Nephrotic syndrome is a disease characterized by severe proteinuria, edema, hyperlipidemia, hypoalbuminemia, increased blood clotting, and lipiduria. Due to various immune disorders, metabolic disorders, toxic effects, and degenerative processes in the body, changes occur in the walls of the glomerular capillaries, causing excessive filtration of plasma proteins. Thus, acute nephrotic syndrome is a consequence of pathological conditions leading to increased permeability of the glomerular capillary wall.
What is nephrotic syndrome?
Nephrotic syndrome is not a disease in itself; rather it is a group of symptoms that:
- indicate kidney damage—especially damage to the glomeruli, the tiny units in the kidney where blood is filtered;
- cause too much protein to be excreted from the body into the urine.
When the kidneys are damaged, the protein albumin , normally found in the blood, will leak into the urine. Proteins are large, complex molecules that perform a number of important functions in the body.
There are 2 types of nephrotic syndrome:
- primary - the most common type of nephrotic syndrome, which begins in the kidneys and affects only the kidneys;
- secondary - the syndrome is caused by other diseases that affect other organs.
Nephrotic syndrome may develop gradually or may occur suddenly. The condition can occur at any age. In children, it is most common between the ages of 18 months and 4 years, more often in boys than girls. In adults and older people, both sexes are affected equally.
Pathogenesis
Hypoproteinemia (decreased blood protein levels) is the main cause of edema. It, in turn, develops due to the loss of proteins (primarily albumin) in the urine. This occurs due to increased permeability of the glomerular filter . Hypoproteinemia causes a decrease in plasma pressure, and the liquid part of it passes into the tissues and lingers in them, causing the development of edema. The condition of the lymphatic capillaries plays a role in the occurrence of edema. Increased filling of tissue with fluid causes a compensatory increase in lymphatic drainage, while tissue proteins are also removed with lymph. This reduces the pressure of the interstitial fluid. As plasma volume decreases, the renin-angiotensin-aldosterone system and antidiuretic hormone . As a result, sodium retention occurs in the renal tubules, which leads to the maintenance and further spread of edema.
The mechanism of toxic kidney damage is associated with the direct toxic effect of poisons on kidney tissue. Mostly the proximal parts of the nephron are affected, in which reabsorption of toxic substances occurs. Dystrophic and degenerative changes (even necrosis) develop in the tubular epithelium. In parallel, there is a disorder of renal hemodynamics in the kidneys - blood flow in the organ is significantly reduced, which causes a decrease in filtration and spasm of the arteries of the renal cortex.
Poor circulation leads to ischemia of the organ, and its consequence is damage to the tubules (up to necrosis) and destruction of the glomerular membrane. As a result of organ ischemia and tubular necrosis, swelling of the kidney tissue itself develops. Renal vascular spasm and toxic coagulopathy due to poisoning lead to the development of diffuse intravascular coagulation.
What are kidneys and what do they do?
The kidneys contain two bean-shaped organs, each the size of a fist. They are located just below the rib cage, one on each side of the spine. Each day, the kidneys filter 120 to 150 liters of blood to produce 1 to 2 liters of urine, which consists of waste and excess fluid.
Children produce less urine than adults, and the amount produced depends on their age. Urine flows from the kidneys to the bladder through tubes called ureters. The bladder stores urine. When the bladder empties, urine flows out of the body through a tube called the urethra, located at the bottom of the bladder.
Urine flows from the kidneys to the bladder through tubes called ureters.
The kidneys work on a microscopic level. The kidney is not one big filter. Each kidney is made up of about a million filtering units called nephrons. Each nephron filters a small amount of blood.
The nephron includes a filter called the glomerulus and a tubule. Nephrons work in two stages. The glomerulus allows fluid and waste to pass through it; however, it prevents the passage of blood cells and large molecules, mainly proteins. The filtered liquid then passes through a tube, which sends essential minerals back into the bloodstream and removes waste.
Each kidney is made up of about a million filtering units called nephrons. Each nephron filters a small amount of blood. The nephron includes a filter called the glomerulus and a tubule.
Diet
Patients are advised to limit salt for edema and high blood pressure. Animal products (meat and fish) also contain sodium chloride , so in the acute period they are excluded from the diet, but it must be borne in mind that long-term protein restriction is also bad. The optimal protein intake is 1 g per kg of weight. During the period of exacerbation Diet No. 7 , and in the remission stage, nutrition can correspond to Table No. 5 .
What causes nephrotic syndrome?
Although idiopathic or unknown diseases are the most common cause of primary nephrotic syndrome in patients, researchers have linked certain diseases and some specific genetic changes that damage the kidneys with primary nephrotic syndrome.
Secondary nephrotic syndrome is caused by an underlying disease or infection. It is the underlying disease or infection that causes changes in kidney function, which can lead to a secondary form of the condition.
Symptoms
Despite the varied etiology of the syndrome, its clinical manifestations are the same and typical.
- Proteinuria is the leading, but not the only, symptom of pathology. Most of the lost protein is albumin. Their amount in the blood decreases, fluid retention occurs in the body, which is clinically manifested by edema of varying localization and prevalence, accumulation of free transudate in the cavities. Daily diuresis is less than 1 liter.
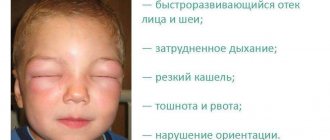
- Patients have a typical appearance: they have a pale, pasty face and swollen eyelids, a coated tongue, and a distended abdomen. The first swelling appears around the eyes, on the forehead, and cheeks. The so-called “nephrotic face” is formed. Then they descend to the lower back, limbs and spread to the entire subcutaneous tissue, stretching the skin. Edema limits the mobility of patients, reduces their activity, complicates the process of urination, and causes constant watery eyes.
- Signs of asthenia include: weakness, lethargy, physical inactivity, dry mouth, thirst, discomfort and heaviness in the lower back, decreased performance.
- Acute nephrotic syndrome is manifested by increased body temperature and signs of intoxication.
- Degenerative-dystrophic changes in the skin - dryness, peeling, the appearance of cracks through which fluid can be released.
- Dyspeptic symptoms do not always occur. These include epigastric pain, lack of appetite, vomiting, flatulence, and diarrhea.
- Pain syndrome – headaches, myalgia and arthralgia, lower back pain.
- Severe chronic nephrotic syndrome is clinically manifested by paresthesias and convulsions.
- Hydrothorax and hydropericardium are manifested by shortness of breath and chest pain.
Forms of the syndrome:
- Persistent is a common form of the disease, characterized by a sluggish and slow course. Even persistent therapy does not provide stable remission. The outcome of the pathology is the development of renal failure.
Recurrent – a frequent change of spontaneous exacerbations and remissions, which are achieved with the help of drug therapy.- Episodic – develops at the beginning of the main disease and ends in stable remission.
- Progressive - rapid development of pathology, leading to the development of renal failure in 1-3 years.
There are also 2 types of syndrome depending on sensitivity to hormone therapy - hormone-resistant and hormone-sensitive.
Who is most likely to suffer from nephrotic syndrome?
In cases of primary nephrotic syndrome, which is caused by idiopathy (an independent disease), researchers cannot accurately determine which patients are more likely to develop the syndrome. However, as researchers continue to study the link between genetics and nephrotic syndrome, it may be possible in the future to predict the occurrence of the syndrome in some children.
The secondary type of syndrome often develops if:
- there are diseases that can damage a person’s kidneys;
- take certain medications (such as NSAIDs);
- develop certain types of infections.
Prevention
Prevention of nephritic syndrome consists of preventing the underlying diseases that caused it. For viral and bacterial infections, cardiac disorders and other diseases that may affect kidney function, you must contact a medical facility for appropriate treatment. All doctors’ recommendations should be followed with precision, making sure to fully treat the disease. The kidneys are the body's filter, helping it get rid of toxins. But this filter also gets clogged and cannot be cleaned, so you should be careful about your health.
Signs and symptoms of nephrotic syndrome
Signs and symptoms of nephrotic syndrome may include
- swelling, most often in the legs, feet, or ankles and less commonly in the arms or face
- albuminuria - when there is a high level of albumin in the urine
- hypoalbuminemia - when there is low level of albumin in the blood
- hyperlipidemia - when the level of cholesterol and fat in the blood is higher than normal
In addition, some people with the condition may experience:
- blood in the urine (hematuria);
- symptoms of infection such as fever, lethargy, irritability, or abdominal pain;
- loss of appetite;
- diarrhea (diarrhea);
- high blood pressure (arterial hypertension).
Features of nephritic syndrome
The symptoms inherent in nephritic syndrome indicate the presence of nephritis (kidney inflammation). In turn, nephritis can cause the following pathological processes:
- damage by viral microorganisms (hepatitis, Corsaki, mononucleosis, ECHO, herpes, etc.);
- infection with bacteria (typhoid fever, endocarditis, pneumonia, meningitis, etc.);
- glomerulonephritis (a disease caused by streptococci);
- systemic (autoimmune) diseases (vasculitis, lupus erythematosus);
- Berger's disease (primary lesion);
- hypersensitivity to certain medications, vaccines, physiotherapeutic effects.
The manifestation of symptoms is usually observed on the 8th – 16th day after the onset of the influence of a negative causative factor on the body. Moreover, the severity of symptoms gradually increases.
Complications
Complications of nephrotic syndrome in a child or adult may include:
- Infections. When the kidneys are damaged, you are more likely to develop infections because the body loses proteins that normally protect against infection. Healthcare professionals will prescribe medications to treat infections. Children with nephrotic syndrome should receive the pneumococcal vaccine and annual flu shots to prevent these infections.
- Blood clots (thrombi). The formation of blood clots can block the flow of blood and oxygen through blood vessels anywhere in the body. Blood clots are more likely to occur when proteins are lost through the urine. Blood clots will be treated with blood thinners.
- High blood cholesterol levels. As albumin passes into the urine, the level of albumin in the blood drops. The liver produces more albumin to compensate for low levels in the blood. At the same time, the liver produces more cholesterol. Sometimes patients may need to be treated with medications to lower blood cholesterol levels.
- Malnutrition. Loss of protein in the blood can lead to weight loss, which may be masked by swelling.
- Chronic kidney disease. Over time, the kidneys may lose their function, requiring dialysis or a kidney transplant.
- Acute renal failure. Kidney damage can cause the kidneys to stop filtering waste, requiring emergency dialysis.
Classification
Nephrotic syndrome occurs:
- Congenital - develops before 3 months of age, renal failure (up to 2-6 years of age).
- Primary - develops with various forms of glomerulonephritis .
- Secondary - against the background of infectious diseases ( syphilis , tuberculosis , malaria , hepatitis , HIV ), intrauterine infections ( toxoplasmosis , cytomegalovirus infection ), systemic diseases, metabolic diseases ( amyloidosis , diabetes ), with hereditary chromosomal diseases.
- Infantile, develops from 3 to 12 months of life and is associated with gene mutations.
First of all, nephrotic syndrome is a manifestation of glomerulonephritis and occurs in nephrotic and mixed forms of glomerulonephritis. Acute glomerulonephritis with nephrotic syndrome occurs some time after a streptococcal infection . Pastiness is the first symptom that is detected in 95% of children. Swelling is localized on the legs, face, eye area, and scrotum. The child develops fatigue, rapid breathing, decreased appetite (up to anorexia ) and abdominal pain. A severe condition with AGN requires hospitalization, strict adherence to diet, bed rest and antibacterial therapy. Auxiliary treatment includes diuretics, antihistamines, vitamin therapy, aminophylline , antiplatelet agents and membrane-stabilizing drugs.
Primary glomerulonephritis is associated with disorders of the morphology (structure) of the kidneys. The morphological forms of primary glomerulonephritis are: minimal change disease, mesangioproliferative glomerulonephritis , membranous nephropathy and focal segmental glomerulosclerosis . With minimal changes, the glomerular membrane is permeable to low molecular weight proteins ( albumin , transferrin ), so selective proteinuria .
With more pronounced changes in the glomerular filter, large proteins (globulins) are filtered out. In childhood, minimal changes in the kidneys predominate, so a biopsy in children with new-onset nephrotic syndrome and selective proteinuria . arterial hypertension and hematuria occurs , as well as the ineffectiveness of corticosteroid therapy, then other variants of glomerulonephritis are possible, and they require morphological examination of the biopsy material. Typically, 90% of patients with minimal change disease respond well to corticosteroids, but with focal segmental glomerulosclerosis, only 20% of children respond to them.
A manifestation of idiopathic membranous nephropathy is also nephrotic syndrome, which appears at the onset of the disease. The course of the disease can be with remissions and relapses. Complete remission is a good sign regarding survival. Partial remission also reduces the risk of developing chronic renal failure . Spontaneous complete remissions of PS occur in 20% of patients, and spontaneous partial remissions occur in 15%. Remissions can occur 14-18 months from the onset of the disease. In half of the patients, nephrotic syndrome has a persistent form (long-term). With persistent nephrotic syndrome, terminal chronic renal failure may develop within 10 years. Such patients are susceptible to infections and thromboembolic complications.
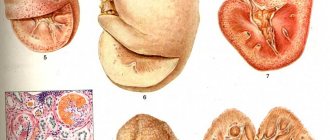
Among the primary kidney pathologies in children can be called lipoid nephrosis . In pediatrics, this term refers to a separate form of glomerulonephritis , which occurs with minimal changes in the glomeruli. This pathology is characterized by protein-lipoid dystrophy of the tubular epithelium. It is more common in children aged 1 to 6 years and is a rare disease. Its etiology is not known, but most researchers consider it to be a hereditary fermentopathy of podocytes (the outer cells of the glomerular capillary). Podocytes are primarily affected and destruction of their legs occurs; podocytes are exfoliated from the basement membrane. Considering that podocytes perform several functions in the renal filter (including limiting the passage of proteins with a negative charge), this leads to a violation of filtration. Thus, kidney damage in this disease is dystrophic in nature.
Previously, lipoid nephrosis was considered as an independent disease, but later it turned out that its cause could be tuberculosis , osteomyelitis , malaria , diphtheria , syphilis , dysentery , chronic enterocolitis , lymphogranulomatosis and intoxication (lead and mercury). In these diseases, the causes of nephrosis are severe metabolic disorders - fat and protein. Cellular nutrition and the permeability of glomerular capillaries are disrupted. Protein particles and lipoids, which are contained in primary urine, penetrate the membrane of the tubules, causing dystrophic changes in the cells.
The disease develops gradually and patients do not feel any discomfort from the kidneys. They may be bothered by significant swelling. The patient's kidneys are enlarged, reaching a weight of 250 g. Microscopically, thickening of the basement membrane is determined due to the loss of processes by podocytes. The kidney stroma is saturated with cholesterol and lipids . When treated, lipoid nephrosis has a favorable prognosis; if left untreated, nephrosclerosis , ultimately leading to chronic renal failure.
Significant kidney damage is observed in hereditary forms of amyloidosis and secondary amyloidosis. In primary amyloidosis, there is loss of amyloid (abnormal protein) in the kidney tissue, but nephrotic syndrome and chronic renal failure do not have time to develop. Increasing proteinuria against the background of cardiomegaly suggests the presence of primary amyloidosis . In many cases, Bence Jones protein .
Nephrotic syndrome with amyloidosis , unlike that with glomerulonephritis , occurs after prolonged proteinuria. Unlike glomerulonephritis, edema syndrome in this disease most often develops against the background of normal or low blood pressure.
Secondary amyloidosis occurs against the background of long-term inflammatory diseases - osteomyelitis , rheumatoid arthritis , tuberculosis , ulcerative colitis , lymphogranulomatosis , tumors . In the clinical course of renal amyloidosis, several stages are distinguished: asymptomatic stage, proteinuric, nephrotic, uremic. Azotemia develops against the background of nephrotic syndrome and low blood pressure, and in most cases, patients die from chronic renal failure.
Necrotic nephrosis has a very severe course - kidney damage that occurs with tubular necrosis, unexpressed changes in the glomeruli and acute renal failure. The identification of this disease as a separate form is associated with the characteristic features of the clinical picture and pathological changes in the kidneys.
Necrotizing nephrosis is an acute shockogenic kidney injury of infectious or toxic origin, which is accompanied by impaired blood supply to the organ, ischemia and necrosis of the tubules. The causes of shock kidney are burns, injuries, septic conditions, intestinal obstruction , severe infectious diseases ( dysentery , malaria , cholera , leptospirosis , diphtheria ).
A special group is necronephrosis, which is caused by intravascular hemolysis (destruction of red blood cells) that occurs during transfusion of incompatible blood. Regardless of the cause, in all cases severe kidney damage leads to anuria , and then to uremia and acute renal failure .
High concentrations of mercury cause acute necronephrosis and, much less frequently, nephrotic syndrome. Mercury compounds cause damage to the vessels of the kidneys, and in severe acute intoxications, focal extracapillary glomerulonephritis with damage to the tubules. In mild and moderately severe chronic mercury poisoning, the tubular apparatus changes mostly, which is manifested by the presence of red blood cells, protein and casts in the urine. There is a tendency for tubular reabsorption to decrease. , chronic glomerulonephritis develops .
oliguria quickly develops (the amount of urine decreases to 300-400 ml per day) and anuria , which lasts up to 6-7 days. A small amount of protein, red blood cells and single white blood cells appear in the urine. As the process increases, kidney failure , manifested by an increase in nitrogenous waste in the blood and the development of acidosis. The patient experiences vomiting, weakness, apathy, stupor and uremic coma . Pericarditis , pleurisy begins and pathological Kussmaul breathing .
Among drugs, aminoglycosides have a pronounced nephrotoxic effect. neomycin ranks first , then gentamicin , followed by monomycin and kanamycin . Neomycin nephrosis occurs with proteinuria , enzymeuria , increased levels of creatinine and urea . oliguria develops . Non-steroidal anti-inflammatory drugs, platinum preparations and radiocontrast agents also have a nephrotoxic effect.
Diagnostics
To diagnose nephrotic syndrome, your doctor will first take a medical history. Asks about symptoms, medications taken, and whether there are any health problems. The doctor will also conduct a physical examination. This may include procedures such as taking your blood pressure and listening to your heartbeat.
Next, the doctor may order tests of biological fluids, which include blood and urine tests, ultrasound examination (ultrasound) of the kidneys and a biopsy.
A kidney biopsy is a procedure that involves removing a small piece of kidney tissue for examination under a microscope. A health care professional performs the biopsy at an outpatient center or hospital. Typically, a specialist will administer local anesthesia, but in some cases general anesthesia may be required. A pathologist—a doctor who specializes in diagnosing diseases—examines the collected pieces of tissue in a laboratory.
What is the difference between the syndromes
The differences between nephritic and nephritic syndrome are in clinical and laboratory manifestations. If in the first case, most patients experience anemia due to hematuria, headaches and high blood pressure, then in the second case they experience poor health, severe weakness, muscle atrophy, more severe anemia, and proteinuria. To make it easier to understand the difference between the two diseases, here is a table:
| Factor of difference | Nephritic syndrome | Nephrotic syndrome |
| Anamnesis | In most cases, it develops against the background of acute infectious pathologies | More often appears in chronic diseases, hyperplastic changes |
| Development | Characterized by unhurried gradual development | Rapidly developing |
| Kidney ultrasound | Enlargement of organs and their heterogeneous structure are visualized | There are signs of deterioration in glomerular filtration rate, but the kidney structure remains unchanged |
| Blood analysis | There is anemia, increased ESR, leukocytosis, decreased CPC | Anemia, increased levels of eosinophils, platelets, increased ESR |
| Analysis of urine | Presence of blood, casts, signs of leukocyturia, relative density increases, protein appears | The appearance of cylinders, relative density increases to 1040, protein - up to 3 g/l |
The difference between diseases is also present in the parameters of biochemical blood tests. With nephritis, hypoproteinemia is often observed, and with nephrosis, the protein level rises to critical levels (up to 60 g/l). Nephrosis is also characterized by a decrease in albumin content.
Treatment of nephrotic syndrome
Healthcare providers will decide how to treat nephrotic syndrome based on its type:
- primary type: medications;
- secondary nephrotic syndrome: treat the underlying disease;
- congenital type of syndrome: medications, surgery to remove one or both kidneys, and transplantation.
Primary nephrotic syndrome
Idiopathic nephrotic syndrome is treated with several types of medications that control the immune system, remove excess fluid, and lower blood pressure.
Drugs Corticosteroids are a group of drugs that reduce the activity of the immune system, reduce the amount of albumin lost in the urine, and reduce swelling. Prednisone or a related corticosteroid is commonly used to treat idiopathic nephrotic syndrome. About 90 percent of patients achieve remission with daily corticosteroids for 6 weeks, followed by slightly smaller doses a few days later for the same 6 weeks. Remission is a period when the patient has no symptoms.
Many patients experience relapses after initial therapy, and health care providers treat them with a short course of corticosteroids until the disease goes into remission again. Children and the elderly may have multiple relapses; however, they most often recover without long-term kidney damage.
When a child has frequent relapses or does not respond to treatment, the doctor may prescribe other medications that reduce the activity of the immune system. These medications prevent the body from producing antibodies that can damage kidney tissue. These include:
- Cyclophosphamide;
- Tacrolimus;
- Cyclosporine;
- Mycophenolate.
Therapeutic measures
Treatment of nephritic syndrome consists of eliminating the underlying disease that became its root cause. Patients are hospitalized in the nephrology department. Experts recommend that patients limit fluid intake, monitor diuresis, and maintain bed rest.
Patients are prescribed diet therapy, which consists of completely eliminating salt from the diet and limiting protein foods. Allowed: vegetarian soups, dairy and fermented milk products, low-fat fish and meat, cereal products, fruit drinks, rosehip decoction, natural juices. Spicy, pickled, spicy, smoked foods, strong coffee, tea, and alcohol are prohibited. Nutrition should be balanced and enriched with vitamins.
Drug therapy:
In case of infectious etiology of the syndrome, antimicrobial agents are prescribed - Cephalexin, Amoxicillin, Azithromycin.- Immunosuppressive therapy is carried out using cytostatics and glucocorticoids - Prednisolone, Methylprednisolone.
- Diuretics reduce the volume of circulating blood - “Diacarb”, “Veroshpiron”.
- Antiplatelet agents and anticoagulants – “Curantil”, “Heparin”.
- To treat arterial hypertension, calcium channel blockers and ACE inhibitors are used - Enalapril, Bisoprolol.
- Pre- and probiotics allow you to restore the intestinal microflora - “Bifiform”, “Lactofiltrum”, “Enterol”.
- Immunostimulants increase the body's resistance to infection - “Imunorix”, “Ismigen”.
- Multivitamins – “Vitrum”, “Centrum”.
- Herbal medicines that support kidney function - “Cyston”, “Canephron”.
- NSAIDs according to indications - “Ibuprofen”, “Nurofen”, “Diclofenac”.
- Antihistamines - “Suprastin”, “Cetrin”, “Diazolin”.
- Restoring hemodynamics and improving microcirculation - Actovegin, Cavinton.
- Dialysis therapy and plasma exchange are indicated for the rapid development of renal failure.
Herbal medicine used to relieve the symptoms of pathology: infusion of dried rose hips, birch leaves, dandelion, horsetail, celery juice, birch sap, decoction of corn silk, sea buckthorn.
If long-term symptomatic therapy and a strict regimen do not restore kidney function and eliminate the cause of the disease, they move on to more radical measures - kidney transplantation.
Forecast
The prognosis of nephrotic syndrome can vary. It depends on what the underlying cause is as well as your overall health.
Some diseases that cause nephrotic syndrome go away on their own or with treatment. After treatment of the underlying disease, nephrotic syndrome should improve. However, other diseases can eventually lead to kidney failure, even with treatment. When this happens, dialysis and possibly a kidney transplant will be required.
If you have warning signs or think you may have nephrotic syndrome, make an appointment with your doctor to discuss your concerns.
Preventive measures
Preventive measures to prevent the development of the syndrome:
- Timely detection and adequate treatment of kidney diseases,
- Careful use of nephrotoxic drugs under medical supervision,
- Sanitation of foci of chronic infection,
- Prevention of pathologies manifested by nephrotic syndrome,
- Dispensary observation by a nephrologist,
- Limiting psycho-emotional stress, stress,
- Elimination of physical overstrain,
- Timely prenatal diagnosis of congenital disease,
- Proper and balanced nutrition,
- Annual medical examination by doctors,
- Pedigree analysis with assessment of renal and extrarenal diseases in close relatives.
The prognosis of the syndrome is ambiguous. It depends on etiopathogenetic factors, age and individual characteristics of the patient, and the treatment performed. Full recovery from this disease is almost impossible. Patients sooner or later experience a relapse of the pathology and its rapid progression. The outcome of the syndrome is often chronic kidney dysfunction, azotemic uremia, or the death of the patient.
Main symptoms of the disease
Since the kidneys are vital organs and their disease can not only reduce the quality and comfort of existence, but in an advanced stage can lead to death, the symptoms of kidney diseases cannot be ignored. These important “bells” from the body about serious problems with the kidneys include:
- regular swelling of the face, arms, legs;
- hematuria and gross hematuria - visually noticeable blood cells in urine (reddening of urine);
- the presence of protein in the urine (a marker of nephritis);
- oligoanuria - the second degree of acute renal failure with a decrease in urine output;
- impetigo is a skin disease caused by streptococci and staphylococci;
- scarlet fever.
The syndromes have similar symptoms and there are differences in the treatment of this renal pathology
There are also nonspecific signs that in themselves may indicate minor or major problems in many body systems, but in combination with the symptoms described above most likely signal a disorder in the functioning of the kidneys:
- persistent pain in the head, abdomen, lower back;
- loss of appetite, sudden weight loss;
- feeling of weakness, weakness;
- nausea, vomiting;
- often high blood pressure;
- heart failure in the acute phase.