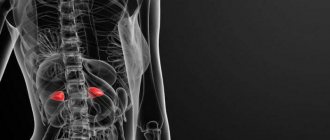
Kidney-related diseases are quite common in the world. There are at least a hundred types of diseases that affect these organs of the excretory system. Among such diseases, nephrotic and nephritic syndromes, which differ from each other, are distinguished.
Both syndromes are concomitant phenomena in many renal diseases, including glomerulonephritis. With this disease, the glomerular apparatus becomes inflamed, resulting in the development of renal failure.
What is nephrotic syndrome?
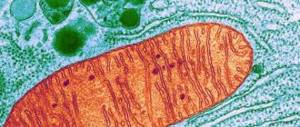
Nephrotic syndrome occurs when tiny blood vessels in the kidneys, called glomeruli, do not work properly. The glomeruli typically act as filters, removing water and waste from the blood and sending them to the bladder as urine, allowing blood cells and proteins to remain in the blood. If the glomeruli are damaged, protein can leak through the filter system into the urine.
Nephrotic syndrome includes the following symptoms:
- Albuminuria
: high levels of protein in the urine - Hypoalbuminemia
: low levels of a protein called albumin in the blood - Hyperlipidemia
: increased levels of fat and cholesterol in the blood
Effective treatments
Therapy of nephritic syndrome involves examining the patient to identify the underlying disease that caused the pathology. A differential approach to diagnosis is based on the use of an instrumental method and is carried out through laboratory analysis. Diagnostic measures:
- blood sampling for biochemical composition, detection of anemia, leukocytosis, ESR rate;
- general urine analysis to determine hematuria, density of biological material, protein, leukocytes, protein casts and cell elements;
- Ultrasound of the kidneys;
- immunogram.
Treatment of the anomaly is aimed at eliminating the disease that caused it, taking into account the form of the clinical course. Acute nephritic syndrome requires hospitalization, assistance is aimed at removing the patient from a serious condition: eliminating edema, hematuria, azotemia, proteinuria.
The chronic form does not require emergency hospitalization of the patient; planned hospitalization once a year is sufficient. It is carried out to adopt a series of procedures that promote final recovery and eliminate relapse.
Review of drugs
Therapy is carried out using:
- Mild diuretics - Midamor, Spironolactone, Triamterene. With an average degree - “Hypothiazide”, “Chlorthalidone”, “Metozolon”. Potent diuretics - Torasemide, Furosemide, Xipamide. The choice is determined by the severity of edema. To normalize blood pressure, Metazolone, Indapamide, and ethacrynic acid are indicated.
- Calcium-containing preparations – “Kantaren”.
- Cytostatic agents – “Azathioprine”, “Cyclophosphamide”. "Leukeran".
- Anticoagulants that prevent the formation of blood clots - Heparin, Antithrombin III, Protein C.
- For infectious bacterial etiology, antibiotics “Amoxicillin” and “Penicillin” are prescribed if the causative agent is enterococcus. For purulent inflammatory processes in the kidneys, Cephalexin, Tsiprolet, and Klaforan are used. The chronic form of nephritic syndrome is treated with Moxifloxacin, Levofloxacin, Nolicin.
- Vitamin-mineral complex – “Rutin”, ascorbic acid.
If necessary, sedative and antihistamine drugs are prescribed.
Folk remedies
Recommendations of alternative medicine can be included in the complex of conservative therapy. Traditional recipes will enhance the effect of medications, and it is also advisable to use them for preventive purposes. To treat pathology, decoctions and infusions based on herbal components are used:
- Herbal mixture consisting of immortelle, calendula flowers, St. John's wort in equal parts (two tablespoons per 0.5 liter of water). Prepare the decoction in a steam bath for 15 minutes, take 250 ml in the morning on an empty stomach and in the evening three hours before bedtime.
- Chamomile, buckthorn bark (20 grams of each ingredient), pour two glasses of boiling water, infuse in a thermos for 2 hours, drink in small portions throughout the day.
- Dried rose hips (2 tablespoons per 300 ml of water) are boiled over low heat for 10 minutes, the resulting decoction is divided into two doses and consumed in the morning and evening.
- Brew fresh birch leaves 150 grams per 0.5 liter of boiling water in a closed container, leave for 4 hours, filter, take 100 ml 5 times at the same time interval.
- Brew horsetail and chicory flowers (1 tablespoon each) in 0.5 liters of water, let steep for 60 minutes, drink in three doses throughout the day.
For the treatment of children, the number of components should be halved; age and allergic reaction to the ingredients of the tinctures should be taken into account.
Nephrotic syndrome - symptoms
Symptoms of nephrotic syndrome include:
- swelling of the ankles, feet and legs
- fatigue
- loss of appetite
- weight gain
- foamy urine
The foaming that occurs due to the presence of protein in the urine is different from the bubbles that can be seen in normal urine. Foam appears in layers of small to medium-sized bubbles that do not dissipate. In contrast, normal urine may contain a single layer of larger bubbles that soon disappear.
Patients with nephrotic syndrome may notice swelling in the legs after standing for long periods of time or puffiness around the eyes after waking up. As the disease progresses, there is constant swelling of the lower extremities and other parts of the body.
Main symptoms of the disease
The clinical picture of the pathology has certain features that make it possible to distinguish nephritic syndrome from all others. There are both general symptoms (associated with damage to the whole body) and local ones (affecting only the kidneys).
Manifestations of the first group include:
- dyspepsia (nausea, vomiting, heartburn without connection with meals);
- general intoxication (headaches in the temporal region, weakness, lethargy, drowsiness);
- an increase in blood pressure by 20–40 mmHg above normal;
- tendency to colds.
Typically for local symptoms:
- the presence of pain and swelling in the lumbar region;
- change in color and turbidity of urine (redness and appearance of foreign impurities);
- swelling of the face (especially eyelids, cheeks and neck);
- decrease in the volume of urine excreted (oliguria).
One of my patients had an atypical course of the disease. The man was completely free of all signs of intoxication and blood was detected in his urine only once. Since the patient suffered from arterial hypertension, other doctors did not pay attention to the increase in blood pressure. It was possible to identify the presence of nephritic syndrome only after additional examination of the kidneys.
Nephrotic syndrome - causes
Doctors classify the cause of nephrotic syndrome as primary or secondary.
Primary cause
The primary causes of nephrotic syndrome are conditions that affect only the kidneys. Examples of primary causes include:
- Focal segmental glomerulosclerosis (FSGS)
: In FSGS, scarring occurs in specific areas of the glomeruli. FSGS occurs more often in men than women and has a higher prevalence among African Americans. - Membranous nephropathy
: Immune complexes accumulate in the glomeruli, causing damage. - Minimal change disease (MCD)
: Damage to the glomeruli can only be seen with a very powerful microscope. MCD is the most common cause of nephrotic syndrome in children. In adults, allergies, infections, or certain medications can cause MCD. - Membranoproliferative glomerulonephritis (MPGN)
: The immune system attacks kidney cells, damaging the glomeruli. Sometimes another disease, such as hepatitis C, causes MPGN.
Secondary cause
Secondary causes are conditions that affect the entire body, leading to nephrotic syndrome. Here are some examples of secondary causes:
- diabetes
- lupus
- infections such as hepatitis B, C or HIV
- cancers such as Hodgkin's disease
Nephritic syndrome and its types
Nephritic syndrome is a complex of characteristic symptoms that develops against the background of inflammatory kidney diseases. The syndrome is accompanied by damage to the renal glomeruli. The glomerulus is a structural unit of kidney tissue and is responsible for filtering blood plasma and the formation of primary urine.
In the International Classification of Diseases, 10th revision (ICD 10), this pathology is identified as a separate unit. According to the definition of the World Health Organization (WHO), nephritic syndrome can be primary or develop against the background of another disease.
There are several forms of pathology:
- Acute nephritic syndrome develops against the background of acute inflammatory kidney diseases (glomerulonephritis). The mechanism of development is based on swelling and inflammation of the renal glomeruli. The formation of the process takes from one to several days.
- Chronic nephritic syndrome usually develops against the background of chronic glomerulonephritis or other kidney diseases. In the chronic form, sclerosis (replacement with connective tissue) of the renal glomeruli occurs. The pathology is characterized by slow progression (from several months to several years). Symptoms are mild, unexpressed, and may appear periodically and then disappear.
A special place is occupied by the rapidly progressing form of pathology. Its symptoms and course are in many ways similar to the acute form, however, renal failure develops within a few months.
Nephrotic syndrome - diagnosis
In addition to a physical examination and history, a doctor will usually diagnose nephrotic syndrome using the following tests:
- Urinalysis
: This test looks for elevated levels of protein in the urine. - Blood test
: This test helps reveal the levels of albumin, cholesterol, and other blood components. - Kidney biopsy
: This is ordered to look for microscopic changes in the kidney. - Ultrasound: This type of imaging is used to see what the kidneys look like.
Preventive actions
Prevention of this condition is the correct and timely treatment of infectious diseases of streptococcal etiology (sore throat, tonsillitis, etc.) in childhood. Specific preventive measures have not been developed.
In conclusion, we note that nephritic syndrome with glomerulonephritis can be practically asymptomatic during the onset of the disease.
The disease is most often detected already during the peak period - when irreversible changes have formed in the kidneys, which causes a number of symptoms. A major role in the occurrence of this pathology is assigned to infectious causes, and especially chronic tonsillitis and tonsillitis in children.
Therefore, it is important to carry out timely and competent treatment of these diseases in order to avoid the development of kidney damage.
The syndrome is quite easily diagnosed by modern medicine, but, unfortunately, the treatment of this pathology is limited only to stopping and preventing further damage to the glomerular apparatus of the kidney.
Nephrotic syndrome - treatment
Treatment for nephrotic syndrome will depend on the cause. However, therapy usually involves medications to treat the underlying cause as well as dietary changes.
Some drug treatments:
- Steroids
: Doctors may prescribe hormonal medications to treat MCD in children or adults. - Diuretics
: Help the body remove excess fluid and reduce swelling. - Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers
: help control blood pressure and reduce protein in the urine. - Immunosuppressive drugs
: Help with conditions such as FSGS, in which the immune system attacks the glomeruli. - Statins
: lower cholesterol levels. - Pneumococcal vaccine.
Dietary changes help treat nephrotic syndrome:
- sodium restriction
- eating less protein
- reducing intake of saturated fat and cholesterol
Manifestation of the clinical picture
The symptoms of nephritic syndrome have several characteristic features and directly depend on the stage of the disease. The pathology also has a number of uncharacteristic signs, these include:
- vomiting, nausea;
- impaired urine flow and constant thirst;
- significant loss of appetite and development of anorexia.
If you divide the symptoms into stages, you can track the stages of development of pathological changes in the glomeruli of the kidneys.
Stages of development
At the initial stage of development of pathology, a person develops hematuria (urine changes color and red blood cells appear in it).
Weakness, increased fatigue, and signs of scarlet fever are present.
Later, hematuria develops into macrohematuria, with this phenomenon the urine has the color of meat slop. Swelling appears on the face, neck, eyelids, and legs. Swelling is a concern in the evening and often occurs in the morning.
Gradually the person gains weight. This increase is considered pathological. The level of blood pressure also increases, and hypertension develops.
At the 3rd, final stage of development of nephritic syndrome, a person is concerned about a decrease in the volume of urine excreted, while there is constant thirst. There is vomiting, nausea, severe pain in the head, and increased sweating.
When complications arise, symptoms of acute or chronic renal failure occur. The color of the skin changes, the patient refuses to eat, and is tormented by severe nausea and vomiting.
Urine passes poorly or does not pass at all, and fluid accumulates in the body, which can lead to swelling of the lungs or brain.
Complications
Complications of nephrotic syndrome often result from the loss of certain proteins in the urine. The body requires proteins to fight infections or control blood clotting.
Other complications of nephrotic syndrome may include:
- coronary artery diseases
- high blood pressure
- anemia, which occurs when there is a shortage of healthy red blood cells
- hypothyroidism, which occurs when the thyroid gland is unable to produce enough thyroid hormones
- temporary decrease in kidney function
Mechanism of development of nephritic symptom
The pathogenesis of nephritic syndrome is based on an immune inflammatory process. The cause of pathology is antigens that enter the human body from the external environment or are formed in the tissues of internal organs. At first they circulate freely in the bloodstream, but gradually penetrate into various structures of the kidneys. The invasion of foreign proteins activates the immune system - increased production of antibodies begins to neutralize and destroy infectious agents.
The formed antigen-antibody complexes settle under the epithelial cells on the semipermeable membrane of the glomerular capillaries. Activation occurs of a complex of complex proteins that are constantly present inside the bloodstream. They represent a cascade system of proteolytic enzymes and are designed to protect against the negative effects of foreign agents. This protection serves as an important component in shaping the immune system's response.
With nephritic syndrome, red blood cells appear in the urine
In nephritic syndrome, complement serves as a humoral mediator of the inflammatory process and is activated by the cleavage or attachment of individual sections of peptides. This condition provokes:
- damage to the basement membrane of the glomerular capillaries;
- includes cellular factors of the pathological mechanism of acute glomerulonephritis (neutrophils, T-lymphocytes, macrophages, endothelial cells).
- involves peptide informative molecules cytokines (biologically active substances that are produced by immune cells and provide communication between them).
Increased basement membrane permeability allows red blood cells, proteins, and metabolites to leak into secondary urine. An increase in protein concentration helps to reduce plasma pressure, its release into the intracellular space, and the occurrence of swelling.
Renin, a hormone that regulates vascular tone, is produced in excess due to an imbalance in the speed of circulating blood. This process is the main factor in the occurrence of arterial hypertension and increased renal pressure.
Forecast
Thanks to timely differential diagnosis of nephrotic syndrome, patients have a better chance of a speedy recovery without complications. In general, the prognosis for patients is favorable. It is important to seek help from specialists at the first symptoms of the disease - competent therapy will help normalize kidney function within a couple of months. The course of the disease largely depends on the stage of the disease, the age of the patient and the presence of chronic diseases, which can aggravate the clinical picture.
In most cases, elimination of the inflammatory process automatically entails stabilization of blood pressure, but this only happens if the cause of hypertension was kidney problems, and not some other disease accompanied by the same symptom.
In the course of nephritic syndrome associated with serious complications (uremic coma, acute heart failure, cerebrovascular accident, etc.), the prognosis is disappointing. Among the most common consequences, it is worth noting severe anemia and repeated hypertensive crises.
Is there a difference between nephritis and nephrosis
As already noted, nephritic and nephrotic syndromes are different sets of clinical signs that manifest themselves during the development of renal pathology. These two conditions have similar features and occur against the background of existing disorders or infectious lesions. Since both pathological processes have a common localization, the symptoms are almost the same for nephritic and nephrotic syndrome. The differences will lie in test results and other signs of damage to the excretory system. As for the general symptoms, the course of nephrotic syndrome is accompanied by swelling, general weakness, back pain and pallor.
Edema
Massive and prolonged albuminuria in a patient with NS ultimately inevitably causes hypoproteinemia, since protein loss exceeds the intensity of its synthesis. Hypoproteinemia leads to disruption of the Starling equilibrium between hydrodynamic, filtration and colloid-osmotic pressure. This leads to a predominance of fluid outflow from the arterial bed over inflow. Edema begins to appear when the plasma albumin level is below 27 g/l, and always develops if hypoalbuminemia reaches 18 g/l.
Secondary hyperaldosteronism, typical of NS, also plays an important role in the pathogenesis of edema. As a result, sodium, and therefore water, is retained in the body, although there is hyponatremia in the blood.
Hypoproteinemia
The main cause of hypoproteinemia in patients with NS is large losses of albumin in the urine and their movement into tissues. In addition, increased catabolism of albumin and disruption of the protein-synthesizing function of the liver are important. The decrease in the content of γ-globulins in the blood of patients is primarily associated with a violation of their synthesis. Hypoalbuminemia and hypovolemia, deficiency of anticoagulants - antithrombin III and proteins C and S, hyperfibrinogenemia, hyperlipidemia pose a threat to thrombotic disorders in patients with MINS.