03.08.2017
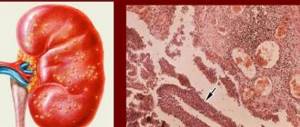
What is pyelonephritis? Pyelonephritis is a kidney disease that is caused by infection of pathogenic microorganisms.
Microbes enter through the descending route from the urinary system. The main causative agent of pyelonephritis is the bacterium Escherichia coli.
Pyelonephritis is included in the list of those diseases that can be prevented by preventive measures rather than cured later.
With improper treatment of inflammation in the urinary tract, microbes enter the kidneys through the descending pathway and cause the inflammatory disease pyelonephritis. Classification of pyelonephritis:
- acute form of kidney disease;
- chronic stage of disease development;
- primary pyelonephritis;
- secondary pyelonephritis;
- unilateral inflammation of the kidneys;
- bilateral pyelonephritis;
- latent stage of the disease;
- form of remission;
- active course of pyelonephritis;
- stage of purulent disease;
- stage of necrotic disease;
- apostematous pyelonephritis;
- pyelonephritis of diabetes mellitus;
- senile pyelonephritis;
- disease in a child's body;
- kidney inflammation during pregnancy.
Signs of pyelonephritis in men appear 5 times less frequently than symptoms of pyelonephritis in women.
General information about the disease
Chronic pyelonephritis is a nonspecific inflammation of kidney tissue. As a result of the spread of the pathological process, destruction of the vessels of the organ and.
The chronic form develops against the background of previously suffered acute pyelonephritis, in which treatment was carried out incorrectly or was completely absent. In some cases, the pathology may be asymptomatic and many patients do not even notice the presence of the disease. Pyelonephritis can become chronic for several reasons:
- urine reflux;
- inadequate treatment of the acute form;
- impaired excretion of urine as a result of narrowing of the urinary tract;
- chronic intoxication.
Chronic pyelonephritis according to ICD-10 has code N11 and is divided into several forms depending on various symptoms.
Statistical data
According to statistics, chronic pyelonephritis occurs in 60% of cases of genitourinary system disease with the development of an inflammatory process. In 20%, the pathology develops against the background of an acute course.
The disease is diagnosed most often in women and girls. This is due to the anatomical structure of the urethra. It is easier for viruses and bacteria to enter the female body through the vagina, from where they penetrate the kidneys and bladder.
The chronic course differs from the acute course in that the pathological process affects both kidneys, while the organs are not affected equally. This form most often occurs latently, and remissions are replaced by exacerbations.
General information
Pyelonephritis is an acute kidney disease caused by nonspecific microbial flora.
The pathological process also affects the system of calyces and pelvis. Usually both kidneys are affected at the same time.
The incidence of acute pyelonephritis reaches 16 cases per 100,000 population per year. There are three age groups most at risk of the disease:
- children under three years old, girls get sick eight times more often than boys;
- adults aged 18-35 years, women get sick seven times more often;
- people over 60 years of age, men and women get sick equally often.
The predominance of incidence in women is due to anatomical features and hormonal levels.
According to ICD 10, the disease is coded N10.
The obstructive form of the disease is accompanied by a violation of the outflow of urine due to the appearance of an obstruction in the ureters or urinary tract.
Obstructive pyelonephritis occurs with a predominance of local symptoms, non-obstructive - general.
Stages of pyelonephritis
The acute stage has the most pronounced symptoms. General symptoms include prolonged fever up to 37.5-38*C, accompanied by chills.
Patients complain of weakness, pain in muscles and joints. Local manifestations include lower back pain and urinary problems.
Acute pyelonephritis is treated with various methods, including. In acute forms of the disease, hospitalization in the department is indicated.
Traditional methods
The main treatment for acute pyelonephritis is medication. Must be assigned from the first day. Drugs are selected depending on the causative agent of the disease. The standard course of treatment is 10 days.
Table. Antibacterial drugs.
The following is used as symptomatic treatment:
- non-steroidal anti-inflammatory;
- antimicrobial;
- vitamins;
- immunocorrectors;
- detoxification therapy.
The person is prescribed bed rest until the temperature returns to normal. Drinking plenty of fluids is recommended - up to 2 liters of acidified liquid per day.
A dairy-vegetable diet is prescribed, with sufficient protein content. Fatty and fried foods, preservatives, and spices are excluded. You should not drink strong tea, coffee, or alcohol. Salt content is limited.
If there is obstruction of the urinary tract, decompression is required - this is a type of surgical treatment. The method involves passing a thin catheter through the urinary tract. If this method is not feasible, a percutaneous nephrostomy is applied.
Surgical treatment is also carried out when abscesses form in the kidney. The surgeon opens them, removes pus and... If the kidney is completely damaged and there is no possibility of its recovery, it is removed.
ethnoscience
Alternative treatment can only be auxiliary and should not be used as an alternative to antibiotic therapy.
Medicinal plants are used that act on the inflammation process and improve:
- bearberry;
- St. John's wort;
- birch buds;
Decoctions and infusions are prepared from these plants. Take the product warm, one glass at a time, throughout the day. Treatment is long-term, lasting at least a month.
Etiology of the disease
Pyelonephritis develops as a result of the activation and spread of pathogenic microbes under the influence of various factors. Most often this is infection with E. coli, streptococci, enterococci and other microorganisms.
Additional causes of inflammation in the kidneys are:
- incorrect treatment;
- , prostate adenoma, urine reflux and other diseases of the genitourinary system that were not promptly diagnosed and treated;
- proliferation of bacteria that remain in the kidney tissues for a long time;
- decreased immunity as a result of prolonged infectious diseases or immunodeficiency states;
- chronic pyelonephritis can be a complication after ARVI, tonsillitis, measles, pneumonia or scarlet fever (children are most susceptible);
- chronic pathologies such as diabetes, tonsillitis, obesity or bowel dysfunction;
- in women, or during the onset of sexual activity;
- unidentified congenital diseases of the genitourinary system.
Hypothermia and the presence of autoimmune reactions can trigger the development of the pathological process.
Clinical picture
The chronic form of pyelonephritis can be asymptomatic. Signs do not appear during remission. They become pronounced during the acute stage. The main clinical manifestations of pyelonephritis include:
- Intoxication of the body
. It is characterized by the presence of general weakness, nausea, vomiting, malaise, decreased appetite, and headaches and chills. When diagnosed, pale skin and tachycardia are noted. - Painful sensations
. Localized mainly in the lumbar region. - Unpleasant urine odor
can especially occur early in the morning, after sleep. - Pain when urinating
, .
Against the background of chronic pyelonephritis, water and electrolyte disturbances occur, which manifest themselves in the form of dry mouth, the appearance of cracks on the lips, peeling of the horse's coat and constant thirst.
The disease has several stages, each of which is manifested by special symptoms, in the presence of which the doctor can determine the degree of development of the pathology and prescribe the necessary treatment.
- Exacerbation
. At this stage, the signs are clearly expressed. Severe pain and intoxication of the body are observed. A laboratory blood test reveals an acceleration of ESR. Anemia is also observed. Lack of treatment at this stage leads to the development of renal failure, the diagnosis and treatment of which is difficult. - Latent
. The symptoms are not pronounced. Patients often complain of increased fatigue and constant weakness. In exceptional cases, hyperthermia is noted. There is practically no pain in the lumbar region and when urinating. Against the background of a pathological process, the ability of the kidneys to concentrate urine decreases, which affects its density. Laboratory testing of urine reveals the presence of bacteria and leukocytes. - Remission
. At this stage there are no symptoms. The disease does not manifest itself with any signs, which complicates diagnosis. During a laboratory test of urine, a slight deviation from normal values may be detected. When exposed to negative factors, the remission stage goes into the exacerbation stage, the symptoms become aggressive, and the patient requires medical attention.
Classification of the disease
Based on ICD-10, the types and forms of chronic pyelonephritis are determined by various factors. Highlight:
- Primary chronic form
. Pathology develops on a healthy organ, the pathological process affects both kidneys. - Secondary chronic form
. It is a complication of another pathology. At first it is unilateral in nature, then the inflammation affects the second kidney.
A certain group of scientists prefers to divide pyelonephritis into a community-acquired form and a hospital-acquired form, when the patient requires hospitalization. Depending on the location of the pathological process, the following are distinguished:
- One-sided.
- Double-sided.
According to the severity of the disease, the disease can be divided into:
- Complicated when other pathologies are associated.
- Uncomplicated, occurring without concomitant diseases.
A separate group includes pyelonephritis, which occurs with renal failure. Most often complicated forms.
Treatment options
Diagnosis and therapy are complicated by the fact that in the remission stage the disease does not show symptoms. Each patient with chronic pyelonephritis requires an individual approach and comprehensive treatment. First of all, to relieve symptoms during the exacerbation stage, medications are prescribed to relieve symptoms and destroy pathological microorganisms.
When a chronic form of pyelonephritis is established, the following groups are assigned:
- Cephalosporins. "Kefzol", "Cefepime" or "Tseporin";
- Semi-synthetic penicillins. “Amoxiclav”, “Ampicillin” or “Oxacillin” are broad-spectrum antibiotics that help destroy microorganisms that cause the development of the disease;
- “Negram”, the drug belongs to the group of nilidixic acids;
- in severe cases, Tobramycin, Gentamicin or Kanamycin are prescribed.
Ascorbic acid, Selenium, and Tocopherol are used as antioxidants. for chronic forms of pyelonephritis, they are prescribed for up to eight weeks. In cases of severe exacerbation, antibacterial drugs are administered intravenously, which helps to achieve greater effectiveness and faster results. “5-NOK” is considered one of the most modern remedies for pyelonephritis. It helps relieve symptoms and relieve inflammation in a short time.
The patient should limit the consumption of fatty foods, salty and spicy foods, and also follow the drinking regime prescribed by the doctor.
Traditional methods
Treatment of the pathology can occur after stopping the exacerbation stage and only after consultation with the attending physician. The most effective are the following recipes:
- White acacia tea
. Brew like regular tea. Drink half a glass for 10 days. - Bean broth
. Chop a glass of beans, pour a liter of boiling water, put on fire and bring to a boil. Take daily for 7 days in a row. - Heather infusion
. Pour two tablespoons of dried herbs into two glasses of boiling water and leave for an hour. Then strain and drink in large sips.
For pyelonephritis, baths with the addition of tincture of pine branches are also useful. The water temperature should not be less than 35 degrees. The duration of the bath is no more than 15 minutes. The course of treatment is 15 procedures.
Disease Prevention
To avoid the development of inflammation in the kidney tissues, you should follow. Experts recommend:
- avoid hypothermia;
- Healthy food;
- strengthen immunity;
- promptly treat infectious diseases.
The chronic form is dangerous because it may not manifest itself for a long time. The disease is diagnosed through the diagnosis of other pathologies. If symptoms occur, you should consult a doctor, since the acute form always develops into a chronic form, which is difficult to treat.
Pyelonephritis is a kidney disease caused by pathogenic microorganisms that penetrate the kidneys and cause inflammation in the renal pelvis. In Russia, the International Classification of Diseases, 10th revision, is in force, which makes it possible to record morbidity, the causes of patient complaints and visits to medical institutions, as well as conduct statistical research. ICD 10 identifies pyelonephritis in chronic and acute forms. From this material you will learn the code for pyelonephritis according to ICD 10, the classification of forms of the disease in this system, as well as the symptoms, causes and methods of treating the pathology.
Forecast
With insufficient treatment, acute pyelonephritis develops and periodically worsens.
If started in a timely manner, it can completely eliminate the infectious and inflammatory process in the kidneys. The treatment period is 2-3 weeks.
Acute pyelonephritis is a disease with a high risk of complications. In the absence of proper treatment, gradual destruction of kidney tissue occurs. Pyelonephritis is especially dangerous for children and pregnant women.
Pyelonephritis is an inflammatory disease of the kidneys. The pelvis and tissue (mainly interstitial) are directly affected. People of all ages are affected, but in women, due to structural features, the pathology occurs more often than in men.
According to the International Classification of Diseases, Tenth Revision (ICD-10), the condition is classified in class XIV “Diseases of the genitourinary system”. The class is divided into 11 blocks. The designation of each block begins with the letter N. Each disease has a three-digit or four-digit designation. Inflammatory kidney diseases belong to the headings (N10-N16) and (N20-N23).
Acute pyelonephritis ICD 10
Acute tubulointerstitial nephritis is the full name of this pathology in the International Classification of Diseases, 10th revision. Acute pyelonephritis code according to ICD 10 is determined by number 10. This code also denotes acute infectious interstitial nephritis and acute pyelitis. When it is important to identify the pathogen in diagnosing a disease, doctors use codes B95-B98. This classification is used for similar agents that cause the disease: streptococci, staphylococci, bacteria, viruses and infections. The use of these codes is not mandatory in the primary coding of the disease.
Causes of pyelonephritis
Most often, pyelonephritis occurs during the off-season, when the body succumbs to various external factors, which become a trigger for the development of the disease. The disease itself is caused by pathogenic microorganisms, including:
- staphylococci;
- pseudomonas;
- enterococci;
- enterobacter;
- Xibella and others.
The penetration of these bacteria into the cavity of the bladder, where they multiply and carry out their vital functions, occurs through the urethra. Often the causative agent of pyelonephritis is E. coli, which enters the body after defecation due to the close location of the anus and urethra. The provoking factor of the pathology may be a decrease in immunity due to:
- transmission of colds and viral diseases;
- observed infectious processes;
- hypothermia of the body;
- neglect of the rules of intimate hygiene;
- diabetes;
- problems with urine outflow: incomplete bowel movements, reverse outflow of urine;
- urolithiasis with complications.
People susceptible to diseases of the genitourinary system are at risk of developing pyelonephritis. People with congenital diseases of the kidneys, bladder and genital organs may also encounter this pathology. The likelihood of getting sick increases if you have undergone surgery, age-related changes, injuries, or have an active sex life.
Prevention
To prevent kidney problems, you need to drink plenty of fluids. On average, it is recommended to drink at least 2 liters per day. It is advisable to drink filtered or mineral water, as well as compotes and berry fruit drinks.
But do not forget about the rules and measures of personal hygiene.
It is necessary to prevent various infections from entering the urethra as much as possible. This can be achieved by using the toilet every day.
genitals, wearing underwear only from natural fabrics, taking a shower every time after sexual intercourse.
Many scientists suggest that any is a good stimulation of blood flow to the kidneys, as well as other internal organs, which has a positive effect on the removal of metabolic products from the body and accelerates cell recovery.
It is necessary to undergo a professional medical examination at least once every six months
, especially for those who are at risk of the disease. It is recommended to take a UBC and OAM in order to examine the kidneys and how they perform their functions. If the doctor detects even small changes in indicators, an additional examination is prescribed.
Female representatives are recommended to visit a gynecologist
to exclude various infectious diseases that are asymptomatic, this will prevent the possibility of infection entering the kidney cells through the ascending route.
Acute symptoms
In the acute course of pyelonephritis, symptoms appear almost immediately after the renal pelvis is damaged by pathogenic microorganisms. The disease can be recognized by the appearance of the following clinical picture:
- Painful sensations in the kidney area during walking, physical activity and even at rest. The pain can be localized in one area, or it can spread throughout the entire lower back, being encircling in nature. When tapping in the area of the kidneys, as well as palpating the abdomen, increased pain may be observed.
- There is a deterioration in health, increased fatigue, general weakness and malaise.
- Lack of appetite, nausea and vomiting.
- Increased body temperature, accompanied by chills, which may last for a week.
- Increased urination and cloudy urine.
- Swelling of the eyelids and limbs.
- Paleness of the skin.
These symptoms appear in almost every case of pyelonephritis. There is also a list of symptoms that are not characteristic of this disease, but indicate it:
- Toxic poisoning resulting from the activity of bacteria. Manifested by fever and a strong increase in temperature (up to 41°C).
- Increased heart rate, accompanied by pain.
- Dehydration of the body.
Ignoring such symptoms can lead to a complicated course of pyelonephritis and the transition of the acute form to the chronic form.
Chronic pyelonephritis ICD 10
The full name of this disease according to the International Classification of Diseases is designated as chronic tubulointerstitial nephritis. Chronic pyelonephritis according to ICD 10 is identified by number 11. Code number 11 also includes chronic forms of diseases such as infectious interstitial nephritis and pyelitis. In a narrower classification of chronic pyelonephritis, ICD 10 is further divided into several points. Number 11.0 denotes non-obstructive chronic pyelonephritis, that is, one in which the outflow of urine occurs as usual. Number 11.1 indicates obstructive chronic pyelonephritis, in which the function of the urinary system is impaired. If necessary, the documentation indicates not only the ICD 10 code denoting chronic pyelonephritis, but also the causative agent of the disease using codes B95-B98.
Symptoms of the chronic form
The chronic form of the disease in a quarter of cases is a continuation of the acute form of pyelonephritis. Due to the structural features of the female genitourinary system, women are more susceptible to developing this disease. Chronic pyelonephritis most often occurs in a latent form, so the symptomatic manifestations are very mild:
- Lower back pain usually does not occur. A weakly positive Pasternatsky Symptom is observed (painful sensations when the lower back is tapped).
- There is no disturbance in the outflow of urine, but the amount of urine produced increases and its composition changes.
- There are headaches, weakness, and increased fatigue.
- There is an increase in blood pressure.
- Hemoglobin decreases.
Chronic pyelonephritis can worsen several times a year during the off-season or due to other diseases. During exacerbation, the chronic form is similar in symptoms to the acute form.
Diagnostics
When the first symptoms of the disease occur, you must consult a urologist, who will listen to the patient’s complaints and prescribe a series of tests to confirm the diagnosis. The following instrumental and laboratory research methods will help identify pyelonephritis:
- Ultrasound of the kidneys. The disease is characterized by the occurrence of stones, changes in the density and size of the organ.
- Computed tomography of the kidneys. It will help determine the condition of the organ and the renal pelvis, as well as eliminate the possibility of urolithiasis and abnormalities in the structure of the kidneys.
- Excretory urography indicates limited mobility of diseased kidneys, the presence of deformation of the renal pelvis or a change in contour.
- Survey urography will help determine the increase in the size of the organ.
- Radioisotope renography will assess the functional capacity of the kidneys.
- General blood analysis. The test results will show an increase in the level of white blood cells with a simultaneous decrease in the level of red blood cells.
- Blood chemistry. Indicates a decrease in albumin, an increase in urea content in the blood plasma.
- Analysis of urine. The presence of protein, an increase in the number of leukocytes and salt levels are observed.
- Bacteriological culture of urine. Detects Escherichia coli, staphylococcus or other microorganisms that provoke pyelonephritis.
- The Zimnitsky test allows you to analyze the organ’s ability to concentrate urine. Using the sample, doctors determine the amount and density of the material taken, and also compare the resulting sample with the daily rate of urine excreted in a healthy person.
- The Nechiporenko test indicates an increase in the level of leukocytes and a decrease in the level of erythrocytes, the presence of bacteria, as well as simple and epithelial casts in the urine.
In chronic pyelonephritis, the readings may differ slightly from the test readings in the acute form of the disease: pathogenic microorganisms are not detected, and inflammatory processes are not detected. However, an experienced doctor, based on test results and manifestations of the disease, can always make the correct diagnosis and prescribe timely treatment.
Symptoms (signs)
CLINICAL MANIFESTATIONS
Acute pyelonephritis often occurs with a clear clinical picture, with purulent pyelonephritis similar to a septic or infectious disease.
Febrile fever with chills and profuse sweat. Pain in the lumbar region, tenderness on palpation, Pasternatsky's symptom is positive, on the side of pyelonephritis - tension in the anterior abdominal wall (peritonism phenomenon). Urinary syndrome - polyuria (more often) or oliguria (less often) with loss of fluid through the lungs and skin, dysuria - frequent and painful urination. Intoxication syndrome - headache, nausea, vomiting. With bilateral acute pyelonephritis, the development of acute renal failure is possible. Chronic pyelonephritis in most patients (50-60%) has a latent course. Low-grade fever, sweating, chilling. Pain in the lumbar region, Pasternatsky's symptom is positive. Urinary syndrome - polyuria, nocturia, less commonly dysuria. Symptoms of intoxication. Arterial hypertension (more than 70% of cases). Anemia (in some patients). Clinical signs of exacerbation
are an increase in body temperature (not always), an increase in blood pressure, increased or appearance of lower back pain, polyuria, dysuria, nocturia.
Laboratory research
.
Acute pyelonephritis.. Blood test... Increased ESR, neutrophilic leukocytosis, sometimes leukopenia, shift of the leukocyte formula to the left (with purulent pyelonephritis)... Increased urea and creatinine in the blood (with acute renal failure)... Urine. May be cloudy (mucus, bacteria, desquamated epithelium), leukocyturia (neutrophils), active leukocytes (Sternheimer-Malbin, “pale”, arachnid) - formed in urine with low osmolarity (with hematogenous introduction, infections may be absent in the first days, with obstruction there are no ureters), bacteriuria, proteinuria, erythrocyturia (less commonly, hematuria - with necrosis of the renal papillae), hyposthenuria (hypersthenuria is possible with oliguria). Chronic pyelonephritis. In urine analysis: moderate proteinuria, leukocyturia, bacteriuria, microhematuria, Sternheimer-Malbin cells, active leukocytes, hyposthenuria, alkaline urine reaction (especially characteristic of infection with Proteus, Klebsiella and Pseudomonas species). Bacteriological culture of urine is required (more than 103-5 microbes in 1 ml of urine) with determination of the sensitivity of the isolated microflora to antibiotics. Instrumental data
. Ultrasound of the kidneys.. In acute pyelonephritis - an increase in size, decreased echogenicity, spasm of the pelvicalyceal system, the contours of the kidney are even, with a renal carbuncle - a cavity formation in the parenchyma.. In chronic pyelonephritis - a decrease in size, increased echogenicity, deformation and expansion of the pelvicalyceal system system, tuberosity of the contours of the kidney, asymmetry of size and contours.. With obstruction of the urinary tract - signs of hydronephrosis on the affected side, stones. . Plain radiography: an increase or decrease in volume of one of the kidneys, tuberous contours, and sometimes a shadow of a stone. . Excretory urography (contraindicated in the active phase, with chronic renal failure).. In acute pyelonephritis - late contrast on the affected side, decreased intensity of contrast, slower removal of contrast.. In chronic pyelonephritis, in addition to these symptoms - expansion and deformation of the calyces and pelvis. . Angiography: in the early stages - a decrease in the number of small branches of the segmental arteries until their disappearance, in the later stages - the kidney shadow is small, there is no border between the cortical and medulla layers; Deformations of blood vessels, narrowing and reduction in their number are detected. . Radioisotope renography and scintigraphy: kidney sizes are normal or reduced, isotope accumulation is reduced, the secretory and excretory phases of the curve are lengthened. . Chromocystoscopy.. In acute pyelonephritis - discharge of turbid urine from the mouth of the ureter of the affected kidney (or both kidneys), slowed or weakened release of indigo carmine on the affected side.. In chronic pyelonephritis, dysfunction of the affected kidney is also determined, however, in many patients, disturbances in the release of indigo carmine are not detected .
Treatment
Only a specialist can prescribe drugs for the treatment of pyelonephritis. Self-medication can cause complications and difficulties in treating pyelonephritis in the future. Most often, doctors prescribe the following therapeutic methods:
- Taking antibacterial drugs.
Antibiotics are effective in eliminating microorganisms that are the main causative agent of pathology. Doctors prescribe both intravenous and oral antibiotics in the absence of contraindications. These may be drugs such as Ampicillin, Cefotaxime, Ceftriaxone or Ciprofloxacin. - Taking herbal preparations.
Products based on herbal components can restore the functional abilities of the kidneys, reduce inflammation and stimulate urination. - Symptomatic treatment.
At high temperatures and severe pain, it is recommended to take antipyretic and painkillers.
Treatment of pyelonephritis can take from a week to several months in particularly difficult cases.
Pyelonephritis is a nonspecific inflammatory disease of an infectious nature, which affects the pyelocaliceal system and interstitial tissue. In 20% of cases, this pathology develops secondary to acute inflammation. Most often the lesion is bilateral. The risk group includes young girls and women, which is associated with easier penetration of microbes from the urethra and bladder. For chronic pyelonephritis, the ICD-10 code is N11.
Pyelonephritis
Preventive actions
The etiology of the disease is under the close attention of specialists. At the same time, the risk of acute damage to kidney tissue can be reduced using preventive measures:
- timely treatment of infections;
- careful adherence to personal hygiene rules;
- timely elimination of obstacles to the normal passage of urine.
The formulation of the diagnosis of “acute pyelonephritis” involves the use of anti-inflammatory and antibacterial agents. In severe cases, surgical intervention is indicated for a child or adult. Much attention is paid to maintaining a strict diet. When the first symptoms of the disease appear, you should contact a medical clinic.
Types of diagnoses
All urologists know about pyelonephritis. The following types of this pathology are distinguished in children and adults:
- Chronic obstructive (code N11.1).
- Non-obstructive, caused by reflux (reflux of urine from the ureters). The ICD-10 code is N11.0.
- Unspecified etiology (code N11.9).
- Infectious.
- Non-infectious.
If a person is diagnosed with pyelonephritis, the ICD-10 code will depend on the etiology of the disease and the results of instrumental and laboratory tests.
Features of chronic pyelonephritis
This disease most often has a microbial (bacterial) nature. Chronic inflammation of the kidneys is caused by cocci, Escherichia coli, Proteus, Pseudomonas aeruginosa and other bacteria. This pathology is preceded by acute pyelonephritis. Predisposing factors for the development of chronic pyelonephritis (according to ICD-10 code N11) are:
- untimely and incorrect treatment of acute inflammation;
- foci of bacterial infection (tonsillitis, inflammation of the prostate, otitis media, inflammation of the paranasal sinuses, urethritis, cholecystitis);
- difficulty in the outflow of urine;
- stones;
- irrational (monotonous) nutrition;
- narrowing of the ureters;
- reflux;
- tumors;
- benign prostatic hyperplasia;
- diabetes;
- immunodeficiency states;
- intoxication of the body;
- childbirth and onset of sexual activity;
- congenital features of the development of the urinary organs (diverticula, spermatocele).
Chronic pyelonephritis
The disease is not as pronounced as acute pyelonephritis. Exacerbations, which occur mainly in the cold season, are replaced by remission. The following symptoms are characteristic of chronic pyelonephritis:
- Low-grade fever.
- Heaviness in the lower back.
- It's a dull pain.
- Disruption of the urination process (pain, frequent micturition).
- Headache.
- Fatigue during work.
- Malaise.
- Signs of arterial hypertension. Characteristic of the hypertensive form of pyelonephritis. Patients experience sudden increases in blood pressure, attacks of hypertensive crisis, severe headache, shortness of breath, nausea and dizziness. Sometimes there is pain in the heart area.
- Positive symptom of lumbar concussion (Pasternatsky).
- Signs of anemia.
- Sleep disturbance.
- Edema. Appears in advanced cases. They occur mainly in the first half of the day. The swelling is soft, symmetrical, mobile, pale, warm to the touch, localized on the face and lower extremities. They appear quickly and disappear just as quickly.
Objective signs of the disease are the presence of protein in the urine (proteinuria), excess of normal levels of leukocytes, the presence of columnar epithelium and bacteria. Sometimes blood appears in the urine. Often the disease is detected already at the stage of chronic renal failure.
Diagnostics
Diagnostics
.
The diagnosis of active pyelonephritis (acute or exacerbation of chronic) is made on the basis of the clinical “triad” - fever, lower back pain, dysuria; laboratory data confirm the diagnosis (see above), incl. results of bacteriological urine culture and determination of sensitivity to antibiotics, instrumental data. . In case of latent pyelonephritis, it is advisable to conduct a prednisolone test (30 mg of prednisolone in 10 ml of 0.9% sodium chloride solution intravenously). The test is positive if, after the administration of prednisolone, the content of leukocytes and bacteria in the urine doubles. . Urinalysis according to Nechiporenko, the leukocyte formula of urine allows us to differentiate chronic pyelonephritis and glomerulonephritis: .. with glomerulonephritis, the number of erythrocytes exceeds the number of leukocytes, with pyelonephritis the number of leukocytes is higher.. with glomerulonephritis, lymphocytes predominate in the leukocyte formula of the blood, with pyelonephritis - neutrophils. . With chronic pyelonephritis, the concentrating ability of the kidneys is impaired early (Zimnitsky test), with glomerulonephritis - later, at the stage of development of chronic renal failure. . Differential diagnosis
. Infectious diseases accompanied by fever (typhoid fever, malaria, sepsis). Pyonephrosis. Hydronephrosis. Acute purulent disease of the lower urinary tract. Kidney infarction. Acute glomerulonephritis. Pneumonia. Cholecystitis. Acute pancreatitis. Acute appendicitis. Splenic infarction. Dissecting aortic aneurysm. Shingles. Accompanying illnesses. Obstruction of the urinary tract. Anomalies of the urinary tract. Pregnancy. Nephrolithiasis. SD. Immunodeficiency states.
Stages of tubulointerstitial pathology
Tubulointerstitial nephritis in ICD-10 is prescribed without stages. There are only 3 of them. Stage 1 is characterized by the following violations:
- infiltration of tissues with leukocytes;
- atrophic changes in the collecting ducts;
- intactness of the renal glomeruli.
At stage 2 of the disease, sclerotic changes are observed. Part of the interstitial tissue is replaced by scar tissue. Hyalinization of the glomeruli and vascular damage also occur. At stage 3, the kidney decreases in volume and shrinks. Its surface becomes lumpy. At this stage, symptoms of renal failure are severe.
Chronic pyelonephritis during pregnancy
The classification separately identifies the gestational form of the disease. Chronic pyelonephritis in pregnant women is much more common than in the rest of the population. This is due to hormonal changes and decreased immunity. In pregnant women, the tone of the urethra, ureters and bladder decreases, which facilitates the penetration of infection. An important factor is that many medications are contraindicated during pregnancy, which complicates the treatment of acute pyelonephritis and contributes to the transition of the disease to a chronic form.
The development of the disease is facilitated by increased pressure on the urinary organs by an enlarged uterus and impaired urine outflow. Pyelonephritis (ICD-10 code N11) in pregnant women is often asymptomatic. Complaints are observed only during exacerbations. Changes are detected during a general urine test.
Chronic kidney inflammation during pregnancy can lead to the following consequences:
- arterial hypertension;
- renal failure;
- gestosis (toxicosis).
Chronic pyelonephritis during pregnancy
What is dangerous - consequences
Pyelonephritis never goes away completely without a trace. Only a few patients who have experienced signs of the disease will forget about them forever. A large number of people suffer every year from the recurrence of the disease after remission. A relapse can be triggered by any malfunction in the body.
The consequences for women and men are basically the same: impaired renal function, renal failure, pathologies in urination. The only difference is neurosis , as a consequence of pyelonephritis in women.
It still seems to you that it is impossible to regain potency
Chronic and acute pyelocystitis, pyelitis and cystopyelonephritis can negatively affect potency. To avoid this, you need to treat the disease in a timely manner. Complex therapy includes:
- Following a strict diet with limited salt. Patients are advised to eat fermented milk products, vegetables, fruits, berries (watermelons), drink juices, fruit drinks and herbal infusions. Alcoholic drinks, coffee, pickles, smoked meats, spices, fatty and spicy foods are excluded from the menu.
- Taking antibacterial agents. They are indicated in the acute phase. For pyelonephritis, fluoroquinolones (Nolitsin), penicillins (Amoxiclav), cephalosporins (Suprax, Ceftriaxone), aminoglycosides and nitrofurans (Furadonin) are used.
- The use of symptomatic drugs (antihypertensives, antispasmodics).
- Physiotherapy (SMT therapy, ultrasound, chloride baths).
Diet recommendations
During exacerbations, you need to follow a diet . Its main goal:
- reduce the load on the kidneys;
- prevent irritation of the urinary canals;
- shift the urine reaction to the alkaline side, to deprive microbes of the conditions for their life and reproduction.
Together with medication treatment, diets will help reduce relapses of pyelonephritis.
Outside of periods of exacerbation, if your state of health improves, you are allowed to consume fish products and meat, only lean meat - rabbit, beef or chicken.
For prevention, many doctors may prescribe that patients follow certain recommendations. The month is divided into 3 parts (1 week, 2 and 3, then 4):
- In 1 week: you need to drink fruit drinks from berries (preference to cranberry), rosehip decoctions.
- In weeks 2 and 3: drink diuretic herbal decoctions.
- In week 4: take a course of antimicrobial medications.