Kidney: structure, functions. Nephron – as a morphofunctional unit of the kidney, its structure. Functions
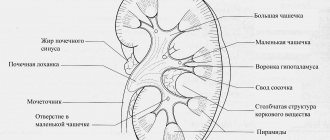
The kidney is a parenchymal zonal organ. On the outside, it is covered with a capsule of dense fibrous connective tissue and serous membrane. Layers of loose fibrous unformed connective tissue extend from the capsule, along which vessels run. The kidney consists of a cortex and medulla. The border between them is uneven: the cortex penetrates into the medulla in the form of columns of Bertini
, and the medulla in the form of the medullary
rays of Ferrein.
Cortex
occupies the outer, superficial part of the kidney and is divided into separate sections by Ferrein's medullary rays. Sections of the cortex with their lower part are embedded between the bases of the cerebral pyramids into the medulla in the form of Bertini columns, separating the pyramids from each other.
Brain matter
formed by brain pyramids. Their wide bases are turned towards the cortex, the apices of the pyramids are called papillae. They face the minor calyces, which then continue into the large calyces and then into the renal pelvis.
Kidney functions:
· urination and urination, consists of the formation of urine by filtering blood plasma and reabsorption back into the blood of metabolic products useful for the body. With the urine formed in the kidneys, the end products of nitrogen metabolism and xenobiotics are released: toxic, medicinal substances and others;
· maintaining acid-base homeostasis;
· regulation of water-salt metabolism;
regulation of blood pressure;
· endocrine function and synthesis of biologically active substances - production of renin, erythropoietin, erythrogenin, prostaglandins, biogenic amines, vitamin D3 (calcitrol), kallikrein, a number of interleukins;
· participation in metabolism, primarily in the metabolism of proteins and carbohydrates;
· participation in the work of the coagulation anticoagulant system, which consists in the production of urokinase (plasminogen activator, fibrinolysis factor), platelet activating factor.
The structural and functional unit of the kidney is the nephron.
It consists of a capsule and proximal convoluted and straight tubules passing into each other, distal convoluted and straight tubules. Each kidney has about 2 million nephrons.
In the nephron there are:
· capsule (together with the vascular glomerulus forms the renal Malpighi corpuscle);
· proximal convoluted section;
· proximal straight section;
· distal convoluted section;
· distal straight section.
The distal convoluted tubules empty into the collecting ducts, which originate in the medullary rays in the cortex, continue into the medulla, and at the top of the pyramids open into the papillary canals. The above sections of nephrons are located both in the medulla and in the cortex.
The cortex includes the following structures:
renal Malpighi corpuscles;
· proximal convoluted tubules;
· distal convoluted tubules.
The cortex also contains components of the juxtaglomerular apparatus
. The medulla contains: proximal straight tubules, thin tubules, distal straight tubules, and also the collecting ducts in the medulla. In cortical nephrons, the cortex contains the renal corpuscle, proximal and distal sections, and only the thin section and the ascending part of the loop lie in the medulla.
Histology of the oral cavity. Large salivary glands: development, structure, histophysiology. Features of the structure of protein, mucous and mixed end sections. Endocrine function, blood supply and innervation of the salivary glands. Age-related changes and regeneration of the salivary glands.
The organs of the oral cavity include lips, cheeks, gums, teeth, tongue, hard and soft palate, tonsils. The excretory ducts of the large salivary glands open into the oral cavity.
DEVELOPMENT. Salivary glands develop from 2 sources: ectoderm (end sections and excretory ducts) and mesenchyme (capsule, stroma and vessels). The type of end sections of the glands changes as they mature, and in the opposite way:
– in the parotid glands, the mucous sections are replaced by serous ones,
- and in the remaining two pairs of glands, serous ones - into mixed and mucous sections.
STROMA. The outside of the glands is covered with a dense connective tissue capsule. Layers extend from it, dividing the glands into lobules and containing interlobular ducts and blood vessels. The salivary glands are complex because... They have branched excretory ducts and terminal sections.
1. Types of end sections. Terminal sections (or acini)
in the glands under consideration
according to the nature
of their
exocrinocytes
, and therefore,
according to the nature of the secretion,
they are divided into three types.
a) Protein (serous)
the sections contain only
serocytes
(protein cells) that produce protein secretions.
b) Mucous (mucosal)
sections contain only
mucocytes
(mucous cells) that produce mucous secretion.
V)
And
the mixed
end sections contain both serocytes and mucocytes, which is why they produce a protein-mucus secretion.
2. The distribution of the terminal sections among the glands is as follows:
a) in the parotid glands
– there are only serous terminal sections;
b) in the submandibular glands
- serous and mixed sections;
c) in the sublingual glands -
all three types of sections: mixed, mucous and serous, with mixed sections predominating and containing seromucocytes (cells with intermediate properties).
All types of terminal sections contain, in addition to exocrinocytes, also myoepithelial cells. Their name is due to the fact that, on the one hand, they are of epithelial origin
, and on the other hand, have
contractility.
Due to contractile activity, myoepithelial cells
facilitate the release of secretions
from the terminal sections.
Salivary ducts
Types of ducts
a) Among the excretory ducts there are intralobular
- intercalated and striated,
interlobular
and
duct
(or ducts)
glands.
b) Moreover, intercalary ducts are present only in the case of serous terminal sections,
directly from which they begin. Then the intercalary ducts become striated.
Nephron functions
The nephron ensures the normal functioning of the entire body, performing a number of important functions:
- Cleanses the blood circulating through the vessels.
- Participates in the formation of primary and secondary type urine.
- Returns water, ions, amino acids.
- Regulates water, acid-base and salt balance in organs and systems.
- Ensures that blood pressure is maintained within normal values.
- Secretes a number of hormones.
In just 60 seconds, the nephrons of both kidneys purify approximately one liter of blood. And in five minutes the entire volume of blood circulating in the human body is filtered.
Nephron as a structural unit of the kidney
Each adult kidney contains at least 1 million nephrons, each of which is capable of producing urine. At the same time, usually about 1/3 of all nephrons function, which is enough to fully perform the excretory and other functions of the kidneys. This indicates the presence of significant functional reserves of the kidneys. With aging, there is a gradual decrease in the number of nephrons (by 1% per year after 40 years) due to their lack of ability to regenerate. For many people in their 80s, the number of nephrons is reduced by 40% compared to those in their 40s. However, the loss of such a large number of nephrons is not a threat to life, since the remaining part can fully perform excretory and other functions of the kidneys. At the same time, damage to more than 70% of the total number of nephrons in kidney diseases can cause the development of chronic renal failure.
Why do we need so many nephrons?
The nephron of the kidney is very small in size, but their number is large, this allows the kidneys to efficiently cope with their tasks even in difficult conditions. It is thanks to this feature that a person can live completely normally with the loss of one kidney.
Modern research shows that only 35% of units are directly involved in “business”, the rest are “resting”. Why does the body need such a reserve?
Firstly, an emergency situation may arise that will lead to the death of some units. Then their functions will be taken over by the remaining structures. This situation is possible in case of illness or injury.
Secondly, their loss happens to us all the time. With age, some of them die due to aging. Until the age of 40, nephron death does not occur in a person with healthy kidneys. Further, we lose about 1% of these structural units every year. They cannot regenerate; it turns out that by the age of 80, even with a favorable state of health, only about 60% of them function in the human body. These numbers are not critical, and allow the kidneys to cope with their functions, in some cases completely, in others there may be slight deviations. The threat of kidney failure awaits us when a loss of 75% or more occurs. The remaining amount is not enough to ensure normal blood filtration.
Such serious losses can be caused by alcoholism, acute and chronic infections, back or abdominal injuries that cause kidney damage.
general information
This is the name of one of the functional units of the kidney (one of its elements). There are at least 1 million nephrons in the organ, and together they form a coherently functioning system. Due to their structure, nephrons allow blood filtration.
Why blood, since it is common knowledge that the kidneys produce urine? They produce urine precisely from blood, where the organs, having selected from it everything they need, send substances:
- or are not required by the body at all at the moment;
- or their surplus;
- which can become dangerous for him if they continue to remain in the blood.
To balance the composition and properties of blood, it is necessary to remove unnecessary components from it: excess water and salts, toxins, low molecular weight proteins.
Loop of Henle
The structural and functional unit of the kidney consists of thin sections, also called the loop of Henle. It consists of 2 segments: descending thin and ascending thick. The wall of the descending section with a diameter of 15 μm is formed by squamous epithelium with multiple pinocytotic vesicles, and the wall of the ascending section is cubic. The functional significance of the nephron tubules of the loop of Henle includes the retrograde movement of water in the descending part of the knee and its passive return in the thin ascending segment, the reuptake of Na, Cl and K ions in the thick segment of the ascending bend. In the capillaries of the glomeruli of this segment, the molarity of urine increases.
Nephron structure
The discovery of the ultrasound method made it possible to find out that not only the heart has the ability to contract, but all organs: the liver, kidneys and even the brain.
The kidneys contract and relax in a certain rhythm - their size and volume either decrease or increase. In this case, there is either compression or stretching of the arteries passing through the depths of the organ. The level of pressure in them also changes: when the kidney relaxes, it decreases, when it contracts, it increases, making the nephron possible.
When the pressure in the artery increases, the system of natural semi-permeable membranes in the structure of the kidney is activated - and substances unnecessary for the body, being pressed through them, are removed from the bloodstream. They enter the formations that are the initial sections of the urinary tract.
In certain sections there are areas where reabsorption (return) of water and part of the salts into the bloodstream occurs.
In the nephron there are:
- primary filtration zone (renal corpuscle, consisting of the renal glomerulus located in the Shumlyansky-Bowman capsule);
- reabsorption zone (capillary network at the level of the initial sections of the primary urinary tract - renal tubules).
Renal glomerulus
This is the name of the network of capillaries that really looks like a loose ball, into which the afferent (another name: afferent) arteriole breaks down.
This structure ensures the maximum area of contact between the walls of the capillaries and the selectively permeable three-layer membrane intimately (very closely) adjacent to them, forming the inner wall of the Bowman capsule.
The thickness of the capillary walls is formed by only one layer of endothelial cells with a thin cytoplasmic layer, in which there are fenestrae (empty structures) that ensure the transport of substances in one direction - from the lumen of the capillary to the cavity of the capsule of the renal corpuscle.
Depending on the location in relation to the capillary glomerulus (glomerulus), they are:
- intraglomerular (intraglomerular);
- extraglomerular (extraglomerular).
Having passed through the capillary loops and freed them from toxins and excess, the blood is collected in the outlet artery. This, in turn, forms another network of capillaries that entwines the renal tubules in their convoluted sections, from which the blood collects in the drainage vein and thus returns to the bloodstream of the kidney.
Bowman-Shumlyansky capsule
The structure of this structure can be described by comparison with a well-known object in everyday life - a spherical syringe. If you press its bottom, it forms a bowl with an inner concave hemispherical surface, which is both an independent geometric shape and serves as a continuation of the outer hemisphere.
Between the two walls of the resulting form there remains a slit-like space-cavity, which continues into the nose of the syringe. Another example for comparison is a thermos flask with a narrow cavity between its two walls.
In the Bowman-Shumlyansky capsule there is also a slit-like internal cavity between its two walls:
- external, called the parietal plate and
- internal (or visceral plate).
Most of all, the podocyte resembles a stump with several thick main roots, from which thinner roots extend evenly on both sides, and the entire system of roots, spread over the surface, both extends far from the center and fills almost the entire space inside the circle formed by it. Main types:
- Podocytes are giant-sized cells with bodies located in the cavity of the capsule and at the same time raised above the level of the capillary wall due to the support of their root-like processes - cytotrabeculae.
- Cytotrabecula is the level of primary branching of the “leg”-process (in the example with a stump, the main roots). But there is also secondary branching – the level of cytopodia.
- Cytopodia (or pedicles) are secondary processes with a rhythmically maintained distance from the cytotrabecula (“main root”). Due to the uniformity of these distances, uniform distribution of cytopodia is achieved in areas of the capillary surface on both sides of the cytotrabecula.
The outgrowths-cytopodia of one cytotrabecula, entering the spaces between similar formations of the neighboring cell, form a figure whose relief and pattern is very reminiscent of a zipper, between the individual “teeth” of which there remain only narrow parallel slits of a linear shape, called filtration slits (slit diaphragms) .
Thanks to this structure of podocytes, the entire outer surface of the capillaries, facing the capsule cavity, is completely covered with intertwining cytopodia, whose zippers do not allow the capillary wall to be pushed into the capsule cavity, counteracting the force of blood pressure inside the capillary.
Renal glomerulus
The nephron begins with a capillary glomerulus. This is the body. The morphofunctional unit is a network of capillary loops, up to 20 in total, which surround the nephron capsule. The body receives blood supply from the afferent arteriole. The vascular wall is a layer of endothelial cells, between which there are microscopic spaces with a diameter of up to 100 nm.
The capsules contain inner and outer epithelial spheres. Between the two layers there remains a slit-like gap - the urinary space, where primary urine is contained. It envelops each vessel and forms a solid ball, thus separating the blood located in the capillaries from the spaces of the capsule. The basement membrane serves as a supporting base.
The nephron is designed like a filter, the pressure in which is not constant, it varies depending on the difference in the width of the lumens of the afferent and efferent vessels. Filtration of blood in the kidneys occurs in the glomerulus. The formed elements of blood, proteins, usually cannot pass through the pores of the capillaries, since their diameter is much larger and they are retained by the basement membrane.
Kidney tubules
Having begun with a flask-shaped thickening (the Shumlyansky-Bowman capsule in the structure of the nephron), the primary urinary tract then has the character of tubes of diameter that varies along their length, moreover, in some areas they acquire a characteristically convoluted shape.
Their length is such that some of their segments are located in the cortical, others in the medulla layer of the kidney parenchyma. On the way fluid from the blood to primary and secondary urine, it passes through the renal tubules, consisting of:
- proximal convoluted tubule;
- loop of Henle, which has descending and ascending limbs;
- distal convoluted tubule.
The same purpose is served by the presence of interdigitations - finger-like indentations of the membranes of neighboring cells into each other. Active resorption of substances into the lumen of the tubule is a very energy-intensive process, therefore the cytoplasm of the tubule cells contains many mitochondria.
The following is reabsorbed into the capillaries that wrap around the surface of the proximal convoluted tubule:
- sodium, potassium, chlorine, magnesium, calcium, hydrogen, carbonate ions;
- glucose;
- amino acids;
- some proteins;
- urea;
- water.
Classification
Based on the layer in which the nephron capsules are located, the following types are distinguished:
- Cortical - nephron capsules are located in the cortical ball; they contain small or medium-sized glomeruli with the corresponding length of bends. Their afferent arteriole is short and wide, and their efferent arteriole is narrower.
- Juxtamedullary nephrons are located in the medullary renal tissue. Their structure is presented in the form of large renal corpuscles, which have relatively longer tubules. The diameters of the afferent and efferent arterioles are the same. The main role is to concentrate urine.
- Subcapsular. Structures located directly under the capsule.
In general, in 1 minute both kidneys purify up to 1.2 thousand ml of blood, and in 5 minutes the entire volume of the human body is filtered. It is believed that nephrons, as functional units, are not capable of repair. The kidneys are a delicate and vulnerable organ, so factors that negatively affect their functioning lead to a decrease in the number of active nephrons and provoke the development of renal failure. Thanks to knowledge, the doctor is able to understand and identify the causes of changes in urine, as well as carry out corrections.
Types of nephrons
Since the renal corpuscles of most nephrons are located in the cortical layer of the kidney parenchyma (in the outer cortex), and their loops of Henle of short length pass in the outer renal medulla along with most of the blood vessels of the kidney, they are usually called cortical, or intracortical.
The rest of them (about 15%), with a loop of Henle of greater length, deeply immersed in the medulla (up to reaching the apices of the renal pyramids), is located in the juxtamedullary cortex - the border zone between the medulla and the cortical layer, which allows them to be called juxtamedullary.
Less than 1% of nephrons located shallowly in the subcapsular layer of the kidney are called subcapsular, or superficial.
What is a nephron?
The nephron, the structure and significance of which is very important for the human body, is a structural and functional unit inside the kidney. Inside this structural element, urine is formed, which subsequently leaves the body through appropriate pathways.
Biologists say that inside each kidney there are up to two million such nephrons, and each of them must be absolutely healthy so that the genitourinary system can fully perform its function. If the kidney is damaged, the nephrons cannot be restored; they will be excreted along with the newly formed urine.
Ultrafiltration of urine
The ability of the “legs” of podocytes to contract with simultaneous thickening makes it possible to further narrow the filtration gap, which makes the process of purifying the blood flowing through the capillary within the glomerulus even more selective in terms of the diameter of the molecules being filtered.
Thus, the presence of “legs” in podocytes increases the area of their contact with the capillary wall, while the degree of their contraction regulates the width of the filtration slits.
In addition to the role of a purely mechanical obstacle, slit diaphragms contain on their surfaces proteins that have a negative electrical charge, which also limits the passage of negatively charged protein molecules and other chemical compounds.
The structure of nephrons (regardless of their location in the kidney parenchyma), designed to perform the function of maintaining the stability of the internal environment of the body, allows them to perform their task, regardless of the time of day, the change of seasons and other external conditions, throughout a person’s life.
Collecting ducts
The collecting duct, also known as the ducts of Bellinium, is not part of the nephron, although it arises from it. The epithelium consists of light and dark cells. Light epithelial cells are responsible for the reabsorption of water and participate in the formation of prostaglandins. At the apical end, the light cell contains a single cilium, and in the folded dark ones, hydrochloric acid is formed, which changes the pH of the urine. The collecting ducts are located in the renal parenchyma. These elements are involved in the passive reabsorption of water. The function of the kidney tubules is to regulate the amount of fluid and sodium in the body, which affect blood pressure.
Types of nephrons in human kidneys
The structure of the human nephron varies depending on the type. There are juxtamedullary, intracortical and superficial. The main difference between them is their location inside the kidney, the depth of the tubules and the localization of the glomeruli, as well as the size of the glomeruli themselves. In addition, scientists attach importance to the characteristics of the loops and the duration of various segments of the nephron.
The superficial type is a connection created from short loops, and the juxtamedullary type is made from long ones. This diversity, according to scientists, appears as a result of the need of nephrons to reach all parts of the kidney, including the one located below the cortical substance.
Histophysiology of the nephron
The renal tubule system and glomeruli specialize in the process of urine formation, which occurs through the process of glomerular filtration, tubular reabsorption and secretion. Filtration is the first stage of urine formation, resulting in the formation of primary urine. This process occurs actively in the cortical nephrons and passively in the supocervical nephrons. Filtration of blood plasma occurs in the renal corpuscle, namely in the glomerulus, due to high blood pressure in the capillaries, which determines the possibility of passing a significant amount of liquid contents of the capillaries through the filtration slits of the renal filtrate into the lumen of the Shumlyansky-Boomer capsule of the renal corpuscle. The occurrence of high hemodynamic pressure in the capillaries of the glomerulus is due to the difference in the diameters of the afferent and efferent arterioles of the cortical nephrons. In the subcoloceral nephrons, the diameters of the afferent and efferent arterioles are almost the same, there is no high hemodynamic pressure, as a result of which the filtration process in the nephrons occurs passively. As a result of the filtration process, 190 liters of urine are produced per day.
Parts of a nephron
The nephron, the structure and significance of which for the body is well studied, directly depends on the tubule present in it. It is the latter that is responsible for constant functional work. All substances that are present inside the nephrons are responsible for the safety of certain types of renal tangles.
Inside the cortical substance one can find a large number of connecting elements, specific divisions of canals, and renal glomeruli. The functioning of the entire internal organ will depend on whether they are correctly placed inside the nephron and the kidney as a whole. First of all, this will affect the uniform distribution of urine, and only then its correct removal from the body.
The number of nephrons is limited
For normal life, approximately a third of the nephrons present in the kidneys are sufficient. The rest are reserve, in case of death of those functioning (as a result of injury or illness). The structural and functional unit of the kidney cannot recover, therefore, as a result of any damage, their number in the kidneys decreases. Over time, if such processes progress, renal failure may develop, negatively affecting the functioning of all organs and systems.
With the invention of means that help restore the filtering structures of the kidney, a lot of problems arising as a result of diseases affecting this organ will be solved. In the meantime, experts say, the only measure to prolong the functional viability of the kidneys is the prevention of diseases of the urinary system and timely comprehensive treatment of acute diseases, which does not allow them to become chronic.
Previous
AnatomyDNA definition, structure and structure of the molecule, functions and properties, formula and decoding, main characteristics of components, synthesis
Next
AnatomyHygienic treatment of hands of medical staff, algorithm according to sanpin, purpose, rules, types, levels and methods of hand treatment in medicine, duration of washing
Nephron anatomy
The anatomy and structure of the nephron is quite complex - each element plays a specific role. If even the smallest component malfunctions, the kidneys cease to function normally.
- capsule;
- glomerular structure;
- tubular structure;
- loops of Henle;
- collecting ducts.
The nephron in the kidney consists of segments communicating with each other. The Shumlyansky-Bowman capsule, a tangle of small vessels, are components of the renal body where the filtration process takes place. Next come the tubules, where substances are reabsorbed and produced.
The proximal portion begins from the renal corpuscle; Then the loops extend into the distal section. The nephrons, when unfolded, are individually about 40 mm long, and when folded together they are approximately 100,000 m long.
The nephron capsules are located in the cortex, are included in the medulla, then again in the cortex, and finally into the collecting structures that exit into the renal pelvis, where the ureters begin. Secondary urine is removed through them.
Capsule
The nephron originates from the Malpighian body. It consists of a capsule and a tangle of capillaries. The cells around the small capillaries are arranged in the shape of a cap - this is the renal corpuscle, which allows retained plasma to pass through. Podocytes cover the wall of the capsule from the inside, which, together with the outside, forms a slit-like cavity with a diameter of 100 nm.
Fenestrated (fenestrated) capillaries (components of the glomerulus) are supplied with blood from afferent arteries. They are otherwise called “magic mesh” because they do not play any role in gas exchange. The blood passing through this mesh does not change its gas composition. Plasma and dissolved substances enter the capsule under the influence of blood pressure.
The nephron capsule accumulates an infiltrate containing harmful products of blood plasma purification - this is how primary urine is formed. The slit-like gap between the layers of the epithelium acts as a filter operating under pressure.
Thanks to the afferent and efferent glomerular arterioles, the pressure changes. The basement membrane plays the role of an additional filter - it retains some blood elements. The diameter of the protein molecules is larger than the pores of the membrane, so they do not pass through.
Unfiltered blood enters the efferent arterioles, which pass into a network of capillaries that envelops the tubules. Subsequently, substances enter the blood and are reabsorbed in these tubules.
The nephron capsule of the human kidney communicates with the tubule. The next section is called proximal; primary urine then passes there.
Mixed Lot
Proximal tubules can be straight or curved. The surface inside is lined with cylindrical and cubic epithelium. The brush border with villi is the absorptive layer of the nephron tubules. Selective capture is ensured by the large area of the proximal tubules, the close dislocation of peritubular vessels and a large number of mitochondria.
Fluid circulates between cells. Plasma components in the form of biological substances are filtered. The convoluted tubules of the nephron produce erythropoietin and calcitriol. Harmful inclusions that enter the filtrate using reverse osmosis are removed with urine.
Nephron segments filter creatinine. The amount of this protein in the blood is an important indicator of the functional activity of the kidneys.
Loops of Henle
The loop of Henle involves part of the proximal and part of the distal section. At first, the diameter of the loop does not change, then it narrows and allows Na ions to pass out into the extracellular space. By creating osmosis, H2O is absorbed under pressure.
The descending and ascending ducts are the components of the loop. The descending region, 15 µm in diameter, consists of epithelium where multiple pinocytotic vesicles are located. The ascending portion is lined with cubic epithelium.
The loops are distributed between the cortex and medulla. In this area, water moves to a downward section, then returns.
At the beginning, the distal canal touches the capillary network at the site of the afferent and efferent vessels. It is quite narrow and is lined with smooth epithelium, and on the outside there is a smooth basement membrane. Ammonia and hydrogen are released here.
Collecting ducts
The collecting ducts are also called “ducts of Belline”. Their internal lining consists of light and dark epithelial cells. The former reabsorb water and are directly involved in the production of prostaglandins. Hydrochloric acid is produced in the dark cells of the folded epithelium and has the ability to change the pH of urine.
The collecting ducts and collecting ducts do not belong to the nephron structure, as they are located slightly lower, in the renal parenchyma. Passive reabsorption of water occurs in these structural elements. Depending on the functionality of the kidneys, the amount of water and sodium ions in the body is regulated, which, in turn, affects blood pressure.
Content
- 1 Structure and functions of the nephron 1.1 Renal corpuscle
- 1.2 Types of nephrons 1.2.1 Glomerulus
- 1.2.2 Nephron capsule
- 1.3.1 Proximal tubule 1.3.1.1 Structure of the proximal tubule
- 1.3.3.1 Transport processes
- 1.3.4.1 Transport processes
- 1.3.5.1 Transport processes
Functional disorders in the activity of nephrons
If malfunctions occur in the functioning of the nephrons, this affects the activity of all organs and systems. Among the disorders that arise due to nephron dysfunction, the following disorders can be mentioned:
- water and salt balance;
- acidity;
- metabolism.
All diseases that develop against the background of impaired transport activity of nephrons are usually called tubulopathies. Among them the following varieties are distinguished:
- Primary tubulopathy occurs against the background of congenital nephron dysfunction.
- Secondary forms of the disease arise due to acquired disorders of the transporting activity of the organ.
Common causes of secondary tubulopathy are damage to the nephron due to toxic damage to the body, malignant neoplasms or heavy metal poisoning. According to the location, all tubulopathies are divided into distal and proximal, depending on which tubules are affected (distal or proximal).
How is a nephron structured?
The structure of the renal nephron is very complex; biologists around the world are still struggling with attempts to recreate it in the form of an artificial formation suitable for transplantation. The loop appears primarily from the rising part, but may also include a delicate part. Once the loop is in the place where the ball is placed, it fits into a curved small channel.
The cells of the resulting formation lack a fuzzy edge, but a large number of mitochondria can be found here. The total membrane area can be increased due to the numerous folds that form as a result of looping within a single nephron.
The structure of the human nephron is quite complex, since it requires not only careful drawing, but also a thorough knowledge of the subject. It will be quite difficult for a person far from biology to depict it. The last section of the nephron is a shortened communication channel that opens into a storage tube.
The channel is formed in the cortical part of the kidney, with the help of storage tubes it passes through the “brain” of the cell. On average, the diameter of each membrane is about 0.2 millimeters, but the maximum length of the nephron canal, recorded by scientists, is about 5 centimeters.
Kidney structure. Functions and structure of the nephron What does the nephron capsule do?
The nephron is not only the main structural but also the functional unit of the kidney. This is where the most important stages take place. Therefore, information about what the structure of the nephron looks like and what exact functions it performs will be very interesting. In addition, the peculiarities of nephron functioning can clarify the nuances of the renal system.
Structure of the nephron: renal corpuscle
Interestingly, the mature kidney of a healthy person contains between 1 and 1.3 billion nephrons. A nephron is a functional and structural unit of the kidney, which consists of the renal corpuscle and the so-called loop of Henle.
The renal corpuscle itself consists of the Malpighian glomerulus and the Bowman-Shumlyansky capsule. To begin with, it is worth noting that the glomerulus is actually a collection of small capillaries. The blood enters here through the afferent artery - this is where the plasma is filtered. The remainder of the blood is removed by the efferent arteriole.
The Bowman-Shumlyansky capsule consists of two layers - internal and external. And if the outer sheet is an ordinary fabric, then the structure of the inner sheet deserves more attention. The inside of the capsule is covered with podocytes - these are cells that act as an additional filter. They allow glucose, amino acids and other substances to pass through, but prevent the movement of large protein molecules. Thus, primary urine is formed in the renal corpuscle, which differs from it only in the absence of large molecules.
Nephron: structure of the proximal tubule and loop of Henle
The proximal tubule is a formation that connects the renal corpuscle and the loop of Henle. Inside the tubule has villi, which increase the total area of the internal lumen, thereby increasing reabsorption rates.
The proximal tubule smoothly passes into the descending part of the loop of Henle, which is characterized by a small diameter. The loop descends into the medulla, where it bends around its own axis by 180 degrees and rises upward - here begins the ascending part of the loop of Henle, which has a much larger size and, accordingly, diameter. The ascending loop rises to approximately the level of the glomerulus.
Structure of the nephron: distal tubules
The ascending part of the loop of Henle in the cortex passes into the so-called distal convoluted tubule. It comes into contact with the glomerulus and contacts the afferent and efferent arterioles. This is where the final absorption of nutrients occurs. The distal tubule passes into the terminal part of the nephron, which in turn flows into the collecting duct, which carries fluid into the nephron.
Nephron classification
Depending on their location, it is customary to distinguish three main types of nephrons:
- Cortical nephrons make up approximately 85% of the number of all structural units in the kidney. As a rule, they are located in the outer cortex of the kidney, as their name suggests. The structure of this type of nephron is slightly different - the loop of Henle is small;
- juxtamedullary nephrons - such structures are located just between the medulla and cortex, have long loops of Henle that penetrate deeply into the medulla, sometimes even reaching the pyramids;
- subcapsular nephrons are structures that are located directly under the capsule.
It can be noted that the structure of the nephron is fully consistent with its functions.
Nephron
- This is the functional unit of the kidney in which blood filtration and urine production occur. It consists of a glomerulus, where blood is filtered, and convoluted tubules, where urine formation is completed. The renal corpuscle consists of a renal glomerulus, in which blood vessels are intertwined, surrounded by a funnel-shaped double membrane - this renal glomerulus is called Bowman's capsule - it continues with the renal tubule.
The glomerulus contains branches of vessels coming from the afferent artery, which carries blood to the renal corpuscles. Then these branches unite, forming the efferent arteriole, in which already purified blood flows. Between the two layers of Bowman's capsule surrounding the glomerulus, there remains a small lumen - the urinary space, which contains primary urine. A continuation of Bowman's capsule is the renal tubule - a duct consisting of segments of various shapes and sizes, surrounded by blood vessels, in which primary urine is cleansed and secondary urine is formed.
So, based on the above, we will try to more accurately describe the nephron of the kidney
according to the pictures located below to the right of the text.
Rice. 1. Nephron is the main functional unit of the kidney, in which the following parts are distinguished:
renal corpuscle
, represented by the glomerulus (K), surrounded by Bowman's capsule (BC);
renal tubule
, consisting of a proximal (PC) tubule (gray), a thin segment (TS) and a distal tubule (DC) (white).
The proximal tubule is divided into the proximal convoluted (PIC) and proximal straight tubule (NIT). In the cortex, the proximal tubules form tightly grouped loops around the renal corpuscles and then penetrate the medullary rays and continue into the medulla. In its depth, the proximal medullary tubule narrows sharply, and the thin segment (TS) of the renal tubule begins from this point. The thin segment descends deeper into the medulla, with different segments penetrating to varying depths, then turns to form a hairpin loop and returns to the cortex, abruptly becoming the distal straight tubule (DTC). From the medulla, this tubule passes through the medullary ray, then leaves it and enters the cortical labyrinth in the form of the distal convoluted tubule (DCT), where it forms loosely grouped loops around the renal corpuscle: in this area the epithelium of the tubule is transformed into the so-called macula densa (see . arrowhead) juxtaglomerular apparatus.
The proximal and distal straight tubules and thin segment form a very characteristic structure
of the kidney nephron
-
the loop of Henle
.
It consists of a thick descending portion (i.e., the proximal straight tubule), a thin descending portion (i.e., the descending portion of the thin segment), a thin ascending portion (i.e., the ascending portion of the thin segment), and a thick ascending portion. The loops of Henle
penetrate to varying depths into the medulla, which determines the division of nephrons into cortical and juxtamedullary.
There are about 1 million nephrons in the kidney. If you pull out a kidney nephron
in length, it will be equal to 2-3 cm depending on the length of
the loop of Henle
.
Short connecting portions (SU) connect the distal tubules to the straight collecting ducts (not shown here).
The afferent arteriole (ArA) enters the renal corpuscle and divides into glomerular capillaries, which together form the glomerulus, glomerulus. The capillaries then unite to form the efferent arteriole (EnA), which then divides into the peritubular capillary network (TCR), which surrounds the convoluted tubules and continues into the medulla, supplying it with blood. Rice. 2. The epithelium of the proximal tubule is single-layer cubic, consisting of cells with a centrally located round nucleus and a brush border (BB) at their apical pole.
Rice. 3. The epithelium of the thin segment (TS) is formed by a single layer of very flat epithelial cells with a nucleus protruding into the lumen of the tubule.
Rice. 4. The distal tubule is also lined with a single-layer epithelium formed by cubic light cells lacking a brush border. The internal diameter of the distal tubule is nevertheless larger than that of the proximal tubule. All tubules are surrounded by a basal membrane (BM).
At the end of the article, I would like to note that there are two types of nephrons, more about this in the article “
Each adult kidney contains at least 1 million nephrons, each of which is capable of producing urine. At the same time, usually about 1/3 of all nephrons function, which is enough for the full performance of excretory and other functions. This indicates the presence of significant functional reserves of the kidneys. With aging, there is a gradual decrease in the number of nephrons
(by 1% per year after 40 years) due to their lack of regeneration ability. For many people in their 80s, the number of nephrons is reduced by 40% compared to those in their 40s. However, the loss of such a large number of nephrons is not a threat to life, since the remaining part can fully perform excretory and other functions of the kidneys. At the same time, damage to more than 70% of the total number of nephrons in kidney diseases can cause the development of chronic renal failure.
Each nephron
consists of a renal (Malpighian) corpuscle, in which ultrafiltration of blood plasma and the formation of primary urine occurs, and a system of tubules and tubes in which primary urine is converted into secondary and final (released into the pelvis and into the environment) urine.
Rice. 1. Structural and functional organization of the nephron
The composition of urine during its movement through the pelvis (calyces, cups), ureters, temporary retention in the bladder and through the urinary canal does not change significantly. Thus, in a healthy person, the composition of the final urine released during urination is very close to the composition of urine released into the lumen (small calyces of the large calyces) of the pelvis.
Renal corpuscle
is located in the cortical layer of the kidneys, is the initial part of the nephron and is formed
by a capillary glomerulus
(consisting of 30-50 interwoven capillary loops) and
the Shumlyansky-Boumeia capsule.
In cross-section, the Shumlyansky-Boumeia capsule looks like a cup, inside of which there is a glomerulus of blood capillaries.
The epithelial cells of the inner layer of the capsule (podocytes) are tightly adjacent to the wall of the glomerular capillaries. The outer leaf of the capsule is located at some distance from the inner one. As a result, a slit-like space is formed between them - the cavity of the Shumlyansky-Bowman capsule, into which blood plasma is filtered, and its filtrate forms primary urine. From the capsule cavity, primary urine passes into the lumen of the nephron tubules: the proximal tubule
(convoluted and straight segments),
the loop of Henle
(descending and ascending sections) and
the distal tubule
(straight and convoluted segments).
An important structural and functional element of the nephron is the juxtaglomerular apparatus (complex) of the kidney.
It is located in a triangular space formed by the walls of the afferent and efferent arterioles and the distal tubule (
macula densa ),
tightly adjacent to them. Cells of the macula densa have chemo- and mechanosensitivity, regulating the activity of juxtaglomerular cells of arterioles, which synthesize a number of biologically active substances (renin, erythropoietin, etc.). The convoluted segments of the proximal and distal tubules are located in the renal cortex, and the loop of Henle is in the medulla.
From the convoluted distal tubule, urine enters the communicating tubule
, from it into
the collecting duct
and
collecting duct
of the renal cortex;
8-10 collecting ducts unite into one large duct ( cortical collecting duct
), which, descending into the medulla, becomes
the renal medullary collecting duct.
Gradually merging, these ducts form
a large-diameter duct
, which opens at the top of the papilla of the pyramid into the small calyx of the large calyx of the pelvis.
Each kidney has at least 250 large-diameter collecting ducts, each of which collects urine from approximately 4,000 nephrons. The collecting ducts and collecting ducts have special mechanisms for maintaining hyperosmolarity of the renal medulla, concentrating and diluting urine, and are important structural components of the formation of final urine.
Nephron structure
Each nephron begins with a double-walled capsule, inside of which there is a vascular glomerulus. The capsule itself consists of two leaves, between which there is a cavity that passes into the lumen of the proximal tubule. It consists of the proximal convoluted tubule and the proximal straight tubule, constituting the proximal segment of the nephron. A characteristic feature of the cells of this segment is the presence of a brush border, consisting of microvilli, which are outgrowths of the cytoplasm surrounded by a membrane. The next section is the loop of Henle, consisting of a thin descending part that can descend deeply into the medulla, where it forms a loop and turns 180° towards the cortex in the form of an ascending thin, turning into a thick part of the nephron loop. The ascending limb of the loop rises to the level of its glomerulus, where the distal convoluted tubule begins, which becomes a short communicating tubule connecting the nephron with the collecting ducts. The collecting ducts begin in the renal cortex, merging to form larger excretory ducts that pass through the medulla and empty into the cavity of the renal calyx, which in turn drain into the renal pelvis. According to localization, several types of nephrons are distinguished: superficial (superficial), intracortical (inside the cortical layer), juxtamedullary (their glomeruli are located on the border of the cortical and medulla layers).
Rice. 2. Structure of the nephron:
A - juxtamedullary nephron; B - intracortical nephron; 1 - renal corpuscle, including the capsule of the glomerulus of capillaries; 2 - proximal convoluted tubule; 3 - proximal straight tubule; 4 - descending thin limb of the nephron loop; 5 - ascending thin limb of the nephron loop; 6 - distal straight tubule (thick ascending limb of the nephron loop); 7 - dense spot of the distal tubule; 8 - distal convoluted tubule; 9 - connecting tubule; 10 - collecting duct of the renal cortex; 11 - collecting duct of the outer medulla; 12 - collecting duct of the internal medulla
Different types of nephrons differ not only in location, but also in the size of the glomeruli, the depth of their location, as well as in the length of individual sections of the nephron, especially the loop of Henle, and in their participation in the osmotic concentration of urine. Under normal conditions, about 1/4 of the volume of blood ejected by the heart passes through the kidneys. In the cortex, blood flow reaches 4-5 ml/min per 1 g of tissue, therefore, this is the highest level of organ blood flow. A feature of renal blood flow is that the blood flow of the kidney remains constant when systemic blood pressure changes within a fairly wide range. This is ensured by special mechanisms of self-regulation of blood circulation in the kidney. Short renal arteries arise from the aorta; in the kidney they branch into smaller vessels. The renal glomerulus includes the afferent (afferent) arteriole, which breaks up into capillaries. When capillaries merge, they form an efferent arteriole, through which blood flows out from the glomerulus. After leaving the glomerulus, the efferent arteriole again breaks up into capillaries, forming a network around the proximal and distal convoluted tubules. A feature of the juxtamedullary nephron is that the efferent arteriole does not break up into a peritubular capillary network, but forms straight vessels that descend into the renal medulla.
Types of Nephrons
Types of nephrons
Based on their structural features and functions, there are two main types of nephrons:
: cortical (70-80%) and juxtamedullary (20-30%).
Cortical nephrons
are divided into superficial, or superficial, cortical nephrons, in which the renal corpuscles are located in the outer part of the renal cortex, and intracortical cortical nephrons, in which the renal corpuscles are located in the middle part of the renal cortex. Cortical nephrons have a short loop of Henle that extends only into the outer medulla. The main function of these nephrons is the formation of primary urine.
Renal corpuscles of juxtamedullary nephrons
are located in the deep layers of the cortex at the border with the medulla. They have a long loop of Henle that penetrates deep into the medulla, right up to the apexes of the pyramids. The main purpose of juxtamedullary nephrons is to create high osmotic pressure in the renal medulla, which is necessary to concentrate and reduce the volume of final urine.
Effective filtration pressure
- EFD = P cap - P bk - P onk.
- P cap
- hydrostatic pressure in the capillary (50-70 mm Hg); - P 6k
- hydrostatic pressure in the lumen of the Bowman-Shumlyaneki capsule (15-20 mm Hg); - Ronk
- oncotic pressure in the capillary (25-30 mm Hg).
EPD = 70 - 30 - 20 = 20 mm Hg. Art.
The formation of final urine is the result of three main processes occurring in the nephron: and secretion.
Kidneys
located in the retroperitoneal space of the lumbar region. The outside of the kidney is covered with a connective tissue capsule. The kidney consists of a cortex and medulla. The boundary between these parts is uneven, since the structural components of the cortex protrude into the medulla in the form of columns, and the medulla penetrates into the cortex, forming medullary rays.
The main structural and functional unit of the kidney
is the nephron.
The nephron is an epithelial tube that begins blindly in the form of a capsule of the renal corpuscle, then passes into tubules of different calibers, flowing into the collecting duct. Each kidney has about 1-2 million nephrons. The length of the nephron tubules is 2-5 cm, and the total length of all tubules in both kidneys reaches 100 km. The nephron
is divided into the capsule of the glomerulus of the renal corpuscle, the proximal, thin and distal sections.
Renal corpuscle
consists of a glomerular capillary network and an epithelial capsule. The capsule has outer and inner walls (leaves). The latter, together with the endothelial cells of the glomerular capillary network, forms the hematonephridial histion. The glomerulus of the capillary network is located between the afferent and efferent arterioles. The afferent arteriole often gives four branches, which break up into 50-100 capillaries. There are numerous anastomoses between them. The endothelium of the capillaries of the glomerular reticulum consists of flat endothelial cells with numerous fenestrae in the cytoplasm measuring about 0.1 μm. Fenestrated (fenestrated) endotheliocytes represent a kind of sieve. Outside the endothelial cells there is a basement membrane common to the endothelium and epithelium of the inner wall of the capsule, about 300 nm thick. It is characterized by a three-layer structure.
Epithelium of the inner wall
The capsule covers the capillaries of the glomerular network on all sides. It consists of a single layer of cells called podocytes. Podocytes have a slightly elongated irregular shape. The podocyte body has 2-3 large long processes called cytotrabeculae. From them, in turn, many small processes extend - cytopodia.
Cytopodia
They are narrow cylindrical structures (legs) with thickenings at the end, through which they are attached to the basement membrane. Between them there are slit-like spaces measuring 30-50 nm. These gaps have a certain significance in the filtration processes during the formation of primary urine. Between the capillary loops of the glomerular reticulum there is a type of connective tissue (mesangium) containing fibrous structures and mesangiocytes.
Outer wall epithelium
The glomerular capsule consists of a single layer of squamous epithelial cells. Between the outer and inner walls of the capsule there is a cavity into which primary urine, formed as a result of glomerular filtration, enters.
Filtration process
is the first stage of urine formation. Almost all components of blood plasma are filtered, with the exception of high molecular weight proteins and blood cells. Fluid from the lumen of the capillary passes through fenestrated endotheliocytes, the basalgum membrane and between the cytopodia of podocytes with their numerous filtration slits covered by diaphragms into the cavity of the glomerular capsule. Hematonephridial histone is permeable to glucose, urea, uric acid, creatinine, chlorides and low molecular weight proteins. These substances are part of the ultrafiltrate - primary urine. Of great importance for effective filtration is the difference in diameters of the afferent and efferent glomerular arterioles, which creates high filtration pressure (70-80 mm Hg), as well as a large number of capillaries (about 50-60) in the glomerulus. In an adult body, about 150-170 liters of primary filtrate (urine) are formed during the day.
So effective plasma filtration
, carried out by the kidneys almost continuously, contributes to the maximum removal of harmful metabolic products from the body - toxins. The next stage of urine formation is the reabsorption (reabsorption) of compounds necessary for the body (proteins, glucose, electrolytes, water) from the primary filtrate with the formation of final urine. The reabsorption process occurs in the nephron tubules.
In the proximal nephron
There are convoluted and straight parts of the tubule. This is the longest section of the tubules (about 14 mm). The diameter of the proximal convoluted tubule is 50-60 µm. Here, obligate reabsorption of organic compounds occurs according to the type of receptor-mediated endocytosis with the participation of mitochondrial energy. The wall of the proximal tubule consists of a single layer of cubic microvillous epithelium. On the apical surface of epithelial cells there are numerous microvilli 1-3 μm long (brush border). The number of microvilli on the surface of one cell reaches 6500, which increases the active absorption surface of each cell by 40 times. In the plasmalemma of epithelial cells between the microvilli there are depressions with adsorbed protein macromolecules, from which transport vesicles are formed.
Total surface
microvilli in all nephrons is 40-50 m2. The second characteristic feature of the structure of epithelial cells of the proximal tubule is the basal striation of epithelial cells, formed by deep folds of the plasmalemma and the regular arrangement of numerous mitochondria between them (basal labyrinth). The plasma membrane of the epithelial cells of the basal labyrinth has the property of transporting sodium from primary urine into the intercellular space.
The structural and functional unit of the kidney is the nephron, consisting of the vascular glomerulus, its capsule (renal corpuscle) and a system of tubules leading to the collecting ducts (Fig. 3). The latter morphologically do not belong to the nephron.
Figure 3. Diagram of the structure of the nephron (8).
Each human kidney has about 1 million nephrons; with age, their number gradually decreases. The glomeruli are located in the cortical layer of the kidney, 1/10-1/15 of them are located on the border with the medulla and are called juxtamedullary. They have long loops of Henle that extend into the medulla and help concentrate primary urine more efficiently. In infants, the glomeruli have a small diameter and their total filtering surface is much smaller than in adults.
The structure of the renal glomerulus
The glomerulus is covered with visceral epithelium (podocytes), which at the vascular pole of the glomerulus passes into the parietal epithelium of Bowman's capsule. Bowman's (urinary) space directly passes into the lumen of the proximal convoluted tubule. Blood enters the vascular pole of the glomerulus through the afferent (afferent) arteriole and, after passing through the capillary loops of the glomerulus, leaves it through the efferent (efferent) arteriole, which has a smaller lumen. Compression of the efferent arteriole increases hydrostatic pressure in the glomerulus, which promotes filtration. Within the glomerulus, the afferent arteriole is divided into several branches, which in turn give rise to the capillaries of several lobules (Fig. 4A). The glomerulus has about 50 capillary loops, between which anastomoses have been found that allow the glomerulus to function as a “dialysis system.” The glomerular capillary wall is a triple filter, including fenestrated endothelium, glomerular basement membrane, and slit diaphragms between the podocyte stalks (Fig. 4B).
Figure 4. Structure of the glomerulus (9).
A – glomerulus, AA – afferent arteriole (electron microscopy).
B – diagram of the structure of the capillary loop of the glomerulus.
The passage of molecules through the filtration barrier depends on their size and electrical charge. Substances with a molecular weight >50,000 Yes are almost not filtered. Due to the negative charge in normal glomerular barrier structures, anions are retained to a greater extent than cations. Endothelial cells
have pores or fenestrae with a diameter of about 70 nm.
The pores are surrounded by glycoproteins that have a negative charge; they represent a kind of sieve through which ultrafiltration of plasma occurs, but the formed elements of the blood are retained. The glomerular basement membrane
(GBM) represents a continuous barrier between the blood and the capsule cavity, and in an adult it has a thickness of 300-390 nm (in children it is thinner - 150-250 nm) (Fig. 5). GBM also contains a large number of negatively charged glycoproteins. It consists of three layers: a) lamina rara externa; b) lamina densa and c) lamina rara interna. An important structural part of the GBM is type IV collagen. In children with hereditary nephritis, clinically manifested by hematuria, type IV collagen mutations are detected. The pathology of GBM is established by electron microscopic examination of a kidney biopsy.
Figure 5. The glomerular capillary wall is the glomerular filter (9).
Below is the fenestrated endothelium, above it is the GBM, on which regularly spaced podocyte stalks are clearly visible (electron microscopy).
Visceral epithelial cells of the glomerulus
, podocytes, maintain the architecture of the glomerulus, prevent the passage of protein into the urinary space, and also synthesize GBM. These are highly specialized cells of mesenchymal origin. Long primary processes (trabeculae) extend from the podocyte body, the ends of which have “legs” attached to the GBM. Small processes (pedicles) extend from the large ones almost perpendicularly and cover the space of the capillary free from the large processes (Fig. 6A). A filtration membrane, the slit diaphragm, is stretched between adjacent podocyte stalks, which has been the subject of numerous studies in recent decades (Fig. 6B).
Figure 6. Structure of a podocyte (9).
A – podocyte feet completely cover the GBM (electron microscopy).
B – diagram of the filtration barrier.
Slit diaphragms consist of the nephrin protein, which is closely related in structural and functional relationships to many other protein molecules: podocin, CD2AR, alpha-actinin-4, etc. Mutations of the genes encoding podocyte proteins have now been identified. For example, a defect in the NPHS1 gene leads to the absence of nephrin, which occurs in congenital nephrotic syndrome of the Finnish type. Damage to podocytes due to exposure to viral infections, toxins, immunological factors, and genetic mutations can lead to proteinuria and the development of nephrotic syndrome, the morphological equivalent of which, regardless of the cause, is the melting of the podocyte feet. The most common type of nephrotic syndrome in children is idiopathic minimal change nephrotic syndrome.
The glomerulus also includes mesangial cells, the main function of which is to provide mechanical fixation of capillary loops. Mesangial cells have contractility, influencing glomerular blood flow, as well as phagocytic activity (Fig. 4B).
Kidney tubules
Primary urine enters the proximal renal tubules and undergoes qualitative and quantitative changes there due to the secretion and reabsorption of substances. Proximal tubules
- the longest segment of the nephron, at the beginning it is strongly curved, and when passing into the loop of Henle it straightens.
The cells of the proximal tubule (a continuation of the parietal epithelium of the glomerular capsule) are cylindrical in shape, covered with microvilli (“brush border”) on the lumen side. Microvilli increase the working surface of epithelial cells, which have high enzymatic activity. They contain many mitochondria, ribosomes and lysosomes. Active reabsorption of many substances (glucose, amino acids, sodium ions, potassium, calcium and phosphates) occurs here. Approximately 180 L of glomerular ultrafiltrate enters the proximal tubules, and 65-80% of water and sodium are reabsorbed. Thus, as a result of this, the volume of primary urine is significantly reduced without changing its concentration. Loop of Henle.
The straight part of the proximal tubule passes into the descending limb of the loop of Henle.
The shape of epithelial cells becomes less elongated, and the number of microvilli decreases. The ascending section of the loop has a thin and thick part and ends in a dense spot. The cells of the walls of the thick segments of the loop of Henle are large and contain many mitochondria, which generate energy for the active transport of sodium and chlorine ions. The main ion transporter of these cells, NKCC2, is inhibited by furosemide. The juxtaglomerular apparatus (JGA)
includes 3 types of cells: cells of the distal tubular epithelium on the side adjacent to the glomerulus (macula densa), extraglomerular mesangial cells and granular cells in the walls of afferent arterioles that produce renin. (Fig. 7).
Distal tubule.
Behind the dense spot (macula densa), the distal tubule begins, which passes into the collecting duct.
About 5% Na of primary urine is absorbed in the distal tubules. The transporter is inhibited by diuretics from the thiazide group. The collecting ducts
have three sections: cortical, external and internal medullary. The internal medullary portions of the collecting duct empty into the papillary duct, which opens into the minor calyx. The collecting ducts contain two types of cells: main ("light") and intercalary ("dark"). As the cortical part of the tube transitions to the medullary part, the number of intercalary cells decreases. The main cells contain sodium channels, the work of which is inhibited by the diuretics amiloride and triamterene. Intercalary cells do not have Na + /K + -ATPase, but contain H + -ATPase. They carry out the secretion of H + and the reabsorption of Cl -. Thus, the final stage of NaCl reabsorption occurs in the collecting ducts before urine exits the kidneys.
Interstitial cells of the kidneys.
In the renal cortex, the interstitium is weakly expressed, while in the medulla it is more noticeable. The renal cortex contains two types of interstitial cells - phagocytic and fibroblast-like. Fibroblast-like interstitial cells produce erythropoietin. There are three types of cells in the kidney medulla. The cytoplasm of one of these types of cells contains small lipid cells that serve as the starting material for the synthesis of prostaglandins.
Nephron: its structure, functional significance
The nephron is a shell for a small ball, which consists of two walls and covers a small ball of capillaries. The inside of this shell is covered with epithelium, the special cells of which help provide additional protection. The space that is formed between the two layers can be transformed into a small hole and channel.
This channel has a brush edge of small hairs, immediately behind it begins a very narrow section of the shell loop, which goes down. The wall of the area consists of flat and small epithelial cells. In some cases, the loop compartment reaches the depth of the medulla, and then unfolds towards the cortex of the renal formations, which smoothly develop into another segment of the nephron loop.
Podocytes in a nephron
The processes of podocytes are separated from each other by shield membranes, on which the nephron itself, the structure of the structural element of the kidney and its performance depend. Thanks to them, the sizes of substances that need to be filtered are determined. Epithelial cells have small processes through which they connect to the basement membrane.
The structure and functions of the nephron are such that, collectively, all its elements do not allow molecules with a diameter of more than 6 nm to pass through and filter smaller molecules that must be excreted from the body. The protein cannot pass through the existing filter due to special membrane elements and molecules with a negative charge.
What does a nephron consist of?
Each nephron is covered by a small capsule that looks like a double-walled cup (the Shumlyansky-Bowman capsule, named after the Russian and English scientists who discovered and studied it). The inner wall of this capsule is a filter that constantly cleanses our blood.
Nephron structure
This filter consists of a basement membrane and 2 layers of integumentary (epithelial) cells. This membrane also has 2 layers of integumentary cells, the outer layer being the vascular cells, and the outer layer being the cells of the urinary space.
All these layers have special pores inside them. Starting from the outer layers of the basement membrane, the diameter of these pores decreases. This is how a filter apparatus is created.
A slit-like space appears between its walls; it is from there that the renal tubules originate. Inside the capsule there is a capillary glomerulus; it is formed due to the numerous branches of the renal artery.
The capillary glomerulus is also called the Malpighian corpuscle. They were discovered by the Italian scientist M. Malpighi in the 17th century. It is immersed in a gel-like substance, which is secreted by special cells - mesagliocytes. And the substance itself is called mesangium.
This substance protects capillaries from unintentional rupture due to high pressure inside them. And if damage does occur, then the gel-like substance contains the necessary materials that will repair these damages.
The substance secreted by mesagliocytes will also protect against toxic substances of microorganisms. It will simply destroy them immediately. Moreover, these specific cells produce a special kidney hormone.
The tubule emerging from the capsule is called a convoluted tubule of the first order. It's really not straight, but crooked. Passing through the medulla of the kidney, this tubule forms the loop of Henle and again turns towards the cortex. On its way, the convoluted tubule makes several turns and necessarily comes into contact with the base of the glomerulus.
A second-order tubule is formed in the cortex and flows into the collecting duct. A small number of collecting ducts join together to form excretory ducts that pass into the renal pelvis. It is these tubes, moving towards the medulla, that form the brain rays.
Functions
Depending on the type, kidney nephrons perform the following functions:
- filtration;
- reverse suction;
- secretion.
The first stage is characterized by the production of primary urea, which is further purified by reabsorption. At the same stage, beneficial substances, micro- and macroelements, and water are absorbed. The last stage of urine formation is represented by tubular secretion - secondary urine is formed. It removes substances that the body does not need.
The structural and functional unit of the kidney is the nephron, which:
- maintain water-salt and electrolyte balance;
- regulate the saturation of urine with biologically active components;
- maintain acid-base balance (pH);
- control blood pressure;
- remove metabolic products and other harmful substances;
- participate in the process of gluconeogenesis (production of glucose from non-carbohydrate compounds);
- provoke the secretion of certain hormones (for example, those that regulate the tone of the vascular walls).
The processes occurring in the human nephron make it possible to assess the condition of the organs of the excretory system. This can be done in two ways. The first is to calculate the content of creatinine (a protein breakdown product) in the blood. This indicator characterizes how well the kidney units cope with the filtration function.
The work of the nephron can also be assessed using a second indicator - glomerular filtration rate. Blood plasma and primary urine should normally be filtered at a rate of 80-120 ml/min. For older people, the lower limit may be the norm, since after 40 years the kidney cells die (there are significantly fewer glomeruli, and it is more difficult for the organ to fully filter fluids).
Functions of some components of the glomerular filter
The glomerular filter consists of fenestrated capillary endothelium, basement membrane and podocytes. Between these structures is the mesangial matrix. The first layer performs the function of coarse filtration, the second filters out proteins, and the third cleanses the plasma of small molecules of unnecessary substances. The membrane has a negative charge, so albumin does not penetrate through it.
Blood plasma is filtered in the glomeruli, and their work is supported by mesangiocytes - cells of the mesangial matrix. These structures perform contractile and regenerative functions. Mesangiocytes restore the basement membrane and podocytes, and, like macrophages, they engulf dead cells.
If each unit does its job, the kidneys function like a well-coordinated mechanism, and urine formation occurs without toxic substances returning to the body. This prevents the accumulation of toxins, the appearance of swelling, high blood pressure and other symptoms.
Nephron function disorders and their prevention
If the functioning of the functional and structural units of the kidneys is disrupted, changes occur that affect the functioning of all organs - the water-salt balance, acidity and metabolism are disrupted. The gastrointestinal tract ceases to function normally, and allergic reactions may occur due to intoxication. The load on the liver also increases, since this organ is directly related to the elimination of toxins.
Similar article - Phlebology Center Moscow reviews
For diseases associated with transport dysfunction of the tubules, there is a single name - tubulopathies. They come in two types:
The first type is congenital pathology, the second is acquired dysfunction.
Active nephron death begins when taking medications whose side effects indicate possible kidney disease. Some drugs from the following groups have a nephrotoxic effect: nonsteroidal anti-inflammatory drugs, antibiotics, immunosuppressants, antitumor drugs, etc.
Tubulopathies are divided into several types (based on location):
With complete or partial dysfunction of the proximal tubules, phosphaturia, renal acidosis, hyperaminoaciduria and glycosuria may occur. Impaired reabsorption of phosphates leads to the destruction of bone tissue, which is not restored during therapy with vitamin D. Hyperaciduria is characterized by a violation of the transport function of amino acids, which leads to various diseases (depending on the type of amino acid).
Such conditions require immediate medical attention, as do distal tubulopathies:
- renal water diabetes;
- tubular acidosis;
- pseudohypoaldosteronism.
Violations can be combined. With the development of complex pathologies, the absorption of amino acids with glucose and the reabsorption of bicarbonates with phosphates may simultaneously decrease. Accordingly, the following symptoms appear: acidosis, osteoporosis and other bone tissue pathologies.
Kidney dysfunction is prevented by proper diet, drinking enough clean water and an active lifestyle. It is necessary to contact a specialist in a timely manner if symptoms of kidney dysfunction occur (to prevent the transition of the acute form of the disease to the chronic form).
It is not recommended to take medications (especially prescription drugs with nephrotoxic side effects) without a doctor's prescription - they can also disrupt the functions of the urinary system.
The renal unit is called the nephron. It is responsible for filtering blood and forming primary urine. The functional unit of the kidney removes toxins and metabolic products from the body. Nephrons work around the clock, filtering up to 1.7 thousand liters of blood plasma. In this case, a little more than a liter of excreted urine is formed. In this case, about 170 liters of primary urine are formed per day. Subsequently, this volume is condensed to the daily urine norm. There are about 2 million nephrons in our kidneys. If we calculate the total surface area of the nephrons performing the excretory function, it will be approximately 8 m². This is three times the area of skin.
Sections of kidneys and nephrons
The nephron, the structure of which became known to scientists for certain only after a number of experiments, is located in each of the structural elements of the most important organs for the body - the kidneys. The specificity of kidney function is such that it requires the existence of several sections of structural elements at once: a thin segment of the loop, distal and proximal.
All nephron channels are in contact with laid storage tubes. As the embryo develops, they improve arbitrarily, but in an already formed organ, their functions resemble the distal part of the nephron. Scientists have repeatedly reproduced the detailed process of nephron development in their laboratories over several years, but true data were obtained only at the end of the 20th century.