Glomerulonephritis - what is it, symptoms and treatment
Glomerulonephritis is an infectious-allergic disease that belongs to the group of acquired kidney diseases. Various forms of glomerulonephritis differ in etiology, manifestations, course of the disease and its outcome. Most often it is characterized by immune inflammation of the renal glomeruli, as well as further, secondary inflammation of the renal tubules and interstitium.
There are acute glomerulonephritis, a fast-acting form of the disease, and chronic glomerulonephritis. The acute form of the disease can most often be caused by a previous streptococcal infection - post-streptococcal glomerulonephritis. According to etiology, primary glomerulonephritis is distinguished and secondary, which occurs in systemic diseases - systemic lupus erythematosus, rheumatism, periarteritis nodosa and others.
Causes
Acute and chronic infectious processes provoked by pathogenic streptococcus and other microorganisms can lead to the development of glomerulonephritis. These include:
- streptoderma;
- scarlet fever;
- chicken pox;
- angina;
- tonsillitis;
- pneumonia;
- measles;
- acute respiratory viral infections.
Also, the reasons that provoke the development of glomerulonephritis may be hypothermia and high humidity, which lead to impaired circulation. The main infectious pathogens that provoke the development of glomerulonephritis are:
- Neisseria;
- toxoplasma;
- streptococcus;
- Staphylococcus aureus;
- viruses.
Most often, the development of glomerulonephritis is observed several days after the infection. The main causative agent is group A beta-hemolytic streptococcus.
Classification
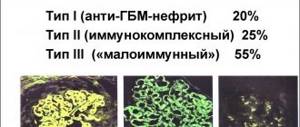
The classification of glomerulonephritis is varied; there are several principles of division. According to the method of occurrence, the following types of glomerulonephritis are distinguished:
- Acute - manifests itself at the first deviations of the renal glomeruli, the onset of the disease is spontaneous. It can be quickly treated, although in advanced cases it becomes chronic.
- Chronic is a protracted cyclic form of acute glomerular nephritis.
- Subacute - known as malignant (rapidly progressive). It is difficult to treat glomerulonephritis of this form, since the streptococcal virus does not respond well to medications. In this case, complications of glomerulonephritis are often observed, such as uremia, chronic renal failure, which can threaten the patient’s life.
Clinical forms of chronic glomerulonephritis are:
| Nephrotic | characterized by severe swelling, the pressure in this case will most likely be normal. |
| Hematuric | the clinic is manifested in the presence of blood clots in urine, an increase in the concentration of protein compounds during a biochemical analysis. There is swelling, but it is small and unnoticeable. In the later stages, hypertension appears. |
| Mixed | The reasons need to be considered in aggregate; it is difficult to determine the main symptom. |
| Latent | with this type of diffuse glomerulonephritis, the patient does not feel any abnormalities in health. There is slight swelling and slight pressure fluctuations. This is where oliguria manifests itself - a decrease in the volume of fluid excreted from the body. Kidney disease can be detected through laboratory tests. |
| Hypertensive | manifests itself as high blood pressure. In this case, the urge to urinate changes its regularity, and when examining urine, an increase in the amount of protein appears and blood discharge is present. |
Classification of chronic glomerulonephritis:
- Primary - considered as a separate kidney disease.
- Secondary - the disease was the result of other abnormalities in the patient’s health. For example, arthritis, periarthritis nodosa, systemic lupus, etc. Focal segmental rheumatoid glomerulonephritis can be caused by various pathologies; the immune system is systemically affected.
A separate item considers acute mesangioproliferative glomerulonephritis, which was caused by allergic streptococcus.
What it is
The term “glomerulonephritis” (or glomerular nephritis) means a set of kidney pathologies that are accompanied by damage to the glomerular apparatus and impaired filtration function. In the domestic medical school, the diagnosis “chronic glomerulonephritis” is actively used, which combines pathologies with slower progression, periodic exacerbations and the development of nephrotic syndrome. However, it should be noted that in the international classification this form is not distinguished separately.
Most often, chronic glomerulonephritis is diagnosed in the age category of 20-40 years. At the same time, men get sick somewhat more often than women. In the 2000s, a number of studies were conducted that showed that the main cause of death in these patients is cardiovascular events, the risk of which increases significantly with impaired renal function. Only in second place is end-stage renal failure, which manages to develop in 20% of patients.
Symptoms of glomerulonephritis
Depending on the various forms of glomerular damage, certain symptoms of glomerulonephritis may predominate.
- Blood in the urine - urine the color of “meat slop”;
- Swelling of the face (especially the eyelids), as well as the feet and legs;
- Increased blood pressure;
- Decreased urine output, thirst;
- Increased body temperature (rare);
- Lack of appetite, nausea, vomiting, headache, weakness;
- Weight gain;
- Dyspnea.
Acute glomerulonephritis develops 6-12 days after an infection, usually streptococcal (tonsillitis, tonsillitis, scarlet fever), including skin infection (pyoderma, impetigo).
The disease can develop after other infections - bacterial, viral, parasitic, as well as after other antigenic influences - serum, vaccine, medicine.
In the classic cyclic course, acute glomerulonephritis is characterized by changes in urine (red urine due to blood), edema, and a decrease in the amount of urine excreted.
Why does glomerulonephritis develop in humans?
For the formation of such a disease, only one active factor is not enough. Often the decisive role in the occurrence of the disease is played by the activity of the human immune system: if he is unstable to various kinds of pathologies, in 90% of cases he will develop glomerulonephritis after suffering a streptococcal infection or chemical poisoning.
What factors provoke the formation of such a condition:
- hypothermia;
- scarlet fever;
- erysipelas;
- influenza and ARVI;
- food poisoning;
- allergic reactions (urticaria, angioedema, anaphylactic shock);
- working with pesticides;
- bites of snakes, insects, wild animals;
- taking narcotic drugs and drug overdose;
- exposure to radiation and exposure.
Complications
In acute diffuse glomerulonephritis, the following complications may occur:
- Acute heart failure (in less than 3% of cases);
- Acute renal failure (in 1% of patients);
- Acute renal hypertensive encephalopathy (preeclampsia, eclampsia);
- Bleeding in the brain;
- Acute visual impairment (transient blindness);
- Transition to chronic diffuse glomerulonephritis.
One of the factors in the chronicization of the inflammatory process in the kidneys may be the so-called hypoplastic dysplasia of the kidney, i.e. lag in the development of renal tissue from the chronological age of the child.
With a progressive course, unresponsive to active immunosuppressive therapy, chronic diffuse glomerulonephritis passes into its final stage - a secondary wrinkled kidney.
Treatment prognosis and likely consequences
The success of treatment largely depends on the patient’s age and state of health. It is known that people suffering from hypertension and diabetes have many more complications compared to other patients. This is largely due to disruption of metabolic processes occurring in the body. Treatment of the disease can last from two weeks to several years.
In children and adolescents, kidney function is restored by an average of 98%, in older people - by 89%, and in the elderly - only by 70%.
What unpleasant consequences can arise from the disease:
- proliferation of connective tissue - glomerulosclerosis;
- acute or chronic kidney failure;
- water-electrolyte imbalance;
- cerebral edema;
- myocardial infarction.
Lifestyle of patients after illness
Glomerulonephritis is a rather serious pathology that leaves its mark on everyday life. Few people think about it, but even performing such ordinary actions as swimming in an open body of water or going to the bathroom may be prohibited. But there are also a huge number of myths about things that should not be done with glomerulonephritis:
- Give birth to a child. The disease itself, with proper treatment, is not a contraindication for pregnancy. However, during exacerbation of glomerulonephritis, doctors recommend waiting for stable remission (at least one year), and only after that engage in offspring planning. Deterioration of the kidneys during pregnancy can negatively affect a woman’s health and lead to premature birth and even fetal death.
- Visit baths or saunas. In acute glomerulonephritis, any heating causes an increase in symptoms, and the course of the disease becomes more severe. That is why doctors advise giving up such entertainment during treatment. During the recovery period, baths can be used as an aid: warm air has a beneficial effect on the body, increasing the activity of the immune system.
- Exercise. Heavy loads associated with dangerous activities (mountain climbing, river rafting, orienteering) will have to be abandoned. However, more gentle types of training (tennis, yoga, badminton, swimming) still remain available to patients.
Diagnostics
Diagnosis of glomerulonephritis is made based on the results of studies that allow one to assess the degree and severity of renal dysfunction and identify the level of activity of the process.
The presence of the disease is indicated by:
- The presence of leukocytosis, accelerated blood ESR in the general blood test.
- In a biochemical study of a blood test, an increase in residual nitrogen and urea, an increase in creatinine and cholesterol, and a decrease in the level of albumin proteins.
- Disturbance of the balance of acids and alkalis in the blood.
- Moderate proteinuria (excretion of albumin protein in the urine) for up to two to three weeks.
- Microscopy of urinary sediment reveals specific casts indicating damage to the renal glomeruli.
- Hematuria is the appearance of blood in the urine (urine is dirty-colored “meat slop”, dark brown or black, and with microhematuria the color is unchanged).
- Decreased diuresis, nocturia (increased urine production at night) with the Zimnitsky test.
Sometimes a kidney biopsy is prescribed for subsequent morphological examination of the bioptic material.
How is the diagnosis made?
Nephrologists diagnose the disease. The main criterion in identifying chronic glomerulonephritis is the data of clinical and laboratory studies. First, the doctor collects anamnesis, takes into account the fact of existing chronic infections, systemic pathologies, and an acute attack of glomerulonephritis.
Laboratory examination of the patient includes the following tests:
- Clinical urine analysis. The sample contains many altered red blood cells, casts (hyaline, granular), leukocytes, a large amount of protein, while the density of urine is reduced or increased - this depends on the stage of the disease.
- Zimnitsky's test. The daily volume of urine and its density are reduced or increased. An increase in the amount of urine and a decrease in density indicate the stage of decompensation of the disease.
- Blood chemistry. There is a decrease in protein fractions (hypoproteinemia and dysproteinemia), the presence of C-reactive protein, sialic acids, high levels of cholesterol and nitrogenous compounds (in the stage of decompensation).
- Blood immunogram. The analysis determines an increase in the titer of antibodies to streptococcus (antistreptolysin, antihyaluronidase, antistreptokinase, antideoxyribonuclease), an increase in the level of immunoglobulins, a decrease in complement factors (proteins involved in the formation of the body's immune response during the interaction of antibodies and antigens).
- Microscopic analysis of a kidney tissue sample taken during biopsy. The method allows you to assess structural changes in the renal glomeruli, which is important for prescribing adequate therapy. Signs of growth (proliferation) of glomerular structures, their infiltration by immune cells - monocytes and neutrophils, and the presence of deposits in the glomeruli of IC (immune complexes) are detected.
A urine test for glomerulonephritis shows deviations from the norm and allows you to determine the stage of the disease
Instrumental examination of the patient includes the following procedures:
- Echography (ultrasound) of the kidneys. A decrease in the size of the kidneys is detected due to sclerosis of the parenchyma.
- Excretory (intravenous) urography. A method that involves injecting a special X-ray contrast agent into the patient’s blood, followed by a series of photographs demonstrating the ability of the kidneys to accumulate and eliminate this substance. In this way, the degree of impairment of the filtering and concentration functions of the kidneys is assessed.
- Ultrasound Dopplerography of the renal vessels. Used to assess renal blood flow disorders.
- Dynamic nephroscintigraphy - radionuclide scanning of the kidneys. Allows you to evaluate structural and functional disorders in these organs.
- Kidney biopsy is necessary to assess destructive changes in the affected organ at the cellular level.
To evaluate changes in the structure of the kidneys, an ultrasound examination is performed
To identify changes in other organs, ultrasound of the heart and pleural cavities, ECG, and fundus examination may additionally be prescribed.
Chronic glomerulonephritis should be differentiated from such pathologies as:
- chronic pyelonephritis;
- polycystic kidney disease;
- nephrotic syndrome;
- kidney amyloidosis;
- nephrolithiasis;
- cardiac pathologies with arterial hypertension;
- kidney tuberculosis.
Video: diagnosis of chronic glomerulonephritis
Treatment of glomerulonephritis
Symptoms and treatment of glomerulonephritis are closely related. Treatment of acute and chronic forms of the disease in the acute phase is carried out only in the nephrological or therapeutic department of the hospital. Patients are recommended to rest in bed, and diet No. 7 is prescribed for therapeutic nutrition for kidney glomerulonephritis.
Treatment of chronic glomerulonephritis:
- General strengthening agents.
- Anti-inflammatory drugs (NSAIDs, corticosteroids).
- Anticoagulants (to reduce blood viscosity and prevent blood clots).
- Regular dialysis for severe renal failure.
- Kidney transplantation if conservative treatment of chronic glomerulonephritis is ineffective (does not eliminate further autoimmune destruction).
Treatment of acute glomerulonephritis:
- Strict bed rest.
- Antibacterial, antiviral treatment (if the disease is infectious).
- Symptomatic drugs (diuretics, antihypertensives, antihistamines).
- Immunosuppressive treatment (cytostatics).
- Dialysis - connecting an artificial kidney to a machine (with the rapid development of renal failure).
What is chronic glomerulonephritis
The chronic form of glomerulonephritis is a progressive inflammatory lesion of the renal glomeruli, leading to their sclerosis (scarring) and loss of functionality. Over time, chronic renal failure develops.
The disease has a relatively high prevalence and can occur at any age, but most often the first signs of damage to the glomeruli (glomeruli) are diagnosed at 25–40 years of age. Men get sick more often. The difference between a chronic process and an acute one is the long-term (more than a year) course of inflammatory-destructive changes and extensive (diffuse) bilateral kidney damage.
The structure of each kidney has a complex structural system, including nephrons, consisting of glomeruli (capillary weaves) in capsules and tiny tubules, in which a continuous process of filtering blood occurs with the formation of urine containing substances unnecessary for the body. The necessary elements remain in the bloodstream.
A continuous process of blood filtration occurs in the renal glomeruli (glomeruli).
With glomerulonephritis, the following changes occur in the kidneys:
- due to the inflammatory process, the walls of the glomerular vessels become permeable to blood cells;
- small blood clots form in the lumen of the glomerular capillaries, clogging their lumen;
- in the affected glomeruli, blood flow slows down or completely stops;
- blood cells clog the lumen of Bowman's capsule (the membrane covering the glomerulus) and the renal tubules;
- in the affected nephron, the entire sequential filtration process is disrupted;
- the tissue of the glomerular capillaries, renal tubules, and then the entire nephron is replaced by scar tissue - nephrosclerosis develops;
- the death of nephrons leads to a significant decrease in the volume of filtered blood, as a result of which renal failure syndrome develops;
- functional kidney failure leads to the accumulation of harmful substances in the blood and the excretion of elements needed by the body in the urine.
Chronic inflammation of the renal glomeruli is often the outcome of an acute immunoinflammatory process in the kidneys, but can also be primary chronic.
With glomerulonephritis, inflammation and destruction of the renal glomeruli occurs
Diet for acute glomerulonephritis
In the fight against this pathology, it is very important to adhere to a special diet. Patients are advised to reduce to a minimum the amount of fluid consumed, as well as salt and protein. A patient can eat no more than two grams of salt per day. Among food products that contain protein, you should give your preference to egg whites and cottage cheese. As for fats, you can eat no more than fifty grams of them per day.
The normal daily amount of fluid in this case is considered to be six hundred to a thousand milliliters. Such patients are strictly prohibited from consuming meat soups. In most cases, a correct and timely course of therapy makes it possible not only to heal the patient, but also to completely restore the functioning of his kidneys.
Pathogenesis
It is also worth paying attention to the pathogenesis of RPGN due to antineutrophil-associated cytoplasmic antibody associated with crescentic glomerulonephritis. In the nephrotoxic nephritis model, T cells and dendritic cells are involved in the activation and proliferation of parietal epithelial cells, which contribute to sickle cell formation and glomerular damage. The role of lysosome-containing membrane protein and neutrophil extracellular traps has been well studied in studies of associated glomerulonephritis.
Folk remedies
Here are some effective remedies that will help quickly restore kidney function:
- Take one tablespoon of dried black elderberry flowers, pour a glass of boiling water, leave until it cools completely. Take the medicine 1/3 cup three times a day before meals. The duration of taking elderflower infusion is 3-4 weeks, until complete cure.
- Healing collection for swelling. Mix flaxseed (4 parts) with dry birch leaves (3 parts) and field steel root (the same amount). Pour boiling water over it and leave to steep for a couple of hours. Then strain and consume a third of a glass three times a day. And so - for a week. After this time, you will forget what swelling is, get rid of pressure and heart pain.
- Mix 1 teaspoon of corn silk and the same amount of cherry tails, pour in 500 ml of boiling water and leave to steep until the medicine cools to room temperature. You need to take the infusion ¼ glass three times a day half an hour before meals. Treatment should be continued until the symptoms of glomerulonephritis disappear.
To boost immunity and help the body quickly cope with the pathological process, you need to take the following medicine every day, a teaspoon: a glass of honey, a tablespoon of walnuts, a tablespoon of hazelnuts, the peel of one lemon. Mix everything and store in a warm place.
Why is the rapidly progressing form of the disease dangerous?
Such glomerulonephritis is dangerous with the risk of developing acute kidney failure. It is necessary to treat glomerulonephritis at this stage, because it can cause kidney failure.
Acute failure is accompanied by severe azotemia and a pronounced drop in the excretory function of the kidney. At the same time, a pronounced disturbance of the acid-base balance occurs in the body. In most cases, acute renal failure is a reversible process, and with proper treatment, the functions of the excretory system are gradually restored. In some cases (with the formation of a deep lesion), the disease turns into a progressive chronic form.
In the oliguric phase of acute renal failure, diuresis does not exceed 0.5 l per day. Urine contains a large amount of protein. Symptoms of this phase:
- severe nausea and vomiting;
- alternating diarrhea and constipation;
- dyspnea;
- moist wheezing (may indicate the development of pulmonary edema);
- increased blood pressure;
- arrhythmia caused by hyperkalemia;
- An increase in the amount of free nitrogen can cause damage to internal organs.
In the diuretic phase, there is a gradual restoration of daily diuresis; Sometimes patients experience polyuria. In this regard, the body may develop hypokalemia. It is accompanied by muscle paresis and severe weakness.
What you need to know about chronic kidney failure
Chronic kidney failure is characterized by a progressive course. It is the outcome of chronic untreated glomerulonephritis. The higher the rate of sclerosis of the kidney parenchyma, the faster the pathology develops. In the initial stage (filtration rate is at least 40 ml per minute), polyuria, pollakiuria, nocturia and hypertension occur.
If the filtration rate drops further, a conservative stage develops. It continues until this figure exceeds 15 ml per minute. The symptoms described earlier include asthenic syndrome, decreased ability to work and decreased appetite. The patient's azotemia increases and body weight decreases.
When the kidney filtration rate decreases to less than 15 ml per minute, the patient develops oliguria and overhydration. Symptoms of end-stage chronic renal failure:
- uncontrolled hypertension;
- dysfunction of the left ventricle;
- pulmonary edema;
- visual impairment;
- drowsiness;
- anorexia;
- muscle twitching;
- ammonia odor from the mouth;
- pericarditis;
- dryness and pallor of the skin, its jaundice;
- human apathy.
During the conservative stage of the disease, the patient is given drugs that support kidney activity and strengthen the body. The amount of table salt and protein products is limited. In the terminal stage, hemodialysis is used, and issues related to kidney transplantation are resolved.
Prevention
Proper treatment of streptococcal diseases, compliance with the calendar of preventive vaccinations and sanitization of foci of infection in the body constitute the main preventive measures. Children who have suffered post-streptococcal glomerulonephritis should be under medical supervision for 5 years after treatment.
Preventive medical examinations and laboratory tests allow you to detect the disease early and avoid complications. Self-medication and neglect of general symptoms most often leads to severe forms of the disease.