One of the most common kidney diseases, difficult to treat and with a serious prognosis, is diffuse glomerulonephritis. The kidneys are a vital organ on whose normal functioning the entire body depends. Every process that occurs in humans is interconnected with the kidneys. Complexion, cheerful sparkle in the eyes, clear skin, clear mind, high performance - these are the qualities that we owe to the kidneys.
When glomerulonephritis begins, the body is gradually destroyed.
The essence of the disease is damage to the glomerular apparatus of the kidneys, which may have:
- spicy;
- subacute;
- chronic course.
First, the glomeruli are affected, then the surrounding interstitial tissue, the process progresses, the kidneys become sclerotic with the development of chronic renal failure (CRF).
The trigger mechanism of the disease is the body's immune response to various provoking factors. The glomeruli are infiltrated by leukocytes and immune complexes, and inflammation of the glomerular apparatus of the kidneys develops.
Considering that all mechanisms in the body are interconnected, a violation of the filtration function of the kidneys entails changes in the acid-base composition, water and electrolyte balance of the body.
The kidney takes part in the metabolism of proteins, carbohydrates, fats, hormones, and vitamins. The preserved nitrogen excretory function of the kidneys ensures the removal of urea, creatinine, indican, and other waste from the blood.
Causes of the disease
Children more often develop acute diffuse glomerulonephritis after streptococcal infection, for example, a complicated course of sore throat, streptoderma.
The chronic process can develop at any age. Acute and chronic presentation of the disease is more common in men.
Previously, it was believed that these were diseases of men from unfavorable social strata. Now all segments of the population are susceptible to chronic diffuse glomerulonephritis, the following provoking factors are identified:
- unfavorable environmental situation - background radiation;
- use of toxic drugs;
- vaccination;
- consumption of low-quality alcohol and other poisons;
- complicated course of childhood infections - chicken pox, infectious mononucleosis, mumps;
- bacterial agents - streptococcus, staphylococcus, diplococcus, syphilis pathogen, enterococcus, toxoplasma, ureaplasma;
- viruses - Epstein-Bar, herpes simplex, hepatitis B, cytomegalovirus;
- systemic connective tissue diseases – systemic lupus erythematosus;
- idiopathic option, when the cause of the disease is unknown.
The most diverse factors in nature lead to damage to the glomerulus, disruption of the filtration function of the kidneys, urine tests change, protein and red blood cells are observed.
The course of glomerulonephritis can be acute or chronic. When diseases develop as a result of complications of diseases of other organs and systems, glomerulonephritis is called secondary, for example, in chronic connective tissue disease.
When diseases are limited only to the kidneys, edema, hypertension are caused by damage to the glomerular apparatus, then this is primary glomerulonephritis.
Primary and secondary glomerulonephritis is idiopathic when the cause is unknown.
Treatment methods
Treatment of acute diffuse glomerulonephritis in children and adults is carried out in a hospital setting. Bed rest is mandatory, as well as a salt-free diet with a reduced protein content, that is, treatment table No. 7 according to Pevzner.
For patients, regardless of age, a single scheme of complex therapy is applied.
- Symptomatic treatment. Aimed at reducing swelling, normalizing blood pressure and restoring urination.
- Pathogenetic therapy. It is carried out to improve blood microcirculation.
- Etiotropic treatment. Prescribed to eliminate the factors that caused the development of the disease.
The choice of drugs depends on the etiology of the disease and is made by the attending physician. An acute diffuse process can be treated using the following medications:
- broad-spectrum antibiotics;
- glucocorticosteroid drugs;
- immunosuppressants;
- nephroprotectors – “Losartan”, “Telmisartan”;
- diuretics - Furosemide, Spironolactone;
- ACE inhibitors for persistent increases in blood pressure - Enalapril, Lisinopril;
- auxiliary drugs - antiplatelet agents, antiallergic agents, vitamins.
This principle of restorative therapy is also applied during exacerbation of the chronic form of the disease, if it is accompanied by severe symptoms. The combination of medications is selected individually in each case.
It is important to know! Patients with acute glomerulonephritis are advised to undergo clinical observation by a nephrologist for the next two years. After completing the course of therapy six months later, in the absence of any complications, the patient is recommended to undergo sanatorium-resort treatment.
The ideal option is a coastal area with warm, dry air, which activates blood circulation, promotes increased sweating and lowers blood pressure.
Classification
Chronic diffuse glomerulonephritis can occur as:
- latent form – changes in urine tests, patients have no complaints;
- with hematuria;
- with high blood pressure (arterial hypertension);
- with the development of nephrotic syndrome, it consists of symptoms - loss of protein, as can be seen from a urine test - proteinuria, edema appears;
- mixed variant, when a set of symptoms of all of the above conditions is observed.
The most insidious and most common, 60% of all chronic glomerulonephritis, is the latent form. There are changes in urine tests, there are no subjective complaints, edema, arterial hypertension are absent in patients, and the kidneys already have serious diseases. This is why it is so important to periodically take blood and urine tests.
The latent form of chronic nephritis, when there is only urinary syndrome, in some cases ends in the development of renal failure.
In some cases, diseases have an undulating course. Exacerbations are replaced by remissions.
Clinic
1). Urinary syndrome:
- Proteinuria
- Hematuria
- Leukocyturia (small)
- Cyllindruria
2). Hypertensive syndrome - see AGN.
3). Edema syndrome - see AGN.
4). Renal failure syndrome.
Clinical forms of CGN:
1). The latent form (the most common) is a weak urinary syndrome without edema and without hypertension. It lasts 10-20 years. Chronic renal failure creeps up unnoticed.
2). Hematuric form (Berge's disease) is isolated hematuria.
3). Nephrotic form (in a third of patients) – proteinuria, severe edema, oliguria. A nephrotic crisis may develop (abdominal pain, fever, erysipelas-like spots on the abdomen, collapse, thrombosis.
4). Hypertensive form (in a third of patients) – hypertension is the only symptom for a long time.
5). Mixed form.
Development of the disease
Depending on which option, the form of glomerulonephritis predominates, different mechanisms of disease development are activated. But they all lead to kidney failure.
In patients, humoral immunity, which is provided by proteins dissolved in body fluids, is reduced. Allergens, or toxins, bind to these proteins rather than being eliminated through the kidneys. Large molecules are formed that settle on the walls of the glomeruli. Microcirculation suffers, ischemia is observed against the background of a perverted immune response - this is the main trigger for the development of glomerulonephritis. Further along the chain, phenomena such as:
- Renal ischemia is regarded by the body as a threat, since it is a vital organ. The main carrier of oxygen, hemoglobin is found in red blood cells. With hypoxia of the renal tissue, an increase in the number of red blood cells is observed. An excess of blood cells leads to a decrease in fluidity and an increase in blood viscosity. The blood supply to organs throughout the body begins to suffer. Secondary hypoxic changes develop.
- The body is trying to make the blood more fluid, to dilute it with liquid. This leads to sodium and water retention, and peripheral edema appears. The body's retention of sodium leads to loss of potassium and disruption of the heart. Excess sodium causes potassium deficiency. Without this microelement, the heart cannot work, which leads to catastrophically progressive heart failure.
- An increase in water in the body against the background of increased blood pressure causes tachycardia. In order to pump an excess amount of blood, the volume of the heart muscle increases - myocardial hypertrophy develops.
- The kidneys produce a substance that helps maintain normal blood pressure. Hypoxia leads to disruption of the production of this hormone. Patients have persistent arterial hypertension that cannot be treated with conventional antihypertensive drugs.
- Large molecules, which are a combination of blood proteins with allergens, settled in the glomerular apparatus of the kidneys, are regarded by the body as a threat that must be eliminated. A large number of leukocytes rush to the kidneys. The vascular endothelium is damaged. An inflammatory response is observed, manifested by a violation of the permeability of the capillary wall. The liquid part of the blood leaves the vascular bed, the body retains the liquid even more to make the blood fluid, and a vicious circle closes. Swelling, symptoms of respiratory failure, heart failure, and disruption of the endocrine system appear and increase.
- The formed elements of blood that clogged the glomerular apparatus gradually became sclerotic, the glomerulus was replaced by connective tissue. When this process affects more than 50% of the glomerular apparatus, glomerulonephritis is called diffuse.
Diffuse glomerulonephritis syndrome
The main clinical syndromes of diffuse glomerulonephritis:
- nephrotic - the body loses protein due to disorders of the glomerular and vascular filters. There is an increase in the protein level in urine tests of more than 3.5, a decrease in the amount of blood protein less than 55, a violation of the ratio of protein fractions, edema, hyperlipidemia;
- nephritic - the body’s reaction to aseptic inflammation of the glomerular apparatus of the kidneys - a certain number of red blood cells and protein appears in urine tests, edema, increased blood pressure (BP).
- Urinary syndrome is manifested by minor changes in tests, in some cases it is an accidental finding.
Causes and symptoms of glomerulonephritis
Glomerulonephritis is an immunoinflammatory process that occurs in the glomerular apparatus of the kidneys.
The disease most often occurs after a streptococcal infection. This is due to the similarity of antigens of streptococcus and kidney tissue.
Antibodies produced by the immune system are aimed at fighting not only the microorganism. The antigen-antibody complex is deposited on the basement membrane of the renal glomeruli, which leads to disruption of microcirculation and organ function.
The development of glomerulonephritis can also be provoked by:
- viruses;
- parasite infestations;
- fungi;
- allergens (food, household);
- medications (antibacterial, sulfonamides);
- serums and vaccines.
The clinical picture develops two to four weeks after streptococcal tonsillitis or other provoking factor. This time period is associated with the formation and accumulation of immune complexes.
The disease can occur latently and be discovered accidentally during preventive examinations, or it can have a violent onset.
Symptoms of glomerulonephritis include:
- pain in the lumbar region;
- change in urine color (takes on a rusty color);
- swelling, most pronounced in the morning, mainly on the face;
- increased blood pressure;
- small amount of urine excreted.
Types and classification
There are acute, subacute (extracapillary, rapidly progressive, malignant) and chronic (lasting over one year) glomerulonephritis.
Based on the extent of kidney damage, the disease is divided into focal and diffuse.
The latter is an unfavorable diagnostic sign, as it leads to a malignant course and pathology and contributes to the rapid development of renal failure.
The nature of the course can be cyclical, manifested by a violent clinical picture with the development of renal edema, arterial hypertension, change in urine color, or latent.
With a latent course, changes are observed only in a general urine test, so patients do not seek medical help, and acute glomerulonephritis becomes chronic.
Clinical picture
At first, patients only experience increased fatigue, dry hair, and brittle nails. Associating this condition more often with hypovitaminosis, they begin to take medications, vitamin supplements, and even greater impairment of kidney function is observed.
The developed clinical picture is characterized by the appearance of:
- decreased appetite;
- weakness, malaise;
- changes in laboratory data - protein, blood, leukocytes, casts in urine tests. The density of urine increases due to the large amount of protein. Reduced protein amount and dysproteinemia, lipidemia, hypercholesterolemia;
- a tendency to increase blood clotting more often leads to the formation of blood clots of any location;
- swelling;
- disruption of the heart leads to heart failure;
- the functions of the pancreas, thyroid gland, and adrenal glands are affected.
Complications of symptoms included in nephrotic syndrome:
- As fluid retention progresses, edema increases, water accumulates in the abdominal cavity - ascites, in the pleural cavity - hydrothorax, and in the pericardial cavity - hydropericardium.
- Edema of the lungs, brain, retina.
- Thrombosis, thromboembolism.
- Ischemic heart disease, myocardial infarction.
- Stroke.
- As a result of a decrease in the volume of circulating blood, its accumulation in peripheral tissues, and protein deficiency, hypovolemic edema develops - a life-threatening condition.
- The addition of infection causes peritonitis, pleurisy, pneumonia, and pleural empyema.
Clinical picture of nephritic syndrome
With a rapidly progressing process, in response to inflammatory changes of a non-bacterial nature, various combinations of specific, nonspecific symptoms of nephritic syndrome develop. Specific symptoms include:
- the appearance of blood in urine tests;
- increased blood pressure;
- decrease in the amount of urine excreted per day;
- swelling;
- changes in immunological blood parameters.
Non-specific symptoms are often characterized by nausea, vomiting, and malaise.
Treatment
Components of treatment:
- elimination of the influence of the etiological factor
- removal of circulating immune complexes and other immune inflammatory factors from the patient’s blood
- reduction of elevated blood pressure and other effects that reduce intraglomerular hypertension
- immunosuppressive therapy
- reduction of edema
- removal of nitrogen metabolic products
- correction of hyperlipidemia and hypercoagulation
In recent years, such a direction as nephroprotective therapy has been developed, which consists of influencing the common non-immune links of their pathogenesis.
General events
The patient needs to exert as little physical effort as possible, avoid hypothermia, and work in low or high temperature conditions. If a person falls ill with an acute respiratory disease, or chronic foci of infection have worsened, they must strictly adhere to bed rest and take antibiotics prescribed by their doctor.
It is recommended to reduce the amount of protein in the diet, with the exception of cases of nephrotic syndrome with hypoalbuminemia below 30 g/l. At the same time, the patient needs to take preparations of essential amino acids and their keto analogues. With nephrotic syndrome, the patient must adhere to a hypocholesterol diet and eat food containing polyunsaturated fatty acids.
Immunosuppressive therapy
Cytostatics and glucocorticoids are used. GCs are effective in severe proteinuria with a high probability of developing nephrotic syndrome and in nephrotic syndrome. For chronic glomerulonephritis, GCs should not be prescribed if the person has chronic renal failure and high arterial hypertension.
In active forms of glomerulonephritis with a high risk of progression of renal failure, cytostatics such as chlorambucil, cyclophosphamide and cyclosporine are relevant. Cyclophosphamide is prescribed as pulse therapy at 15 mg/kg (or 0.6-0.75 g/m2 of body surface) intravenously monthly. A combination of glucocorticosteroids and cytostatics provides a better effect than monotherapy with glucocorticoids.
Selective immunosuppressants such as mycophenolate mofetil and cyclosporine are effective The latter is prescribed for frequent relapses of GC-sensitive nephrotic syndrome and for GC-resistant nephrotic syndrome.
Anticoagulants and antiplatelet agents are used as part of combined regimens for the hypertensive form of glomerulonephritis and chronic glomerulonephritis with isolated urinary syndrome and reduced filtration function of the kidneys.
Danger
Urinary syndrome is characterized by the appearance of small amounts of leukocytes, red blood cells, and protein in the urine. More often, urinary syndrome manifests itself as isolated proteinuria, microhematuria, and leukocyturia, which go unnoticed. There are no changes in the general condition of the patients. Arterial hypertension, no edema. If an increase in the level of leukocytes in the urine is accidentally detected, a person more often begins to independently treat for pyelonephritis, which causes even more harm. Consulting a doctor is necessary with any minimal changes in urine in the initial stages of the disease.
Diagnosis of chronic glomerulonephritis
For diagnosis, it is important to identify the leading syndrome: nephrotic, acute nephrotic, isolated urinary, arterial hypertension. Symptoms of chronic renal failure are also important.
Nephrotic syndrome most often occurs with:
- membranous glomerulonephritis
- glomerulonephritis with minimal changes
- kidney amyloidosis
- diabetic glomerulosclerosis, renal amyloidosis
Acute nephritic syndrome is a combination of hematuria, hypertension, edema and often deterioration of the filtration function of the kidneys. It can occur with the following diseases:
- mesangiocapillary glomerulonephritis
- rapidly progressive glomerulonephritis
- exacerbation of lupus nephritis
- mesangioproliferative glomerulonephritis
Arterial hypertension in combination with proteinuria and minimal changes in urinary sediment occurs, in addition to chronic glomerulonephritis, with diabetic nephropathy, kidney damage as part of hypertension.
Urinary syndrome is a combination of proteinuria, hematuria, cylindruria, leukocyturia with lymphocyturia (any combination of the above).
There are the following causes of isolated hematuria :
- infection
- stone
- tumor in the urinary tract
- Berger's disease
- Allport's disease
Proteinuria occurs with inflammatory and non-inflammatory lesions of the glomeruli or with tubulointerstitial lesions of various etiologies. A special variant of massive proteinuria is overflow proteinuria, which is associated with the presence of paraprotein in the blood and myeloma. Benign proteinuria occurs with obstructive sleep apnea syndrome, heart failure; sometimes occurs during emotional stress, hypothermia, or becomes a consequence of a febrile reaction. It is called benign because the prognosis for kidney function is favorable.
Kidney biopsy
A puncture biopsy of the kidney is performed to determine the morphological form of chronic glomerulonephritis, which affects the choice of treatment tactics. Contraindications :
- Hypocoagulation
- The presence of not two, but one functioning kidney
- Suspicion of renal vein thrombosis
- Suspicion of malignancy
- Increased venous pressure in the systemic circulation
- Polycystic kidney disease
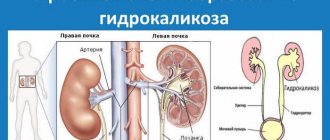
- Hydro- and pyonephrosis
- Impaired consciousness
- Renal artery aneurysm
Differential diagnosis
Differential diagnosis is carried out with the following diseases:
- acute glomerulonephritis
- chronic pyelonephritis
- chronic tubulointerstitial nephritis
- nephropathy in pregnancy
- amyloidosis
- alcoholic kidney damage
- kidney damage in systemic connective tissue diseases
- diabetic nephropathy
Characteristic features of chronic pyelonephritis that need to be taken into account when diagnosing:
- neutrophiluria
- bacteriuria
- exacerbations with fever and chills
- changes in the collecting system
- asymmetry of the lesion
In acute glomerulonephritis, a history of connection with a previous streptococcal infection is considered, but, however, unlike IgA nephropathy, the time interval is 10-14 days. Typically acute onset. Among the patients are mainly teenagers and children.
Chronic tubulointerstitial nephritis has the following features (taken into account in differential diagnosis):
- slight proteinuria
- polyuria
- urine acidification disorder
- decreased relative density of urine
If amyloidosis is suspected, an underlying pathology should be looked for, namely chronic inflammation, which occurs, for example, with rheumatoid arthritis. Amyloidosis is suspected when chronic renal failure persists with enlarged or normal kidney size and in the presence of nephrotic syndrome. Tissue biopsy is of decisive importance in the differential diagnosis of such cases.
The diagnosis of diabetic nephropathy is likely (as well as chronic pyelonephritis) if a person has diabetes mellitus or its complications, slowly increasing chronic renal failure, scanty changes in urinary sediment, normal or slightly enlarged kidney sizes.
Nephropathy in pregnant women is said to occur if symptoms of kidney damage appear in the second half of the gestational period, accompanied by high hypertension and other signs of preeclampsia and eclampsia.
When can glomerulonephritis be diagnosed?
List of manifestations that should alert and urgently send patients
to the doctor:
- A few weeks after streptococcal or any other infection, swelling appears, an increase in blood pressure, protein, and blood cells in urine tests are noted. The latter are not visible to the naked eye. Important! 1-2 weeks after any infectious or viral disease, take a urine test.
- Suddenly detected arterial hypertension should immediately send patients to examine not only the heart, but also the kidneys to find the cause and prescribe adequate treatment.
- Minor changes in urine tests accidentally discovered during a routine examination should alert you. Given the excellent compensatory abilities of the kidneys, severe disorders appear in advanced stages. Diseases must be identified at the very beginning. This will improve treatment results and significantly prolong life.
- If there is hypertrophy of the heart muscle, along with a cardiac examination, it is necessary to undergo a kidney examination. Heart damage is observed, which is often secondary to kidney disease. Isolated treatment of the heart will not be effective.
- Swelling of the face in the morning is one of the most dangerous symptoms of kidney disease.
- More than 80% of waste, toxins, and end products of metabolism are removed from the body with urine. The appearance of skin itching and rashes is a reason to examine the kidneys.
Acute diffuse glomerulonephritis
Suddenly, acutely after an infection, intoxication or vaccination, swelling appears on the face, the amount of urine decreases to 400-500 ml per day, and its density increases. This is observed as acute diffuse glomerulonephritis. Some of the main symptoms are protein in the urine and a reduced amount of sodium. More often, patients pay attention to the appearance of blood in the urine, a rapid increase in body weight by 10-15 kg in a short period of time.
This form of glomerulonephritis rarely ends in anuria. For acute nephritis, one of the most significant symptoms is arterial hypertension. Pain in the kidney area often develops with increasing size and tension of the capsule.
Against the background of an acute attack of diffuse glomerulonephritis, eclampsia or cerebral edema is more often observed. The second significant danger of acute nephritis is that arterial hypertension appears that is resistant to taking antihypertensive drugs.
The predominance of night urination over daytime urination, which does not happen normally, and low urine density should alert patients. At the slightest suspicion of acute nephritis, you should consult a doctor. Performing the Zimnitsky, Nechiporenko, Volgard tests will allow you to quickly make a diagnosis and begin adequate treatment of acute nephritis or a chronic process.
Important! Edema, impaired renal function in the form of protein, red blood cells in the urine, increased pressure require immediate medical attention, as they are symptoms characteristic of acute diffuse glomerulonephritis.
Chronic diffuse glomerulonephritis
- urinary;
- hematuric;
- hypertension;
- neurotic;
- mixed.
Exacerbation of chronic nephritis is most often manifested by swelling of the face in the morning, change in the color of urine, decreased diuresis, increased blood pressure, headache, malaise, general weakness, and decreased performance.
Chronic diffuse glomerulonephritis may have a latent course, then there will be no clinical symptoms. Diseases in remission are also manifested by the absence of symptoms. In contrast to acute diffuse glomerulonephritis, in chronic glomerulonephritis there is always hypertrophy of the left ventricular myocardium. Violations of the nitrogen excretory function of the kidneys are more common, and many patients develop chronic renal failure within 1 year.
Difference between pyelonephritis and glomerulonephritis: differential diagnosis of diseases
Glomerulonephritis and pyelonephritis are kidney diseases.
If untimely and incorrectly selected treatment can lead to functional failure of the organ.
What is the difference in the clinical picture, diagnosis and treatment of diseases?
Causes and symptoms of glomerulonephritis
Glomerulonephritis is an immunoinflammatory process that occurs in the glomerular apparatus of the kidneys.
The disease most often occurs after a streptococcal infection. This is due to the similarity of antigens of streptococcus and kidney tissue.
Antibodies produced by the immune system are aimed at fighting not only the microorganism. The antigen-antibody complex is deposited on the basement membrane of the renal glomeruli, which leads to disruption of microcirculation and organ function.
The development of glomerulonephritis can also be provoked by:
- viruses;
- parasite infestations;
- fungi;
- allergens (food, household);
- medications (antibacterial, sulfonamides);
- serums and vaccines.
The clinical picture develops two to four weeks after streptococcal tonsillitis or other provoking factor. This time period is associated with the formation and accumulation of immune complexes.
The disease can occur latently and be discovered accidentally during preventive examinations, or it can have a violent onset.
Symptoms of glomerulonephritis include:
- pain in the lumbar region;
- change in urine color (takes on a rusty color);
- swelling, most pronounced in the morning, mainly on the face;
- increased blood pressure;
- small amount of urine excreted.
Types and classification
There are acute, subacute (extracapillary, rapidly progressive, malignant) and chronic (lasting over one year) glomerulonephritis.
Based on the extent of kidney damage, the disease is divided into focal and diffuse.
The latter is an unfavorable diagnostic sign, as it leads to a malignant course and pathology and contributes to the rapid development of renal failure.
The nature of the course can be cyclical, manifested by a violent clinical picture with the development of renal edema, arterial hypertension, change in urine color, or latent.
With a latent course, changes are observed only in a general urine test, so patients do not seek medical help, and acute glomerulonephritis becomes chronic.
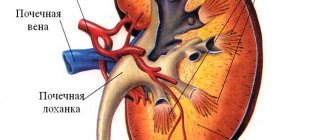
Etiology and clinical picture of pyelonephritis
Pyelonephritis is an inflammatory disease of the renal pyelocaliceal structures involving microorganisms. The disease can affect the right, left, or both kidneys. Provoking factors for pyelonephritis include:
- frequent hypothermia;
- the presence of a focus of chronic inflammation in the body;
- anatomical features of the kidneys;
- diabetes;
- immunodeficiency;
- urolithiasis disease;
- prostate adenoma in men.
Pathogenic microorganisms can enter the kidneys through the ascending route, as well as through the blood and lymph. The ascending path occurs in the presence of inflammation in the ureters, bladder, and urethra.
In women, the urethra is shorter and wider than in men, so urethritis and cystitis are more common in them.
Microorganisms are spread throughout the body from another source of the infectious process through the blood and lymph.
Symptoms of pyelonephritis include:
- intoxication of the body (body temperature 38-40 C, feeling of weakness, fatigue, chills);
- pain in the lower back, can be localized either on the right or on the left, it depends on the side of the lesion, the pain syndrome can shift to the groin;
- cloudy urine with a strong foul odor.
Shapes and types
Pyelonephritis is divided into acute and chronic. Acute has a sudden onset and a violent clinical picture. With proper therapy, the patient recovers completely.
Chronic pyelonephritis is a sluggish bacterial inflammatory process with periodic exacerbations. Subsequently, the renal tissue gradually becomes sclerotic, which leads to renal failure.
The disease can affect either one or two kidneys.
Differential diagnosis
To carry out a differential diagnosis of pyelonephritis and glomerulonephritis, the patient’s complaints are clarified, an anamnesis is collected, an examination, laboratory, instrumental and morphological research methods are performed.
Glomerulonephritis studies
Glomerulonephritis is supported by recent tonsillitis, vaccination, allergic diseases, and the presence of the disease in close relatives.
With glomerulonephritis, both kidneys are affected, so the pain syndrome is evenly expressed on both sides. Since the vascular glomeruli are damaged, the patient notes a change in urine color from pink to rusty.
In a general urine test, the following changes are observed:
- hematuria (red blood cells in the urine, normally absent);
- proteinuria (protein in urine);
- decreased urine density (concentrating ability of the kidneys decreases).
Ultrasound, computed tomography and magnetic resonance imaging reveal changes in the renal parenchyma.
A reliable diagnosis can only be made after a morphological study. In this case, a kidney biopsy (a fragment of organ tissue) is taken and its cortex and medulla are studied. Based on this study, a prognosis of the disease can be made.
Study of pyelonephritis
Since pyelonephritis often affects one kidney, the pain syndrome is clearly localized to the right or left. The disease is accompanied by massive intoxication of the body (fever).
The urine becomes cloudy and has a foul odor due to the presence of bacteria in it.
A general urine test contains leukocytes and bacteriuria (a large number of microorganisms).
Ultrasound of the kidneys shows dilation of the collecting system.
In chronic pyelonephritis with frequent exacerbations, renal failure gradually develops.
Differences between pyelonephritis and glomerulonephritis
| Sign | Pyelonephritis | Glomerulonephritis |
| Kidney damage | Most often unilateral | Always two-sided |
| Symptoms | Fever, cloudy urine with a strong foul odor, lower back pain | Swelling on the face mainly in the morning, change in urine color from pinkish to red |
| General urine analysis | Cloudy urine with a large number of white blood cells and bacteria | Red blood cells and protein in urine |
Basic treatment of glomerulonephritis
When a diagnosis of glomerulonephritis is established, glucocorticosteroids are prescribed to suppress the immune system and reduce the formation of antigen-antibody complexes.
In a rapidly progressing process, cytotoxic drugs may be added to steroids.
Doses are selected individually. Medicines have many side effects, so treatment is carried out under the strict supervision of a doctor.
Glucocorticosteroids are discontinued gradually, as otherwise acute adrenal insufficiency can be caused.
Of great importance is the patient's adherence to a diet that limits the intake of protein and salt.
Spicy, smoked, and canned foods are completely excluded. Strict recording of the amount of fluid consumed and excreted is kept.
In the presence of high blood pressure and edema syndrome, antihypertensive drugs and diuretics are prescribed. Prevention of blood clots (clopidogrel) is carried out. To improve microcirculation, pentoxifylline is prescribed.
In some cases (rapidly progressing glomerulonephritis), hemodialysis may be necessary, which is performed using an “artificial” kidney apparatus.
Therapy of pyelonephritis
In case of acute and exacerbation of chronic pyelonephritis, antibacterial drugs are mandatory.
The patient is prescribed a diet. Plentiful consumption of non-concentrated fruit drinks made from cranberries, lingonberries and tea is recommended. This contributes to the speedy sanitation of the source of infection.
Treatment of chronic pyelonephritis in the remission stage is aimed at preventing exacerbations of the disease (prevention of hypothermia, strengthening the immune system).
Disease Prevention
Prevention of pyelonephritis and glomerulonephritis includes:
- maintaining a healthy lifestyle (moderate physical activity, healthy eating, hardening);
- avoiding hypothermia;
- timely treatment of infectious diseases;
- rehabilitation of chronic foci of infection;
- annual preventive examinations.
Prognosis for recovery
Acute glomerulo- and pyelonephritis, with timely diagnosis and correct treatment, result in complete recovery of the patient.
The subacute form of glomerulonephritis is malignant, requires the use of cytostatics, is difficult to treat and leads to renal failure.
In chronic pyelo- and glomerulonephritis, prevention of exacerbations of the disease is important. The more often exacerbations occur, the more the kidneys suffer.
With frequent exacerbations, the renal parenchyma is replaced by connective tissue. Thus, the organ cannot perform its function, and kidney failure develops.
Kidney failure progresses steadily, and then treatment is hemodialysis and kidney transplantation.
We recommend other articles on the topic
Source: //UroHelp.guru/pochki/glomerulonefrit/otlichie-ot-pielonefrita.html
Diagnostics
A quick and accurate diagnosis will prevent the onset of chronic renal failure. Despite the similarity of clinical manifestations, the mechanism of development of kidney diseases is different, treatment will be different. To identify the predominant mechanism of development of syndromes, symptoms, and determine structural changes in kidney tissue, the following are performed:
- biopsy;
- immunological diagnostics;
- blood and urine tests;
- Ultrasound;
Differential diagnosis should be carried out with the following types of kidney diseases:
- Pyelonephritis differs from acute glomerulonephritis by increased body temperature, absence of red blood cells, and a high content of leukocytes in the blood of patients.
- Nephropathy in pregnant women is characterized by severe urinary syndrome.
- Tubulo-interstitial nephritis is characterized by the appearance of disease of the tubules, interstitium, in contrast to acute glomeruloneuritis.
- Toxic, for example alcoholic kidney damage.
- Amyloidosis is a disorder of protein metabolism throughout the body. At the initial stages of the disease, accumulation of amyloid protein occurs in all organs and tissues of patients, in contrast to acute or chronic glomerulonephritis.
- Lupus nephritis in patients with systemic lupus erythematosus.
- Periarteritis nodosa, or Kussmaul-Mayer disease, has a benign course, the cutaneous form of the lesion predominates. The kidneys are extremely rarely involved in the process, and the phenomena of chronic latent glomerulonephritis develop.
- Wegener's granulomatosis in patients is characterized by autoimmune damage to the walls of small vessels of the bronchi, lungs, and eyes. The kidneys are the last to join when there is a generalized form of the lesion. The phenomena of intoxication, pain in muscles, joints, and increased body temperature come to the fore. After this, the phenomena of acute glomerulonephritis occur and kidney function is impaired.
- Goodpasture's disease is characterized by a set of symptoms - pulmonary hemorrhages, pneumonia, a form of damage with the development of glomerulonephritis. The course of the disease is unfavorable.
- Hemorrhagic vasculitis in patients is characterized by.
- Urolithiasis disease.
- Oncological diseases.
- Hypersensitive vasculitis, Henoch-Schönlein disease in patients is characterized by thrombosis of small vessels after suffering streptococcal and viral infections. It differs from chronic nephritis and acute glomerulonephritis by the presence of skin rashes. The joint form is characterized by muscle and joint pain. The abdominal form is accompanied by gastrointestinal bleeding and hemorrhages in the abdominal organs. The phenomena of classic acute glomerulonephritis often occur when there is a fulminant form of the disease, which usually ends in death.
- Hereditary nephritis - Alport's diseases. The disease begins to manifest itself at 5-7 years of age. The child has asymptomatic microhematuria and protein in the urine. They are detected by chance when there is a latent course of chronic glomerulonephritis. Along with pronounced urinary syndrome, there is a decrease in hearing, vision, edema, and additional external congenital developmental anomalies. Kidney function begins to suffer significantly by the age of 18-20 years, and chronic renal failure develops.
A guide to internal medicine, propaedeutics, and general care. / CHRONIC GLOMERULONEPHRITIS
CHRONIC GLOMERULONEPHRITIS
This is a bilateral inflammatory disease of the kidneys of immune origin, which is characterized by gradual but steady death of the glomeruli, shrinkage of the kidney, gradual decrease in function, development of arterial hypertension and death from chronic renal failure.
The frequency is about 4 per 1000 autopsies. The incidence of men and women is the same. It is found in all countries of the world, but more often in cold ones.
Etiology
It is not completely clear, some have a history of acute glomerulonephritis, other cases are not clear. Sometimes the provoking factor can be repeated vaccination, drug therapy - for example, antiepileptic drugs.
Pathogenesis
It is based on an immunological mechanism. Morphologically, deposits of immune complexes consisting of immunoglobulin and complement are found in the area of the basement membrane. The nature of immune deposits can be different: if there are a lot of them, coarse deposits, severe damage. Sometimes the protein composition of the membrane itself may change.
Classification
- Clinical:
A). The latent form is nephritis with isolated urinary tract.
b). Chronic glomerulonephritis with a nephrotic component (nephrosonephritis). The main manifestation is nephrotic sm.
V). The hypertensive form occurs with an increase in blood pressure and progresses slowly.
G). Mixed form.
- Histological (arose with the advent of intravital biopsy followed by electron microscopy.
A). Chronic glomerulonephritis with minimal lesions. At el. microscopy reveals changes in the basement membrane, mainly in podocytes - cells of the visceral layer of the Shumlyansky-Bowman capsule. The outgrowths of podocytes merge, representing a single system with immune deposits. Clinic: often in children (65-80%). Previously it was called lipoid nephrosis, but this is incorrect, since nephrosis is a lesion of the renal tubules, and here the glomeruli are affected. Corresponds to chronic glomerulonephritis with nephrotic syndrome: severe proteinuria (high selectivity) can be up to 33%; hypoproteinemia (hypoalbuminemia); edema due to a decrease in plasma ocotic pressure (hypoxia), due to edematous fluid, the amount of blood proteins decreases even more - hypovolemia, secondary hyperaldosteronism, increased edema; hypercholesterolemia, as well as an increase in triglycerides (up to 3-5 thousand mg). Previously, it was believed that hypercholesterolemia compensatory increases oncotic pressure. It has now been established that oncotic pressure increases slightly due to lipids. The reason for hypercholesterolemia is a decrease in the lipolytic activity of the liver. In general, this is a benign form. It almost never leads to death, but infection, hypertension, and hematuria may result in a shriveled kidney.
b). Membranous variant of nephritis: the basement membrane is affected more deeply. With conventional microscopy, there is thickening, membrane ruptures, and large deposits of immunoglobulins and complement. The clinical picture is most often based on the type of nephrosonephritis. The course is more malignant. Slight hematuria, gradual increase, outcome in a secondary shriveled kidney.
V). Fibroplastic variant: processes on the basement membrane occur quickly, the mesangium is activated, the membrane continues to grow, the growth of the glomeruli occurs more slowly. Clinic: hypertension, urinary syndrome is mild, sometimes there are only periodic changes in the urine, there is no edema at the beginning; then real glomerulonephritis appears with edema and hypertension. This form is favorable in terms of the duration of the disease, but almost always results in a secondary wrinkled kidney and chronic renal failure.
G). Proliferative variant: there is a massive proliferation of mainly the vascular endothelium (endocapillary type), less often proliferation is of the extracapillary type - from the side of Bowman’s capsule. More often it is a mixed form, the clinical manifestation is arterial hypertension.
d). Membranous-proliferative: b) + d) . The hypertensive form of chronic glomerulonephritis with the clinic of the classical form of hypertension is specially distinguished, but there are changes in the urine. The degree of change in the fundus may be greater than in HD.
Differential diagnosis
- Acute glomerulonephritis: anamnesis is important, the time from the onset of the disease, the specific gravity is high throughout the disease, and with chronic glomerulonephritis there may be a decrease in the specific gravity of urine. Left ventricular hypertrophy may be pronounced. Hypertension. Histological examination is of decisive importance - the presence of hyperplastic processes.
- A malignant form of hypertension: now extremely rare. Persistent high blood pressure 260/130-140 or more. Significant changes in the fundus. Then, urinary syndrome may also occur.
- Chronic pyelonephritis: a history of often gynecological diseases, abortions, cystitis. There is a tendency to low-grade fever. Pyuria. Bacteriouria, early decrease in urine specific gravity. The presence of radiological signs of pyelonephritis (the calyces become sclerotic early and change their shape).
- Polycystic kidney disease: appears at 30-40 years of age. The presence of enlarged kidneys on both sides. X-ray examination shows the presence of an uneven scalloped edge of the kidneys and a cyst. Hypertension, azotemia. Early causes chronic renal failure.
- Renal amyloidosis: usually a picture of nephrotic syndrome. Occurs against the background of long-term chronic inflammation. Often combined with amyloidosis of the liver and spleen, there may be intestinal amyloidosis (diarrhea, exhaustion, weight loss). There may also be primary amyloidosis - there is no history of suppurative diseases. May occur in very old people; the tongue becomes very large (does not fit in the mouth), enlargement of the heart. Diagnostics is helped by a test with Congo-r. Biopsy of the oral mucosa or, preferably, the rectum with a test for amyloid (with iodine).
- Diabetic glomerulosclerosis: occurs when diabetes is unrecognized or severe and poorly treated. Hyalinosis of the renal vessels and death of the renal glomeruli occurs.
Clinic: only neurotic syndrome, and only in the later stages hypertension and renal failure are added.
- Multiple myeloma with myeloma kidney: nephrotic syndrome is often associated with kidney damage. Diagnostics is helped by a picture of the blood and bone marrow, an increase in protein fractions of the blood, and the appearance of paraproteins in the blood - Ben-Jones protein.
Forecast
For glomerulonephritis with minimal changes - good. Recovery may be defective - small but progressive proteinuria. Most often the course is progressive and results in chronic renal failure.
Complications
1. In the hypertensive form - cerebral hemorrhage, retinal detachment.
2. With nephrosclerosis - the addition of various infections.
3. Chronic renal failure.
Treatment
1. In case of exacerbation of streptococcal infection - penicillin.
2. For hypertension - antihypertensives, saluretics - furosemide, lasix. Doses should be moderate, because due to kidney damage there may be cumulation. Veroshpiron.
3. Impact on autoimmune processes: corticosteroids and cytostatics are advisable only for glomerulonephritis with minimal lesions - this is an absolute and justified indication, the effect is 80-100%: prednisolone 40-60 mg/day. 3 weeks. If the treatment is effective, then a positive effect will appear at week 4; if there is a positive effect, they switch to maintenance doses of 5-10 mg/day. during a year. It is better to carry out therapy in courses, as side effects are reduced: a/4+3 (4 days prednisolone, 3 days rest) 6/7+7, you can combine hormones with cytostatics - imuran 100 mg. cyclophosphamide 150-200 mg/day. In fibroplastic forms, cytostatics are futile.
4. To reduce proteinuria: indomethacin 0.025.
5. Anabolic agents: retabolil (increases protein synthesis).
6. Anticoagulants: heparin - improves microcirculation in capillaries, anti-complementary effect, but can increase hematuria.
7. Vitamins in large doses, especially vitamin C.
8. Glucose 40% IV solution.
9. Diet therapy: water-salt regimen (since the amount of water and salt decreases with edema): for hypertension, heart failure - water restriction: in the absence of azotea, the amount of protein is 1 g/kg of weight: for nephrotic syndrome, food protein in adults is raised to 2 g/kg per day. Protein loss is determined in the daily amount of urine - proteinuria over 5 g/day is considered massive.
10. Normal mode. Bed rest - in the most severe cases.
11. Spa therapy.
12. Physiotherapy: diathermy, heat.
13. Sanitation of foci of chronic infection.