, furunculosis, etc.), hormonal changes characteristic of pregnancy. Under the influence of progesterone produced by the placenta, relaxation of the smooth muscles of the intestines, bladder and ureters is observed. In this case, there is a tendency to constipation and a significant slowdown in the passage of urine due to expansion, lengthening, curvature of the ureters with kinks and looping, and an increase in the cavity of the pelvis. The urodynamics of the upper urinary tract and blood circulation in the kidneys are disrupted. Under these conditions, a favorable background is created for the spread of infection ascending from the urethra and bladder through the subepithelial layer of tissue into the renal pelvis. At the same time, dysuria, dysfunction of the bladder, an increase in its volume as a result of decreased tone, impairs the evacuation of urine from the upper urinary tract, which contributes to its retention and the development of inflammation in the kidneys. The pathological process develops in the interstitial tissue of the kidney and ends with its sclerosis, compression of the renal tubules, and the concentrating ability of the kidneys is early impaired. Against this background, renal hypertension may develop, which is observed in 20% of pregnant women with pyelonephritis. In the malignant course of arterial hypertension, renal failure may develop. Infection of the ureteral wall disrupts its peristalsis, leading to urinary stasis. Infection in the renal pelvis contributes to the formation of stones that injure the epithelium of the urinary tract. A vicious circle is formed - during pregnancy, urine evacuation decreases, promoting the development of infection, and urinary tract infection aggravates the stasis and severity of the pathological process [10,11,14,16,19]. Pyelonephritis has an adverse effect on the course of pregnancy and the condition of the fetus, manifested in a significant frequency of threatened miscarriage, premature birth, placental insufficiency, fetal hypoxia, intrauterine infection, gestosis and a complicated course of the adaptation period in the newborn [5,10,15,18,19 ]. In addition, progressive pregnancy can provoke exacerbation of pyelonephritis, increased frequency of attacks of renal colic, and worsens the function of the only kidney in women who have undergone nephrectomy. There are three degrees of risk for pyelonephritis, depending on the presence or absence of hypertension, azotemia, duration of kidney disease and the severity of kidney damage [11]: I degree – acute pyelonephritis that occurred during pregnancy; II degree – chronic uncomplicated pyelonephritis that existed before pregnancy; III degree – pyelonephritis with hypertension, chronic renal failure, pyelonephritis of a single kidney. In women with kidney disease throughout pregnancy, starting from the early stages, careful monitoring of the functional state of the kidneys and the course of pregnancy is necessary. With risk degree I, pregnancy and childbirth proceed, as a rule, safely. Complications such as anemia, threat of miscarriage, and late toxicosis occur with approximately the same frequency as in healthy pregnant women. However, intrauterine infection of the fetus can often occur. With risk degree II, there is a significant frequency of complications - 20–50% (spontaneous abortion, premature birth, fetal malnutrition, late toxicosis, increased perinatal mortality), and the course of pyelonephritis worsens. Tactics are individual. If renal function is preserved, there is no hypertensive syndrome, and there are no toxicoses, then pregnancy can be maintained, even if there were multiple exacerbations of the disease, ureteral catheterization, or kidney surgery during pregnancy. With risk degree III, as a rule, pregnancy is contraindicated, since severe forms of late toxicosis develop and renal failure progresses. With pyelonephritis of a single kidney, pregnancy is permissible only if it is in good functional condition. At the slightest deterioration in kidney function, urgent termination of pregnancy is indicated, regardless of gestational age. There are the following classifications of pyelonephritis: – Based on the duration of the inflammatory process, it is divided into acute or chronic (recurrent). Acute pyelonephritis is an acute exudative inflammation of the kidney and pelvis tissue with severe fever, intoxication, pain, and impaired renal function. Chronic - progressive inflammation of the tissue and tubules of the kidney, causing destructive changes in the pyelocaliceal system and wrinkling of the kidney; characterized by a long latent or recurrent course; – According to the clinical course, serous or purulent pyelonephritis is distinguished. Serous occurs at low-grade or even normal temperature, without symptoms of intoxication. It is recognized mainly by laboratory signs. Purulent is divided into a diffuse purulent (non-destructive) form - cured by conservative methods and a focal purulent form (apostematous nephritis, carbuncle and kidney abscess) - surgical treatment. The causative agents of pyelonephritis in pregnant women are often opportunistic microorganisms. In case of pyelonephritis, microorganisms of the group of enterobacteria (Escherichia coli, Proteus, Klebsiella) are determined predominantly (in approximately 70–80% of patients) in urine culture, less often – enterococcus, Pseudomonas aeruginosa. Along with the listed pathogens, urinary tract infections can be caused by candida, chlamydia, ureaplasma, mycoplasma and viruses. When examining patients, a monoculture of the pathogen is rarely isolated in the urine. As a rule, associations of microorganisms are found. Infection of the kidney most often occurs via an ascending route from the lower urinary tract or hematogenous - when there is an extrarenal focus in the body. Predisposing factors to the occurrence of pyelonephritis in the gestational period are disturbances in the urodynamics of the urinary tract and blood circulation in the kidneys. Starting from the early stages of pregnancy, 80% of healthy women experience functional changes in the urinary tract, manifested by impaired tone and contractile activity, hypotension, hypokinesia, dilatation of the pyelocaliceal system and ureters. Against this background, vesicoureteral and renal pelvic refluxes develop, as a result of which intrapelvic pressure increases, leading to the penetration of urine, microbes, and toxins into the kidney tissue, which predisposes to the development of acute pyelonephritis. In addition, the prerequisites for the development of the inflammatory process in the kidneys are created by abnormalities in the development of the urinary tract, stones, tumors, kinks of the ureter, etc. Most often, pyelonephritis occurs in 22–28 weeks of pregnancy. Acute pyelonephritis in pregnant and postpartum women is characterized by a sudden onset, high body temperature, chills, severe intoxication with the presence of characteristic local symptoms: pain in the lumbar region, corresponding to the side of the lesion, radiating to the upper abdomen, groin area, labia, thigh. The most severe course of pyelonephritis occurs when combined with other diseases of the urinary system: nephrolithiasis, developmental anomalies, nephroptosis, with pyelonephritis of a single kidney. With combined pathology, frequent relapses, severe forms of toxicosis and deterioration in the functional state of the kidneys are observed. In modern conditions, latent forms of chronic pyelonephritis predominate, accompanied by repeated relapses during pregnancy. Its signs may include asymptomatic bacteriuria and pyuria. Diagnosis of pyelonephritis is based on medical history, clinical picture of the disease, laboratory tests, ultrasound, chromocystoscopy, and x-ray methods. In recent years, magnetic resonance imaging has been the most significant in the diagnosis of diseases of the urinary system. The advantages of magnetic resonance imaging are: it is an objective method of medical visualization of all systems and organs for various diseases; non-invasiveness, safety of use and high diagnostic informativeness; the ability to visualize not only the structures of various organs, but also their relationships with adjacent tissues, obtaining information about their blood supply; Possibility of use in pregnant women. Recommended laboratory tests for pyelonephritis: 1) Hemogram: acute pyelonephritis - leukocytosis with band shift of neutrophils, hypochromic anemia; biochemical indicators – hypoproteinemia, dysproteinemia, moderate increase in the concentration of urea and creatinine; 2) General urine analysis: acute pyelonephritis – pyuria, bacteriuria, proteinuria less than 1 g/l, microhematuria; chronic pyelonephritis – unstable bacteriuria, leukocytes more than 10–15 in the field of view; 3) Urinalysis according to Nechiporenko: with pyelonephritis there is a sharp increase in the content of leukocytes; 4) Bacteriological examination of urine: identification of the pathogen, determination of the degree of microbial colonization (for pyelonephritis?? 105 CFU/ml) and sensitivity of the isolated microflora to antibiotics; 5) To study kidney function, the Zimnitsky test (for chronic pyelonephritis - isohyposthenuria, nocturia) and the Rehberg test are used; 6) Ultrasound of the kidneys allows you to determine the size of the kidneys, the thickness of the cortical layer, the size of the pyelocaliceal complex, to identify anatomical and functional disorders of the upper urinary tract (developmental anomalies, tumors, stones, hydronephrosis, etc.); 7) Among additional research methods, chromocystoscopy can be used, which allows you to clarify the localization of the process and contrast urography, which is performed before surgery on the urinary tract for a more accurate diagnosis of the localization of the inflammatory process and the degree of kidney damage; The criteria for prescribing magnetic resonance imaging are: the presence of anomalies of the urinary organs; frequent exacerbations of infectious and inflammatory kidney diseases during pregnancy; suspicion of the formation of severe complications in the form of a carbuncle, apostematous nephritis; the need to assess the functional state of the kidneys. MRI signs of an acute inflammatory process - swelling of the perinephric tissue, deformation and expansion of the pyelocaliceal system. MRI signs of a chronic inflammatory process - decreased differentiation of the cortex and medulla. thinning of the renal cortex. Acute pyelonephritis (exacerbation of chronic) in pregnant and postpartum women does not always have a clear clinical picture. Often, the clinical picture of acute pyelonephritis can simulate the picture of acute appendicitis, cholecystitis, influenza, etc., which can lead to diagnostic and tactical errors. Pyelonephritis in postpartum women can be regarded as a postpartum infectious disease. Basic principles of treatment for acute gestational pyelonephritis: timely antibacterial therapy (empirical and etiotropic), long-term treatment with herbal uroseptics, if necessary, restoration of impaired urine passage (catheterization, ureteral stenting, percutaneous puncture nephrostomy). The complex also provides: infusion, detoxification, sedative, desensitizing, symptomatic therapy, vitamin therapy, etc. If traditional therapy is ineffective, efferent detoxification methods can be used. In addition, careful monitoring of the course of pregnancy, the condition of the fetus, and prevention of hypoxia and fetal malnutrition are carried out. When treating patients in the first trimester of pregnancy, i.e. During the period of organogenesis, to prevent a damaging effect on the embryo, only low-toxic natural and semi-synthetic penicillins, which inhibit the growth of many gram-negative and gram-positive bacteria, and plant uroseptics are used. In the II and III trimesters of pregnancy, i.e. when fetal organogenesis is completed and the placenta begins to function, performing a barrier function in relation to some antibacterial and anti-inflammatory drugs, the range of antibacterial drugs can be expanded: natural and semi-synthetic penicillins, cephalosporins, macrolides; nitrofurans can be used as the second stage of treatment. In the postpartum period, in addition to this therapy, fluoroquinolones can be used. In this case, during the period of antibacterial therapy you should refrain from breastfeeding. Antibacterial therapy for pyelonephritis lasts 7–10 days, depending on the severity of the disease: for the first 5 days, parenteral administration of drugs is carried out, then treatment is carried out with oral forms of drugs until clinical and laboratory parameters are normalized. Antibacterial drugs of choice are: amoxicillin/clavulanate (1.2 g IV), ampicillin (0.5–1.0 g IM, IV), ampicillin/sulbactam (1.5–3.0 g IV /m, i.v.), carbenicillin (1.0 g i.m.), cephalosporins of various generations (1.0 g i.v.), etc. Of particular importance in the prevention and treatment of urinary tract infections, and, in particular, gestational pyelonephritis, is given to herbal uroseptics. Currently, there has been a clear increase in interest in the problems of herbal medicine - treatment with herbal medicines. Herbal medicine has a long history and today the effectiveness of the use of medicinal plants has been proven not only experimentally, but also using scientifically based methods at the molecular and cellular levels. In certain situations, extracts of medicinal plants are not inferior in effectiveness to chemical substances and even surpass them. The clinical significance of herbal medicines is evidenced by the fact that many of the largest pharmacological enterprises that produced synthetic drugs are mastering the production of products based on medicinal plants. Modern herbal preparations are produced using high technology and undergo multi-stage quality control. One of the new generation herbal medicines, widely used in urology, obstetrics, gynecology, etc. is Canephron N. This is a combination drug that includes centaury herb (Centaurium umbellatum), lovage root (Levisticum officinale) and rosemary leaves (Rosmarinus officinale). The substances included in the drug have an antiseptic, antispasmodic, anti-inflammatory effect on the organs of the urinary system, reduce the permeability of the capillaries of the kidneys, have a diuretic effect, improve kidney function, and enhance the effect of antibacterial therapy (Table 1). Various types of action of Canephron N are due to the essential oils, phenolcarbolic acids, phthalides, and bitternesses included in its composition. For example, the diuretic effect of the drug is due to the combination of various points of application of its components. Essential oils dilate the blood vessels of the kidneys, which improves the blood supply to the renal epithelium, and also influence the processes of reabsorption by the cells of the renal tubules. This manifests itself mainly in a decrease in the reabsorption of sodium ions and the corresponding amount of water. The diuretic effect of phenol carbonic acids is explained by the osmotic effect: when they enter the lumen of the renal tubules, they create high osmotic pressure (these substances are not subject to reabsorption); at the same time, the reabsorption of water and sodium ions is significantly reduced. Thus, an increase in water excretion occurs without disturbing the ion balance (potassium-saving effect). The antispasmodic effect is due to the flavonoid component of the drug. Phthalides (lovage) and rosemary oil have a similar effect. Phenolcarboxylic acids have weak antispasmodic properties. The anti-inflammatory effect is mainly due to the presence of rosmarinic acid, which blocks the nonspecific activation of complement and lipoxygenase with subsequent inhibition of leukotriene synthesis. Like other phenolic compounds, rosemary acid shows an antioxidant effect and interrupts free radical chain reactions. All medicinal plants that make up the Kanefron N contain substances that have a wide antimicrobial spectrum of action: phenolcarboard acids affect bacterial protein; Essential oils destroy the cytoplasmic membrane of bacteria and reduce the activity of aerobic respiration, which leads to a decrease in the release of the energy necessary for the synthesis of various organic compounds; Flavons, flavonoids and flavonols are able to contact the proteins of the cell wall and destroy cell membranes of bacteria. This ensures the activity of the drug even with microflora resistant to synthetic agents. The advantage of Kanefron N is also a combination of antimicrobial and anti -inflammatory effects, which is especially valuable in chronic processes in the urinary tract. In addition, the release of organic phenolcarbon acids and their glucuronidized and sulfate metabolites in urine leads to a change in its acidity, which counteracts the growth of bacteria. In addition to the listed properties, the elimination of bacteria from the urinary tract is facilitated by the following factors: bioflavonoids slow down bacterial hyaluronidase and thereby limit the spread of bacteria in tissues; The diuretic effect prevents adhesion of microorganisms. It was established that Kanefron N enhances the excretion of uric acid salts. This side of action is only partly associated with the diuretic effect and is quite specific. Strengthening the release of uric acid prevents the loss in the urinary tract of crystals, the growth of existing stones and the formation of new ones. It was also noted that this drug is enclosing the urine if it is sharply acidic, and supports the value of the pH within 6.2–6.8, which also prevents the formation of urate stones. The pharmacologically proven effect of Kanefron N on the tubular apparatus of the kidney clearly shows that the release of protein in the urine of previously transferred pathological processes that damage the tubular apparatus is significantly reduced. At the FSU "NC AGIP named after IN AND. Kulakova Rosmedtekhnologii ”There is experience in the use of kanephron n in pregnant women with high infectious risk (asymptomatic bacteriuria, pyelonephritis, anomalies in the development of urinary tract, etc.) [3.4,6–8]. If the asymptomatic bacteriuria is detected in the amount of 104–5-5 CFU/ml, a course of treatment with Kanephron H is 2 dragees 3 times a day for 3 weeks, followed by a control microbiological examination of urine. In the absence of the effect of therapy or the presence of higher concentrations of bacteria, as well as in the treatment of gestational or exacerbation of chronic pyelonephritis, antibacterial drugs are prescribed in combination with catneaphron and in the same dosages in order to potentiate the effect. After the cessation of antibacterial therapy, it is necessary to continue taking Kanefron N 2 dragees 3 times a day for 2-3 weeks. In the future, for the prevention of complications, it is necessary to take Kanefron N 2 Drage 3 times a day, within a week 1 time per month before the delivery period. In addition, given the positive effect of the drug on the filtration function of the kidneys, taking the drug in the same mode after delivery for 6 months. The cure of pyelonephritis are: the disappearance of the clinical manifestations of the disease, a positive dynamics in ultrasound examination of the kidneys and the lack of pathological changes in the urine with a threefold study within 8-10 days. Thus, pyelonephritis is a formidable complication, which requires a thorough examination and comprehensive treatment. Timely prevention, diagnosis and treatment can significantly reduce the frequency of pregnancy complications and improve perinatal outcomes.
Literature 1. Alyaev Yu.G., Amosov A.V., Grigoryan V.A. and others. The use of the herbal preparation Canephron N in patients with chronic cystitis and urolithiasis. // Urology, 2005;4:29–33. 2. Amosov A.V. Herbal preparation Canephron in urological practice. // Doctor, 2000;6:36–38. 3. Elohina T.B., Ordzhonikidze N.V., Emelyanova A.I. et al. Efficiency and safety of the use of Canephron®N in the prevention of exacerbations of chronic and gestational pyelonephritis in pregnant women // Materials of the XII International Forum “Medical and Environmental Safety, Rehabilitation and Social Protection of the Population” (Turkey, Kemer). M., 2002:180–181. 4. Elohina T.B., Ordzhonikidze N.V., Emelyanova A.I. The use of Canephron®N for hydronephrosis in pregnant women // Proceedings of the conference “Current problems of obstetrics and gynecology”. Yerevan, 2001:82–83. 5. Iremashvili V.V. Urinary tract infections: a modern view of the problem. // Russian Medical Journal, 2007;15,29:2231–2236. 6. Kravchenko N.F., Murashko L.E. Use of the drug Canephron®N for the prevention and treatment of gestosis in pathologies of the urinary system // Problems of pregnancy, 2007, No. 13, pp. 26–31. 7. Ordzhonikidze N.V., Potapova S.Yu. The effectiveness of complex therapy for infectious and inflammatory complications of renal malformations in pregnant women // Proceedings of the 36th annual congress of the international society on the pathophysiology of pregnancy and the organization of gestosis. M., 2004:168–170. 8. Pustotina O.A., Alekseeva M.L., Gurtova B.L. et al. The influence of Canephron®N on the functional state of the kidneys in the fetus // Abstracts of reports at the XI Russian National Congress “Man and Medicine”. M., 2004:470. 9. Pytel Yu.A., Amosov A.V. Herbal preparation Canephron in urological practice. // Attending Physician, 1999;6:38–39. 10. Safronova L.A. Pyelonephritis and pregnancy. // Russian Medical Journal, 2000;8,18:778–781. 11. Shekhtman M.M., Pavlov V.V., Lineva O.I. Kidneys and pregnancy. // Samara: State Enterprise “Perspective”, 2000; 256 pp.; 12. Yakovlev S.V., Derevyanko I.I. What antibiotics are really needed to treat urogenital infections? // Consilium medicum, 2004;6,1:40–45. 13. Condron C., Toomey D., Casey RG, Shaffii M., Creagh T., Bouchier–Hayes D. Neutrophil bactericidal function is defective in patients with recurrent urinary tract infections. //Urol. Res., 2003;31(5):329–34. 14. Delzell JEJr., Lefevre ML Urinary tract infections during pregnancy. // Am Fam Physician. 2000;61:713–721. 15. Foxman B, Barlow R, d'Arcy H, et al. Urinary tract infection: estimated incidence and associated costs. // Ann Epidemiol. 2000;10:509–515. 16. Krieger JN Urinary tract infections: what's new? // J Urol 2002;168:2351–2358. 17. Nickel JK Management of urinary tract infections: historical perspective and current strategies: part 2 – modern management. // J Urol. 2005;173:27–32. 18. Nicolle LE Urinary tract infections: traditional pharmacologic therapies. // Am J Med. 2002;113(1A):35S–44S. 19. Schaeffer AJ, Rajan N, Cao Q, et al. Host pathogenesis in urinary tract infections. // Int J Antimicrob Agents. 2001;17:245–251. 20. Suman E., Gopalkrishna Bhat K., Hegde BM Bacterial adherence and immune response in recurrent urinary tract infection. // Int. J. Gynaecol. Obstet., 2001,75(3):263–268.
Prognosis and prevention
The outcome of pregnancy is determined by the characteristics of the disease. The most favorable prognosis is for patients with acute pyelonephritis that occurs during the gestational period. The frequency of major obstetric complications in this case does not exceed those in healthy pregnant women, but the risk of intrauterine infection of the child increases. With exacerbation of chronic uncomplicated pyelonephritis, which debuted before pregnancy, gestation is complicated 20-50% more often, but with adequate therapy it can be preserved. The combination of a chronic form of the disease with arterial hypertension or renal failure makes bearing a child problematic. Prevention of gestational pyelonephritis involves early registration at the antenatal clinic, timely detection of bacteriuria, correction of diet and physical activity to improve urine passage, and sanitation of foci of chronic infection.
LiveJournal
Complications
The occurrence of gestational pyelonephritis complicates the course of pregnancy and worsens its prognosis. The disease poses a threat to both the woman and the fetus. One of the frequent obstetric complications of pyelonephritis in pregnant women in the second trimester is a combined form of gestosis with the appearance of edema, increased blood pressure, the occurrence of proteinuria, changes in the vessels of the fundus, gross violations of capillary architecture and pulmonary hypertension. The risk of threatened miscarriage, spontaneous abortion, and premature birth increases due to increased excitability of the uterus against the background of severe pain and fever. Anemia often develops due to inhibition of erythropoietin synthesis in the kidney tissue.
Perinatal complications are usually caused by placental insufficiency, leading to fetal hypoxia and delayed fetal development. With pyelonephritis, intrauterine infection of the fetus, leakage of amniotic fluid, and amnionitis are more often observed. Newborns are more likely to develop acute respiratory distress syndrome. Perinatal mortality reaches 2.4%. A separate group of complications of the gestational period consists of infectious-septic conditions associated with kidney inflammation - septicemia, septicopyemia, infectious-toxic shock. The development of pregnancy aggravates the course of chronic pyelonephritis, leads to more frequent attacks of renal colic, and provokes renal failure.