Hepatorenal syndrome is the final stage of a sequence of reductions in renal perfusion caused by severe liver damage. Hepatorenal syndrome is a diagnosis of exclusion and is associated with a dismal prognosis. During the 19th century, Frerichs and Flint made the original description of impaired renal function. In the 1950s, clinical descriptions by Sherlock, Popper, and Vesin emphasized the functional nature of the syndrome, the coexistence of systemic circulatory disorders, and its dismal prognosis. Over the next two decades, research has shown that renal failure arises from renal vasoconstriction and intense systemic arteriolar vasodilation, leading to decreased systemic vascular resistance and hypotension.
In HRS, the histological appearance of the kidneys is normal, and they often resume normal function after liver transplantation. This makes hepatorenal syndrome a unique pathophysiological disorder that provides an opportunity to study the interactions between the vasoconstrictor and vasodilator systems of the renal circulatory system.
These studies also include those related to the renin-angiotensin-aldosterone system (RAAS), the sympathetic nervous system (SNS), and the role of renal prostaglandins (RPs). There are strong associations between spontaneous bacterial peritonitis (SBP) and HRS, and the use of vasopressin analogs with volume expanders in management and prevention is known. Although a similar syndrome occurs in acute renal failure, HRS is usually described in the context of chronic liver disease. Despite some encouraging studies of new pharmacological treatments, the development of cardiovascular disease in people with cirrhosis portends a grim prognosis; kidney failure is usually irreversible unless transplanted.
Acute renal failure (ARF) has been proposed to characterize renal dysfunction in patients with cirrhosis. In this case, stage 1 HRS will be classified as an increase in serum creatinine level by 0.3 mg or an increase of 50%, while stages 2 and 3 will be two and three times higher.
What is hepatorenal syndrome?
Hepatorenal syndrome ( HRS ) is a form of kidney dysfunction that occurs in people with advanced liver disease. Individuals with hepatorenal syndrome do not have any specific cause of kidney dysfunction, and the kidneys themselves are not structurally damaged. Thus, hepatorenal syndrome can be called a “functional” form of renal failure. In fact, if the kidney of a person with HRS were transplanted into another healthy person, it would function normally.
GRS is divided into two different types. Type I is a rapidly progressive condition that leads to kidney failure; Type II HRS does not have a rapid course and progresses slowly over weeks or months. Although hepatorenal syndrome occurs in people with liver disease, the exact cause of this condition is unknown.
Researchers note that people with the disorder have poor circulation. The arteries that circulate oxygenated blood from the lungs to the rest of the body (systemic circulation) dilate, unlike the kidney arteries, which narrow, causing decreased blood flow through the kidneys. Many sick people also have high blood pressure in the branches of the portal vein (portal hypertension), the main vein that carries blood from the intestines to the liver.
How is the treatment carried out?
The main principle that veterinarians adhere to when treating hepatic encephalopathy is symptomatic therapy. It is necessary to eliminate the manifestations of pathology by controlling the urea content and ammonia transformations in the intestinal wall.
Lowering the pH level in the intestinal tract reduces the production of an enzymatic substance, urease, which breaks down metabolic products into toxic substances. The basis of therapy is a properly selected diet. A diet for hepatic encephalopathy involves reducing the amount of protein components, which in turn reduces the production of the urease enzyme.
The first stage of treatment for hepatoencephalopathy is the restoration of water and electrolyte balance in the body, as well as the elimination of toxic substances from the body, preventing their adsorption by the walls of the intestinal tract. Depending on the cause that provoked the pathology, medications are prescribed.
If the cause of hepatic encephalopathy is a violation of the functional characteristics of the liver structures, it is necessary to reduce the administration of drugs. Acute stages of pathology involve the introduction of a starvation diet. In the future, the animal is allowed to give food in small portions at a strictly designated time. The body must obtain protein components from dairy and plant products.
It is forbidden to give the patient meat and fish products.
Medications used to treat hepatic encephalopathy:
- Antimicrobial agents - give good results for suppressing gram-negative microorganisms that produce urease;
- Enzymatic non-absorbable carbohydrates - artificially produced carbohydrates are resistant to enzymes of the gastrointestinal tract, are destroyed by bacterial microflora and reduce the activity of urease, provoking the transition of a toxic substance - ammonia, into neutral ammonium ions.
In the treatment of hepatoencephalopathy, cleansing enemas with a warm solution of electrolytes are used. This allows you to eliminate hardened stool and reduce the risk of intoxication of the body. Next, retention enemas are carried out with enzymatic non-absorbable carbohydrates and antimicrobial drugs.
In sick animals with diagnosed hepatic encephalopathy, ulcerative lesions of the intestinal walls of the digestive tract are often recorded. Therapy includes the prescription of medications that reduce acidity and promote healing of ulcers.
To eliminate the eruption of gastric contents against the background of intoxication, the animal is prescribed antiemetic drugs - Metoclopramide, Ondansetron. In the presence of convulsive phenomena, anticonvulsants are used. The pressure inside the skull is reduced by administering diuretics.
Prevention of dehydration of the body is carried out through infusion therapy. Violation of the water-salt balance provokes an exacerbation of hepatoencephalopathy against the background of an increase in the level of nitrogenous substances in the bloodstream. The pet must be weighed daily, its circumference and blood pressure measured.
After treatment, veterinary specialists recommend carrying out preventive examinations to determine the effectiveness of treatment. Research is carried out for infection of the urinary system, a biochemical blood test, measuring the amount of gases in the blood and monitoring bowel movements. An important aspect of the diagnostic examination is the measurement of body temperature.
Signs and symptoms
Patients with HRS have a variety of nonspecific symptoms, including:
- fatigue;
- abdominal pain;
- general poor health (malaise).
Those affected also have symptoms associated with advanced liver disease, including:
- accumulation of fluid in the abdominal cavity (ascites);
- yellowing of the skin and sclera of the eyes (jaundice);
- enlarged spleen (splenomegaly);
- enlarged liver (hepatomegaly).
Hepatorenal syndrome type I is characterized by a rapid decline in kidney function. The kidneys act as a filtration system, removing unwanted substances and excess fluid from the body. Symptoms of decreased kidney function include the accumulation of excess watery fluid in the spaces between tissues and organs, causing swelling in these areas, severely decreased urination, and the presence of elevated nitrogen waste products such as creatinine and BUN in the blood (azotemia). Type I HRS can progress to life-threatening kidney failure within a few days.
People with HRS type I are more likely to suffer from hepatic encephalopathy, a condition that occurs when the liver is unable to break down (metabolize) certain substances in the body. These substances pass through the bloodstream into the brain with toxic consequences. Hepatic encephalopathy may cause confusion, drowsiness, recognizable changes in judgment and other intellectual processes, and other psychological changes. It is also more common in acute liver failure from any cause.
Symptoms
The acute form of hepatorenal syndrome is characterized by a rapidly developing clinical picture and a sharp deterioration in the patient’s condition. The chronic form occurs in a more latent form, and the patient's condition worsens gradually.
In general, the following symptoms are characteristic of this pathological process:
- general weakness;
- increased fatigue;
- decreased appetite;
- yellowness of the skin;
- swelling in the legs and arms;
- upon palpation, the enlargement of the liver is clearly visible;
- red spots on the palms (“liver palms”);
- little urine output, and in more complex cases, no bladder emptying at all;
- decreased blood pressure;
- an increase in the volume of the abdomen due to the accumulation of fluid in it - ascites begins;
- increased dryness of the skin and mucous membranes;
- nausea, which in some cases is accompanied by vomiting;
- loss of appetite;
- enlarged spleen;
- dilated veins are clearly visible around the navel;
- Due to tension in the abdominal wall, an umbilical hernia may develop.
If you have at least a few symptoms from the clinical picture described above, you should immediately seek medical help. Under no circumstances should you take any medications or traditional medicine on your own. This will only worsen the situation and lead to death in any case.
Causes and risk factors
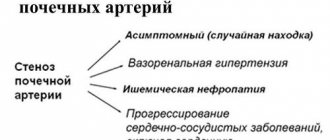
The exact cause of hepatorenal syndrome is unknown. The disease occurs in people with advanced liver disease, especially people who have cirrhosis of the liver. A characteristic feature in people with hepatorenal syndrome is a narrowing of the blood vessels supplying the kidneys (renal vasoconstriction), which leads to decreased blood flow to the kidneys, which ultimately impairs kidney function.
The cause of renal vasoconstriction is unknown. Researchers believe it is a complex interaction between several different factors, including high blood pressure in the liver's main vessels (portal hypertension), abnormalities in the physical factors that regulate blood flow (systemic hemodynamics), and activation of substances that cause blood vessels to constrict (vasoconstrictors). and suppression of substances that cause vasodilation (vasodilators).
The researchers also determined that cirrhotic cardiomyopathy may also contribute to the development of hepatorenal syndrome in some people. Cirrhotic cardiomyopathy refers to a dysfunction of the heart in people with cirrhosis of the liver. Cirrhotic cardiomyopathy causes decreased cardiac output (heart failure) and abnormal dilation of some arteries in the body.
Some patients with hepatorenal syndrome may have certain triggers that make patients with liver disease more likely to develop the disorder. These triggers are called precipitants. The most common trigger is spontaneous bacterial peritonitis (SBP), an infection of the thin membrane (peritoneum) that lines the abdominal cavity. SBP is a known complication in people with ascites and cirrhosis. Other common causes are acute blood loss from the gastrointestinal tract, low blood pressure and infection of any etiology.
Pathophysiology
The hallmark of HRS is renal vasoconstriction, although the pathogenesis is not fully understood. It is likely that multiple mechanisms are involved and there is an interaction between disturbances in systemic hemodynamics, activation of vasoconstrictor systems, and decreased activity of vasodilator systems. The hemodynamic pattern of patients is characterized by increased cardiac activity, low blood pressure, and decreased systemic vascular resistance. Renal vasoconstriction occurs in the absence of a decrease in cardiac output and blood volume, in contrast to most clinical conditions associated with renal hypoperfusion.
Although the pattern of increased renal vascular resistance and decreased peripheral resistance is characteristic of HRS, it also occurs in other conditions such as anaphylaxis and sepsis.
Affected Populations
Hepatorenal syndrome affects men and women in equal numbers. The exact frequency of the disorder is unknown. It is estimated to occur in about 8 to 10 percent of people with fluid buildup in the abdomen (ascites) and cirrhosis of the liver. Although HRS most often occurs in people with advanced cirrhosis and ascites, HRS also occurs in people with other forms of liver disease, including acute liver failure.
Liver cirrhosis as the most common cause
Cirrhosis is a chronic disease, with the progression of which the death of liver cells - hepatocytes - is observed. The disease is accompanied by active proliferation of connective tissue and uncontrolled division of surviving hepatocytes.
In liver cirrhosis, hepatorenal syndrome is a common complication.
Pathology often occurs due to the use of nephrotoxic drugs and an inadequately prescribed drug therapy regimen. If liver cirrhosis is accompanied by ascites, hepatorenal syndrome progresses as a result of a decrease in venous blood return or after the procedure of removing a large volume of fluid without replacement therapy.
Diagnostics
The diagnosis of hepatorenal syndrome is made based on a thorough clinical assessment, a detailed patient history, and various specialized tests.
The main diagnostic criteria are:
- the presence of severe liver failure with portal hypertension;
- high levels of creatine;
- no other causes of kidney failure, such as bacterial infection, shock, or taking medications that are toxic to the kidneys;
- lack of improvement in kidney function when diuretics are stopped and plasma is expanded with albumin (a protein produced in the liver that is low in patients with liver disease);
- low levels of protein in the urine without any evidence of urinary tract disease (uropathy) or parenchymal kidney disease.
Clinical picture
General symptoms:
- The appearance of weakness, increased fatigue. Yellowness of the skin, sclera.
- Changing taste preferences.
- Deformation of the joints on the toes and hands with the formation of the symptom of “drumsticks” against the background of “glazing” (“mirroring”) of each nail.
- Development of palmar erythema.
- The appearance of xanthomas (yellow-brown plaques) mainly in the area of the upper eyelids, “spider veins”.
- Hepatolienal syndrome.
- Oligo- and anuria during water load and a decrease in the level of sodium ions in the blood.
- A peri-umbilical hernia and peripheral edema appear.
- Dilatation of the saphenous veins on the anterior abdominal wall (“head of the jellyfish”).
- In men, the mammary glands become enlarged.
- Azotemia.
- Arterial hypotension.
The above-described symptoms appear even before kidney damage; with the addition of hepatorenal syndrome, signs of disruption of the glomerular apparatus progress quickly.
Against the background of the above picture, two types of hepatorenal syndrome are distinguished: the first is determined by a rapidly progressive deterioration of kidney function (less than 2 weeks), an increase in the level of blood creatinine by 2 or more times, urea nitrogen up to 120 mg/dl, oliguria or anuria, in the second type insufficiency of renal functions develops gradually, urea nitrogen increases to 80 mg/dl, blood sodium decreases, this type has a more favorable prognosis.
Standard Treatments
The only curative therapy for people with hepatorenal syndrome is a liver transplant, which corrects both the liver disease and the associated impaired kidney function. Even after successful liver transplantation, patients who previously had hepatorenal syndrome may not fully recover kidney function. A small percentage may cause permanent damage requiring dialysis. A large number of studies are currently being conducted to determine which patients will recover and which will not. Those who cannot recover may require a kidney transplant with a liver transplant. However, due to the limited number of donors and long waiting lists, liver transplantation is not always feasible.
In patients who develop hepatorenal syndrome with acute liver failure rather than cirrhosis, recovery from the disease can occur if the liver recovers. However, individuals with hepatorenal syndrome requiring dialysis or having progressive kidney failure within 6 to 8 weeks before receiving a liver transplant may require a kidney transplant with a liver graft because kidney function may not recover.
Disease prevention
Recommendations to avoid such a complex disease as hepatorenal syndrome are as follows:
- careful attention to your health. Systematic, at least once a year, even with complete external health, examination and blood and urine tests, blood pressure checks;
- treatment of chronic kidney and liver diseases, as they can provoke this pathology;
- fighting bad habits: alcohol, smoking, overeating. Drug addiction treatment;
- prevention and treatment of poisoning.
These clinical recommendations will help prevent hepatorenal syndrome.
Forecast
Hepatorenal syndrome (HRS) type I has a median survival of 2 weeks, with few patients surviving more than 10 weeks. Type II disease has a median survival of 3-6 months.
Mortality/morbidity
Doctors should be aware that there are 2 different forms of HRS. Although their pathophysiology is similar, their manifestations and signs are different.
HRS type I is characterized by rapid and progressive renal failure and is most often caused by spontaneous bacterial peritonitis (SBP). Type I disease occurs in approximately 25% of patients with SBP, despite rapid resolution of the infection with antibiotics. Without treatment, the median survival of patients with type I HRS is less than 2 weeks, and virtually all patients die within 10 weeks of the onset of kidney failure.
HRS type II is characterized by a moderate and stable decrease in glomerular filtration rate (GFR) and usually occurs in patients with relatively intact liver function. These patients are often resistant to diuretics, with a median survival of 3–6 months. Although this is noticeably longer than in type I HRS, it is still shorter compared to patients with cirrhosis and ascites who do not have renal failure.
Medicines
Treatment of hepatorenal syndrome involves the use of antioxidants, vasoconstrictors, and agonists.
The following drugs are used for drug treatment:
- vasopressin agonists - Terlipressin, Remestip;
- sympathomimetic "Dopamine";
- general vasoconstrictors – Sandostatin, Octreotide (long-term);
- antioxidant – “Acetylcysteine” (in case of overdose of paracetamol drugs);
- neutralizer for reducing the volume of circulating blood - “Albumin”.