Diffuse glomerulonephritis is an immunoallergic disease with predominant damage to the glomerular vessels: it occurs as an acute or chronic process with repeated exacerbations and remissions. In more rare cases, subacute glomerulonephritis is observed, which is characterized by a rapid progressive course, quickly leading to renal failure. Diffuse glomerulonephritis is one of the most common kidney diseases.
Acute glomerulonephritis is a disease of infectious-allergic nature with primary damage to the capillaries of both kidneys. Distributed everywhere. They are most often affected at the age of 12-40 years, somewhat more often in men. Occurs in countries with cold and humid climates and is a seasonal disease.
Occurrence of the disease Acute glomerulonephritis
The disease most often occurs after tonsillitis, tonsillitis, upper respiratory tract infections, scarlet fever, etc. Streptococcus plays an important role in the occurrence of gpomerulonephritis, especially type 12 beta-hemolytic streptococcus group A. In countries with hot climates, acute glomerulonephritis is most often preceded by streptococcal skin diseases. It can also develop after pneumonia (including staphylococcal), diphtheria, typhus and typhoid fever, brucellosis, malaria and some other infections. Glomerulonephritis may occur under the influence of a viral infection, after the administration of vaccines and serums (serum, vaccine nephritis). Ethnological factors also include cooling the body in a humid environment (“trench” nephritis).
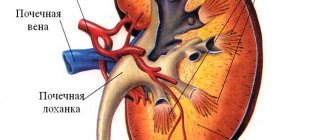
Cooling causes reflex disorders of the blood supply to the kidneys and affects the course of immunological reactions. Currently, the generally accepted idea is that acute glomerulonephritis is an immune complex pathology; the appearance of symptoms of glomerulonephritis after an infection is preceded by a long latent period, during which the body’s reactivity changes and antibodies to microbes or viruses are formed. Antigen-antibody complexes, interacting with complement, are deposited on the surface of the basement membrane of capillaries, mainly in the glomeruli. Generalized vasculitis develops, affecting mainly the kidneys.
Mechanisms of occurrence
When glomerulonephritis develops in the human body, the entire body is exposed to the disease due to the penetration of pathogenic microorganisms into the kidney tissue. In addition, the protective system also damages the kidney tissue in the process of providing protection from harmful factors. The disease also has a very large impact on the body due to a hereditary predisposition to this disease.
Streptococcus is the most common cause of glomerulonephritis
The most important cause of the disease is streptococcus, which can affect the upper respiratory tract through ordinary infections, as well as cause inflammation of the skin, and when the body tries to protect itself from the disease, it will damage the kidneys.
Acute glomerulonephritis that occurs due to exposure to streptococcal disease is called post-streptococcal glomerulonephritis. Other diseases, as well as other types of viruses, may well be the main cause of glomerulonephritis, but they are not so common.
Infectious-immune glomerulonephritis is so called because it was caused by one of the types of infection, but there are also non-infectious-immune glomerulonephritis, and they arise due to personal intolerance to drugs and vaccines, as well as due to increased sensitivity to them.
This also applies to any chemicals, insect poisons and plant pollen.
If a person has a hereditary predisposition to this type of disease, which plays a significant role, then alcohol intoxication may be the cause of its occurrence.
Diseases such as ARVI and hypothermia can become a platform for the formation of post-streptococcal glomerulonephritis, this also applies to carrying streptococcus in the mouth or on the skin.
Carriage of this disease is not the disease itself and does not pose any threat to other people, but this condition only lasts until the immunity decreases, because after that this type of bacteria becomes active and causes the disease.
The main reason for the development of the disease is immune reactions, however, in order to understand the mechanism of disease development, it is necessary to consider some of the concepts of immunity mechanisms.
Course of the disease Acute glomerulonephritis
Various immunological disorders play a role in pathogenesis.
1) Formation of conventional antibodies. The antigen-antibody complex can settle on the renal membrane, since it has rich vascularization, predominantly large deposits settle. The antigen-antibody reaction takes place on the renal membrane itself, while complement and biologically active substances are present: histamine, hyaluronidase, and the capillaries of the whole body may also suffer.
2) With streptococcal infection, streptococcal antigen can damage the endothelium of the renal capillaries, the basement membrane, the epithelium of the renal tubules - autoantibodies are formed, and an antigen-antibody reaction occurs. Moreover, damaged cells act as antigens.
3) The basement membrane of the kidneys and streptococcus have common antigenic structures, so normal antibodies to streptococcus can simultaneously damage the basement membrane - a cross-reaction.
Proof that the disease is based on immune processes is that between streptococcal infection and the onset of acute nephritis there is always a time interval during which the accumulation of antigens and antibodies occurs, which is 2-3 weeks.
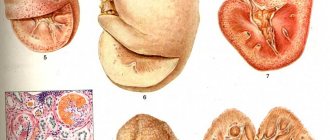
Pathological anatomy
At autopsies of those who died from acute diffuse glomerulonephritis, kidneys of normal or enlarged sizes and gray-brown or brown color are found. On the section, Malpighian bodies protrude in the form of pinpoint tubercles. Microscopically, at the initial stages of the disease, enlarged, hyperemic renal glomeruli are detected. At later stages of the disease - ischemia of the renal glomeruli, fibrinoid swelling of the renal capillaries, accumulation of protein exudate between the capillary loops and the glomerular capsule, blood stasis, thrombosis of the capillary loops, hemorrhages. Pathological changes are determined in the tissues of both kidneys.
Prevention is the surest way to prevent disease
In order not to treat acute glomerulonephritis, preventive measures are taken. Prevention is based on timely treatment of pathologies of the respiratory organs located at the top. It is required to undergo timely diagnosis and fight pathogenic viruses and bacteria. It is not recommended to overcool the pelvic organs and allow allergic reactions in the body. It is important to strengthen the immune system through proper nutrition and taking vitamin and mineral complexes. With timely detection and treatment, the prognosis for a favorable outcome is 80%; in children this figure is higher - 95%. In this case, it is possible to completely restore the functioning of the internal organ. To avoid relapse, regular examinations by a doctor are carried out.
Symptoms of the disease Acute glomerulonephritis
Acute glomerulonephritis is characterized by three main symptoms - edematous, hypertensive and urinary. Mainly protein and red blood cells are found in urine. The amount of protein in the urine usually ranges from 1 to 10 g/l, but often reaches 20 g/l or more. However, a high protein content in the urine is observed only in the first 7-10 days, therefore, with a late urine test, proteinuria is often found to be low (less than 1 g/l). In some cases, slight proteinuria may be present from the very beginning of the disease, and in some periods it may even be absent. Small amounts of protein in the urine of patients who have had acute nephritis are observed for a long time and disappear only after 3-6, and in some cases even 9-12 months from the onset of the disease.
Hematuria is a mandatory and constant sign of acute gpomerulonephritis; in 13-15% of cases there is macrohematuria, in other cases there is microhematuria, sometimes the number of red blood cells may not exceed 10-15 in the field of view. Cylindruria is not a necessary symptom of acute gpomerulonephritis. In 75% of cases, single hyaline and granular casts are found, sometimes epithelial casts are found. Leukocyturia, as a rule, is insignificant, but sometimes 20-30 leukocytes or more are found in the field of view. At the same time, there is always a quantitative predominance of erythrocytes over leukocytes, which is better revealed when counting the signature elements of urine sediment using the Kakovsky-Addis, De Almeida-Nechiporenko methods.
Oliguria (400-700 ml of urine per day) is one of the first symptoms of acute nephritis. In some cases, anuria (acute renal failure) occurs for several days. Many patients experience slight or moderate azotemia during the first few days of the disease. Often with acute glomerulonephritis, the hemoglobin content and the number of red blood cells in the peripheral blood decrease. This is associated with hydremia (increased water content in the blood), and may also be due to true anemia as a result of the influence of an infection that led to the development of glomerulonephritis (for example, with septic endocarditis.
An elevated ESR is often detected. The number of leukocytes in the blood, as well as the temperature reaction, are determined by the initial or concomitant infection (usually the temperature is normal and there is no leukocytosis).
Of great importance in the clinical picture of acute glomerulonephritis are edema, which serves as an early sign of the disease in 80-90% of patients; They are located mainly on the face and, together with the pallor of the skin, create the characteristic “nephritic face.” Often fluid accumulates in cavities (pleural, abdominal, pericardial cavity). Body weight gain in a short time can reach 15-20 kg or more, but after 2-3 weeks the swelling usually disappears. One of the cardinal symptoms of acute diffuse gpomerulonephritis is arterial hypertension, observed in 70-90% of patients. In most cases, blood pressure does not reach high levels (180/120 mm Hg). Increases in blood pressure occur less frequently in children and adolescents than in adults. Acute arterial hypertension can lead to the development of acute heart failure, especially left ventricular failure. Later, hypertrophy of the left ventricle of the heart may develop. The examination reveals an expansion of the boundaries of cardiac dullness, which may be due to the accumulation of transudate in the pericardial cavity and myocardial hypertrophy. Often a functional systolic murmur is heard at the apex, an accent of the second tone on the aorta, and sometimes a gallop rhythm: dry and moist rales in the lungs. The ECG may show changes in the R and T waves in standard leads, often a deep Q wave and a slightly reduced voltage of the ORS complex.
Arterial hypertension in acute glomerulonephritis may be accompanied by the development of eclampsia, but there is no uremia. Eclampsia is more correctly considered acute encephalopathy, since it is caused by arterial hypertension and edema (hypervolemic cerebral edema). Despite the severe clinical picture of eclamptic seizures, they rarely end in death and mostly pass without a trace.
There are two most characteristic forms of acute glomerulonephritis. The cyclic form begins violently. Swelling, shortness of breath, headache, pain in the lumbar region appear, and the amount of urine decreases. Urine tests showed high levels of proteinuria and hematuria. Blood pressure rises. Swelling lasts 2-3 weeks. Then, during the course of the disease, a turning point occurs: polyuria develops and blood pressure decreases. The recovery period may be accompanied by hyposthenuria. However, often, when patients feel well and have almost completely restored their ability to work, slight proteinuria (0.03-0.1 g/l) and residual hematuria may be observed for a long time, for months. The latent form is common, and its diagnosis is of great importance, since often with this form the disease becomes chronic. This form of glomerulonephritis is characterized by a gradual onset without any significant subjective symptoms and is manifested only by slight shortness of breath or swelling in the legs. In such cases, glomerulonephritis can only be diagnosed with a systematic examination of urine. The duration of the relatively active period in the latent form of the disease can be significant (2-6 months or more).
Acute glomerulonephritis may be accompanied by nephrotic syndrome. Any acute glomerulonephritis that does not end without a trace within a year should be considered to have become chronic. It should be remembered that in some cases, acutely onset diffuse glomerulonephritis can take on the character of subacute malignant extracapillary glomerulonephritis with a rapidly progressive course.
What complications can there be?
Complications of acute glomerulonephritis are rare today. But we must know about them and try to warn them. Acute renal glomerulonephritis can be complicated by the following syndromes: renal eclampsia, acute left ventricular failure, acute renal failure.
Renal eclampsia is a syndrome caused by narrowing of the blood vessels in the brain, as well as its swelling, manifested by loss of consciousness, convulsions, and short-term loss of vision. Attacks of renal eclampsia usually last two to three minutes, but can occur in succession of three to four attacks. Occurs in 8% of cases.
Acute left ventricular failure is a weakened ability of the left ventricle of the heart to contract. It manifests itself predominantly in older patients, usually with concomitant cardiovascular pathology. It occurs due to a sharp rise in blood pressure and overload of the left side of the heart. The left ventricle cannot pump out the increasing volumes of blood, and congestion occurs. Occurs in 3% of cases.
Acute renal failure is a fast-acting disease leading to cessation of kidney function. He is being treated in the intensive care unit. The artificial kidney device helps maintain the condition and promotes kidney recovery. Occurs in 1% of cases.
What could be the prognosis?
Recovery occurs in approximately 80% of patients (in children - in 90% of cases). The transition of the disease to a chronic form occurs when contacting a qualified specialist is late, patients are of advanced age, if the period of anuria is more than 7 days (lack of urination), in the presence of complications, unfavorable working and living conditions, alcohol abuse, repeated hypothermia. Fatal outcome in acute glomerulonephritis is due to complications of the disease; currently it is extremely rare.
Is medical examination necessary?
Dispensary observation after discharge from the hospital should be carried out in the clinic at the place of residence by a urologist or nephrologist. Patients with acute glomerulonephritis in the complete absence of the triad of characteristic symptoms should be under active observation for three years.
Patients discharged with so-called residual manifestations undergo clinical follow-up for three years after the restoration of all urine parameters.
If pathological changes in the urine do not disappear within one and a half years, and the symptoms of the disease persist, it is generally accepted that acute glomerulonephritis has become chronic. Such patients are observed for many years in a dispensary with periodic inpatient treatment if there is an exacerbation of chronic glomerulonephritis or deterioration of kidney function.
Restrictions on severity are recommended for acute glomerulonephritis, heavy physical work, and hypothermia should not be allowed.
Vaccination is contraindicated for patients with allergic reactions.
More information about kidney disease is discussed in the video:
How to prevent the disease?
Basic preventive measures should be aimed at risk factors, their prevention and early detection. Therefore it is very important:
- Sanitation of foci of chronic infection of the upper respiratory tract: caries and its complications, pharyngitis, sinusitis, tonsillitis
- Prevention of acute respiratory diseases: hardening, prophylactic use of antiviral drugs, compliance with basic hygiene procedures
- Dispensary observation of patients with infectious diseases: tonsillitis, infective endocarditis, tuberculosis
- Caution when using antibiotics that have a destructive effect on kidney tissue
- Prevention of cancer, its early detection and radical treatment
- Prevention of allergic reactions
- Vaccination taking into account all indications and contraindications, only after consultation with a specialist doctor
- Observation by a physician of women who have suffered glomerulonephritis during pregnancy, especially in the first two months after childbirth.
Diagnosis of the disease Acute glomerulonephritis
The diagnosis of acute diffuse glomerulonephritis does not present great difficulties with a pronounced clinical picture, especially among young people. It is important that often the leading symptoms in the picture of the disease are symptoms of heart failure (shortness of breath, edema, cardiac asthma, etc.). To establish a diagnosis in these cases, it is essential that the acute development of the disease occurs in patients without previous heart pathology and that a pronounced urinary syndrome, especially hematuria, as well as a tendency to bradycardia are detected.
The differential diagnosis between acute glomerulonephritis and exacerbation of chronic glomerulonephritis is difficult What is important here is to clarify the period from the onset of the infectious disease to the acute manifestations of nephritis. In case of acute glomerulonephritis, this period is 1-3 weeks, and in case of exacerbation of the chronic process - only a few days (1-2 days). Urinary syndrome may be the same in severity, but a persistent decrease in the relative density of urine below 1.015 and a decrease in the filtration function of the kidneys are more typical for exacerbation of the chronic process. It is difficult to diagnose the latent form of acute gpomeruponephritis. The predominance of erythrocytes over leukocytes in the urine sediment, the absence of active and pale leukocytes (when stained according to Sternheimer-Malbin), and the absence of a history of dysuric phenomena help to distinguish it from chronic, latent pyelonephritis. Data from x-ray urological studies may be important for differential diagnosis with pyelonephritis, kidney stones, renal tuberculosis and other diseases occurring with small urinary syndrome.
Classification
In medical practice, several classifications of glomerulonephritis .
The first involves division according to the course of the pathology:
- Acute diffuse glomerulonephritis . It, in turn, has two forms:
- Cyclic. Acute diffuse glomerulonephritis of this form is characterized by a rapid course and is characterized by a clear clinical picture. However, even after effective treatment, the patient experiences rare bursts of hematuria and proteinuria.
- Latent. Acute diffuse glomerulonephritis is characterized by a weak clinical picture.
- Chronic glomerulonephritis . It can take one of the following forms:
- Nephritic. The main syndrome is nephritic, which is accompanied by symptoms of kidney inflammation.
- Hypertensive. The main syndrome is hypertensive.
- Mixed. It is characterized by the manifestation of symptoms characteristic of nephritic and hypertensive forms.
- Latent. It occurs mostly unnoticed by the patient. The clinical picture is characterized by mild disturbances of urinary function.
- Hematuric. Manifests itself in the form of hematuria (the presence of blood in the urine).
- Rapidly progressive glomerulonephritis.
In addition, in medicine it is customary to distinguish other forms of acute glomerulonephritis:
- Primary. It develops against the background of kidney destruction.
- Secondary. It is a consequence of an underlying pathology such as an infectious or viral lesion of the body, a malignant tumor, and so on.
Treatment of the disease Acute glomerulonephritis
Bed rest and diet are prescribed. A sharp restriction of table salt in food (no more than 1.5-2 g/day) in itself can lead to increased release of water and the elimination of edematous and hypertensive syndromes. At first, sugar days are prescribed (400-500 g of sugar per day with 500-600 ml of tea or fruit juice). In the future, watermelons, pumpkins, oranges, and potatoes are given, which provide almost completely sodium-free nutrition.
Long-term restriction of protein intake in acute glomerulonephritis is not sufficiently justified, since retention of nitrogenous wastes, as a rule, is not observed, and the sometimes supposed increase in blood pressure under the influence of protein nutrition has not been proven. Of the protein products, it is better to eat cottage cheese, as well as egg whites. Fats are allowed in the amount of 50-80 g/day. Carbohydrates are added to provide daily caloric intake. Liquids can be consumed up to 600-1000 ml/day. Antibacterial therapy is indicated when there is a clear connection between glomerulonephritis and an existing infection, for example, in prolonged septic endocarditis, chronic tonsillitis. For chronic tonsillitis, tonsillectomy is indicated 2-3 months after the acute effects of glomerulonephritis have subsided.
It is advisable to use steroid hormones - prednisolone (prednisone), triamcinolone (dexamethasone). Treatment with prednisolone is prescribed no earlier than 3-4 weeks from the onset of the disease, when general symptoms (in particular, arterial hypertension) are less pronounced. Corticosteroid hormones are especially indicated for the nephrotic form or prolonged course of acute glomerulonephritis, as well as for the so-called residual urinary syndrome, including hematuria. Prednisolone is used starting with a dose of 10-20 mg/day, quickly (within 7-10 days) the daily dose is increased to 60 mg. This dose is continued to be given for 2-3 weeks, then it is gradually reduced. The course of treatment lasts 5-6 weeks. The total amount of prednisolone per course is 1500-2000 mg. If during this time a sufficient therapeutic effect is not achieved, you can continue treatment with maintenance doses and prednisolone (10-15 mg/day) for a long time under medical supervision. Corticosteroid therapy affects both edema and urinary syndrome. It can promote recovery and prevent the transition of acute glomerulonephritis to chronic. Moderate arterial hypertension is not a contraindication to the use of corticosteroid drugs. If there is a tendency to increase blood pressure and increase edema, treatment with corticosteroid hormones should be combined with antihypertensive and diuretic drugs. If there are foci of infection in the body, then antibiotics must be prescribed simultaneously with corticosteroid hormones.
In the presence of arterial hypertension and especially in the occurrence of eclampsia, complex antihypertensive therapy with peripheral vasodilators (verapamil, hydralazine, sodium nitroprusside, diazoxide) or sympatholytics (reserpine, clonidine) in combination with saluretics (furosemide, ethacrynic acid) and tranquilizers (diazepam, etc.) is indicated. . Ganglioblockers and (3-adrenergic blockers) can be used. To reduce cerebral edema, osmotic diuretics (40% glucose solution, mannitol) are used. For convulsions (at stage 1), ether-oxygen anesthesia is given. For persistent convulsions, bloodletting is performed.
Forecast.
Full recovery may occur. Death in the acute period of the disease is rare. The transition of acute glomerulonephritis to a chronic disease is observed in approximately 1/3 of cases. Due to the use of corticosteroid hormones, the prognosis has now improved significantly. In the acute period, patients are unable to work and must be hospitalized. In a typical course, complete recovery may occur after 2-3 months: survivors of the disease can return to work even in the presence of moderate urinary syndrome or residual albuminuria. Persons who have suffered acute glomerulonephritis are subject to clinical observation, since clinical recovery can often be apparent. To avoid relapse of the disease, special attention should be paid to the fight against focal infection. Cooling work in humid environments should be avoided for a year.
Types of glomerulonephritis and stages of the disease
The classification of the disease in question is very extensive.
Based on the symptomatic picture, there are 3 types of glomerulonephritis:
- Spicy . Appears suddenly and progresses quickly. With timely treatment, complete recovery results. In some cases, it can develop into a chronic disease.
- Chronic . Exacerbations (spring/autumn) alternate with recoveries.
- Subacute . Responds poorly to treatment measures. Progresses quickly, and in 80% of cases leads to death.
All described types of illness can occur in various forms, each of which is characterized by a unique clinical picture. These forms were discussed in more detail in the previous section.
Depending on the etiological symptom, the disease in question is of two types:
- Primary . It develops as an independent pathology.
- Secondary . It occurs against the background of other pathologies that systemically affect the body.
Based on the nature of histological transformations in the kidneys, glomerulonephritis occurs:
- Mesangioproliferative . The functioning of the kidneys is impaired due to the narrowing of the lumen of the capillaries. This phenomenon is caused by the proliferation of connective tissue.
- Intracapillary . The filtration function undergoes negative changes because the vessels become too narrow: the inner layer of their walls thickens.
- Mesangiocapillary. It is a combination of the two types of glomerulonephritis listed above.
- Diffuse membranous nephropathy . The main provocateurs of degenerative conditions are immune complexes that accumulate on the walls of the capillaries of the glomeruli of the kidneys.
- Rapidly progressive . The pathology in this case is provoked by severe inflammatory phenomena. The disease develops quickly, leading to kidney failure.
There are several stages of glomerulonephritis:
- The initial stage is the acute course of the pathology. After 3 weeks, without adequate therapy, the disease becomes “chronic.”
- Stage of recovery (convalescence).
- Chronic form of the disease . This stage can last for decades, provided that the functional activity of the kidneys remains normal.
- The stage of decompensation is the development of exacerbations. It is characterized by the progression of the disease in question, which leads to serious malfunctions of the kidneys. Chronic renal failure occurs.