Chronic renal failure occurs as a result of a long course of chronic diseases of the urinary system (pyelonephritis, glomerulonephritis, prostate adenoma), diabetes mellitus, hypertension, or as a result of aging of the body (sclerotic changes occur in the vessels of the kidneys).
This disease is characterized by the replacement of nephrons with connective tissue, as a result of which the kidneys can no longer function adequately and their functions progressively deteriorate.
At the onset of the disease, patients experience weakness, polyuria, nocturia, and anemia may be detected. For a long time, the only symptom of chronic renal failure may be a persistent increase in blood pressure.
The disease is diagnosed by a biochemical blood test, which reveals elevated levels of urea and creatinine, and by urine testing, which reveals the presence of protein and a decrease in the relative density of urine.
“Development of kidney failure in women: forms, symptoms and treatment”
2 comments
Human life is impossible without timely cleansing of the body from harmful toxins, metabolic products and excess fluid.
These functions are assigned to the urinary system, where the kidneys bear the greatest burden. They continuously clean and filter the blood from harmful substances, performing the function of treatment facilities in the body. Renal failure is when renal function fails as a result of various pathological influences. The disease is not characterized by gender differences, but according to statistics, symptoms of renal failure in women appear much more often. The very anatomical difference between the female genitourinary system and the male one is a prerequisite for the development of kidney diseases. This is, first of all, the shorter and wider female urethra, through which the infection easily penetrates through the ascending route into the renal structures, forming foci of inflammation in them.
Extensive inflammatory processes affecting parenchyma tissue (the lining of the kidneys), renal calyces and the tissue structure of the pelvis cause disturbances in the processes of urine filtration and excretion. As a result of prolonged stagnant processes of urine, extensive cellular and tissue intoxication of the organ develops. Multiple external and internal causes of the development of the disease determine the manifestation of unique symptoms in each specific case.
Prevention
As a preventative measure, older patients are recommended to undergo an annual examination and check the condition of their internal organs. It is worth taking vitamin complexes that improve immunity and reduce the risk of disease. It is not recommended to overcool the kidneys. Do not perform heavy physical work. It is recommended to drink enough fluids, but not to drink more than the daily limit. It is worth taking the choice of medications seriously, since many of them have a negative effect on the kidneys.
Forms of clinical manifestations
Renal failure can occur in acute or chronic form. At the same time, the signs of the disease depend on the severity (stage) of the pathological process. The time of transition from the acute to the chronic form is determined by the general health of the woman and the body’s ability to resist infectious influence.
Acute renal failure (ARF) develops with sudden intoxication damage to the structural tissues of the kidneys. This may be a consequence:
- various tumor processes in the organ itself and in the adrenal glands;
- tuberculous kidney damage;
- deep skin thermal damage;
- radioactive influence and certain medications;
- massive hemorrhagic processes;
- chronic course of diseases of the urinary organs;
- compression of the kidneys as a result of injury;
- disturbances in the hemostasis system caused by surgery;
- congenital renal pathologies;
- endocrine diseases;
- a difficult birth process, or a difficult pregnancy.
The result of intoxication is manifested by the functional failure of the kidneys in the processes of excretion and filtration, which causes a number of pathological disorders - the accumulation of harmful substances in the blood:
- urea and its nitrogen-containing compounds;
- pathogenic microflora;
- increased blood creatinine levels;
- glucose.
How to carry out diagnostic measures
The first thing a doctor begins with when a patient with kidney disease appears on his doorstep is an examination and physical examination. It is especially important to study the condition of the patient’s skin and mucous membranes: with a long-term disease, they may be pale and have a yellowish tint, which is associated with the deposition of uric acid salts in the tissues.
The lumbar region is painful on palpation, and there is pronounced swelling of the upper half of the body and face. Renal edema does not spread to the legs. The patient's tongue is wet and coated with a white or yellowish coating. Body temperature is moderately elevated.
It is possible to determine whether a patient has acute or chronic renal failure using laboratory and instrumental research methods. Some clinical symptoms of kidney failure are very similar to other diseases.
List of diseases for differential diagnosis of acute or chronic kidney disease:
- gastroenteritis or gastroenterocolitis;
- migraine;
- atherosclerosis of abdominal vessels;
- thrombosis of the vessels of the pelvis and retroperitoneum;
- hormonal deficiency;
- infectious diseases of a parasitic or bacterial nature;
- hepatitis and cirrhosis of the liver;
- hepatic coma;
- diabetic coma;
- coma due to stroke;
- acute or chronic cerebrovascular accident;
- physiological urinary retention.
Thanks to laboratory methods, it becomes possible to establish the stage of the disease, as well as determine the presence of compensation or decompensation.
Laboratory tests necessary to make a diagnosis:
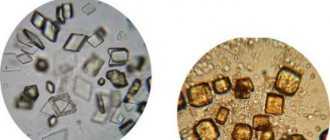
- General analysis of urine, where a change in density will be observed towards its increase, a change in the color of urine from straw yellow to dark red, red blood cells and protein, which are not normally found. During laboratory testing of urine, changes in its characteristics are often observed.
- Bacteriological examination of urine is one of the most important methods. With its help, you can isolate the main causative agent of the disease by inoculating it on different nutrient media. In parallel, it is possible to determine the sensitivity of the pathogen to antibiotics.
- Urine testing according to Zimnitsky involves collecting urine during the day in eight different containers. Then, separately in each container, the number of leukocyte and epithelial cells is counted, which will be increased in case of renal failure.
- A general blood test shows the course of the pathological inflammatory process throughout the body. With insufficient kidney function, the level of leukocytes, monocytes, macrophages, and lymphocytes increases. Anemia may occur in the form of a decrease in hemoglobin and red blood cell levels. A complete blood count is indicative of renal failure.
Thanks to instrumental techniques, it becomes possible to see the condition of both kidneys, their connective tissue capsule, ureters and bladder, as well as assess the functional state of the main renal vessels. The use of such studies is widespread both abroad and in Russia.
To diagnose renal failure, use:
- Ultrasonography. This technique allows you to examine the entire pyelocaliceal system of the kidneys and evaluate its condition over time. When contrast is added to the renal vein, its movement can be tracked using an ultrasound scanner and the level of vascular occlusion, atherosclerotic lesions, developmental anomalies and deformities can be determined. Kidney ultrasound can reliably confirm the diagnosis
- Computed tomography or magnetic resonance imaging shows the pelvic and retroperitoneal organs in several projections at once. This allows us to exclude tumors, cysts and the absence of one kidney. It is recommended to conduct such a study no more than once a year, since computed tomography is performed using an X-ray camera, which has a certain effect on the human body. Kidney examination using CT or MRI shows the organs in the form of a three-dimensional image
- A biopsy involves removing a small piece of kidney tissue for microscopic and biochemical analysis using a long needle. The operation is invasive and painful, but does not pose any practical risks to the person. This procedure will eliminate cancer. Before a kidney biopsy, tissue anesthesia is performed
Signs of kidney failure in a woman
The manifestation of symptoms of acute renal failure is determined by the reasons that caused acute renal failure and the stage of development of the pathological process.
- Causes of a prerenal nature (independent of renal disorders) cause the development of the disease against the background of heart failure, shock, or cardiovascular collapse, severe arrhythmia or a significant decrease in blood flow to the kidneys (for example, with blood loss).
- The renal factor (the reason lies in the structural disorders of the kidney itself) is caused by acute necrosis (death) of the renal tubules that filter the blood. What can happen under the influence of toxic substances, various surrogates, medications and lack of blood supply to the kidneys. Sometimes, this may be a consequence of acute inflammatory kidney diseases.
- The postrenal (obstructive) factor causes the development of acute renal failure against the background of decreased vascular patency (occlusion), for example, acute bilateral blockage of the ureters.
Stages of symptom development
The onset of the disease (stage 1) is manifested by severe migraines, chills, muscle pain and fever, if the cause is due to infectious influence. Signs of functional gastrointestinal disorders in the form of nausea, vomiting and diarrhea appear after an hour. The toxic effect of toxic substances is expressed by yellowing of the skin, signs of anemia and tremors of the extremities.
The development of the disease is manifested by a rapid increase in symptoms:
- Manifestation of confusion, which is replaced by deep fainting;
- Increased sweating is noted (cold sweat covers the forehead);
- Signs of thread-like pulsation;
- A characteristic manifestation of arterial hypertension with an alternating decrease in blood pressure to critical limits.
In case of infectious damage to the organs of the urinary system, pain appears in the lumbar area, problems in the urination process and the presence of bloody inclusions in the urine.
The next stage of development (2nd) is characterized by a decrease in the volume of urine excreted, or a complete cessation of its excretion. Loss of consciousness and development of coma are noted. Edema processes in the subcutaneous tissue significantly increase the patient's weight. Swelling of the brain and lung tissue may occur.
Signs of the terminal stage of acute renal failure appear with inadequate treatment of the disease or its complete absence. Symptoms are expressed:
- The appearance of a large amount of foaming sputum at the mouth;
- Manifestation of subcutaneous and internal hemorrhages;
- Syncope (fainting);
- Frequent cramps in the calf muscles;
- Cardiovascular disorders.
At this stage of the disease, it is no longer possible to help the patient.
Diagnosis of the disease
Diagnosis of CKD involves consulting doctors:
- therapist; urologist; cardiologist; endocrinologist; ophthalmologist; neurologist; nephrologist.
Diagnosis of CKD involves taking an anamnesis, after consultation with a number of specialists, and a fairly objective examination.
The doctor will collect an anamnesis (all symptoms of the disease, concomitant diseases, in children - the presence of physical developmental delay, as well as features of the family history). An objective examination includes percussion and palpation of the kidneys. In children - examination of the ridge, the presence of weight deficiency, stunted growth, the presence of high blood pressure, signs of anemia, etc. Chronic renal failure is determined by tests:
- Urinalysis - small amounts of protein, decreased density, the presence of red blood cells, casts and an increased number of leukocytes. A blood test reveals an increase in leukocytes and ESR, a decreased amount of hemoglobin and red blood cells. Biochemical analysis - increased creatinine, urea, nitrogen, potassium and cholesterol in the blood. Decreased protein and calcium. Determination of glomerular filtration rate - calculated based on a blood test for creatinine, age, race, gender and other factors. An ultrasound of the kidneys and urinary system will help to see the condition of the kidney. MRI visualizes the structure of the kidney, its components, ureter and bladder. Doppler ultrasound evaluates the condition of the kidney vessels. Zimnitsky test - shows the state of kidney function, and you can also see the volume of urine excreted in the morning and afternoon.
Chronic renal failure
In essence, chronic renal failure is a syndrome of irreversible disorders in renal function. The disease progresses slowly, the clinical symptoms are not very pronounced, so a visit to the doctor is usually postponed until better times.
Meanwhile, the number of nephrons actively involved in filtration is decreasing every day. The connection of nephrons that are not involved in the work of the kidneys gives only a temporary effect, as they are destroyed over time. As a result, the final stage of the chronic process is expressed by the shrinking of the kidney and the complete loss of its functional abilities.
At the initial stage of the disease, symptoms may be completely absent. Their painful manifestation is noted in parallel with the destruction of renal nephrons and the processes of their deformation
- Impaired urination causes dehydration. The volume of urine production doubles as expected. The number of trips to the toilet increases at night. Worsening of the pathology reduces the frequency of urination. The color of the urine becomes almost brown and it smells foul.
- Women are weakened and apathetic, their mouth is constantly dry and bitter, they are prone to fatigue and insomnia.
- Disturbances in the digestive functions are manifested by signs of intoxication - debilitating nausea, frequent vomiting, the appearance of sour belching and bloating, diarrhea, or difficulty defecating.
- There is constant twitching and trembling of the hands.
- Disturbances in blood clotting processes provoke the appearance of hemorrhages throughout the body.
- There are bloody impurities in the stool and urine.
Symptoms
Kidney tissue dies differently at different stages of the disease.
Therefore, there are several stages of progression of chronic renal failure.
Each stage has its own symptoms.
- Latent stage (hidden) - no symptoms. The patient is unaware of the pathology. But during power loads the following may occur:
- lethargy;
- dry mouth;
- asthenia;
- drowsiness;
- the amount of urine produced is greater than usual.
- Clinical stage – symptoms of poisoning appear:
- headache;
- vomit;
- ammonia odor from the mouth;
- decrease in urine volume;
- cardiac arrhythmia;
- lifelessness of the skin;
- diarrhea;
- nausea;
- drowsiness;
- cardiac tachycardia;
- fatigue.
- Stage of decompensation - complications are added to the above in the form of frequent colds and inflammatory processes of the urinary system.
- Terminal stage (compensation stage) - the work of all organs is disrupted, as a result of which a person’s death occurs. Symptoms such as:
- straw color of the skin;
- neurological disorders;
- heavy smell of ammonia from the mouth.
Symptoms of kidney failure in men
The progression of the abnormal process is reflected in the form of symptoms. A man may initially experience pain during urination and loss of appetite. Symptoms depend on the form of the disease.
Symptoms of acute renal failure in men depending on the stage:
- First stage
- nausea;
- pale complexion, body.
Symptoms of chronic renal failure in men depending on the stage:
- Hidden stage . There are usually no symptoms. Fatigue may occur during power loads. A urine test shows the presence of protein.
- Compensatory stage. The volume of urine produced increases.
- Intermittent stage . Kidney performance deteriorates significantly. The stage is different:
- decreased appetite;
- lethargy;
- dry skin;
- feeling of thirst;
- yellow skin color.
Symptoms of kidney failure in women
Signs of kidney failure in women are related to the extent of kidney dysfunction:
- Initial degree - there are no symptoms of the development of pathology, but changes are already taking place in the tissues.
- Oliguric stage – symptoms begin to appear and progress. Powerlessness, shortness of breath, slowness, pain in the abdomen, pelvis, nausea, cardiac arrhythmia appear. The volume of urine excreted within 24 hours decreases. Heart rate increases. Duration – 1.5 weeks.
- Polyuric stage – the patient’s well-being improves. Urine becomes larger. But infectious and inflammatory diseases of the urinary system may develop.
- Rehabilitation stage - The kidneys mostly restore their filtration capacity. If during an acute form of renal failure an impressive number of structural units are damaged, then the organ can no longer fully recover.
At the beginning, signs of kidney failure in women may not even be noticed. But with inflammation, symptoms arise that are difficult to miss.
Chronic renal failure appears due to the progression of the acute form.
Treatment and prognosis
Treatment of renal failure begins with the elimination of all disorders in the kidneys and restoration of their functional properties. The use of detoxification techniques helps cleanse the blood of harmful toxins and wastes and restore normal urination processes. For this purpose, course sessions of hemodialysis, plasmapheresis, and hemosorption are carried out.
Prognosis for recovery
It all depends on the patient’s position and the stage of the syndrome. With acute renal failure without complications, 90% of people recover safely.
If complications occur, death occurs in 25-50% of cases. The most common causes of death: blood poisoning (sepsis), damage to the nervous system, problems with blood circulation.
In the case of chronic renal failure, mortality depends on the age of the patient, the condition of his body, and the diseases that caused the filtration problems. Organ transplantation and artificial blood purification have reduced the number of deaths.
According to statistics, 600 out of one million Europeans are affected by this disease. The number of patients increases by 10–12% every year. Older people get sick 5 times more often.
Men have a longer urethra, so kidney failure is less common in them than in women.
Chronic kidney disease in the elderly: features of diagnosis and management
Published in the journal, Clinical Nephrology 3 - 2014 V.V. Fomin, Yu.S. Milovanov, L.Yu. Milovanova, S.V. Moiseev, N.A. Mukhin GBOU VPO “First MSMU IM. THEM. Sechenov" of the Ministry of Health of Russia, Moscow
The epidemiology, causes, risk factors, clinical features and outcomes of chronic kidney disease in the elderly are discussed. approaches to the management of chronic kidney disease in the elderly are presented, incl. rationale for choosing the method of renal replacement therapy and principles of conservative management.
Keywords: Chronic kidney disease, elderly, management
Epidemiology, risk factors, causes, clinical course and outcomes of chronic kidney disease in elderly population are discussed. approaches to renal replacement therapy and conservative management are revived.
Keywords: Chronic kidney disease, elderly, management.
Chronic kidney disease (CKD), incl. those stages that are characterized by a persistent decrease in glomerular filtration rate (GFR) and, therefore, are associated with the greatest deterioration in long-term prognosis, are increasingly found in the general population among the elderly. The results of large-scale epidemiological studies clearly indicate that CKD is particularly common among people in older age groups [1, 2]. That is why the relationship between CKD and the aging population became the main theme of World Kidney Day 2014 [3].
The dramatic increase in the incidence of CKD among representatives of older age groups is associated primarily with the spread of general population risk factors (arterial hypertension, diabetes mellitus, obesity) [4]. The results of a pooled analysis of the large population-based programs NHANES and KEEP, which included a total of 32,555 examined people, as well as a 5% sample of the Medicaid insurance database (1,236,946 cases) [5] showed that the prevalence of a persistent decrease in estimated GFR 2 and/or albuminuria was especially increases significantly in persons aged 80 years and older and as the number of comorbid conditions increases. In turn, the number of comorbid conditions increases as the estimated GFR decreases, and this relationship was especially noticeable in the elderly.
The prognostic danger of CKD for the elderly is largely complemented by the fact that its diagnosis is often not entirely accurate, especially when only one laboratory indicator characterizing the condition of the kidneys is chosen as a guideline. M. Heras et al. (2012) [6], with a 5-year follow-up of elderly people (average age 83 years), demonstrated that with initial creatininemia >1.1 mg/dL, mortality was significantly higher than in individuals with serum creatinine levels 2 ), active cancer diseases, chronic heart failure of functional classes III-IV (NYHA), diabetes mellitus, heart rhythm disturbances, as well as behavioral disorders and when starting hemodialysis for emergency indications [38]. Along with program hemodialysis, it accumulates, incl. and according to the results of controlled clinical studies, there is a positive experience in performing peritoneal dialysis in elderly patients: in particular, this method of renal replacement therapy allows one to avoid at least some of the problems that arise during the formation of vascular access in them and maintaining its functioning [39].
A particular problem for elderly patients remains disturbances in nutritional status, which often occur in this age group and with preserved renal function, but always increase significantly as CKD progresses. The term “protein-energy malnutrition” is also used to designate malnutrition syndrome in elderly patients with CKD; it is often aggravated by program hemodialysis [40]. The key components of protein-energy malnutrition in an elderly patient undergoing program hemodialysis include weight loss, primarily due to an increasing deficiency of muscle mass, activation of the acute phase inflammatory response syndrome, worsening anemia, disturbances of phosphorus-calcium metabolism and cognitive disorders [41]. Correction of protein-energy malnutrition also becomes of paramount importance for elderly patients who, for various reasons, do not begin program hemodialysis. From this point of view, the generally accepted recommendation of experts is to control the calorie content of food (for persons >60 years old, 30 kcal/kg/day), and, if necessary, use energy and microelement supplements [41]. Currently, successful experience has been accumulated in the use of medicinal preparations of keto analogues of amino acids for the prevention and correction of protein-energy deficiency in patients with CKD. At the same time, the administration of a complex of keto analogues of amino acids in combination with a low-protein diet for patients with CKD provides a clinically significant antiproteinuric effect, alleviates the symptoms of chronic renal failure, and allows for better control of metabolic disorders and arterial hypertension. An algorithm for the prevention and correction of protein-energy deficiency in patients with CKD using keto analogues of amino acids is given in the work of Cs. Kovesdy et al. (2013) [47]. The use of anabolic steroids [42], as well as growth hormone [43], to correct protein-energy deficiency in elderly patients with CKD is actively discussed.
Increasing the duration of the pre-dialysis period while maintaining residual renal function is of paramount importance in elderly patients. From this point of view, a low-protein diet brings significant benefits, arguments in favor of its use continue to accumulate based on the results of randomized controlled clinical trials [44].
Classification of types and stages of the disease
Currently, several classifications are widely used among nephrologists. They allow you to most accurately reflect the severity and course of the pathological process occurring in the genitourinary system of the body.
Classification by level of damage:
- Prerenal renal failure. This type of pathology occurs when the cause of the disease does not lie in the kidneys: impaired electrolyte metabolism, low water intake in the body, severe dehydration or burns.
- Renal renal failure occurs due to pathological processes that develop in the kidney tissue. Pyelonephritis, glomerulonephritis, cysts and kidney tumors provoke the development of renal failure.
- Postrenal renal failure is associated with disturbances in the outflow of urine, which are most often caused by mechanical reasons: stone, foreign body, purulent embolus, tangle of parasites.
Classification by time of occurrence:
- Primary failure. It occurs as an independent disease and requires an individual approach to treatment.
- Secondary failure is the result or outcome of any other chronic disease of non-renal etiology.
Classification of kidney failure by stages:
- The first stage is characterized by a decrease in glomerular filtration rate to ninety milliliters per minute and signs of kidney pathology.
- The second stage is characterized by a decrease in the glomerular filtration rate to sixty to eighty milliliters. Additionally, the severity of organ damage increases.
- The third stage is diagnosed when the filtration parameters decrease to thirty milliliters per minute. Pronounced changes in renal tissue and organs are observed.
- At the fourth stage of the disease, the kidneys practically stop filtering urine: the speed of its passage through the collecting system does not exceed fifteen milliliters per minute. The patient is in extremely serious condition.
- The terminal stage is characterized by an increase in the syndrome of general intoxication, coma and death of the patient. The glomerular filtration rate can reach zero.
Classification of the disease by stage of compensation:
- Compensated kidney failure: the body is still able to independently fight the disease and regulate the exchange of water and electrolytes in the body through tension and adaptation of other organ systems. There are no manifestations, the disease is detected only by random examination.
- Subcompensated failure occurs after several months of disease progression. This is manifested by edema syndrome and a pronounced increase in blood pressure. Other organs and systems are affected.
- The decompensated stage is the final episode of any kidney disease. The body's adaptive reserves are completely depleted, the kidneys cannot cope with removing fluid from the body, the patient develops coma and acute uremic intoxication with urine breakdown products.
Development of kidney failure in women: forms, symptoms and treatment
Therapy is based on two main points: diet and taking specialized medications. It is worth remembering that treatment is selected individually by the doctor, taking into account the woman’s age and the severity of the disease. The use of traditional methods is prohibited; if you treat kidney failure with herbs alone, you can only achieve the development of complications that were described just above.
The diet involves a balanced diet, eating foods low in protein and table salt. The amount of fluid that enters the patient’s body per day is taken under control. The goal pursued by the doctor in this case is to lower blood pressure and reduce the load on the renal glomeruli.
As for medications, infusion therapy often comes to the fore - intravenous administration of solutions of microelements and glucose to restore water and electrolyte balance. Additionally, in rare cases, the doctor recommends oral tablets with a complex of vitamins and minerals.
To relieve arterial hypertension, two main groups of drugs are prescribed: sartans (angiotensin receptor blockers) and angiotensin-converting enzyme inhibitors (ACE inhibitors). Treatment of arrhythmias is selected by a cardiologist depending on the type of disorder.
The rehabilitation period after acute renal failure usually takes six months or a year. During this time, the woman must be registered at the dispensary. The chronic form of the disease implies constant monitoring of the patient’s well-being, but complete recovery cannot be achieved through outpatient or inpatient treatment.
Renal failure is a serious disease of the urinary system, which is characterized by a decrease in the efficiency of the renal apparatus. Symptoms of kidney failure in women differ depending on the type of pathological abnormality or the stage of the disease.
If the diagnosis was not carried out in time and there was no adequate treatment, as a result of a violation of the water-salt balance, severe intoxication of the body with decay elements occurs. This phenomenon can be fatal.
In case of attacks of acute renal failure, it is necessary to carry out emergency hospitalization of the patient.
The treatment of acute renal failure is influenced by factors such as the stage of the disease and the cause of the disease. First, the etiological aspect is eliminated, then homeostasis and kidney function are restored.
Depending on the causes of acute renal failure, the following treatment methods are used:
- taking antibacterial drugs in tablets or injection form in the presence of infection (Cefepime, Cefaclor);
- increased fluid intake (with reduced circulating blood volume);
- the use of diuretics to reduce swelling (Lyzax, Diacarb, Furosemide);
- the use of heart medications that lower blood pressure during shock (Atenolol, Losartan);
- detoxification of the body, gastric lavage in case of poisoning.
The main task in the case of chronic renal failure is to detect the disease as early as possible and slow down the process of atrophy of renal tissue while preventing changes in the functionality of the organ.
The following procedures are used for the treatment of CPH:
- peritoneal dialysis. The procedure is based on the natural ability of the patient’s own peritoneum to filter, which allows one to cleanse the blood of harmful toxins and metabolic elements. During the event, the abdominal organs act as a kind of filter, which is selective in the passage of useful and dangerous substances into the body;
- hemodialysis. The procedure for purifying blood using a semi-permeable porous membrane, which serves as an “artificial kidney”. This device takes on the function of a non-functioning organ and filters the blood from toxins, urea, eliminates excess water, normalizes the electrolyte balance, restores blood pressure and acid-base balance.
- transplantation. Replacement of the affected organ with a donor kidney. The latter is a relative or deceased person. Before surgery, a series of tests are performed to determine compatibility. A donor kidney can take up to a year to take root. A significant disadvantage of this method is the need for the patient to take medications – immunosuppressants – throughout his life. This group of drugs has a detrimental effect on the immune system, which subsequently increases the risk of various infectious diseases.
This disease is very dangerous and should not be left without due attention. The difficulty is that renal failure in the early stages can be hidden and symptoms in women may not appear. During the development of the disease, external well-being and well-being gradually changes due to the loss of the kidney’s basic functions and severe intoxication of the body.
Treatment
Home{amp}gt; Kidney diseases {amp}gt;
Renal failure is a serious disease of the urinary system, which is characterized by a decrease in the efficiency of the renal apparatus. Symptoms of kidney failure in women differ depending on the type of pathological abnormality or the stage of the disease.
If the diagnosis was not carried out in time and there was no adequate treatment, as a result of a violation of the water-salt balance, severe intoxication of the body with decay elements occurs. This phenomenon can be fatal.
The following types of renal failure in women are distinguished:
- spicy. With this type of disease, there is an unexpected deterioration in kidney function, which leads to a deterioration in blood composition due to an imbalance in the body's water balance. If timely measures are taken and the correct treatment is prescribed, symptoms disappear with complete restoration of kidney function;
- chronic. With this form, there is a gradual development of the disease, characterized by a regular decrease in the function of the main units of the kidneys - nephrons. Using competent therapy, it is possible to improve the patient’s general condition, but it is impossible to restore damaged organ tissue and return the full functionality of the system.
Attention! At the primary stage of the disease, changes are almost invisible. The more nephrons die as a result of the disease, the more the basic function of the kidneys to remove waste products decreases, and the more intense the intoxication increases.
Peculiarities
In women, symptoms of the disease appear much more often. This is due to the fact that the female body has a greater predisposition to kidney diseases due to the anatomical structure of the genitourinary system.
The female urethra, unlike the male one, has a wider and shorter shape. This allows pathogenic microorganisms to freely enter the bladder with the formation of foci of inflammation. The infection then travels through the urinary tract to the kidneys.
Significant damage to the parenchyma, calyces, and pelvis leads to disruption of the filtration and excretion process. Urinary retention causes intoxication of the cells and tissues of the body. As can be seen, both endogenous and exogenous factors influence the formation of the disease.
Symptoms and treatment of the disease depend on a number of factors. These include: forms of the disease, causes of occurrence and stages of progression. Signs of kidney failure in women directly depend on what caused the exacerbation.
Root cause Symptoms
| Presence of infection | migraine, muscle pain, fever with chills. |
| Intestinal poisoning | vomiting, loose stools, headache. |
| Poisoning with toxic substances | muscle cramps, symptoms of jaundice. |
| Shock | decreased blood pressure, rare pulse, perspiration, fainting. |
| Glomerulonephritis | presence of blood in the urine, pain in the lumbar region. |
Depending on the stage of the disease, the symptoms of the disease also change significantly.
Stage Symptoms
| Initial. | It proceeds without significant manifestations. The main discomfort is caused by the symptoms of the disease that caused the pathology. The first changes in kidney tissue begin. |
| Oliguric. | Reduced amount of urea due to decreased kidney function. Intoxication with harmful decomposition products, disturbance of the water-ionic state with the following symptoms: decrease in the amount of urine to 400 ml per day, weakness, lethargy, loss of appetite, vomiting, muscle cramps, disruption of the cardiovascular system with rapid heartbeat, arrhythmia, abdominal pain cavities, disruption of the gastrointestinal tract with the occurrence of ulcers and bleeding, the occurrence of infectious diseases against the background of a decrease in the immune system. This form is considered the most difficult and can last from 6 to 12 days |
| Polyuric. | The patient's general well-being stabilizes, and the amount of urine increases to an exaggerated level. This can lead to dehydration of the body with the addition of infectious diseases. |
| Final restoration. | Complete restoration of kidney function. The duration of the period can last from 5 to 12 months. |
Attention! If a significant portion of the kidney tissue has been damaged as a result of the disease, complete restoration of organ function does not occur.
The symptoms of chronic renal failure (CRF) are very similar to those of the acute form. The difference lies in the prolonged form of manifestation.
Stage Symptoms
| Initial. | Chronic deficiency does not manifest itself in the form of symptoms. The person's health is normal. The first signs begin to appear when 80% of the kidney tissue loses its ability to function. Despite this, the disease is well diagnosed even in the earliest stages |
| Second. | The first symptoms begin to appear in the form of: lethargy, weakness, increased fatigue, frequent ailments, urinary dysfunction with the formation of large amounts of urine (up to 4 liters), frequent urination at night, the development of dehydration, nausea and vomiting, muscle spasms, itching of the skin, a feeling of dryness in the mouth, pain in the abdominal region, diarrhea, bleeding in various locations due to decreased blood clotting, skin hemorrhages, and the addition of infectious respiratory diseases due to a weakening of the general immune system. |
| Third. | The patient's condition worsens significantly. The following are observed: a decrease in the amount of urine, which entails severe intoxication, swelling of the subcutaneous tissues, an increase in blood pressure, blurred vision, the appearance of an ammonia odor from the mouth, decreased appetite, decreased body weight, yellow skin discoloration, disruption or cessation of the menstrual cycle , fragility of blood vessels, attacks of shortness of breath, frequent loss of consciousness, falling into a coma. |
Attention! If diagnosis is delayed, when the disease has entered its final phase, only forced hemodialysis can save the patient.
Symptoms of renal failure in women are not particularly different from signs of functional decline of the organ in men and children of any age. There is an acute form and exacerbations against the background of chronic renal failure, while chronic renal failure occurs in 90% of clinical cases among patients with nephrotic syndrome of any nature.
Chronic renal failure is a progressive, irreversible disorder of the excretory and filtration functions of the organ. The terminal stages of chronic renal failure lead to the complete cessation of renal function due to the death of an impressive volume of kidney tissue.
Symptoms of renal failure in women appear depending on the stage of the pathological process
The acute form of PN occurs rarely, mainly against the background of acute toxic reactions, shock, acute heart or liver failure, as well as in the absence of replacement therapy for chronic renal failure.
Symptoms of kidney failure in women include constant fatigue and malaise at an early stage. As the pathological process develops, appetite is disrupted, nausea, vomiting, and swelling of the limbs and face appear. The terminal stage is characterized by the addition of life-threatening complications due to arterial hypertension.
Renal failure refers to a multifactorial condition where multiple intrinsic or extrinsic factors can affect kidney function. Common causes of organ failure are:
- inflammatory processes in the renal structures (glomerulonephritis, pyelonephritis);
- internal bleeding;
- polycystic kidney disease, multicystic;
- dehydration;
- infectious-septic and purulent diseases;
- coma, shock;
- side effects from long-term drug therapy;
- tumors, malignant neoplasms;
- injuries;
- alcoholism.
Traumatic and hereditary factors play an important role in the development of renal failure. The mechanism of development of chronic renal failure is due to a violation of adequate blood circulation in the renal tissues, which blocks access to oxygen and normal nutrition of the organ cells.
The kidneys are quickly depleted, all functions of the organ are disrupted. Against the background of chronic renal failure, toxic compounds accumulate in the body and intoxication occurs.
Symptomatic manifestations of renal failure are conventionally divided into three large groups: general, organ and specific.
Treatment of kidney failure includes medications and replacement therapy
If a woman is responsible for her health, she will definitely notice some deviations at an early stage of the development of the disease.
Clinicians highlight the following list of possible common symptoms in women:
- increased frequency of headaches;
- malaise;
- dizziness, tinnitus;
- pale skin;
- decreased immunity, frequent colds.
General signs may resemble the course of many diseases at an early stage of development, therefore, without knowing the possible cause of such a condition, it is recommended to undergo a routine medical examination.
Specific signs are directly related to the kidneys and genitourinary system and are characterized by the following manifestations:
- disturbance of urination, weakening of the flow pressure;
- decrease or increase in urine volume (in the second case, the density of urine sharply decreases);
- inadequate diuresis - the process of urination;
- changes in the structure and color of urine, the appearance of pus and flakes;
- hematuria - the appearance of blood in the urine;
- lower back pain or positive tapping reaction, renal colic (it is important to distinguish from spinal osteochondrosis).
Important symptoms of renal failure are laboratory parameters of blood and urine. If impaired renal function is provoked by an inflammatory process in the organs of the nephrourological system, then characteristic infection symptoms appear.
Organ manifestations occur when complications occur, but they should be differentiated from other independent diseases:
- noticeable heart rhythm disturbances;
- tremor of the hands;
- arterial hypertension;
- dry suffocating cough;
- yellowness of the skin, ascites;
- disturbance of the psycho-emotional background.
A common concomitant manifestation of chronic renal failure is heart failure. The heart and liver are the main target organs that are involved in the pathological process and at the same time are accompanied by characteristic symptoms.
Causes
Acute renal failure
Acute kidney injury develops abruptly and is characterized by a rapid decline in renal function. The reasons are divided into three groups:
- Prerenal.
- Renal (renal).
- Postrenal.
With prerenal causes, the kidneys are healthy, but the blood supply to the organ is disrupted, which precludes normal functioning, since the renal parenchyma is in a state of lack of nutrients and oxygen.
Blood supply disruption occurs when there is a sharp decrease in blood flow volume. This can result from dehydration in infectious diseases or significant blood loss from various injuries. Kidney function will decrease in heart failure, when the heart is not able to pump blood to the required extent, which will cause hypoxia of the kidney tissue. In addition to general conditions of the body, acute kidney injury will be caused by local changes in the blood vessels supplying the kidneys: stenosis (narrowing) of the renal arteries, thrombosis of the renal vein.
The renal causes of acute kidney injury are located in the kidney itself. The structure of the kidney contains functional units - nephrons. The nephron consists of a glomerulus (glomerulus), tubules and is surrounded by interstitial tissue. Inflammatory diseases of these structures can cause acute kidney injury: glomerulonephritis, acute tubular necrosis, interstitial nephritis. Tumor decay products and nephrotoxic substances can also damage kidney tissue. Nephrotoxic poisons include mercury compounds, acetic acid, alcohol substitutes and some medications: antibiotics (aminoglycosides), radiocontrast agents, antitumor drugs. In addition to external toxins, myoglobin, which is part of muscle tissue, can damage the kidney. With muscle injuries, dystrophies, diabetic ketoacidosis, hypothyroidism, muscle tissue breaks down and myoglobin enters the general bloodstream.
Postrenal causes are usually associated with urinary tract obstruction. The resulting urine accumulates in the kidney and compresses the renal parenchyma, disrupting blood microcirculation and causing tissue death. Symptoms of this condition usually include urolithiasis, bladder and ureter cancer, and retroperitoneal fibrosis.
Chronic renal failure
Typically, the cause of chronic renal failure is diabetes mellitus combined with hypertension.
These pathologies slowly lead to the formation of a secondary wrinkled kidney, as the organ undergoes sclerosis. The formation of a primary wrinkled kidney occurs in chronic pyelonephritis and glomerulonephritis. Also, congenital anomalies of the urinary organs will cause chronic renal failure: systemic lupus erythematosus, polycystic kidney disease, Alport syndrome, congenital Fanconi syndrome, amyloidosis.
Chronic and acute renal failure: symptoms and treatment
Classification
Acute kidney injury and chronic kidney disease can lead to kidney failure.
In the first case, the disease develops with a sharp decrease in kidney function (over a period of about 7 days). The causes of acute kidney injury are numerous.
This usually occurs when there is impaired blood flow in the renal tissue, inflammatory processes, difficulty in the urinary tract, or exposure to toxic substances on the renal parenchyma. The consequence of acute injury, regardless of the causes of development, is an increase in creatinine and urea levels and a decrease in urine formation. The diagnostic criterion is not only laboratory data, but also a decrease in the number and volume of urination.
Chronic kidney disease
A type of kidney failure in which loss of kidney function occurs over a period of months or years. The condition is caused by long-term chronic diseases, so restoration of renal function is impossible and the damage is irreversible. At the beginning of the disease, there are no symptoms, but later swelling, weakness, secondary arterial hypertension, and anemia appear.
Complications
Disturbances in mineral and ionic balances can cause bone fractures, convulsive syndrome, cardiac failure, and the development of secondary arterial hypertension.
Patients with late-stage renal failure have an increased risk of developing kidney cancer.
The prognosis of renal failure syndrome depends on the etiology of its occurrence and the stage of the pathology. With properly selected therapy, acute kidney injury is reversible, and with chronic kidney disease, it is possible to prolong the life of patients for many years.
Epidemiology
Renal failure syndrome develops in approximately 30-60 people out of 1,000,000 with acute injury, and the prevalence of chronic kidney disease ranges from 200 to 600 cases out of 1,000,000. These statistics are given in the Russian clinical guidelines edited by Yu.G.
Alyaeva. Among all causes of death, chronic kidney disease ranks eleventh. Recent advances in pharmacotherapy and the possibility of replacement treatment allow people with chronic kidney disease to significantly increase their life expectancy, so currently there has been an increase in patients of various ages with this pathology.