Author of the article
Arthur Viniaminovich Artemyev
Urologist, gynecologist, practicing specialist
Articles written
64
Contact the author
Staphylococci are the most studied of the resident flora of human skin due to their ubiquitous colonization and the wide range of diseases they cause. Although most microorganism-skin interactions are commensal, they can cause opportunistic infections that range from skin diseases to urinary tract injuries. Staphylococcus is detected in urine after it enters the opening of the urethra. Colonization is achieved using a variety of adhesins, surface proteins and secreted enzymes. Bacteria adhere to the walls of the urethra, multiplying and moving into the bladder.
Classification of staphylococcus
Staphylococci are opportunistic bacteria localized on the skin and mucous membranes of human internal organs. With normal functioning of the immune system, they do not manifest themselves and do not have a negative effect. As soon as a person’s protective properties weaken, staphylococcal colonies begin to actively multiply, releasing exotoxins and endotoxins harmful to the body.
In total, there are about 30 species of this bacterium, but several of the most dangerous varieties are distinguished:
- Golden (staphylococcus aureus) is the most pathogenic species and poses the greatest threat. It is capable of provoking inflammatory and purulent processes in almost all human systems and organs.
- Saprophytic (staphylococcus saprophyticus). This type of bacterium causes cystitis, urethritis and inflammatory processes in the kidneys and bladder.
- Epidermal (staphylococcus epidermidis) is a bacterium that affects any mucous membrane. Its name comes from the word “epidermis” (the surface layer of the skin). It provokes conjunctivitis, septic tissue lesions, purulent phenomena of wound surfaces and the genitourinary system.
- Hemolytic (staphylococcus haemolyticus) is a pathogen that causes sore throat, inflammatory processes in the mucous membranes of the respiratory tract and organs.
Causes and methods of infection
A pathogenic bacterium can actively reproduce due to the following factors:
- stress;
- poor nutrition;
- diseases of the gastrointestinal tract;
- long-term therapy with antibacterial drugs;
- alcohol and smoking abuse;
- chronic inflammatory and infectious processes in the body;
- lack of vitamins and microelements;
- helminthic infestations;
- pregnancy;
- immunodeficiency.
A person can become infected with staphylococcal bacteria during illness, when his immunity is most weakened and cannot resist the external environment. For example, pregnant women become infected because their body has a low protective barrier during pregnancy. If left untreated after birth, bacteria can appear in the milk and infect the baby.
Staphylococcus often enters the body through abrasions and wounds. In a similar way, the pathogenic bacterium affects internal vital organs - the liver, heart, kidneys and genitourinary system.
Staphylococcus aureus usually comes from low-quality and fatty food, which is a favorable habitat and reproduction for this type of bacteria. Also, pathogenic microorganisms can exist in the intestines and become active after a decrease in immunity.
Symptoms
Symptoms in men and women depend on where the pathogenic bacteria enters the body. Signs of infection can resemble various other diseases, and people often confuse them with symptoms of a common sore throat or runny nose. A person infected with staphylococci may have the following symptoms:
- skin lesions on the face, nose, ear and other parts of the body: acne, dermatitis, folliculitis, boils, eczema, blepharitis;
- severe cough;
- sore and sore throat;
- cutting pain when urinating in the lower abdomen and lower back;
- runny nose.
In children, practically no manifestations of staphylococcal infections are observed. Epidermal and saprophytic types of bacteria do not pose a threat to the child’s body, because the immune system is able to control the proliferation of pathogenic microorganisms, protecting against diseases.
The most formidable is Staphylococcus aureus, which manifests itself with more serious symptoms. Symptoms depend on the age of the child and the state of his immunity. Newborns may develop serious complications that are life-threatening. At the age of 1 to 3 years, the infection also has serious consequences, since the child’s immunity is finally formed only after three years. After reaching this age, staphylococcal damage does not pose a serious threat, and the prognosis in most cases is favorable.
Staphylococcus aureus during pregnancy: how to distinguish normal from pathology
In obstetric practice, detection of Staphylococcus aureus in the fourth degree is considered to be a normal variant. In this situation, you can limit yourself to preventive measures: maintain the immune system, eat well, adhere to hygiene standards, and avoid skin trauma.
If Staphylococcus aureus in a smear during pregnancy is 104 or higher, then there is a risk of developing a staphylococcal infection. Based on the results of the smear and the general clinical picture, the woman’s condition is monitored or treatment is prescribed.
Important! Indicators of Staphylococcus aureus in the analysis, which exceed the norm tens of times, are the reason for the immediate prescription of antibacterial and immunostimulating therapy.
Diagnostics and norms
In order to identify a pathogenic microorganism in the body, it is necessary to conduct various studies:
- blood analysis;
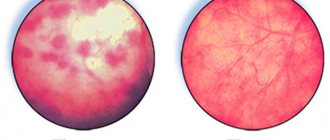
- culture of urine to detect increased levels of bacteria, proteins and leukocytes;
- analysis of other biomaterials: feces, vaginal smear, cerebrospinal fluid, etc.
When performing sowing, nutrient media for the biomaterial are selected to identify the type of bacteria and determine their sensitivity to certain medications. When staphylococcus is detected, a group of antibiotics is released to which pathogenic microorganisms are unstable. For example, Staphylococcus aureus cannot be cured using the penicillin group of antibacterial agents.
Often, when urine is cultured, cystitis caused by staphylococci is diagnosed in young and adult women. Due to the fact that the examination of the tests taken takes from 7 to 10 days, treatment is started immediately with broad-spectrum antibiotics, and after receiving the result, the therapy is adjusted.
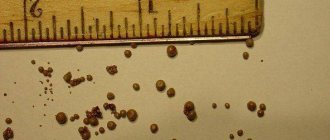
For example, when pregnant women submit urine for bacteriological culture, the interpretation of the results may be as follows:
- the norm is less than 1000 colony-forming units per milliliter;
- Repeated studies are required when the concentration is up to 10 to 5 CFU/ml;
- there is an infectious-inflammatory process - more than 100,000 CFU/ml.
How to get tested correctly
It is important to correctly collect urine for analysis.
In order to find staphylococcus in urine you need:
- Collect it in the morning on an empty stomach.
- Before collection, you should wash the external genitalia in the morning, followed by wiping until the skin is completely dry.
- As a container, you should use a special sterile container sold in pharmacies.
- For the study, the middle portion of the material is important - the first and last are poured into the toilet.
- When urinating, it is important that no discharge from the vagina or anus gets into the container.
- It is also necessary to ensure that urine does not get on the mucous membrane of the lips.
Treatment
If staphylococcus is detected in the urine, treatment is immediately prescribed, since any delay can lead to the progression of the infection process up the body, affecting internal organs, skin, bones and blood. To do this, a certain type of antibacterial drug is used, which is chosen after a thorough examination of the pathogenic bacteria.
With conventional drug treatment, the doctor prescribes the following drugs:
- Amoxicillin - to destroy pathogenic bacteria, suppress their growth and reproduction;
- Cloxacillin - to prevent the process of division of microorganisms;
- Vancomycin - to eliminate infection by destroying the membrane walls;
- Cephalexin - to reduce the synthesis of pathogenic microorganism cells;
- Oxacillin - to destroy staphylococcal bacteria in the later stages of division;
- Cefotaxime - to suppress growth and reproduction rate.
The patient is prescribed immunomodulatory agents that stimulate the body's protective function against a certain type of staphylococcus, and medications to normalize the microflora. Women are often prescribed anti-inflammatory drugs and are advised to pay great attention to vaginal sanitation with antiseptic drugs.
Sulfonamides are often used together with antibacterial drugs. In some cases, bacteriophages are prescribed - viruses that multiply inside pathogenic bacteria, destroying them. This group of drugs does not have a negative effect on the body, since after fulfilling their purpose they die on their own.
All doctor's orders must be strictly followed. To cure a pathogenic bacterium, it is necessary to undergo a full course of treatment to prevent the microorganisms from developing resistance to the medications used. All treatment measures are recommended to be carried out under the close supervision of a specialist. After a course of therapy, the patient should re-submit urine for bacteriological culture to ensure the destruction of pathogenic colonies.
Prevention
Staphylococcal infection is fraught with complications and long-term, expensive treatment, so it is recommended to carry out preventive measures on an ongoing basis. It is necessary to lead a healthy lifestyle, observe the rules of personal intimate hygiene, eat right and get rid of bad habits.
To minimize the risk of infection by pathogenic bacteria, it is recommended to follow certain rules:
- cover the slightest damage to the skin with iodine or brilliant green;
- avoid temperature changes that cause overheating and hypothermia;
- adhere to strict rules of intimate hygiene to avoid accidental entry of staphylococcal bacteria from the intestines into the cervical canal;
- periodically take tests to promptly detect staphylococcus in the body;
- maintain immunity at the proper level, taking immunomodulatory drugs if necessary;
- do not use antibacterial agents without a doctor’s prescription;
- do not have unprotected sex and avoid casual sex;
- If gynecological inflammation is detected, promptly treat;
- do not use synthetic underwear.
The greatest danger hangs over women during pregnancy, who must follow all the preventive measures presented. By following simple recommendations, you can maintain a healthy microflora in the body, thanks to which beneficial bacteria promptly suppress the increase in pathogenic ones.
A small number of staphylococci do not pose a serious threat to health, therefore, even if they are detected, treatment is not required. If the concentration is too high, then the patient needs immediate treatment with antibacterial agents. It is highly not recommended to self-medicate, since a certain type of pathogenic bacteria can be resistant to certain drugs.
Preventive actions
Staphylococcus is not easy to treat, so doctors recommend adhering to the basic rules of prevention, which will help prevent pathogenic bacteria from damaging the body. Thus, preventive measures include:
- balanced and rational nutrition;
- maintaining personal hygiene;
- regular exposure to fresh air;
- performing dosed physical activity;
- daily wet cleaning of the room and ventilation.
To prevent staphylococcus from becoming more active, it is necessary to avoid prolonged exposure to the cold, and also wear loose-fitting clothes, preferably made from natural fabrics. Prevention of the development of pathogenic bacteria includes special diagnosis and treatment of various acute and chronic pathologies. In addition, it is important to periodically visit an antenatal clinic, and during pregnancy undergo the required tests in a timely manner and monitor the condition of the mammary glands.
Source: etopochki.ru