General information about the disease
Humanity has known about glomerulonephritis for a very long time. This disease was first described in 1827. This work was carried out by the English doctor R. Bright. At the beginning of the next century, a classification of glomerulonephritis according to the course of the disease appeared. However, this did not mean that the disease was being carefully studied by specialists. The active stage of research and development of clinical guidelines for glomerulonephritis began in 1951 with the development of the kidney biopsy technique.
The cause of symptoms lies in the entry of harmful microorganisms into the body. The disease is caused by streptococci, staphylococci, enterococci, diplococci, etc. Glomerulonephritis develops after streptococcal infections (sore throat, scarlet fever, pharyngitis, bronchitis, pneumonia, etc.)
Why is the disease called glomerulonephritis (according to ICD-10 - N00, N01, N03, N18)? The term comes from the word "glomerulus". It is borrowed from the Greek language. This word is translated as “ball”. This is the name of the main part of the kidney tissue. To explain what a glomerulus is, let's start with the nephron. This is the structural unit of the kidney. The nephron contains a collection of small blood vessels. They are all intertwined and resemble a ball in appearance. It is this structure that is affected, causing the symptoms of glomerulonephritis.
Indicators and interpretation of urine analysis for glomerulonephritis
Glomerulonephritis is a serious infectious disease that affects the tissue structure of the renal vessels, which leads to their functional failure in the formation of urine and the removal of toxins from the body.
The main reasons for its appearance are: infection with streptococcus, untreated viral diseases, hypothermia. And the consequence can be serious complications that pose a danger to human life.
Along with other examination methods, urine analysis for glomerulonephritis helps not only to clarify the diagnosis, but also to identify the stage, form of the disease, and also prescribe effective treatment.
Urinalysis happens:
- general;
- Rehberg breakdown;
- Zimnitsky's breakdown;
- microscopic examination of sediment.
General urine analysis
During the general examination, the levels of protein, leukocytes, erythrocytes, and casts are determined. Urine of healthy people is a clear, yellowish liquid. Its approximate composition:
- protein concentration does not exceed 0.033 g/l;
- leukocytes are no more than 4000 per 1 milligram;
- casts and red blood cells are absent.
What does the Rehberg test determine?
Increased standard indicators identified by general analysis require more thorough laboratory examination. The degree of renal filtration is determined by the Rehberg test. It detects the disease in the initial stages of manifestation, simultaneously measuring the level of creatinine in the excreted daily portion of urine.
Before carrying out the test, preliminary preparation of the patient is required in the form of refusal:
- smoking;
- eating meat and fish dishes;
- drinking alcoholic beverages.
On the day of the examination, it is also recommended to avoid any physical and emotional stress.
The patient collects urine for a day, the volume of which should reach three liters. The container is stored in a cool place. After 24 hours, the medical worker measures the mass, mixes it, and sends the required amount to the laboratory.
The rate of kidney filtration is different for women and men, depending on the age category. The average standard value is 110-125 milliliters per minute. A change of 10-15 points in any direction is not a sign of glomerulonephritis.
What is the Zimnitsky sample?
The analysis is carried out to assess the functioning of the kidneys, the dynamics of urine excretion in the daytime and evening, as well as to determine the density of the consistency.
The method consists of collecting eight daily portion samples every 3 hours. The degree of the disease is reflected in the volume of urine produced. Normal daily diuresis is 60%-80% of the total daily volume.
The density of urine is influenced by the concentration of excreted organic components (salts, uric acid, urea), as well as the volume of fluid exiting. The standard density indicator varies between 1008 -1010 g per liter. Changes in the standard indicate the presence of inflammation.
Examination of urinary sediment
This is the final stage of laboratory research. It is recommended to confirm the results of a general analysis that revealed deviations in the normative levels of red blood cells, epithelial cells, casts and leukocytes.
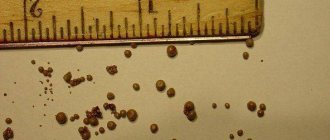
This method involves processing the required amount of the patient’s urine with a centrifuge. As a result of the procedure, a mass in the form of salts, blood cells, and epithelium falls to the bottom of the vessel. The laboratory technician transfers the composition onto a glass slide and, using a special staining agent, examines it under a microscope for the presence of certain components.
With glomerulonephritis, not only color and density change, but also components such as protein mass, red blood cells, and white blood cells. The amount of protein is especially high at the initial stage of the disease, when it exceeds 20 g per liter. This is accompanied by slight hematuria.
After 15-20 days, a decline in its intensity is observed. Protein is reduced to 1 g.
However, this fact does not indicate that a person has been cured; rather, it is a temporary phenomenon that effectively manifests itself again after a certain period.
The presence of hyaline or granular cylindrical deposits is not always observed; in rare cases, epithelial casts are detected. As the disease progresses, their levels rise sharply.
Purulent streaks in the urine are a sign of an increased level of leukocytes, the levels of which reach up to 30 units in the field of view.
The study of urine according to Nechiporenko also reveals a high content of red blood cells. The presence of these trace elements is accompanied by nephritic syndrome, which is characterized by:
- swelling of the face and legs;
- high blood pressure;
- constant thirst;
- malaise with temperature changes;
- lumbar pain.
A study using the Nechiporenko method determines not only the quantity, but also the condition of red blood cells. If they are deformed, then glomerular hematuria, typical of glomerulonephritis, is diagnosed. With their other form, this diagnosis is not confirmed.
According to the degree of infection, glomerulonephritis is divided into several stages:
- spicy;
- subacute;
- chronic.
Urine in the acute stage of glomerulonephritis
The first sign of an inflammatory process is a different color, cloudiness of the composition, and a change in structure. In addition, flakes or bloody streaks may often be visible. Using a general analysis, the following pathologies can be identified:
- unusual shade;
- altered density;
- decreased volume of urination;
- presence of protein mass;
- exceeding the standard of red blood cells and leukocytes.
The appearance of blood cells is a symptom of impaired renal filtration functions (macrohematuria), as a result of which the color of urine turns brownish-red, resembling water after washing meat (the color of meat slop). A more saturated brown tone appears when the norm of urate salts is exceeded. With an increased amount of phosphates and uric acid, the color range becomes lighter and sometimes discolored.
With glomerulonephritis, along with a change in color, the volume of exiting fluid, its structure and density, which depends on the concentration of released organic components (salts, uric acid, urea), are also disrupted.
The limit for the presence of components is 1010 per liter. Their actual presence is more accurately determined by the Zimnitsky method.
During this period, despite the amount of liquid drunk, infected people at different times of the day experience a sharp reduction in the frequency of urination, and also a decrease in the volume of urine released. There is also an increase in nighttime and a sharp decrease in daytime output.
In a healthy person, daytime diuresis is about 2 times higher than nighttime, and the daily volume is in the range of 0.8-1.5 liters. A decrease in these indicators is a sign of impaired renal filtration, the degree of which is revealed by the Rehberg test.
It determines the effectiveness of the kidneys in cleansing the body of harmful substances and reveals the clearance of creatinine, the main element of filtration. For men and women, the speed of this process is different, depending on their age category.
The average standard value is from 110 to 125 milliliters per minute.
Acute glomerulonephritis has two characteristic forms: cyclic and latent. The first is characterized by the rapid manifestation of all symptoms. In the second form, the period of infection occurs slowly, without obvious manifestations. Changes can only be detected through examinations. An untreated disease progresses to subsequent forms.
Urine indicators at the subacute stage
This is a more severe stage of inflammation, characterized by a high content of protein and red blood cells in the urine, pronounced swelling, a tendency to increase pressure, and an increase in temperature.
The presence of a large protein mass is indicated by the appearance of foam in the urine. During urination, increased levels of albumin, the main component of blood plasma, are washed out along with protein.
The color of urine becomes more saturated, the composition becomes cloudy. The process of leaching of this element is called “albuminuria”, which occurs when blood cells exceed 300 mg.
per day passes into another stage - proteinuria.
It is also characterized by the presence of various types of sediments that disrupt the functioning of the renal canals. These include cylinders. At this stage of inflammation, complications often appear. The kidneys may lose their functionality within a few weeks, followed by the onset of acute renal failure.
Features of urine composition in chronic form
Chronic glomerulonephritis is characterized by a slow course of the disease (latent form). Sometimes this happens without any special visual symptoms, only the composition of the urine changes.
Progressive proteinuria is observed when more than 20 grams of protein are lost per day (with a standard of 3 g). The urine becomes more cloudy and foamy, but there may be no bloody streaks or they appear in rare cases. There are no pressure or temperature changes.
Mild symptoms usually do not alarm infected people, who classify them as manifestations of a cold. Delayed consultation with a doctor and lack of treatment can contribute to the transition of this condition into a serious illness - uremia with irreversible consequences.
Chronic glomerulonephritis is divided into several clinical forms:
- nephrotic – a combination of kidney inflammation with nephrotic syndrome (proteinuria, edema, hematuria);
- hypertensive, accompanied by an increase in blood pressure;
- mixed, combining the two previous ones;
- latent - with mild symptoms that can last more than 5-9 years;
- hematuric – with the presence of blood in the urine and a low protein content.
All of the listed forms of the chronic stage of the disease are dangerous due to their relapses.
Glomerulonephritis is not a death sentence, but a treatable disease. The sooner the patient consults a doctor, the faster the diagnosis will be made and effective treatment will be prescribed.
Source: https://MoiPochki.ru/laboratornaya-diagnostika/analiz-mochi-pri-glomerulonefrite-pokazateli.html
Types of glomerulonephritis
There are several classifications of the disease. In accordance with the nosological principle, primary and secondary glomerulonephritis are distinguished. In the first option, the cause of the pathological condition is unknown, and in the second, the disease develops due to systemic diseases, liver diseases, and the use of certain medications.
Taking into account the course of the disease, glomerulonephritis is divided into:
- For an acute form. With proper and timely treatment of glomerulonephritis, recovery occurs.
- For subacute form. It is characterized by a rapid, often malignant course. With such glomerulonephritis, acute renal failure may develop.
- For the chronic form. This type of disease is characterized by a progressive course leading to chronic renal failure.
Acute glomerulonephritis, in turn, is divided into post-streptococcal and post-infectious (classification by etiology), as well as epidemic and sporadic (classification by epidemiology). Chronic glomerulonephritis also has several forms:
- latent – changes are detected only in the urine of a sick person;
- hematuric – the presence of edema and arterial hypertension;
- hypertensive – changes in urine, arterial hypertension are observed;
- nephrotic – nephrotic syndrome is detected, there is no arterial hypertension;
- mixed - in this form, nephrotic syndrome can be combined with arterial hypertension, hematuria, and azotemia.
Contents of urine tests.
Laboratory studies for glomerulonephritis show the following data:
- decrease in urine volume;
- increase in urine density;
- detection of large amounts of protein;
- traces of blood in the analysis;
- the presence of bacteria characteristic of this disease.
The reddish color of urine should alert both the patient and the doctor, as it indicates glomerulonephritis. The diagnosis is confirmed by an excess of albumin levels, approximately 10 ml and above.
Sometimes changes in urine persist for a long time, even when there are no clinical manifestations. In half of the patients, tests demonstrate the presence of protein, leukocytes, casts and epithelial cells.
Red blood cells in this disease have a deformed shape, which indicates a violation of filtration in the kidneys. When the analysis shows normal-shaped red blood cells, doctors diagnose another disease.
Symptoms and course of acute glomerulonephritis
The acute form of the disease in many people begins with a simple sore throat. First, your throat hurts and your temperature rises. Unpleasant symptoms last for several days. Then recovery comes. It seems that the disease has subsided, but then the sore throat is replaced by acute glomerulonephritis (after about 1–2 weeks). It makes itself felt with high fever and deterioration in health. The amount of urine produced decreases, and it also takes on a reddish tint. Swelling appears quickly. Blood pressure also rises and headaches begin to occur.
Edema is one of the important symptoms of glomerulonephritis. A red tint to the urine may not be observed, but swelling occurs in 70–90% of cases. Very often they appear on the face. They indicate that the kidneys cannot cope with the function of excreting urine. The swelling is very noticeable in the morning. By evening they usually decrease. It is important to note that swelling is not always visible. Sometimes fluid accumulates in the pleural, abdominal, or pericardial cavities. Due to such hidden edema, body weight increases significantly.
Experts recommend that people have their urine tested after a sore throat or other illnesses. In adults, the picture of glomerulonephritis is not too bright. Sometimes the disease is indicated not by symptoms, but by changes in tests. Mostly in children and adolescents, the acute form of glomerulonephritis occurs with a rapid onset.
Urinary sediment studies
The method is used only if a general biochemical analysis reveals deviations from the norm. Research is carried out to verify the diagnosis and prescribe a course of treatment if the patient requires it.
The essence of the method is to process urine in a special centrifuge. After this procedure, a precipitate in the form of salt, blood cells and epithelium falls out of the urine. Further, additional studies are being conducted using drugs that color certain components of urine.
Experts note that urine with glomerulonephritis can change its color to dirty red. The course of the disease affects the density of urine and the elements contained in it: proteins, erythrocytes and leukocytes.
During the development of pathology, the level of proteins in the body decreases, which is not evidence that the patient has been cured, since after 2-3 weeks it will return to its previous level.
Features of chronic glomerulonephritis
The chronic type of the disease is divided into several forms, which were discussed above. Each of them is characterized by certain symptoms of glomerulonephritis. For example, the latent form is characterized by mild urinary syndrome. A person may not be aware of the presence of an illness. As a result, the disease will progress for a long time - maybe 10, maybe 20 years. Eventually it will lead to the development of uremia. Due to impaired kidney function, the body will be poisoned by the products of protein metabolism.
But for example, the hypertensive form. In most cases, it develops from a latent form of acute glomerulonephritis. The most striking sign of the disease over a long period of time is severe hypertension. During the day, the pressure changes greatly, but it still does not reach high values. Due to changes negative for the body, left ventricular hypertrophy develops.
All forms of chronic disease are characterized by periodic relapses and remissions. Exacerbations of glomerulonephritis are most often recorded in autumn and spring and after harmful microorganisms that provoke sore throat and other diseases enter the body. Any form of chronic glomerulonephritis requires treatment. The onset of remission does not mean that a miracle has occurred and recovery has occurred. If you get sick, you need the help of a specialist. In the absence of treatment, glomerulonephritis progresses to the final stage - a secondary wrinkled kidney.
Specificity of tests for chronic glomerulonephritis.
The chronic form of glomerulonephritis is a consequence of the acute course of the disease. The reasons for this are different, but mainly it is hypothermia, alcoholism, and injury. Signs of a chronic disease appear periodically. The exacerbation is replaced by rest, when a weak urinary syndrome appears; its first signs are observed 14 days after the onset of the disease.
Laboratory tests of urine in this form of the disease are aimed at identifying the extent of the disease, preventing renal failure in time.
The chronic course of the disease is reflected in the analyzes as follows:
- Urine loses transparency and its density decreases.
- The volume of fluid released exceeds the norm, the patient is especially concerned about nighttime diuresis, which is greater than daytime diuresis.
- With nephritis, protein increases sharply.
- Microhematuria or macrohematuria is less commonly noted.
- Fibrin threads are determined.
Diagnosis of the disease
Diagnosis begins with interviewing the patient and clarifying complaints. The doctor suspects glomerulonephritis when the patient begins to complain of headache, dark urine, and swelling. Some people report nausea and vomiting. The doctor who has suspected glomerulonephritis must evaluate the medical history in the medical record. The document may indicate a previous infection several days or weeks before the exacerbation.
After the interview, a physical examination is performed. It allows you to detect signs of glomerulonephritis - swelling on the face, legs, increased blood pressure, etc. Laboratory and instrumental studies are also performed:
- general blood analysis;
- biochemical blood test;
- Analysis of urine.
The main diagnostic measure for suspected glomerulonephritis is a kidney biopsy. The indication for this procedure is the need to clarify the morphological form of the disease and conduct a differential diagnosis. Additionally, an ultrasound may be prescribed. Thanks to this diagnostic study, doctors exclude focal kidney diseases and urinary tract obstruction.
GLOMERULONEPHRITIS
Read:- Glomerulonephritis, pyelonephritis in pregnant women
- Diagnosis of acute glomerulonephritis
- Diagnosis of acute diffuse glomerulonephritis
- Diagnosis of chronic glomerulonephritis
- Differential diagnostic signs of chronic pyelonephritis, chronic glomerulonephritis and hypertension.
- Objectives of treatment of chronic glomerulonephritis
- Classification of glomerulonephritis
- Classification of glomerulonephritis
- Clinical forms of acute glomerulonephritis.
(based on the classification of Tareev E.M., 1982)
| Clinical forms (variants) | Disease phase | Functional state of the kidneys |
| 1. With isolated urinary syndrome (latent) 1.1. Hematuric (Berge's disease) 2. Hypertensive 3. Nephrotic 4. Mixed | Exacerbation Remission | 1. Function sufficient (not impaired) 2. Chronic renal failure (CRF): 2.1. Compensated, conservative stage (relative failure) 2.2. Terminal stage (absolute failure) |
EXAMPLES OF DIAGNOSIS:
1. Chronic glomerulonephritis, with isolated urinary syndrome, in the acute phase, with sufficient renal function.
2. Chronic glomerulonephritis, nephrotic form, in the acute phase. Chronic renal failure, end stage.
Appendix 3a
TESTS TO DETERMINE INITIAL LEVEL OF KNOWLEDGE
| Tests | Answers | |
| 1. | The following are filtered into the primary urine of a healthy person: a) water b) all blood protein c) only albumin d) sugar e) lipids | abg |
| 2. | In the tubular apparatus of the kidneys the following are reabsorbed: a) potassium b) water c) glucose d) albumins e) globulins | bvg |
| 3. | The following factors are involved in the pathogenesis of glomerulonephritis: a) immune inflammation of the basement membrane b) deposition of antigen-antibody complexes on the filtering surface of the glomerulus c) formation of capillary microthrombi d) none of the listed signs e) all of the listed factors | d |
| 4. | Glomerulonephritis can be a complication of all of the following diseases, except: a) SLE b) hemorrhagic vasculitis c) infective endocarditis d) myeloma e) streptococcal tonsillitis | G |
| 5. | What is the level of blood protein in nephrotic syndrome? a) hyperproteinemia; b) hypoproteinemia; c) norm | b |
| 6. | What is the urine protein level in nephrotic syndrome? a) proteinuria less than 1 g per day; b) proteinuria within 1 – 3 g per day; c) proteinuria more than 3–5 g per day. | IN |
| 7. | The following are not filtered into the primary urine of a healthy person: a) water b) potassium c) sodium d) magnesium e) nitrogenous wastes | bgd |
| 8. | For glomerulonephritis, urinary syndrome is characterized by: a) changes in the relative density of urine; b) proteinuria; c) glucosuria; d) bacteriuria; e) leukocyturia; f) erythrocyturia; g) cylindruria. | be |
| 9. | Markers of urinary syndrome in glomerulonephritis are: a) changes in the relative density of urine; b) proteinuria; c) glucosuria; d) bacteriuria; e) leukocyturia; f) erythrocyturia; g) cylindruria. | beige |
| 10. | What changes does nephrotic syndrome include? a) proteinuria more than 3 - 5 g per day; b) hypoproteinemia; c) hypoglycemia; d) hypercholesterolemia, triglyceridemia; e) hyperuraturia; f) bacteriuria; g) swelling. | abgzh |
| 11. | Nephrotic syndrome is characterized by all the signs except: a) hypoalbuminemia b) daily protein loss of more than 3 g/l c) isosthenuria d) hyperlipidemia e) edema | V |
| 12. | All symptoms are characteristic of glomerulonephritis, except: a) hypertension b) pain in the lumbar region c) changes in urine d) edema e) dysuria | d |
| 13. | What main syndromes do not occur with glomerulonephritis? a) hypertension; b) anemic c) edematous; d) infectious-toxic; d) nephrotic. | G |
| 14. | Name drugs not from the group of ACE inhibitors. a) verapamil, b) renitec; c) enalapril; d) trandalapril; e) fosinopril. | A |
| 15. | Determination of which indicator is most informative for identifying nephrotic syndrome? a) the amount of proteinuria; b) glomerular filtration; c) serum creatinine; d) serum cholesterol; e) tubular reabsorption of water. | A |
| 16. | What is the normal daily amount of urine? a) 0.25 - 0.5 l b) 0.5 - 1 l c) 1 - 1.5 l d) 1.5 - 2.5 l | |
| 17. | The criteria for the transition of acute glomerulonephritis to chronic are: a) persistence of general edema for more than 1 week; b) persistence of general edema for more than 2 weeks; c) persistence of arterial hypertension for more than 2 weeks; d) persistence of arterial hypertension for more than 2 months; e) persistence of proteinuria for more than 2 weeks; f) persistence of proteinuria for more than 2 months; f) persistence of proteinuria for more than 6 months. | bge |
| 18. | In acute glomerulonephritis, it is possible to detect: a) an increase in the relative density of urine; b) decrease in the relative density of urine; c) increase in leukocyturia; d) decrease in leukocyturia. | aw |
Appendix 3b
TESTS TO DETERMINE THE FINAL LEVEL OF KNOWLEDGE
| Test | Answer | |
| 1. | Glomerulonephritis can be a complication of all of the following diseases, except: a) SLE; b) hemorrhagic vasculitis; c) infective endocarditis; d) multiple myeloma; e) streptococcal sore throat. | G |
| 2. | Gross hematuria is characteristic of all kidney diseases, except: a) acute glomerulonephritis; b) kidney infarction; c) renal amyloidosis; d) kidney stone disease; e) hypernephroma. | V |
| 3. | In a 32-year-old man, examination revealed: blood pressure 170/120 mm Hg. Art., no edema, in the urine: protein 2.5 g/day, red blood cells 6-10 in the visual field, many granular casts, creatinine 88 µmol/l. Probable diagnosis? a) nephrotic syndrome; b) chronic pyelonephritis; c) chronic glomerulonephritis, latent form; d) chronic glomerulonephritis, hypertensive form; d) chronic renal failure. | G |
| 4. | The main indication for prescribing glucocorticoids for chronic glomerulonephritis: a) nephrotic syndrome; b) arterial hypertension; c) renal failure; d) hematuria; e) prevention of exacerbations; | A |
| 5. | Nephrotic syndrome is characterized by all the signs except: a) hypoalbuminemia; b) daily protein loss more than 3 g/l; c) isosthenuria; d) hyperlipidemia; d) swelling. | V |
| 6. | Chronic nephritis in the stage of chronic renal failure is characterized by: a) anemia b) oligoanuria c) arterial hypertension d) isohyposthenuria e) all of the above | d |
| 7. | In acute glomerulonephritis, the following statements are true: a) in the initial period, arterial hypertension develops in all patients; b) the appointment of indomethacin is mandatory; c) the most common form of the disease is nephrotic; d) all of the above are true; e) all of the above are incorrect. | d |
| 8. | All judgments regarding the cause of chronic renal failure are correct, except: a) renal amyloidosis b) massive diuretic therapy in elderly and senile people c) chronic glomerulonephritis d) chronic pyelonephritis e) chronic obstruction of the urinary tract | b |
| 9. | Recovery from the “defect” of acute glomerulonephritis occurs if the patient experiences: a) persistence of general edema for more than 1 week; b) persistence of general edema for more than 2 weeks; c) persistence of arterial hypertension for more than 2 weeks; d) persistence of arterial hypertension for more than 2 months; e) persistence of proteinuria for more than 2 weeks; f) persistence of proteinuria for more than 2 months; f) persistence of proteinuria for more than 6 months. | e |
| 10. | Dangerous complications of acute glomerulonephritis are all except: a) acute left ventricular failure b) hyperkalemia c) eclampsia d) anemia e) acute renal failure | G |
| 11. | For pathogenetic therapy of chronic glomerulonephritis, all means are used except: a) glucocorticoids; b) non-steroidal anti-inflammatory drugs; c) cytostatics; d) anticoagulants; e) hypotensive. | d |
| 12. | List the side effects of glucocorticosteroids a) (S-m Itsenko-Cushing) b) (Arterial hypertension) c) (Diabetes mellitus) d) (Osteoporosis) e) (Gastropathy) | a B C D E |
| 13. | The main indication for prescribing glucocorticoids for chronic glomerulonephritis: a) nephrotic syndrome; b) arterial hypertension; c) renal failure; d) hematuria; e) prevention of exacerbations. | A |
| 14. | Complications of chronic glomerulonephritis are all except: a) acute left ventricular failure; b) acute vascular insufficiency; c) hyperkalemia: d) eclampsia e) anemia f) acute renal failure g) chronic renal failure | abge |
| 15. | The outcomes of acute glomerulonephritis are: a) recovery; b) recovery from a “defect”; c) transition to a chronic form; d) all of the above. | G |
| 16. | The outcomes of chronic glomerulonephritis are: a) recovery; b) recovery from a “defect”; c) transition to chronic renal failure. | V |
| 17. | The criteria for the latent form of acute glomerulonephritis are: a) nephrotic syndrome; b) arterial hypertension; c) swelling of the face and/or anasarca; d) urinary syndrome | G |
| 18. | The criteria for the latent form of chronic glomerulonephritis are: a) nephrotic syndrome; b) arterial hypertension; c) swelling of the face and/or anasarca; d) urinary syndrome | G |
| 19. | The hypertensive form of chronic glomerulonephritis is characterized by the following: a) proteinuria less than 1 g per day; b) proteinuria within 1 – 3 g per day; c) proteinuria more than 3–5 g per day. | A |
| 20. | The criteria for the mixed form of chronic glomerulonephritis are: a) nephrotic syndrome; b) arterial hypertension; c) swelling of the face and/or anasarca; d) urinary syndrome | ab |
Appendix 4a.
Scheme of a step-by-step differential diagnostic search for the leading syndrome - “edema”
| Acute development of local edema after the use of vaccines, serums, antibiotics, other medications, food allergens, insect bites is dense, pale, and does not leave a pit when pressed. | Yes | Quincke's edema |
| No | ||
| Previous history of thyroiditis or strumectomy. The swelling is diffuse, does not shift, is dense (mucous), and develops gradually. Patients are slow and complain of chilliness and drowsiness. Bradycardia, hypotension, hypercholesterolemia | Yes | Hypothyroidism |
| No | ||
| The occurrence of edema is preceded by a long-term protein-free diet, severe enterocolitis with predominant damage to the small intestine, and resection of a significant part of the small intestine. They are localized in the lower extremities, back, doughy, and easily move when changing body position. Hypoproteinemia. | Yes | Hypoproteinemic edema |
| No | ||
| History of rheumatism, myocarditis, coronary heart disease. The appearance of edema is preceded by an enlarged liver. Localized on the lower extremities, increase towards the end of the day, cold, displaceable. From the circulatory system, physical data characteristic of a particular lesion of the heart muscle (myocarditis, cardiomyopathies, myocardial infarction, cardiosclerosis, etc.). | Yes | Chronic heart failure |
| No | ||
| Clinical manifestations of diabetes mellitus. Long history (more than 5 years). Edema syndrome develops gradually. Swelling is common and easily shifts when changing body position. Hypoproteinemia, hypoalbumininemia, hypercholesterolemia. Proteinuria, glucosuria. | Yes | Diabetic nephropathy |
| No | ||
| Anamnestic indications of chronic suppurative processes (osteomyelitis, abscesses, etc.), rheumatoid arthritis, tuberculosis. The swelling is diffuse, loose and easily displaced. Anemia, leukocytopenia, hypocholesterolemia. Proteinuria, cylindruria, microhematuria | Yes | Amyoloidosis of the kidneys |
| No | ||
| A history of possible acute glomerulonephritis, the use of vaccines, serums, etc., a wavy progressive course leading to the development of chronic renal failure. The swelling is general, pale, and easily shifts when changing body position. Hypoproteinemia, hypoalbuminemia, hypercholesterolemia. Various severity of urinary syndrome. May have hypertension | Yes | Chronic glomerulonephritis |
| Yes | ||
| Acute glomerulonephritis |
Appendix 4 b
Step-by-step scheme of differential diagnostic search in the presence of “Proteinuria” syndrome
| Proteinuria | ||
| High (more than 3 g/day t) | Moderate (from 1 to 3 g/day) | Mildly expressed (less than 1 g/day) |
| Nephrotic syndrome | ||
| Diabetic nephropathy | Hypernephroma | |
| Lupus nephritis | Hypertonic disease | |
| Kidney amyloidosis | Kidney tuberculosis | |
| Glomerulonephritis • acute · chronic | Pyelonephritis · acute · chronic | |
| Congestive kidney in chronic heart failure | ||
| Urolithiasis disease | ||
| Infectious-toxic kidney |
Appendix 4 in
Step-by-step scheme of differential diagnostic search in the presence of “Proteinuria” syndrome (mildly expressed)
| Multiple symptoms of clinical extrarenal manifestations (articular syndrome, skin symptoms: rashes, erythema, hemorrhages, etc.), pleurisy, non-infectious fever, drug intolerance, detection of LE cells in the blood, high ESR, in the urine - the predominance of erythrocyturia, cylindruria | Yes | Lupus nephritis |
| No | ||
| Fever, chills. In the blood: increased ESR, thrombocytosis, possible anemia. Often microhematuria | Yes | Hypernephroma |
| No | ||
| “Cardiac” history, shortness of breath, tachycardia, expansion of the borders of the heart, enlarged liver, swelling in the lower extremities | Yes | Congestive kidney in chronic heart failure |
| No | ||
| At the height of a severe inflammatory process (pneumonia, infectious diseases) and intoxication, pathological changes in the urine: proteinuria, microhematuria, disappearing during the period of convalescence | Yes | Infectious-toxic kidney |
| No | ||
| Anamnestic indications of the presence of hypertension for decades, the age of patients over 50 years old, combination with cardiac and cerebral manifestations (angina pectoris, myocardial infarction, cerebrovascular accidents, absence of anemia, the appearance of changes in urine often after hypertensive crises | Yes | Hypertonic disease |
| No | ||
| Chronic suppurative processes (osteomyelitis, abscesses of any location), rheumatoid arthritis, history of tuberculosis. In the blood: anemia, leukocytopenia, hypoalbuminemia, hyperfibrinogenemia. In the urine: persistent leukocyturia, cylinder-uria | Yes | Kidney amyloidosis |
| No | ||
| Clinical manifestations of diabetes mellitus over 5 years, macro- and microangiopathy. In urine: absence of glucosuria, normal relative density, cylindruria | Yes | Diabetic nephropathy |
| No | ||
| A history of tuberculosis of the lungs or other organs, dysuria, pain in the lumbar region. In the urine: hematuria (sometimes the only symptom of the disease), persistent massive pyuria, difficult to respond to nonspecific therapy, mycobacteria are cultured | Yes | Kidney tuberculosis |
| No | ||
| Attacks of renal colic, dysuria, stone passage, obstructive anuria. In urine: macro- or microhematuria | Yes | Urolithiasis disease |
| No | ||
| Acute onset, high fever, dysuria, severe intoxication of the body, pain in the lumbar region. In urine: normal relative density, significant pyuria, bacteriuria | Yes | Acute pyelonephritis |
| No | ||
| Chills in the evenings, fever, asymmetry of pain in the lumbar region, undulating course of the disease. In urine: low relative density, moderate leukocyturia, bacteriuria | Yes | Chronic pyelonephritis |
| No | ||
| Acute onset, association with streptococcal infection, possible edema, arterial hypertension. Reverse development of symptoms within 0.5-1 year. Urinary syndrome is characterized by proteinuria, which in dynamics can reach a high level (more than 1 g/day), micro- or macrohematuria, prevailing over leukocyturia, cylindruria, high relative density of urine, bilateral lesions. | Yes | Acute glomerulonephritis |
| No | ||
| There is often a history of acute glomerulonephritis, repeated streptococcal infections, and a wavy progressive course leading to the development of chronic renal failure. Urinary syndrome, as in acute glomerulonephritis, often low relative density of urine | ||
| Yes | ||
| Chronic glomerulonephritis |
· For a step-by-step scheme of differential diagnostic search in the presence of the syndrome - arterial hypertension, see the methodological development on the topic “Hypertension. Secondary arterial hypertension."
Appendix 5.
Date added: 2015-09-27 | Views: 1057 | Copyright infringement
Previous4Next
Nutritional Features
With glomerulonephritis, as with other kidney diseases, diet is one of the most important therapeutic agents. The acute form of this disease necessitates reducing the volume of fluid consumed (up to 600–800 ml per day). In the first days, they adhere to a fruit-sugar diet. With glomerulonephritis, they subsequently eat dairy and plant foods. It is allowed to eat dishes made from potatoes, vegetables, cereals, and pasta without adding salt. Recommended methods of cooking are boiling, stewing, and making purees.
For chronic glomerulonephritis, a gentle regimen is followed. First of all, limit the addition of salt to food. The permissible daily dose of this ingredient is from 2 to 4 g. Experts also recommend that for chronic glomerulonephritis, periodically completely eliminate salt from your diet for a while - for about 1-1.5 months. Following this advice will help you avoid exacerbations.
With chronic glomerulonephritis, patients strictly monitor their water balance. The volume of fluid consumed in 24 hours should be equal to the volume of urine excreted and slightly exceed this figure by about 300–500 ml. When swelling appears, they switch to fasting days. They are effective if carried out a couple of times a week. At such moments, adhere to an apple or potato-apple diet.
Features of collecting analyzes of different types.
Any examination requires preparation. Urine is collected in each case according to certain rules.
The Rehberg test requires the patient to give up smoking, alcohol and protein foods one day before the tests are collected. On the day of the examination, you need to minimize physical activity and psycho-emotional stress. For this analysis, blood is donated in the morning on an empty stomach, and urine is collected for 24 hours, starting at six in the morning. During the examination, urine volume is determined and creatine concentration is analyzed. With this method, the weight, height and age of the patient are taken into account.
A general analysis is carried out in the morning, collecting urine in a clean container, after performing a morning toilet of the intimate area. An average portion of urine is suitable for analysis. This test should be avoided during menstruation and for 7 days after cystoscopy. For an accurate laboratory examination, at least 50 ml of urine is required.
The Zimnitsky test is carried out over the course of 24 hours, collecting urine every 3 hours in separate jars, and the time is marked on each of them. Fluid intake should be minimized to 1.5 liters. The study determines the specific gravity of urine and the amount of fluid consumed. In this case, the density of urine should not be greater than the density of plasma.
The Nechiporenko examination is carried out in the morning, collecting an average portion of urine in a separate container. In terms of volume, the study requires at least twenty-five milliliters.
Bacterial culture is carried out before prescribing antibacterial therapy. The minimum amount of urine for analysis is 10 milliliters.
Sample menu for the day
What kind of nutrition can there be for the disease in question? Following a diet for glomerulonephritis, people cook cereal in milk for breakfast, cook pasta, and eggs. Drinks allowed include coffee with milk, tea with sugar, and tea with milk. Particular attention should be paid to eggs. They are not fried for glomerulonephritis. Methods for preparing them are soft-boiled (cook for 3 minutes) and in a bag. With the latter option, simply break the eggs into boiling salted water and cook covered for 2 minutes. If you want to cook scrambled eggs, you just need to break the eggs into a container and place it in a bowl of boiling water. After some time, the mass will curl up and turn into scrambled eggs.
During lunch, dairy, vegetable, cereal, and potato soups (vegetarian options) are served as the first course. The second dish can be stewed potatoes, vegetable purees, cereal casseroles, cabbage rolls. For dessert they eat fruits, and for drinks they drink compotes, juices, and jelly. An afternoon snack for glomerulonephritis is a small snack. You can satisfy your hunger with fruit, juice, milk, kefir, and baked apples. For dinner, they boil potatoes, make casseroles, bake pancakes, buns, and cheesecakes.
Treatment of the disease
Therapy is prescribed by a doctor after testing for glomerulonephritis and identifying the form of the disease. In acute cases, the sick person is sent to a hospital, prescribed bed rest and a special diet. In hospital, treatment sometimes takes quite a long time. With a mild form, people have to stay in bed for 2 to 4 weeks, and with more severe forms, for several months.
In treatment, doctors sometimes use an etiological approach, that is, they prescribe drugs that should eliminate the cause of the disease:
- for nephritis associated with subacute infective endocarditis and for post-streptococcal nephritis, antibiotics are prescribed;
- for virus-associated glomerulonephritis, antiviral drugs, etc. are indicated.
However, the etiological approach cannot be applied in all cases. Most often, it is necessary to begin therapy with pathogenetic treatment aimed at certain pathogenesis processes (inflammation, immune processes). One of the groups of drugs related to pathogenetic treatment is glucocorticoids. They have anti-inflammatory and immunosuppressive effects.
General analysis
This analysis is prescribed to monitor the body’s vital functions and identify problems in the initial stages of the disease. Failure of the kidneys is determined by changes in the amount, color and composition of urine. The violations identified during the study of this analysis give rise to more extensive research. In the normal state of the kidneys, there is no protein, red blood cells, ketone bodies, hemoglobin, or bilirubin in urine. And urine with glomerulonephritis shows proteinuria (increased protein content) from 1 g/l to 10 g/l, hematuria (presence of red blood cells) from 5 to 15 red blood cells in the field of view and an increase in specific gravity to 1030 - 1040. Normal indicators and possible changes can be see in the table:
| Indicators | Norm | Changes |
| Urine color | Straw, yellow | From dark yellow to red-brown |
| Transparency | Full | Incomplete |
| Specific gravity | 1018 in the afternoon | 1025 — 1040 |
| Protein | Less than 0.002 g/l | 1 g/l – 10 g/l |
| Cylinders | Single hyaline | Granular and hyaline more than 20 in p/zr |
| Epithelium | 1 -5 units | More than 10 units |
| Glucose | Not found | _ |
| Bilirubin | Absent | In stock |
| Red blood cells | 0 — 3 | More than normal |
| Leukocytes | 0 — 6 | More than normal |
All tests for glomerulonephritis indicate changes in the functioning of the glomerular apparatus of the kidneys, damage to capillary membranes and, as a consequence, impaired filtration. Laboratory studies can also provide insight into the etiology of the disease and opportunities for differential diagnosis.
Rehberg's test
For acute glomerulonephritis, the Rehberg test is prescribed. This study requires donating blood and 24-hour urine. All blood in the body is filtered in the kidneys. Some substances are absorbed completely, some partially, but there is a substance that is completely eliminated from the body after filtration - this is creatine. To assess the functioning of the glomerular apparatus of the kidneys and identify disorders, it is necessary to examine the amount of this substance in the blood and then in the excreted urine, thus the glomerular filtration rate can be calculated.
Blood is always donated in the morning on an empty stomach. Urine is usually collected starting at 6 a.m. throughout the day. The examination takes into account the amount of urine and creatine concentration. The glomerular filtration rate for a healthy man is 88-146 ml/min; for a woman it is 81-134 ml/min; a decrease in this indicator indicates damage to the glomerular apparatus of the paired organ. The main thing in this method is to take into account the start time of urine collection, as well as the height, weight and age of the person.
Zimnitsky test
To study the ability of the kidneys to concentrate secreted fluid, the Zimnitsky test is used. This test does not diagnose specific diseases; it evaluates kidney function. The normal functioning of the paired organ is characterized by the specific gravity of urine, which expresses the ability of the kidneys to secrete or retain water. Specific gravity is the weight of a solution relative to the weight of water. This indicator is influenced by the amount of waste (urea, glucose, protein and creatine) excreted by the kidneys along with the fluid after filtration.
The material for the study is collected every 3 hours for 24 hours to make 8 servings, and it is necessary to reduce the amount of liquid consumed to 1-1.5 liters. The time of collection must be written on all portions and stored in a cool place. When examining the obtained material, the amount of liquid drunk is taken into account and the specific gravity of urine is determined. Normally, diuresis during the day is greater than at night. The density should be less than the density of blood plasma and be 1005-1025 during the day and 1035 at night. In acute glomerulonephritis, the density increases to 1040 and the amount of fluid released relative to the ingested decreases.
Nechiporenko's technique
This is the most common method for examining urine; it studies the microscopy of the composition of the sediment. It is prescribed, like other studies, to clarify the identified deviations in the general analysis. The sediment is examined for the presence of red blood cells, casts and leukocytes. An average portion of morning urine is taken, after a thorough toilet, in the amount of 120-00 ml. It is important to deliver the test material to the laboratory within 1.5 hours. Using a centrifuge, the precipitate is separated, 1 ml of material is taken and its composition is studied in a special chamber.
In a healthy person, per 1 ml of sediment, the analysis will show leukocytes up to 2000, hyaline casts up to 20, red blood cells up to 1000. Completely different indicators will be in case of kidney dysfunction. Red blood cells in the urine with glomerulonephritis predominate over leukocytes and contain more than 20 hyaline and granular casts. Urine tests according to Nechiporenko are taken continuously throughout the entire period of the disease, so that changes in the clinical picture of the disease can be observed and treatment can be adjusted.
Prognosis for glomerulonephritis
The outcome of the disease depends on several factors - the morphological variant of glomerulonephritis, the frequency of exacerbations, and the development of chronic renal failure. In the acute form, the prognosis is favorable. However, it is worth remembering that only with treatment does recovery occur. Incorrect, untimely or completely absent therapy increases the likelihood of progression of the disease and the transition of the acute version to chronic.
With chronic glomerulonephritis, everything is much more complicated. The prognosis depends on the types of this disease. In the latent form of chronic glomerulonephritis, the prognosis is favorable, in the hypertensive form it is serious, and in the mixed form it is unfavorable.
What are the causes of acute glomerulonephritis
All causes of the disease can be divided into three groups:
- infectious;
- non-infectious;
- genetic.
The main cause of acute glomerulonephritis is streptococcal infection. This pathogenic microorganism, which first causes diseases of the respiratory tract, leads to damage to kidney tissue. Non-infectious causes include the body's reaction to exposure to poisons, toxins, chemicals or medications. By and large, any intoxication can cause damage to kidney tissue. At the same time, the body's immune reactions are activated.
Factors provoking non-infectious immune glomerulonephritis:
- vaccinations;
- individual intolerance to drugs and chemicals;
- alcohol abuse;
- insect bites;
- exposure to plant pollen.
With a genetic predisposition, usually more than one person in the family is sick, and most often, in all patients, acute and chronic glomerulonephritis begins at approximately the same age.
Preventive measures
Prevention of acute glomerulonephritis includes prevention and early treatment of acute infectious diseases, elimination of focal infection. Experts recommend that people harden the body, avoid prolonged and sudden hypothermia, and not work in jobs that involve exposure to cold conditions or physical stress. After treatment, you should not plan a pregnancy for the next 3 years. It is advisable to periodically undergo medical examinations, have your urine tested, and monitor your blood pressure.
To prevent chronic glomerulonephritis, similar preventive measures have been established. Need to
- promptly eliminate foci of infection in the body;
- treat intestinal infections;
- avoid hypothermia and exposure to humid air;
- be under medical supervision;
- do not go on long business trips, do not get a job with night shifts, do not be exposed to harmful substances;
- regularly go to sanatorium-resort treatment;
- Healthy food;
- to refuse from bad habits.
In general, you should lead a healthy lifestyle.
In conclusion, it is worth noting that you need to be more attentive to your body, value your health and life. Only with this approach, as well as with timely consultation with a doctor and compliance with his clinical recommendations, can glomerulonephritis be avoided, like any other disease.
Symptoms requiring immediate investigation.
Many patients are faced with the fact that it is much easier to cure a disease in the early stages than in an advanced state. Unfortunately, not everyone listens carefully to their body, to the signals it sends long before the active phase of the disease.
You should contact your doctor immediately if:
- In the morning on the face, and in the evening in the ankle joint, stable swelling is observed;
- the volume of fluid excreted is much less than that consumed;
- urination becomes less frequent;
- the shade of urine changes to darker than before;
- the temperature rises to subfibrile, and later increases;
- appetite and sleep are disturbed;
- thirst becomes unbearable;
- body weight changes dramatically without a special diet;
- breathing problems appear in a calm state;
- Pain in the lumbar region appears periodically.