Internal urethral opening
[cm. note 5 in block C00-D48]
ICD-10 alphabetical indexes
External Causes of Injury - The terms in this section are not medical diagnoses, but rather a description of the circumstances under which the event occurred (Class XX. External Causes of Morbidity and Mortality. Heading Codes V01-Y98).
Medicines and chemicals - table of medicines and chemicals that have caused poisoning or other adverse reactions.
In Russia, the International Classification of Diseases
10th revision (
ICD-10
) was adopted as a single normative document for recording morbidity, reasons for the population’s visits to medical institutions of all departments, and causes of death.
ICD-10
introduced into healthcare practice throughout the Russian Federation in 1999 by order of the Russian Ministry of Health dated May 27, 1997 No. 170
The release of the new revision (ICD-11) is planned by WHO in 2022.
Abbreviations and symbols in the International Classification of Diseases, 10th Revision
NOS
- without other instructions.
NEC
— not classified in other categories.
†
— code of the main disease. The main code in the dual coding system contains information about the underlying generalized disease.
*
- optional code. An additional code in the double coding system contains information about the manifestation of the main generalized disease in a separate organ or area of the body.
The bladder is an organ of the urinary system that is located in the pelvis. Bladder cancer has an ICD-10 code of C67.
According to statistics, bladder cancer affects approximately 55% of the world's population. The tumor occurs in most cases in men whose age category is 60-75 years.
Causes
Etiology.
The occurrence of bladder cancer is associated with tobacco smoking, as well as with the action of certain chemical and biological carcinogens.
Industrial carcinogens used in rubber, paint, paper and chemical manufacturing have been implicated in bladder cancer. Bladder bilharzia often leads to squamous cell carcinoma. Other etiologic agents include cyclophosphamide, phenacetin, kidney stones, and chronic infection. Morphology (
bladder tumors are most often of transitional cell origin).
papillary. transitional cell. squamous. adenocarcinoma. Classification
.
TNM .. Primary lesion: Ta - non-invasive papilloma, Tis - cancer in situ, T1 - with invasion into the submucosal connective tissue, T2 - with invasion into the muscular layer: T2a - inner layer, T2b - outer layer, T3 - Tumor grows into peri-vesical tissue : T3a - determined only microscopically; T3b - determined macroscopically; T4 - with invasion of adjacent organs: T4a - prostate gland, urethra, vagina, T4b - pelvic and abdominal walls.. Lymph nodes: N1 - single up to 2 cm, N2 - single from 2 to 5 cm or damage to more than 5 nodes, N3 - more than 5 cm. Distant metastases: M1 - presence of distant metastases. Grouping by stages
.
Stage 0a: TaN0M0. Stage 0is: TisN0M0. Stage I: T1N0M0. Stage II: T2N0M0. Stage III: T3-4aN0M0. Stage IV .. T0-4bN0M0 .. T0-4N1-3M0 .. T0-4N0-3M1. Clinical picture
.
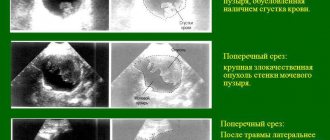
Hematuria. Dysuria (pollakiuria, imperative urges). When an infection occurs, pyuria occurs. Pain syndrome does not always occur. Diagnostics
. Physical examination with mandatory digital rectal examination and bimanual examination of the pelvic organs. OAM. Excretory urography: filling defects with large tumors, signs of damage to the upper urinary tract. Urethrocystoscopy is the leading research method for suspected cancer and is absolutely necessary to assess the condition of the mucous membrane of the urethra and bladder. To determine the volume of the lesion and histological type, an endoscopic biopsy of the tumor is performed. Examine the mucous membrane. In the presence of carcinoma in situ, the mucous membrane is externally unchanged, or diffusely hyperemic, or resembles a cobblestone pavement (bullous change in the mucous membrane). Cytological examination of urine is informative both for severe tumor lesions and for carcinoma in situ. Ultrasound: intravesical formations and the condition of the upper urinary tract. CT and MRI are the most informative for determining the extent of the process. X-rays of the chest organs and skeletal bones are performed to identify metastases. Bone lesions in highly malignant forms of cancer may be the first signs of the disease.
Classification according to the TNM system
This classification (European Association of Urology, 2009) uses numerical designations of different categories to indicate the extent of the tumor and the presence or absence of local and distant metastases.
T - from lat. tumor 'tumor'. Describes and classifies the main tumor site.
Ta - non-invasive papillary carcinoma
Tis - carcinoma in situ
(flat tumor)
T1 - tumor extends to subepithelial connective tissue
T2 - tumor invasion of the muscle layer
T2a - tumor invasion of the superficial muscle layer (inner half)
T2b - tumor invasion of the deep muscle layer (outer half)
T3 - tumor extends to paravesical tissue
T3a - microscopically
T3b - macroscopically (extravesical conglomerate)
T4 - tumor invasion of any of the following organs: prostate, uterus, vagina, pelvic wall, abdominal wall
T4a – tumor has spread to the prostate or uterus or vagina
T4b - tumor invasion of the pelvic wall or abdominal wall
N - from lat. nodulus 'knot'. Describes and characterizes the presence of regional metastases, that is, metastases to regional lymph nodes.
Nx—regional lymph nodes cannot be assessed
N0 - no metastases in regional lymph nodes
N1 - metastasis in one regional lymph node (internal iliac, obturator, external iliac, presacral)
N2 - multiple metastases in regional lymph nodes (internal iliac, obturator, external iliac, presacral)
N3 - metastases in the common iliac lymph nodes
M - from lat. metastasis 'metastasis'. Characteristics of the presence of distant metastases, that is, metastases to distant lymph nodes, other organs, tissues (excluding tumor germination).
Mx - distant metastases cannot be assessed
M0 - no distant metastases
M1 - distant metastases
P, G
For some organs or systems, additional parameters are used (P or G, depending on the organ system), characterizing the degree of differentiation of its cells.
Treatment
Treatment depends
depending on the stage of the disease, no clear standards for the treatment of bladder cancer have been developed. . With carcinoma in situ, malignant transformation of the cells of the mucous membrane occurs. Local chemotherapy may be used. In the case of widespread damage (urethra, prostate ducts) and progression of symptoms, early cystectomy with simultaneous bladder plastic surgery or transplantation of the ureters into the intestines is indicated. . Transurethral resection: used for superficial tumor growth without damage to the muscular lining of the organ. At the same time, relapses are quite frequent. Intravesical chemotherapy reduces the frequency of relapses of superficial bladder tumors. Doxorubicin, epirubicin and mitomycin C are effective. The drug is diluted in 50 ml of physiological solution and injected into the bladder for 1-2 hours. With the degree of differentiation G1, a single instillation immediately after transurethral resection is sufficient. For stage G1-G2 tumors, a 4-8 week course of instillations is carried out. Local immunotherapy with BCG reduces the frequency of relapses. External beam radiation therapy does not provide long-term remission (relapses within 5 years in 50% of cases). Interstitial radiation therapy is rarely used. Cystectomy is used to treat patients with diffuse superficial lesions if transurethral resection and intravesical chemotherapy fail. . Invasive bladder cancer.. Intensive local treatment with cytostatics is prescribed to patients to eliminate a rapidly progressing tumor without metastasis.. Radiation therapy. For some tumors, irradiation at a total dose of 60-70 Gy to the bladder area has proven effective. Radical cystectomy is the method of choice in the treatment of deeply infiltrating tumors. Involves removal of the bladder and prostate in men; removal of the bladder, urethra, anterior vaginal wall and uterus in women. After radical cystectomy, urine is diverted using one of the following methods: ileal reservoir, intestinal stoma for self-catheterization, bladder reconstruction, or ureterosigmostostomy. For villous tumors and localized “in situ” tumors, treatment often begins with transurethral resection, adjuvant immunotherapy (BCG), and intravesical chemotherapy. If such tumors recur, it is necessary to decide on performing a cystectomy.
Postoperative follow-up
.
After transurethral resection, the first control cystoscopy is 3 months later, then depending on the degree of tumor differentiation, but not less than 1 time per year for 5 years in case of grade TaG1 and for 10 years in other cases. After reconstructive operations - ultrasound of the kidneys and urinary reservoir, biochemical blood test: the first year every 3 months, the second or third year every 6 months, from 4 years - annually. The prognosis depends
on the stage of the process and the nature of the treatment performed. After radical surgery, the 5-year survival rate reaches 50%
ICD-10. C67 Malignant neoplasm of the bladder. D09 Preinvasive bladder cancer
Often, with advanced cancer, a tumor can be identified in women by bimanual palpation through the vagina and anterior abdominal wall, and in men through the rectum. Urine tests for bladder cancer show an increase in the number of red blood cells, and blood tests show a decrease in hemoglobin levels, indicating ongoing bleeding. One way to diagnose bladder cancer is urine cytology, which is usually performed several times. The detection of atypical cells in the urine is pathognomonic for bladder neoplasm. In recent years, another laboratory diagnostic method has appeared, the so-called BTA (bladder tumor antigen) test. Using a special test strip, urine is examined for the presence of a specific bladder tumor antigen. This technique is usually used as a screening diagnostic method. Ultrasound diagnostics is of great importance in diagnosing bladder cancer. Transabdominal examination can detect tumors larger than 0.5 cm with a probability of 82%. The formations located on the lateral walls are most often visualized. When the tumor is localized in the bladder neck, the use of transrectal examination may be informative. Small neoplasms are best diagnosed using transurethral scanning, performed with a special sensor inserted through the urethra into the bladder cavity. The disadvantage of this study is its invasiveness. It must be remembered that an ultrasound of a patient with a suspected bladder tumor must necessarily include an examination of the kidneys and upper urinary tract in order to identify dilatation of the collecting system as a sign of compression of the ureteral orifice by the tumor. Large tumors are detected by excretory urography or retrograde cystography. Sedimentary cystography according to Kneise-Schober helps to increase the information content of the study. Spiral and multislice computed tomography with contrast is of great importance in the diagnosis of bladder cancer. Using these techniques, it is possible to establish the size and localization of the formation, its relationship to the orifices of the ureters, germination into neighboring organs, as well as the condition of the kidneys and upper urinary tract. However, this method can be used if the patient is able to accumulate a full bladder and hold urine during the study. Another disadvantage of CT is the insufficient information content in identifying the depth of tumor invasion into the muscle layer due to the low ability to visualize the layers of the bladder wall. Magnetic resonance imaging is also used in the diagnosis of bladder tumors. Unlike CT, tumor invasion into the muscle layer of the bladder or adjacent organs can be assessed with much greater accuracy. Despite the informative nature of high-tech methods, the main and final method for diagnosing bladder cancer is cystoscopy with biopsy. Visualization of the tumor, a morphologist's conclusion about the malignant nature, structure and degree of differentiation of the bladder neoplasm are leading in the choice of treatment method. Fluorescence cystoscopy can increase the information content of cystoscopy. The peculiarity of this technique is that after treating the mucous membrane of the bladder with a solution of 5-aminolevulinic acid during cystoscopy using light from the blue violet part of the spectrum, the tumor tissue begins to fluoresce. This is due to increased accumulation of fluorescent agent by neoplasm cells. The use of this technique makes it possible to identify small formations that often cannot be detected by any other method.
Oncological lesions of internal organs have recently experienced a tendency towards rejuvenation. They are often diagnosed at a fairly young age. Very often, patients under 50 years old hear a terrible diagnosis - bladder cancer. According to data provided by medical statistics, this dangerous oncological process, which affects the genitourinary system of people, has become diagnosed 4 times more often over the past decade.
In the urinary system, the development of the process of malignancy occurs much more often than in other structural elements of the body. This is due to its direct functioning. Thus, a bladder tumor is in 11th place among all malignant neoplasms of the human body. Experts have a simple explanation for this - caustic urine passes through this organ, containing a large amount of carcinogens excreted by the kidneys.
Bladder cancer
The pathological mechanism of their effect on the mucous membrane of the main urinary organ is as follows:
- an aggressive liquid containing a large amount of carcinogens, after entering the bladder, remains in it for quite a long time, from 20 minutes to several hours, depending on the frequency of the urge to urinate in a person;
- urine, which has pronounced caustic properties, has a corrosive effect on the mucous membrane, which provokes the development of a mutation process in its cellular structures, which is expressed in their accelerated growth;
- a consequence of increased division of epithelial cells is the development of papilloma on the walls of the bladder, which is initially benign in nature;
- further prolonged exposure to aggressive fluid leads to increased cell division and the acquisition of pronounced atypia by this process.
Malignancy of the epithelial layer of the main organ of the urinary system occurs very quickly, and at the time the patient consults a doctor, 90% of neoplasms detected in the bladder are malignant. This tendency to rapidly mutate makes the disease very dangerous, but due to the fact that it has quite pronounced symptoms, the pathological process can be identified in the early stages and emergency measures can be taken to stop it in a timely manner.
Important!
A cancer tumor developing in the bladder has an increased tendency to invasion (spreading into neighboring organs) and distant metastasis, and therefore requires timely and adequate treatment. Otherwise, the pathological process can quickly lead to death.
Diagnosis of bladder cancer
The most important factor in the successful treatment of such diseases is early diagnosis. The earlier the tumor is detected, the lower the risk of complications. BC can recur in 50% of cases, so not only diagnosis is important, but also complete removal of foci of cancer cells. The diagnosis is made based on anamnesis, physical examination, and the results of laboratory and instrumental diagnostics.
Diagnosis of bladder cancer includes:
- Analysis of patient complaints and subsequent physical examination. During the examination of the patient, the doctor palpates the bladder and possible areas of metastasis.
- Laboratory tests of blood and urine. General and biochemical blood tests do not provide the necessary information to establish a diagnosis of bladder cancer. A specific method is the determination of the UBS protein, the bladder cancer antigen. If the result is positive, the amount of protein is increased 15 times. However, false-positive results are possible in inflammatory diseases of the urinary system. Among other urine tests, microexamination of urine sediment is used to detect the presence of pathological cells. In this case, a study of swabs from the walls of the affected organ is more informative. Cystoscopy does not always provide an opportunity to determine an unmistakable conclusion and is used in the presence of contraindications to cystoscopy or as a screening test to determine bladder cancer at an early stage;
- Instrumental research. The most informative way to detect bladder cancer is cystoscopy. This invasive but highly informative method allows you to determine the size, location, shape and growth pattern of the pathological lesion. Cystoscopy provides the opportunity to take a biopsy - a piece of tissue for the differential diagnosis of cancer and a precancerous condition. If a biopsy is performed correctly, the procedure is not dangerous to the patient’s health and does not affect the rate of development of the tumor.
Classification
ICD 10, the latest international classification of diseases, tenth revision, identifies several types of bladder cancer. First of all, they are distinguished by histological characteristics. All types of cancer, the distinguishing feature of which is their tissue structure, are detected only after examination under a microscope, taken during diagnostic measures.
Based on the cellular structure of the main organ of the urinary system, a tumor in the bladder is divided by leading oncologists into the following histological types:
- () type of tumor structure. The most common type of malignant neoplasm affecting the human genitourinary system. It is detected in 90% of cases. A feature of this type of tumor is its papillary growth, and the absence of a tendency to grow into the deep layers of muscle tissue or other internal organs.
- . It usually occurs against the background of cystitis, which has a chronic course. The process of atypia in this case affects the flat cells of the superficial epithelial layer of the main urinary excretory organ. There is a tendency of malignant structures to germinate and metastasize.
- . It is rare and has a fairly unfavorable prognosis. The tumor structure of this is localized in the muscular layer of the urinary organ and is prone to rapid growth and germination of metastases into neighboring organs at the earliest stages of development.
- . It is formed from the connective tissue of the urinary organ due to prolonged exposure to carcinogenic substances contained in urine. It is characterized by high malignancy, a tendency to early metastasis and frequent relapses.
- Carcinosarcoma. The rarest (0.11% among all bladder oncologies) type of malignant tumor, characterized by obvious heterogeneity, that is, heterogeneity of cellular structure and structure. In such a neoplasm, sarcomatoid and urothelial components are always simultaneously present. The disease has a very high aggressiveness and an unfavorable prognosis for life.
In addition to the so-called division of bladder cancer according to histological characteristics, leading oncologists also take into account the degree of tumor growth into the wall of the urinary organ. on this basis, it is divided into th (the neoplasm is located exclusively in the upper layer of the bladder and usually has a thin stalk) and (the tumor almost completely grows into the wall of the bladder and begins to destroy its muscle layer).
Stages of bladder cancer
In addition to identifying the histological structure of bladder cancer, its location and the degree of damage by the process of destruction of the urinary organ, specialists need to know at what stage of development the malignant process is in order to correctly prescribe treatment. , just like other organs and systems of the human body, goes through several stages in its development. Each of them has a direct relationship with the degree of tumor invasion of the bladder walls and the presence of metastases in the lymph nodes and nearby or distant internal organs.
Leading oncologists distinguish 4 stages of disease development:
- The tumor process at stage 1 affects only the upper, mucous layer of the urinary organ. The growth of anomalous structures into its wall does not occur at this stage. Also, this stage is not characterized by the earliest appearance of metastases in the regional lymph nodes.
- Stage 2 bladder cancer is characterized by germination up to the muscle layer. The favorable prognosis of the disease depends on how affected it is. In the case when the oncological process spreads only to its inner layer (substage 2A), a person’s chances of life increase, since the danger of abnormal cells sprouting into regional lymph nodes is minimal. The growth of a malignant neoplasm into the outer layers of muscle tissue is indicated by specialists with the symbol 2B, the presence of which in the patient’s medical history indicates the need for more serious therapy.
- Stage 3 bladder cancer indicates tumor growth into soft tissues located in the immediate vicinity of the bladder. The peritoneum, pelvic walls, etc. are also affected by secondary malignant foci. A cancerous tumor at this stage usually has pronounced symptoms and poses a serious threat to the patient’s life.
- At stage 4 of urinary cancer, the formation increases significantly in size and grows not only into nearby pelvic organs, but also into, and. This stage in the course of the pathological condition is considered the most difficult, since at this stage it is impossible to carry out radical surgical intervention, and the period of life is reduced to several months or even weeks.
To clarify the diagnosis, the following measures are used:
- General urine analysis. With its help, the specialist confirms the presence of hidden blood in it, and can also detect the presence of infectious agents. Such a study is prescribed first. It helps to minimize the causes of internal bleeding.
- Cytological test for bladder cancer. For this analysis, a centrifuge is used, through which urine is passed, and then the resulting residue is examined under a microscope. If a histologist finds (atypical cells) in it, he most likely assumes the presence of a malignant process in the human genitourinary system.
- An ultrasound of the kidneys and bladder gives the diagnostician the opportunity to detect the presence of an oncological tumor. In addition, with the help of this diagnostic study, pathological conditions of the urinary system with similar symptoms are identified.
- CT and MRI. These types of diagnostics provide a clearer picture of pathological changes than ultrasound.
After the diagnostic results have confirmed the expected diagnosis, the leading oncologist will select the appropriate one for the specific situation.
Important!
Only through timely and correctly conducted diagnostic tests do doctors have the opportunity to prescribe adequate therapy that helps prolong a person’s life and alleviate the severe symptoms associated with the disease.
Prognosis and survival rate for bladder cancer:
| Stage | Description | Treatment | Forecast | Survival percentage |
| 1 | At this stage, cancerous tumors are located in the superficial layers. | Shrink or completely remove cancerous tumors using a procedure called transurethral resection (TURP). Use of chemotherapy or immunotherapy. | Fast recovery. | More than 91% |
| 2 | Cancer cells enter the muscle wall of the bladder. | Transurethral resection of the bladder along with chemotherapy (less commonly radiation therapy). | Fast recovery. | More than 73% |
| 3 | Cancer cells have spread to nearby organs. | MPs are often removed and chemotherapy is used. | After surgery, the cancer may return. | 50% can live more than 5 years. |
| 4 | Metastases to regional and distant lymph nodes, the tumor is inoperable. | It is not possible to remove cancer surgically. Uses unverified clinical trials. | Restoration is not possible. Solution: help the patient cope with the manifestations of the disease. | Less than 7%. |
Bladder cancer treatment
Currently, in the treatment of this type of malignant process, the same techniques are used as in general to eliminate abnormal cellular structures. But they have a narrower specialization, which allows them to more effectively influence oncological tumors with such localization.
Bladder cancer is treated through the combined effects of the following therapeutic measures:
- . In this case, removal of bladder cancer can be carried out either after opening the abdominal cavity or without it. In the latter case, the insertion of surgical instruments is performed by a catheter inserted into the opening of the urethra. For medical reasons, radical surgery can also be used. For bladder cancer, it is prescribed when the tumor is very large and to remove it it is necessary to completely cut out the urine storage device. But this type of surgery has a significant disadvantage - it increases the risk of kidney disease.
- . It is used at all stages of the development of the disease to destroy abnormal cellular structures. Also, antitumor drug treatment is used as a preventive measure to avoid relapses of the disease.
- . The best effect is achieved when this therapeutic technique is used in conjunction with chemistry. But for medical reasons it can be prescribed separately.
- (BCG vaccine administered to prevent recurrence of cancer inside a damaged organ). It is used as an additional method that increases human immunity. BCG for bladder cancer is included in the treatment protocol in cases where there is a high risk of relapse of the disease.
In the event that surgical intervention is impossible for medical reasons or the cancer patient refuses to undergo surgery, the oncologists leading the patient recommend treatment methods such as ionizing, radiation, radiation and chemistry. They can be used either isolated from each other or together.
Important!
Any therapeutic technique will be effective only in cases where the pathological condition is detected in the initial stages. With early consultation with a doctor and adequate implementation of all prescribed treatment measures, a cancer tumor localized in the urinary organ can be defeated and a long-term remission can be achieved. If extensive metastasis develops or if the patient refuses radical surgery, his chances of further life become minimal.
Nutrition and alternative treatment as auxiliary therapy
In order to enhance the therapeutic effect of traditional medicine, experts recommend the additional use of herbal medicine. Herbal preparations are used for it, helping to destroy abnormal cellular structures and having a restorative effect. Auxiliary includes taking decoctions and infusions from medicinal plants that simultaneously have antitumor and diuretic properties (birch or lingonberry leaves, knotweed, bearberry).
Nutritional correction also plays an important role in bladder cancer. A proper diet enhances the effect of ongoing medications and promotes a speedy recovery. The diet for cancer patients with a cancerous tumor in the bladder is selected by a specialist, taking into account that the patient’s daily menu includes all the necessary microelements and vitamins. The basis for this disease should be fresh vegetables and fruits containing a large amount of plant fiber.
Metastases and relapse in bladder cancer
Late diagnosis of bladder cancer increases the risk of tumor metastasis to other organs. Unfortunately, they are detected in approximately half of cancer patients with a tumor structure that has spread to the muscle layer of the bladder. Even those patients who have undergone radical cystectomy are not immune from their occurrence. Most often, not only regional lymph nodes, but also the liver, lungs and bone structures are affected by the germination of abnormal cells. The presence of metastases in the human body always provokes a recurrence of bladder cancer.
In addition, the following factors contribute to the recurrence of the disease:
- insufficient therapeutic measures to eliminate primary carcinoma;
- high degree of malignancy of the cancerous structure;
- large tumor size;
- its later detection.
In case of relapse, the most important indicator is the time of development of the secondary tumor. The earlier the daughter neoplasm appeared, the higher the degree of aggressiveness it has. The most dangerous is the occurrence of a relapse of the disease in the first six months after therapy.
Complications and consequences of treatment
If the development of this type of disease is ignored by the patient, it will quickly, like any other oncology, enter an advanced stage, which is fraught with the occurrence of some complications. Usually in the later stages, in addition to the appearance of extensive metastases in nearby and distant organs, people experience severe problems with urination, a general deterioration in health due to intoxication of the body with tumor decay products, kidney failure and death. Bladder cancer has such consequences in the absence of adequate treatment, but experts also note the occurrence of some complications after radical treatment.
The most common of them are:
- Macrohematuria (presence of bloody inclusions in the urine).
- Impotence. It can occur quite often, despite the preservation of the nerve endings of the cavernous bodies during radical cystectomy.
- Renal failure and urinary tract obstruction.
These complications disrupt a person’s quality of life, but they can be quite effectively eliminated thanks to innovative methods of therapy, so in no case should you abandon the treatment protocol proposed by a specialist for fear of their occurrence. Only timely and adequately implemented therapeutic intervention can save a person’s life.
Symptoms
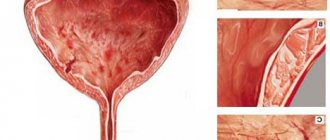
One of the first signs of bladder cancer is hematuria (blood in the urine), although it can be caused by other causes. Blood clotting in the bladder cavity can lead to the development of acute urinary retention.
Another common symptom of the disease is frequent, painful urination. Pain above the womb is also possible. Compression of the ureteric orifices by the tumor leads to disruption of the outflow of urine from the kidneys, as a result of which pyelonephritis or chronic renal failure can develop.
There is a known case of weekly priapism, which, as it later turned out, was a symptom of the disease [3].
How long do patients live?
Life expectancy for bladder cancer is directly influenced by the degree of malignancy of the tumor and the stage of its development.
The smaller they are, the more favorable the treatment outcome:
- at the initial stage of development of the pathological condition, five-year survival is observed in 90% of patients, and ten-year or more in 80%;
- in the second stage, half of cancer patients survive up to 5 years, and 35% of patients overcome the 10-year mark;
- the third stage gives 30% of patients a chance to live 5 or more years;
- The last stage of the disease is predicted to be almost hopeless. There is no information on ten-year survival at this stage of the disease, and only 10% of cancer patients reach 5 years.
From these statistics it follows that bladder cancer has a more favorable prognosis only if its detection and subsequent adequate treatment were timely.
Preventing bladder cancer
The best way to help prevent the development of bladder cancer is to prevent the aggressive effects of carcinogens on the body.
Taking into account all possible risk factors for the development of bladder cancer, in order to avoid the occurrence of the disease, it is necessary:
- treat any urological diseases in a timely manner, that is, seek medical help when the very first signs of the disease appear;
- strengthen the drinking regime, since liquid dilutes carcinogens contained in urine and promotes their rapid elimination from the body;
- undergo regular preventive examinations, and if alarming symptoms appear, immediately consult a doctor for advice;
- begin timely treatment of any pathological changes in the genitourinary system and, if possible, undergo endoscopic monitoring;
- at the first urge to urinate, visit the toilet, and do not hold the aggressive liquid in the bladder;6. adequately treat compliance with safety regulations when working in hazardous industries;
- give up such a bad habit as smoking.
Only properly carried out prevention of bladder cancer can prevent the development of a life-threatening disease even in those people who are at risk. Paying attention to your health helps to avoid the occurrence of not only malignant processes, but also any other pathological changes in the body.
Prevention
Preventive measures for bladder cancer include:
- Quitting bad habits (alcohol and especially smoking).
- Increasing immunity through sports and hardening the body.
- In the presence of diseases of the genitourinary system, a complete cure is required so that bladder diseases or inflammatory processes do not progress to the chronic stage.
- Stop drinking chlorinated tap water and drink only boiled or filtered water.
- If any symptoms associated with urological diseases occur, immediately consult a doctor for urine and blood tests and an ultrasound to rule out cancer.
Informative video
Bladder cancer is most often transitional cell. Symptoms include hematuria; later, urinary retention may be accompanied by pain. Diagnosis is confirmed by imaging or cystoscopy and biopsy. These include surgical treatment, destruction of tumor tissue, intravesical instillations or chemotherapy.
Much less common are other histological types of bladder cancer that have epithelial (adenocarcinoma, squamous cell carcinoma of the bladder, mixed tumors, carcinosarcoma, melanoma) and non-epithelial (pheochromocytoma, lymphoma, choriocarcinoma, mesenchymal tumors) origin.
The bladder can also be affected due to direct germination of malignant tumors from neighboring organs (prostate, cervix, rectum) or distant metastasis (melanoma, lymphoma, malignant tumors of the stomach, breast, kidneys, lungs).
General information
Bladder cancer accounts for 3% of all cancer sites. People whose bodies are exposed to aromatic amines, as well as those suffering from chronic cystitis, are at risk.
More than half of bladder cancer cases among men are associated with smoking (about a third in women)[1]. Researchers argue that there is a direct link between smoking and risk, while stopping smoking reduces risk[2].
The most common form of bladder cancer is transitional cell carcinoma.
(developing from the transitional epithelium of the urinary tract), squamous cell carcinoma and adenocarcinoma (a tumor originating and built from the glandular epithelium) are more rare.
The disease can manifest itself as papillary growths (non-linear mural inclusions) with malignancy or a solid, ulcerated, invasive tumor. There are bladder cancer in situ
, superficial cancer (T1-2) and cancer invading the muscle layer and surrounding tissues (T3-4).
The main focus of papillary bladder cancer often produces multiple metastases. Superficial bladder cancer forms metastases much less frequently. As the disease progresses, the pelvic (N1-2), retroperitoneal lymph nodes (N3-4) are affected, and metastasis occurs to the lungs, liver, and bones.
What causes bladder cancer?
In the United States, there are more than 60,000 new cases of bladder cancer and approximately 12,700 deaths annually. Bladder cancer is the fourth most common cancer in men and less common in women; The ratio of men to women is 3:1. Bladder cancer is diagnosed more often in whites than in African Americans, and its incidence increases with age. In more than 40% of patients, the tumor recurs in the same or a different site, especially if the tumor is large, poorly differentiated, or multiple. Expression of the p53 gene in tumor cells may be associated with progression.
Smoking is the most common risk factor, causing more than 50% of new cases. The risk is also increased by excessive use of phenacetin (analgesic abuse), long-term use of cyclophosphamide, chronic irritation (particularly from schistosomiasis, calculi), exposure to hydrocarbons, tryptophan metabolites, or industrial chemicals, especially aromatic amines (aniline dyes, such as naphthylamine, used in industrial painting) and chemicals used in the rubber, electrical, cable, dyeing and textile industries.
Diagnosis of bladder cancer
Bladder cancer is suspected clinically. Excretory urography and cystoscopy with biopsies from abnormal areas are usually performed immediately because these tests are necessary even if urine cytology, which can detect malignant cells, is negative. The role of urinary antigens and genetic markers has not been fully established.
For clearly superficial tumors (70-80% of all tumors), cystoscopy with biopsy is sufficient for staging. For other tumors, computed tomography (CT) of the pelvis and abdomen and chest x-ray are performed to determine the extent of the tumor and identify metastases.
Bimanual examination using anesthesia and magnetic resonance imaging (MRI) may be helpful. The standard TNM staging system is used.
Diagnostics
To identify an oncological process, a detailed examination is required, including laboratory and instrumental research methods.
- general blood analysis;
- blood chemistry;
- general urine analysis;
- bacteriological urine culture;
- cytological examination to identify atypical cells;
- prostate specific antigen test;
- coagulogram (blood clotting test).
- cystoscopy;
- Ultrasound;
- transrectal scanning;
- biopsy;
- endoluminal echography;
- excretory urography;
- pelvic venography and lymphography.
Bladder cancer treatment
Early superficial bladder cancer, including initial muscle invasion, can be completely removed by transurethral resection or tissue destruction (fulguration). Repeated instillation of chemotherapy drugs into the bladder, such as doxorubicin, mitomycin, or thiotepa (rarely used), may reduce the risk of relapse. Instillation of the BCG vaccine (Bacillus Calmette Gurin) after transurethral resection is generally more effective than instillation of chemotherapy drugs for cancer in situ and other highly differentiated, superficial, transitional cell variants. Even when the tumor cannot be completely removed, some patients may benefit from instillation. Intravesical BCG therapy with interferon may be effective in some patients who have relapsed after BCG therapy alone.
Tumors that extend deep into or beyond the walls usually require radical cystectomy (removal of the organ and adjacent structures) with concomitant urinary diversion; resection is possible in less than 5% of patients. Cystectomy is increasingly being performed after initial chemotherapy in patients with locally advanced disease.
Urine diversion traditionally involves diversion into an isolated loop of ileum exposed to the anterior abdominal wall and collection of urine in an external urine bag. Alternatives, such as orthotopic new bladder or cutaneous diversion, are very common and acceptable to many—if not most—patients. In both cases, the internal reservoir is built from the intestine. During the formation of the orthotopic new bladder, the reservoir is connected to the urethra. Patients empty the reservoir by relaxing the pelvic floor muscles and increasing abdominal pressure so that urine flows through the urethra almost naturally. Most patients maintain urinary control during the day, but some incontinence may occur at night. When urine is diverted into a subcutaneous reservoir (a “dry” stoma), patients empty it by self-catheterization throughout the day as needed.
If surgical treatment is contraindicated or the patient objects, radiation therapy alone or in combination with chemotherapy can provide a 5-year survival rate of about 20-40%. Radiation therapy can cause radiation cystitis or proctitis or cervical stenosis. Patients should be monitored every 36 months for progression or relapse.
Prognosis and prevention
When diagnosed with bladder cancer, the prognosis after any treatment (except for surgery to remove the organ) is a high risk of relapse. If the disease returns, it is recommended not to take any more risks, but to remove the organ. The 5-year survival rate for stage 1-2 tumors, taken as the standard, is guaranteed in 88-94% of cases. It is possible to say exactly how long people live with bladder cancer only in relation to a specific patient, and then only approximately, since the body’s capabilities cannot be predicted. According to statistics, the death of patients with stage 1-2 tumors is more often associated with complications after operations - colitis, urinary outflow disorders, than with relapses. For stage 3-4 cancer, survival rate is much shorter, depending on the malignancy of the process and the timing of treatment.
When diagnosed with bladder cancer in men, survival depends not only on the therapy provided, but also on further monitoring of the patient. Patients should regularly visit the oncologist according to the schedule: in the first 2 years every 3 months, in the 3rd year - every 4 months, 4-5 years after treatment - every 6 months, and after the past 5 years it is enough to visit the oncologist once every year. According to practice, doctors claim that about 80% of patients stop coming to the clinic after 4 years have passed from the completed course of treatment. This behavior cannot be called responsible, since relapses can occur later.
To summarize, it can be noted that a bladder tumor will be less dangerous for the patient if diagnosed early.
The later cancer is detected, the less chance of a successful outcome. Even after successful treatment, there is a high risk of relapse, so it is advisable for the patient to visit the doctor with some regularity so as not to miss warning signs and take timely measures.