Pyelonephritis is based on an infectious lesion of the pelvis and calyces of the kidney, as well as its parenchyma. Most often it is caused by pathogenic bacteria that enter the body from the outside. This is one of the most common inflammatory diseases and the most common among various kidney pathologies. Moreover, very often pyelonephritis disguises its symptoms as other diseases, which significantly complicates treatment, which is already quite difficult.
But each of us may encounter pyelonephritis in our lives. And in order to suspect the onset of the disease in time and begin effective treatment, you need to know what it is and how it usually manifests itself. We will talk about this and much more in this article.
Classification and causes of pyelonephritis
There are chronic and acute, unilateral and bilateral, primary and secondary forms of pyelonephritis. Moreover, secondary pyelonephritis is noticeably more common (in 80% of cases), which develops as a result of functional and organic changes in the urinary tract and the kidneys themselves, leading to problems with the outflow of urine, lymph and venous blood from the kidney.
In children, the disease is most often associated with congenital dysplastic foci in the renal tissues and microobstruction (obstructed urine outflow) at the nephron level. The disease is often observed in pregnant women (gestational pyelonephritis). This is explained by the fact that in most expectant mothers the tone of the upper urinary tract decreases. Such processes are caused by both endocrine (hormonal changes) and enlargement of the uterus during pregnancy.
Typical causative agents of pyelonephritis are white and aureus staphylococci. They are the ones who can provoke the onset of the disease in a completely healthy person without any reason.
Other microorganisms cause pyelonephritis only in the presence of certain local factors.
conclusions
In conclusion, it is worth saying that pyelonephritis is a rather complex disease. Its clinical picture can vary greatly depending on the individual characteristics of each person’s body. There is also a risk of confusing pyelonephritis with other pathologies of the kidneys or other organs of the urinary system. For example, a person without medical education is not able to perform a differential diagnosis of acute glomerulonephritis and pyelonephritis.
For this reason, you should not engage in amateur activities. A nephrologist knows everything about acute and chronic pyelonephritis, etiology, pathogenesis, clinical picture, diagnosis, treatment. This is the specialist you should trust with your health.
If there is a suspicion of chronic or acute pyelonephritis, children should be examined by a pediatrician.
Share:
Chronic pyelonephritis
Complaints
All complaints of patients with pyelonephritis can be divided into two main groups: specific and general.
So, common complaints include:
- Headache;
- Decreased appetite;
- Poor sleep;
- Decreased performance;
- Weakness.
Specific complaints:
- Aching pain in the lower back (usually one-sided). In the painful form of pyelonephritis, they can be quite intense. In addition, pain often radiates to the lower abdomen, thigh or genitals;
- Dysuric phenomena (for example, frequent urination associated with cystitis);
- Discharge of rather cloudy urine, which often has an unpleasant odor;
- Chilling (during an exacerbation) with periodic rises in temperature up to 39 degrees. As a rule, it returns to normal by morning.
Remember! Never hide your complaints from your doctor. After all, every little detail can be important when making a final diagnosis and prescribing subsequent effective treatment.
Inspection
The next point that the doctor also focuses his attention on is examining the patient. So, signs of pyelonephritis that appear during examination:
- Paleness of visible mucous membranes and skin;
- Reduced body weight (not always);
- Facial pastiness. Severe swelling is extremely rare;
- Pain when tapping and palpating the lumbar region (can be both unilateral and bilateral);
- Tofilo's symptom - lying on his back, the patient bends his legs and presses them to his stomach.
Examination of internal organs
Chronic pyelonephritis is characterized by the following:
- Arterial hypertension;
- Expansion of the left borders of the heart;
- Muffled heart sounds;
- Functional liver disorders;
- Reduced secretion of gastric juice.
Doctors often note pronounced psychasthenic and neurasthenic personalities of the patient. In addition, if the disease is left without proper treatment, it gradually develops into chronic renal failure.
Affected kidney
The first signs of problems with the functional state of the kidneys are:
- Polyuria (daily urine volume more than 2 liters);
- Nocturia (night diuresis prevails over daytime diuresis);
- Dry mouth;
- Thirst;
- Decreased urine density.
It should be noted that chronic renal failure, which occurs against the background of pyelonephritis, often has a recurrent nature. This is largely due to inflammatory processes in the interstitium of the kidney.
Important! Chronic pyelonephritis in diabetes mellitus and in pregnant women can be extremely severe, often with the presence of papillary necrosis. In such cases, there is severe chills, a rise in temperature up to 40 degrees, a sharp deterioration in the general condition, leukocytosis, pyuria, as well as cutting pain in the lower abdomen and lower back.
Clinical forms of chronic pyelonephritis
Today, all practicing doctors prefer to distinguish several clinical forms of CP. Their presence greatly facilitates the diagnosis of this disease.
Latent form
Characterized by mild symptoms. Often patients are bothered by unmotivated weakness, nocturia, chills, and mild pain in the lumbar region (it is often described as a manifestation of spinal osteochondrosis). Such vague and vague symptoms create many problems for diagnosing the disease. In such cases, the doctor needs to carry out OAM, the Nechiporenko test and bacterial urine culture as often as possible. This form is detected mainly by ultrasound.
Recurrent form
It represents alternating periods of remissions and exacerbations of pyelonephritis. So, in the second case, the clinical picture is quite clearly visible and almost always specific symptoms and changes in laboratory data are detected. Sometimes this form is confused with acute pyelonephritis, but a thorough study of the disease history helps to establish the correct diagnosis. During exacerbations, rapid development of chronic renal failure is possible. With timely relief of relapse, clinical and laboratory parameters gradually return to normal.
Hypertensive form
With this course, arterial hypertension syndrome comes to the fore. In this case, urinary syndrome is observed quite rarely or is mildly expressed.
Important! If a person has hypertension, it is always necessary to exclude CP as its main cause.
Anemic form
In this situation, the clinical picture will be dominated by anemia, which is usually caused by impaired production of erythropoietin (the hormone responsible for the formation of red blood cells) and severe intoxication. As a rule, severe anemia appears with pyelonephritis only in combination with chronic renal failure. In this case, minor and inconsistent changes in the urine are observed.
Septic form
This form develops with severe exacerbation of CP. It is accompanied by high body temperature levels, severe chills, hyperleukocytosis, severe intoxication and bacteremia. It is quite easy to recognize the septic form of pyelonephritis, since in such cases there are clear clinical and laboratory symptoms.
Hematuric form
It is extremely rare. It is characterized by gross hematuria. When diagnosing “hematuric form of chronic pyelonephritis,” the doctor must carry out a differential diagnosis with the following diseases: malignant tumors or tuberculosis of the bladder, kidneys, hemorrhagic diathesis, urolithiasis, nephroptosis.
Diagnostic methods
Historically, the main object of study for kidney disease has been urine. Ancient Greek and ancient Indian doctors, even before our era, were able to make diagnoses based on its color, transparency, smell and even taste. Today, urine is subjected to numerous manipulations using the most modern devices - centrifuges, spectrometers, gas analyzers and microscopes.
Urine tests
Patients' urine is subjected to the following types of analysis:
- Bacteriological - under a microscope and using specific reactions, the quantitative and qualitative composition of a biological fluid is determined. Urine itself has antiseptic properties and therefore in healthy people it is practically sterile. If there is an inflammatory process in the kidneys or bladder, there are so many bacteria in the urine that not all die. Pathology is considered to be the presence of 100 thousand bacterial cells in 1 ml.
- Chemical. There is a norm for the content of proteins, carbohydrates, and salts in the urine. A sign of inflammatory and other pathological processes is albuminuria - excess proteins, crystalluria - excess salts and some other conditions. All of them are detected by chemical analysis of urine. Another important task of chemical analysis is determining the pH reaction of urine. This is important when prescribing treatment. Thus, aminoglycoside antibiotics effectively destroy bacteria in an alkaline environment, but are destroyed very quickly in an acidic environment. When prescribing aminoglycosides, it is important to know the acidity of urine and, if necessary, alkalize it with the help of special medications and diet.
- Clinical analysis. It is designed to determine the content of specific and nonspecific cells and particles in the urine that are formed during the inflammatory process. The content of leukocytes, phagocytes, epithelial cells and pieces of exfoliated epithelium in the urine is calculated. The more acute the inflammatory process in the kidneys, the cloudier the urine and the more foreign inclusions it contains. To determine the level of leukocyturia, the so-called Nechiporenko test is used. Another popular test is the Zimnitsky urine test.
The so-called three-glass urine sample is considered optimal. When urinating, the patient divides the biological fluid into three doses. This allows you to get the most objective picture. Unfortunately, such a test is almost impossible to obtain in young children. Sometimes difficulties with urination occur in older people. If urinary tract obstruction occurs during pyelonephritis, difficulties with dividing urine into portions are also possible.
As an alternative technique, the Litos system, proposed in the early 90s of the last century by Russian scientists Professor Shatokhina and Academician Shabalin, is becoming increasingly popular. The essence of the method is to study not liquid urine, but a dried (dehydrated) drop, which is called facies. The evaporation of the liquid takes about a day, after which a preparation appears on laboratory glass in which all the solid components are amazingly structured in accordance with the osmotic properties of the components. Proteins go to proteins, salts to salts, bacterial cells to bacterial cells. The authors “spied” this process in geology - this is how the deposition of rock layers in the lithosphere occurs. Hence the name of the technique.
More information about the method can be found in the video recorded by its co-author, Doctor of Medical Sciences Svetlana Shatokhina:
Cultural analysis
In addition to the usual one-time bacterial examination of urine under a microscope, cultural diagnostics extended over time are possible. The sample is placed in nutrient media that are optimal for the development of various bacteria and it is observed whether the colony will germinate or not. If a colony, for example, of Pseudomonas aeruginosa, develops quickly, staining the preparation with a characteristic blue-green color, then this bacterium took an active part in the occurrence of pyelonephritis. This technique does not allow determining the pathogen with absolute accuracy, since potential pathogens may be present in the urine by chance, but the analysis guarantees an 80% probability. Its disadvantages are the length of time (the growth of a microbial colony takes up to a week) and strict sanitary and epidemiological rules - samples must be stored in specially equipped rooms without the access of outsiders. Proper laboratory conditions are available only in large medical institutions.
Serological study
A modern type of diagnosis is serological testing of biomaterials. Most often it is carried out as part of a biochemical blood test. The task is to detect the presence of specific antibodies to certain pathogenic antigens. If antibodies to streptococcus pyogenes are found in the blood, and streptococci themselves are found in the urine, then they are definitely involved in the occurrence of pyelonephritis and it is necessary to immediately prescribe drugs that will ensure the destruction of uninvited guests. Pyogenic beta-hemolytic streptococcus most often enters the kidneys from the tonsils during tonsillitis and scarlet fever. There is no need to talk about its harmfulness - as is known, it not only causes purulent inflammation in various organs, but also provokes autoimmune rheumatic reactions.
Urinary tract infection
“Industry sponsors have no obligation to serve public health. They have a duty to the shareholders and the right to pay for the tests of their choice” B. Psaty, N. Weiss, C. Furberg
CLASSIFICATION OF URINARY TRACT INFECTION
• Etiology: Escherichia coli, Proteus, Klebsiella, Enterobacter, Pseudomonas, Staphylococci. • Localization: cystitis, pyelonephritis, urethritis, urosepsis. In men: prostatitis, epididymitis, orchitis. • Settings: nosocomial (catheter), community-acquired. • Relapses: recurrent infection (same strain [infected stone or calyx cyst, chronic prostatitis, duplication of the ureter]), repeated infection (different strain [contamination of intestinal flora]).
Escherichia coli
Escherichia coli is the main causative agent (80%) of urinary tract infections.
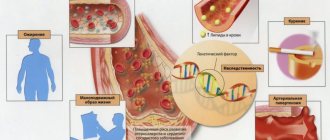
RISK FACTORS
• Women. • Sex life. • Pregnancy. • Urinary tract obstruction. • Neurogenic bladder dysfunction.
• Vesicoureteral reflux.
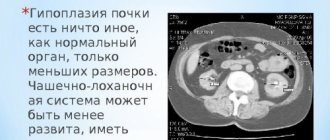
STAGES OF REFLUX NEPHROPATHY
Stage I: reflux into the ureters. Stage II: reflux into the pelvis and calyces. Stage III: mild dilatation of the urethra and pelvis. Stage IV: moderate dilatation of the urethra, pelvis and calyces; obliteration of sharp corners of the arches.
Stage V: pronounced dilatation of the urethra (+ tortuosity), pelvis, calyces; There are no papillae in most calyxes.
Leukocyturia
LABORATORY DIAGNOSTICS
• Urinalysis: pyuria (>10 in the field of view of centrifuged urine, x400). Affected by leukopenia and hydration. • Leukocyte esterase test strip (sensitivity 80–90%, specificity 95–98%). • Rapid test for bacteriuria: nitrite test. • Urine culture: bacteriuria without symptoms is not sufficient for diagnosis (contamination, asymptomatic bacteriuria). • Analysis for chlamydia, gonococci. • General blood analysis. • Blood test: creatinine, eGFR. • Blood culture. • Sonography of the kidneys (urinary tract obstruction, abscess), prostate. • Computed tomography with contrast (renal ischemia).
• Scintigraphy with 99Tcm (renal ischemia).
• Excretory urography.
• Cystoscopy.
Test strips
URINE CULTURE
Indications (EUA) • Suspected acute pyelonephritis. • Symptoms persist or recur 2–4 weeks after the end of treatment. • Women with atypical symptoms.
Criteria for bacteriuria
• Cystitis: ≥103/ml. • Pyelonephritis: ≥104/ml • Complicated infection, men: ≥105/ml.
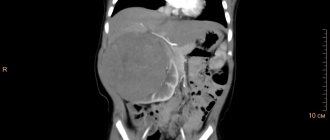
Obstructive pyelonephritis with abscess
Prieto-Gonzalez S, Alemany M. New Engl J Med. 2014;371:1332.
CLINIC
• Acute cystitis: painful frequent urination, urgency, pain above the pubis. • Acute urethritis: painful frequent urination, urgency. • Acute pyelonephritis: fever >38°C, nausea, vomiting, pain on tapping and deep palpation in the costovertebral angle, tubulointerstitial syndrome (low urine density). • Chronic pyelonephritis: relapses due to urodynamic disorders, nephrosclerosis, arterial hypertension, wrinkled kidney, CKD.
Emphysematous pyelonephritis
FORMULATION OF DIAGNOSIS
Ds: Chronic pyelonephritis, exacerbation, CKD stage 2. [N11.8]
Ds: Acute right-sided pyelonephritis, paranephritis on the right. [N10]
Ds: Acute cystitis. [N30.0].
TREATMENT (EUA)
Uncomplicated cystitis • Fosfomycin 3 g 1 time per os, 1 day. • Nitrofurantoin (furadonin) 100 mg 2 times per os, 5 days. • Pivmecillinam 400 mg 3 times per os, 3–5 days. • Cefpodoxime 200 mg 2 times per os, 3 days.
Uncomplicated pyelonephritis
Outpatient. • Ciprofloxacin 500–750 mg 2 times per os, 7–10 days. • Levofloxacin 750 mg 1 time per os, 5 days. • Ceftibuten 400 mg 1 time per os, 10 days. • Cefpodoxime 200 mg 2 times per os, 10 days.
Hospital, parenterally until improvement, then 7–10 days per os. In men, fluoroquinolones, up to 14 days.
• Ciprofloxacin 400 mg IV 2 times. • Levofloxacin 750 mg IV once. • Ceftriaxone 1–2 g IV once. • Cefepime 1–2 g IV 2 times. • Imipenem/cilastatin 500/500 mg IV 3 times. • Ertapenem 1 g IV once.
Complicated urinary tract infection
• Treatment 7–14 days. • Amoxicillin/clavulanate 1500 mg IV 3 times + aminoglycoside (gentamicin 5 mg/kg IV or amikacin 15 mg/kg IV 1 time). • Cefotaxime 2 g IV 3 times. • Ceftriaxone 1–2 g IV once. • Cefiderocol.
Acute bacterial prostatitis
• Treatment until improvement, then fluoroquinolones for 2–4 weeks per os. • Ciprofloxacin 500 mg IV 2 times + aminoglycoside (gentamicin 5 mg/kg IV or amikacin 15 mg/kg IV 1 time). • Levofloxacin 500 mg IV 2 times + aminoglycoside. • Ceftriaxone 2 g IV 1 time + aminoglycoside. • Cefepime 2 g IV 2 times + aminoglycoside.
• Piperacillin/tazobactam 4.5 g 3 times + aminoglycoside.
TREATMENT OF ASYMPTOMIC BACTERIURIA (EUA)
Indicated: • Pregnant women, • urological interventions with a risk of bleeding of the mucous membrane.
Not shown
• Elderly, • diabetes, • bladder catheter, • kidney transplant recipients after 6 months, • spinal cord injury,
• candiduria.
PREVENTION FOR FREQUENT RECURRENCE (EUA)
• General hygiene measures. • Cranberry preparations (juice) daily (effect not proven, Cochrane Review). • Drink plenty of fluids (Hooton T et al, 2018). • Postcoital administration (contacts less than once a week, pregnant women): nitrofurantoin 50–100 mg, cephalexin 250 mg. • Daily at night: nitrofurantoin 50–100 mg, cephalexin 125–250 mg, cefaclor 250 mg, fosfomycin 3 g every 10 days.
• An indwelling bladder catheter (Foley) is 100% colonic after 2 weeks with microbes (bacteria, Candida [common in the ICU]), but antibiotics are not indicated in the absence of symptoms.
GENERAL HYGIENIC EVENTS FOR WOMEN
• Prefer liquid soap, shower (not bath). • Wash the urethral area first. • Wipe from front to back, once. • 1 towel for the urethral area, sterilization of towels. • Do not use hygiene products in the genital area. • Tampons instead of pads. • Reduce the intervals between urination (
Source: https://therapy.irkutsk.ru/edinf.htm