Disruption of the excretory tract in childhood is usually a congenital condition. Such pathologies are very dangerous. After all, they directly affect the functioning of the kidneys. Moreover, since in children the kidneys grow, like all other organs, pathologies of the excretory tract grossly disrupt the natural growth process. One of the most serious diseases is megaureter in children.
About the disease
In the most general explanation, “megaureter” should be understood as a pathology of expansion of the transverse part of the ureter in its different parts. A more extensive description of the pathology includes:
- unnatural curvature of the ureter;
- low tone of the smooth muscles of the ureter;
- different cellular composition of the ureter;
- abnormalities in the development of ureteral cells;
- different biochemical composition of the organ;
- oncology of the ureter (benign and malignant tumors);
- associated anomalies - hyperplasia (tumor) of the tissues surrounding the ureter; duplication of the ureter or kidney; absence of one ureter or kidney; pathological dilatation of the posterior part of the urethra and renal pelvis;
- pathological narrowing of the ureter at the border of the entrances to the pelvis and bladder (ureteral obstruction).
The defect can be detected in the fetus in the last months of development, in the newborn, in children and in adults. Pathology can develop latently - a genetically and physiologically inherent predisposition can manifest itself at a certain age:
- most often these are children 2-3 years old;
- less often - adolescents from 10 to 15 years old;
- very rarely - adults.
Both women and men suffer from the pathology, but in men this disease manifests itself more severely. The defect can be treated non-surgically before the end of the prepubertal period, especially for infants and young children. Unsuccessful treatment of an illness is the basis for establishing disability. The decision to assign a disability category is made by a special medical commission.
The normal cross-section of the ureter in newborn boys is 3-5 mm, in girls 4-6 mm. Anything above this value is pathological. Normally, the ureter maintains its diameter throughout its entire length.
Expansion of the tubular process
The walls of the ureter have a three-layer structure, which helps urine move slowly to the bladder. The outer muscular layer includes nerve and collagen fibers that help move urine up to five contractions per minute. As the size of the ureter increases, contractile force begins to decrease, movement of urine becomes difficult, and the patient's intrarenal pressure increases. Prolonged stagnation of urine provokes the onset of infection, which only worsens the person’s condition. If treatment of the lesion is not started in a timely manner, then problems with the functioning of the kidneys will soon arise.
Often, infectious processes in the ureter only increase the expansion of the organ. Enlargement of the ureter and renal pelvis is diagnosed using ultrasound examination of the fetus.
If after birth the child does not have a megaureter, then expansion of the tubular organs will not occur in the future. In a normal state, the diameter of the ureter does not exceed 5 mm; if an expansion was detected during the examination, the doctor prescribes a more extensive examination of other internal organs.
In adolescents with this form of damage, the following symptoms most often present: the presence of blood in the urine, incontinence, complaints of persistent pain in the abdomen and lower back, and the formation of stones in the urinary organs.
Causes
The immediate cause of megaureter is neuromuscular dysplasia (pathological formation of ureteral tissue). Pathologies of abnormal development of organs are most often a consequence of a person’s genetic predisposition to such a phenomenon. Poor heredity can cause the appearance of megaureter and other anomalies of the genitourinary system.
However, hereditary predisposition is not the only factor influencing the appearance of the defect. There are reasons due to the lifestyle of the child’s mother:
- an unhealthy diet can lead to abnormal development of fetal organs;
- bad habits of the mother can also affect the development of the fetus - tobacco, alcohol, drugs;
- dangerous infectious diseases can cause phenotypic abnormalities of fetal development;
- working in production with toxic substances will be dangerous to the health of an unborn child;
- metabolic disorders in the mother's body;
- autoimmune reactions, diseases in the mother’s body during gestation.
The above reasons are largely interdependent. For example, toxins that enter the blood of a pregnant woman in a hazardous workplace can cause an autoimmune disease. An autoimmune disease, in turn, can lead to changes in blood composition and disruption of normal metabolic reactions. Metabolic dysfunction in the mother's body will cause abnormal development of the fetus.
Urethritis is an infectious or non-infectious lesion of the walls of the urethra, which, if left untreated, can develop into serious complications. You can find out how children are treated, as well as the main causes of this disease.
An organ formed under the influence of genetic and phenotypic factors becomes vulnerable to dynamic effects. For example, an infection that has entered the child’s genitourinary system can cause inflammation of the ureter and damage it due to excess urine pressure.
Relative readings
A relative indication is a disease that is at stage 1 of development and does not pose a particular danger to a person’s life, but significantly affects his condition. For example, it brings fatigue, headaches, reduces performance, and provokes nausea.
The ureter in this case is minimally dilated. The patient has time during which he can take a course of effective medications, which will help prevent even further expansion of the ureter. This will help prepare the patient's body for surgery.
Varieties
The typology of megaureter involves dividing the defect into 4 types:
- Obstructive megaureter. A pathological narrowing (obstruction) forms at the junction of the ureter and bladder. Insufficient urine flow creates excess pressure on the walls of the organ and cripples it.
- Refluxing megaureter. Reflux, in this case, should be understood as the physical process of fluid returning against its normal course. Abnormal development of muscle tissue, underdevelopment of the closing valve at the ureteral anastomosis can cause urine backflow. The resulting excess pressure damages the tissue of the ureter, stretching it.
- Mixed (obstructive-refluxing) is a megaureter that has signs of obstruction and reflux.
- Cystic megaureter. Urine accumulates in the bladder; if there is no outflow, it will begin to create excess pressure. Fluid from the bladder destroys the valve at the ureteral anastomosis and returns urine back.
Depending on the cause that caused the defect, it is classified as follows: congenital and acquired. The classification, aimed at assessing the severity of the disease, involves division into three stages - mild (up to 70% of urine is excreted), moderate (40 to 70% of urine is excreted), severe (up to 40% of urine is excreted).
Stages of development of the disease
There are three stages depending on the extent of the damage.
- Hidden, achalasia. This is a compensation process. If it is detected, the patient - infant or adult - is placed under observation. The child is examined for two to six months. It is believed that the genitourinary organs are not yet mature at birth and can independently normalize during this period;
- Progression, actually megaureter.
- The development of kidney disorders due to improper outflow of fluid from the body.
Each stage develops slowly, as it is associated with purely physical factors - stretching of the walls due to urine pressure. This is not a very optimistic trend, since sometimes difficulties arise in diagnosing the disease.
Symptoms
The most common and easily diagnosed symptom of megaureter is biphasic urination. The first occurs in the form of a small portion of urine, the second is more intense, with a large amount of urine. Urine released during the second phase of urination may contain sediment, blood, pus, and have an unpleasant, pungent odor.
Other symptoms you can add:
- dryness and pallor of the skin;
- temperature increase - insignificant (up to 37.4 ° C) if there is no pathogenic invasion, and significant (above 37.4 ° C) if there is;
- high blood pressure;
- vomit;
- thirst;
- unpleasant odor of ammonia from the child’s mouth;
- bloating; the child responds negatively to palpation.
You must understand that secondary symptoms do not say anything on their own; the first thing that should alert the diagnostician is biphasic urination.
Diagnostics
Medical statistics show that the majority of detected pathologies of the fetal urogenital system are diagnosed during a routine ultrasound of pregnant women in the third trimester. This fact makes ultrasound diagnostics the fastest method for detecting defects. In addition to conventional ultrasound, a version with Lasix loading is used - the patient is given a diuretic (Lasix) and the patency of the ureter is monitored.
Other ways to detect a defect:
- Radioisotope and radiocontrast methods . This is a family of numerous methods based on the introduction into the blood of a substance that has:
- ability to reflect X-ray radiation;
- expose a special film to radioactive radiation. Substances are excreted in the urine, and therefore it is easiest to use them to check the functioning of the organs of the genitourinary system.
- Laboratory research methods. Routine and advanced clinical blood and urine tests can show an abnormality in the functioning of the urogenital system.
Megaureter is a defect that is often accompanied by an infectious disease. An infection can cause a defect, but the megaureter itself also contributes to the occurrence of infectious diseases - it is easier for pathogens to enter the kidneys through an abnormal ureter.
Carrying out electronic urography
An effective diagnostic method is urography, which does not cause discomfort in the patient and helps to obtain accurate information about the condition and functioning of organs, the location of the lesion, the anatomical structure of the ureters, as well as dilated areas.
Contraindications to the procedure are severe kidney disease, nervous breakdowns, problems with concentration abilities and other processes in which, due to the accumulation of large amounts of urine in the blood, it is impossible to accurately determine the clinical picture of the disease.
Women carrying a child are prohibited from performing the procedure or only for special indications. For example, if there is a suspicion of malignant or benign formations in the ureter.
Treatment
Megaureter is treated primarily surgically. However, newborns are patients who undergo rapid physiological development. Sometimes it is enough to restore normal nutrition to the child’s body for the ureter to return to normal. For treatment, low-traumatic or minimally invasive methods of treating megaureter are also used - bougienage and balloon dilatation. But according to the general opinion of experts, they are ineffective.
Surgery
The decision on surgical intervention is made by the council. The basis for the operation is the ascertainment of the loss of function of the newborn kidney. Surgeons have found 4 ways to solve the problem of megaureter:
- Reconstruction. The surgeon performs a resection (truncation) of the diseased organ, and then suturing it so that it begins to perform its function normally. There are many nominal operations of this type. The most successful operation for reconstruction of the ureter is called the development of N. A. Lopatkin-L. N. Lopatkina. It contains a successful anti-reflux idea. The authors of the operation went by duplicating the ureters - both ureters retain nutrition to the body. This means that the abnormal ureter will not lose its ability to peristalsis and will be a useful addition to its healthy duplicate.
- Implantation. This type of surgery involves using part of the small intestine to create a ureter. The operation is used in cases where the patient has organ agenesis.
- Anastomosis. The operation involves removing the abnormal (dilated) section of the ureter and then joining the normal parts by longitudinal or lateral connection (suturing). The operation is used in cases where neuromuscular dysplasia of the ureter has only partially affected the organ.
- Ureterocutaneostomy. This type of surgery involves bringing the ureter out. The operation was developed a long time ago and is criticized by the modern medical community for increasing the threat of infectious infection to the patient. However, it has undeniable advantages, the main one of which is immediate assistance to a patient in serious condition.
In modern urology, a surgical solution to the problem of megaureter by creating a normally functioning organ is usually called “modeling”.
Megaureter therapy is not limited to a successful operation. To fully restore the function of the ureter, long-term drug treatment and medical supervision are required.
Minimally invasive methods
To treat megaureter in urology, in addition to surgical methods, “minimally invasive treatment methods” are also used. Let's look at them in more detail:
- Bougienage. A probe (stent, catheter) is inserted into the ureter. The presence of a probe prevents urine from accumulating in abnormal parts of the organ, and it leaves the body unhindered.
- Balloon dilatation. For this operation, a special hollow, flexible catheter (stent) is used. The stent contains a container of gas or liquid. The stent operator can use this capacity to adjust the volume of the stent at a specific location. A stent is inserted into the ureter, identifying the location where the pathological narrowing of the organ coincides with the catheter capacity. The operator supplies liquid or gas into the cavity, the catheter expands and the narrowing is removed.
- Endoscopic therapy (introduction of medical gels and removal of tissue fragments). Endoscope is an optical probe. It can be used to detect pathological areas of narrowing of the ureter. If the situation allows, an endoscope can be used to remove tissue growth or introduce a medical volume-forming gel.
Minimally invasive methods, according to experts, are a temporary solution that has a weak therapeutic effect. They are significantly inferior in effectiveness to surgical treatment. But in the case of therapy for newborns, they have a greater chance of success - the child is in the stage of active growth, the metabolic rate is very high. The use of one or another minimally invasive treatment method can lead not to a temporary, but to a full-fledged therapeutic result.
Why is megaureter dangerous?
Because of this syndrome, irreversible changes often occur:
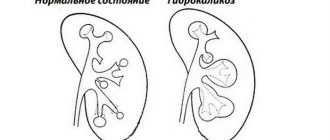
- the pelvis dilates;
- hemodynamics are impaired;
- pressure in the kidney cavity increases;
- organ function gradually decreases;
- chronic failure develops;
- arterial hypertension develops;
- Infections are added, leading to chronic diseases and even sepsis.
If the inflammatory process lasts for a long time, the renal parenchyma becomes scarred and nephrosclerosis develops.
Forecast
Megaureter is a problematic disease that requires long-term treatment (1-2 years). If the conditions of clinical observation of the child’s condition are met, the prognosis in 80% of cases is positive, that is, it assumes a complete cure of the patient. The remaining 20% of patients have a conditionally positive prognosis - their genitourinary system will work in a limited mode. A state assistance program is provided for such patients.
You can also get acquainted with the opinion of a specialist by watching this video about the treatment of hydronephrosis in children, how this disease is detected.
Recovery after surgery
The patient's recovery continues for quite a long time. Evaluation of the results of the operation will be long-term. Doctors will judge the quality and effectiveness of the surgical intervention only after several years have passed after the operation itself.
It is important to remember that there is nothing scary or dangerous about the operation. You should not be afraid of it and put it off for some time. According to statistics, success with surgical intervention is observed in 90% of patients. The sooner treatment for the disease is started, the higher the chance of getting a positive result.
When treating ureteral enlargement, special attention should be paid to its severity. The severity will be determined after receiving the results of clinical diagnostics and a multifactorial assessment by a physician. In normal cases of ureteral dilatation, the patient's condition will recover within a few weeks after the operation. In more complex cases, the patient will need 10-15 weeks for rehabilitation.
To avoid dilation of the ureter, it is important to monitor the condition of the body and promptly treat diseases of the genitourinary system. It is also important to stop taking large amounts of fluid if the urinary system does not have time to remove it from the body in time.