General information
Urachal cyst is a urological pathology, which is 2 times more often registered in newborn boys.
This embryonic defect accounts for 42% of all developmental anomalies of the urinary canal. About a third of people at birth have one or another pathology of the urachus, which is not always detected during life, but is confirmed by the results of autopsies. In adults, the tumor is more often diagnosed incidentally during imaging studies or during surgery. The clinic develops with complications: perforation of the cyst, formation of a fistula, infection. In women, the pathology is rare; sometimes symptoms manifest during pregnancy as the fetus grows.
Urachal cyst
What methods are used to detect the disease?
At the first signs, you should contact a urologist. Women first need to visit a gynecologist to rule out pathologies of the reproductive system.
During diagnosis, the doctor listens to the patient’s complaints and then conducts research. These include:
- General urine analysis. Almost always, when a cyst appears, it contains bacteria, leukocytes, salts, red blood cells and protein.
- General blood analysis. Helps to see the inflammatory response. With frequent bleeding, anemia may develop.
- Ultrasound of the bladder. The shape of the bladder and kidneys can reveal the presence of cysts, stones, and pathologies.
- Cystoscopy. Helps to see the cyst from the inside. To do this, the endoscope is inserted through the urinary canal into the bladder.
Cystography and fistulography are also used. But since most patients present in emergencies, there is little time for diagnosis.
Bladder cyst: causes of development, diagnosis and treatment
Bladder cysts are rare in the practice of urologists; according to various statistical estimates, the percentage of situations varies from 1.5 to 3%. The likelihood of developing a pathological process increases significantly against the background of long-term or often recurrent diseases of the genitourinary system of an infectious, less often autoimmune nature.
In some cases, the likelihood of developing such a process is determined by congenital anomalies in the development of anatomical structures. Often, people confuse other formations with a bladder cyst.
Definition
A bladder cyst is a non-tumorous mass formation.
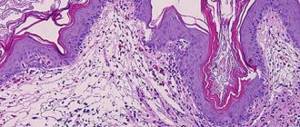
It differs from a tumor in its non-solid structure, lack of tendency to proliferation and growth due to cell division (if a cyst grows, it is due to stretching of the capsule and increasing the volume of the liquid component inside), and lack of ability to germinate tissue. It is possible to differentiate a cyst from a tumor only based on the results of tomography or biopsy with further histological examination.
Symptoms are not always present. In most cases, patients do not even know that something is wrong with them and that there is pathology. Diagnosis is not difficult. Treatment is surgical, if necessary. But it is required relatively rarely.
Causes
Bladder cysts develop in women much more often when compared with the process in men. This is believed to be due to an increased tendency to genitourinary infections, especially inflammation of the bladder itself. A cyst in the bladder in men is rare and does not manifest itself for a long time. There are no fundamental differences, other than the occurrence, either in the causes or in the clinical picture.
The reasons for the development of bladder cysts are poorly known; the question is still open and being studied by the medical community. The following factors are believed to increase the risk or directly cause the onset of the pathological process:
- Acute inflammatory process in the bladder. The so-called cystic cystitis of the bladder. Provokes the development of non-tumor space-occupying formations. In the same way, frequent relapses of chronic pathology affect the state of the excretory system. Much less often, a similar result is found with prolonged existence of an autoimmune form of inflammation.
- Urolithiasis, “sand” in the bladder. The factor is approximately the same. The walls of a hollow organ are constantly irritated when in contact with small concretions (stones), which, in fact, is what is called sand. There is no such term in medical practice; this is nephrolithiasis, albeit in the early stages. Without treatment, if this situation exists for a long time, the risk of developing tumors increases. Not only cysts, but also full-fledged tumors. Benign and malignant.
- Bladder surgeries performed. Rare reason. Several factors must coincide for such a violation to occur. The question is that most patients, as statistics show, already suffered from inflammatory diseases of the bladder even before surgery. What causes it: the operation itself or the current condition even before this is a controversial issue.
- Bladder catheterization. The same thing that was said about the operation is true here.
- Belonging to the female gender. The issue is highly controversial. Usually we are talking about a more frequent development of genitourinary infections, primarily cystitis, which affects the likelihood.
- Congenital anomalies of the development of the genitourinary apparatus.
In most cases, it is not possible to establish the exact cause of the pathological process. Fortunately, this is almost never required when it comes to a specific patient. Cysts do not recur; after treatment, the problem completely resolves itself. However, in terms of prevention as such, the issue plays a huge role.
A bladder cyst itself almost never produces symptoms. Especially considering the fact that the dimensions of the volumetric formation are small and rarely the volumetric structure reaches more than 1 cm in diameter. At large sizes, the manifestations become obvious.
In other situations, manifestations of the underlying pathological process that accompanies the cyst are detected. Accordingly, clinical signs can be divided into two groups.
The first are the actual manifestations of the cyst.
- Aching or nagging pain in the groin, lower abdomen, pubic area. They accompany the patient for a long time, but are not constant. Episodic. Intensity: minimal or medium. The reason is the pressure on the bladder wall and surrounding structures. As they grow, the symptoms intensify, the pain becomes stronger and significantly reduces the person’s quality of life.
- Feeling of pressure in the groin area.
- Frequent false urge to empty the bladder. They occur even against the background of complete imaginary well-being, if there are no other symptoms. Usually there is no pain during the emptying of the hollow organ itself, which is typical for infectious processes. Urine is not excreted at all or comes out in small portions: a thin stream or drops.
There are no other symptoms. Those that exist are non-specific, which does not allow a diagnosis to be made quickly, without special studies, and sometimes does not motivate a person to see a doctor.
The second group of symptoms are signs of concomitant pathologies. Among them:
- Intense pain in the groin, lower back, pubic area, perineum. Much stronger than in the isolated course of a cystic lesion. It provokes attacks, spasms, and is painful to bear, so patients tend to see a doctor or take painkillers, which blurs the clinic and complicates diagnosis. The cause of intense pain is cystitis or cystic cystitis. The second is more aggressive and often recurs.
- Burning while emptying the bladder. Corresponds to a genitourinary infection, usually cystitis, provoked by pyogenic flora (staphylococci, streptococci), E. coli and other agents.
- Frequent false urge to visit the toilet. As in the previous case. We are talking about pollakiuria. The pathological process is painful to bear, the urge does not stop even at night, the daily volume of urine is normal, which makes it possible to exclude kidney problems.
- Increase in body temperature. Not always. If present, then at a level of up to 39-40 degrees Celsius.
- Symptoms of general intoxication of the body. Weakness, asthenic phenomena, nausea, rarely vomiting, drowsiness, feeling of weakness, decreased performance, apathy, headaches, dizziness.
Symptoms of the underlying disease do not last forever. They occur periodically, just during an exacerbation of cystitis. The approximate duration of the disease (episode) is about 10-14 days, rarely more. Prolonged relapses are also possible. With treatment, the time frame is reduced to 4-8 days or less.
Symptoms of bladder cysts in women are more pronounced, but the overall course of the disease is shorter; in the stronger sex, the duration of relapse is longer, by several days. There is a tendency to long-term, sluggish variants, when the disease does not completely go away at all, it only subsides.
In most cases, the cyst does not manifest itself in any way. In the absence of sufficient qualifications, the urologist will not suspect a problem and will not refer the patient for examination. In such a situation, the problem can persist for years, gradually, progressing or standing still, depending on the case.
Diagnostics
Examination of patients with bladder cysts does not present any problems. A few methods are enough.
- It all starts with an oral questioning of the patient regarding complaints and collecting an anamnesis. It is worth finding out all the significant factors. Complaints are objectified and put together into a single clinical picture. This is the basis of diagnosis, determining its vector.
- General urine examination. Laboratory assessment of urine allows us to identify inflammatory processes. But it does not answer what kind they are, why they arose, and at what stage they are. Therefore, assessment is necessary in the system. Analysis alone is not enough.
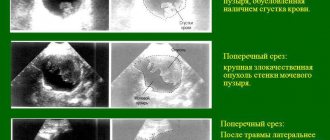
- Ultrasound of the bladder. Requires some preparation. With the right approach, it allows you to visualize formations. It is impossible to give exact data on what its origin is, whether it is a tumor. The essence of the study is to establish the fact of the presence of a certain neoplasm of an unclear nature.
- MRI of the bladder. The main study in the framework of identifying neoplastic and tumor processes. As part of the diagnosis, contrast enhancement is used. A gadolinium-based drug is administered intravenously. Particles of the contrast agent accumulate in the changed tissues and enhance the pattern, allowing the doctor to assess the structure, size, shape, expected type, metabolic activity, and degree of blood supply of the space-occupying formation. A typical feature of a classic bladder cyst is that it does not accumulate contrast at all. What makes it different from tumors? With a non-standard structure, accumulation of the substance in the capsule is possible. The same applies to the situation if the formation has a mixed, solid-cystic structure, but this is a completely different question.
If a controversial formation accumulating contrast is detected, a biopsy is performed. Targeted puncture of the bladder, the cyst itself, sampling of a piece of tissue (or even several), and, if necessary, the contents of the cyst.
Then, through a morphological examination and histological assessment, doctors give an answer to what exactly they are dealing with. Based on the results of laboratory evaluation, we can talk about one or another therapy method.
Treatment
Treatment mainly consists of dynamic observation. Strictly speaking, this is not therapy, but waiting. Watchful waiting is indicated in most cases.
A typical cyst practically does not grow, does not create discomfort for the patient, there is no dynamics, and therefore the issue of treatment becomes irrelevant. Assessment of the size and other physical characteristics of the tumor is carried out using MRI and/or ultrasound. It is recommended to conduct research every six months to a year, depending on the case.
If there is continued growth or, against the background of a cyst, inflammatory processes develop (which is relatively rare, the cause-and-effect relationship is not obvious), surgical treatment is required. It is carried out by two main methods.
- The first is puncture of the cyst and drainage of the cavity using a special catheter. Doesn't make much sense. Despite the minimal invasiveness, there is a high probability that the cyst will fill with contents again and everything will return to normal. The capsule is not going anywhere.
- It makes sense to carry out a total excision of the structure. Endoscopic surgery is performed by inserting instruments through small skin incisions. This is a somewhat more traumatic technique, after which some period of rehabilitation is required, but the absence of relapse in the future is guaranteed. A total excision of the cyst is performed, removing the capsule and its contents.
Diagnostics
Examination of patients with bladder cysts does not present any problems. A few methods are enough.
- It all starts with an oral questioning of the patient regarding complaints and collecting an anamnesis. It is worth finding out all the significant factors. Complaints are objectified and put together into a single clinical picture. This is the basis of diagnosis, determining its vector.
- General urine examination. Laboratory assessment of urine allows us to identify inflammatory processes. But it does not answer what kind they are, why they arose, and at what stage they are. Therefore, assessment is necessary in the system. Analysis alone is not enough.
- Ultrasound of the bladder. Requires some preparation. With the right approach, it allows you to visualize formations. It is impossible to give exact data on what its origin is, whether it is a tumor. The essence of the study is to establish the fact of the presence of a certain neoplasm of an unclear nature.
- MRI of the bladder. The main study in the framework of identifying neoplastic and tumor processes. As part of the diagnosis, contrast enhancement is used. A gadolinium-based drug is administered intravenously. Particles of the contrast agent accumulate in the changed tissues and enhance the pattern, allowing the doctor to assess the structure, size, shape, expected type, metabolic activity, and degree of blood supply of the space-occupying formation. A typical feature of a classic bladder cyst is that it does not accumulate contrast at all. What makes it different from tumors? With a non-standard structure, accumulation of the substance in the capsule is possible. The same applies to the situation if the formation has a mixed, solid-cystic structure, but this is a completely different question.
If a controversial formation accumulating contrast is detected, a biopsy is performed. Targeted puncture of the bladder, the cyst itself, sampling of a piece of tissue (or even several), and, if necessary, the contents of the cyst. Then, through a morphological examination and histological assessment, doctors give an answer to what exactly they are dealing with. Based on the results of laboratory evaluation, we can talk about one or another therapy method.
Pathogenesis
The role of the urachus is to divert fetal urine into the amniotic fluid during embryogenesis. This duct is a derivative of the allantois stalk and is formed by 2-3 months of pregnancy. The closure of the urachus begins in the fifth month of gestation. By the time of birth, the embryonic canal normally closes completely in most children, transforming into the median vesico-umbilical ligament.
With the development of ultrasound diagnostics, it has been discovered that a small hole in the rudimentary process can persist in healthy children. The opinion of practitioners is divided - this is a pathology or a variant of the norm. A urachal cyst is formed due to non-obliteration of the duct in the middle part and can persist throughout life. The epithelium of the canal in adults produces fluid, which promotes the growth of the cyst; in children, the cystic cavity may also contain mucus, meconium masses, and urine. There are observations when fusion of the embryonic duct occurred independently by 1.5 years of age.
Why do cysts occur?
Human organs are formed in the womb. In the bladder, the duct plays an important role until the age of five months. Its function is that it connects the urea with the amniotic fluid. Afterwards changes occur in it, it closes. If only the ends of the duct are closed, leaving space in the middle part, this can become a catalyst for a cyst.
The tumor fills with mucus, feces and urine, and can remain like this for quite a long time without showing symptoms.
Symptoms of a urachus cyst
Neoplasms of the bladder and related organs are asymptomatic in most cases. Clinical signs appear when the cavity grows and interferes with normal functioning. Or a rupture occurs, the fluid spreads into the adjacent cavities and the bladder becomes infected.
Urine with blood.
- nagging pain in the pelvic organs (a common sign of urachus cysts in women);
- pain with the urge to urinate (more often appears as a sign of a urachus cyst in men);
- blood clots in urine;
- frequent urge;
- incontinence;
- large volume of urine at one time;
- acute pain in the lumbar region;
- cloudy urine color;
- sharp sour smell;
- swelling in the navel area;
- elevated temperature - with the development of complications.
The pathology is characterized by frequent urination and defecation of women, which is due to the anatomical feature - a short urethra. Painful sensations and a feeling of fullness are more often diagnosed in men. The release of purulent exudate indicates the risk of complications. These symptoms also indicate cystitis in any form.
Frequent urge to urinate and defecate in women.
The presence of an inflammatory process provokes a sharp growth rate of the cyst with accompanying symptoms:
- The tumor is felt when palpating the abdomen. The formation is dense to the touch, pressure causes pain.
- The abdominal organs (ureters, bladder, stomach, intestines) are compressed.
- Problems with the gastrointestinal tract develop.
Gastroesophageal reflux can develop as another complication of the disease. Food and hydrochloric acid from the stomach move back into the esophagus. This happens when the walls of the stomach are compressed, as a result its size decreases. The esophagus becomes inflamed, causing a constant feeling of nausea and heartburn.
Signs of pathology are observed only when tumors of significant size form. The progression of the disease occurs against the background of inflammatory processes. An enlarged lump can be felt through the abdominal cavity.
The list of symptoms of bladder cysts in women includes:
- acute pain in the abdominal cavity;
- problems with urination;
- defecation disorder;
- chills all over the body;
- temperature increase;
- leakage of urine.
The clinical picture will depend on the size of the compaction and the severity of the disease. Urinary incontinence and problems with stool occur in the presence of large cysts. When defecating, the patient will feel significant discomfort.
With a long course of the pathology, a symptom of “acute abdomen” is observed. In this case, the disorder can only be dealt with through surgery.
Treatment
Urologists categorically do not recommend self-treatment with the help of medications, as well as traditional methods. Only a specialist can develop adequate treatment tactics.
This takes into account:
- age and weight of the person;
- stage of the disease;
- concomitant pathologies (if any);
- patient tolerance to medications;
- cyst condition;
- features of its impact on neighboring organs.
Drug therapy
Image courtesy of Baitong333 on FreeDigitalPhotos.net
Drug treatment cannot affect the presence of a cyst; it is removed surgically. However, taking medications is indicated to eliminate complications of cystic formation.
Main groups of drugs:
- Antibiotics . Ceftazidime or Ceftriaxone intramuscularly or intravenously suppress the harmful pathogen. Contraindicated in severe kidney and liver diseases, intolerance and pregnancy.
- Uroseptics . A course of taking Furazolidone (Furadonin), Nifuratel or 5-NOK helps to relieve the main problems with bladder emptying and destroy pathogenic microflora that has spread throughout the genitourinary tract. The drugs normalize the process of urination, pain and burning sensations go away. Contraindicated for pathologies of the stomach, kidneys and liver, as well as for intolerance, pregnancy and lactation.
- Detoxifiers . Rheosorbilact, Metrogyl and saline solutions intravenously. They improve the general condition after damage to the body by pathogens.
- Immunomodulators and vitamin complexes . Strengthens the body's immune defense.
- Nonsteroidal anti-inflammatory drugs and analgesics are prescribed to relieve pain. Contraindicated for stomach diseases.
Surgery
There are several methods of surgical intervention for cystic formations of the bladder.:
- Cystoscopy . Above, we described the procedure as a diagnostic method, but during its implementation it is possible to remove cysts, polyps and other tumors of the bladder.
- Transurethral resection (TUR) . This is a minimally invasive way to remove a cyst using an endoscope. During this procedure, the surgeon excises and removes the cyst without damaging the healthy tissue of the organ.
- Laparoscopy . Access to the organ is provided by several small punctures in the abdominal cavity, through which a laparoscope with a camera and instruments are inserted to carry out the necessary manipulations. The cyst is excised, then the area where it is located is cleared of harmful contents, the puncture sites are sutured and a sterile bandage is applied.
- Cystectomy . An operation in which an organ is removed. Cystectomy is prescribed only as a last resort, for example, when cancer is detected.
Surgical intervention is possible only in the absence of an exacerbation of the inflammatory process.
Which doctor treats bladder cysts?
A surgeon treats cysts in the bladder in women.
If there is a neoplasm in men, additional consultation with a urologist will be required. The specialist prescribes a suitable treatment regimen after an external examination of the patient and taking into account his complaints. From the patient, the specialist learns information about how long ago unpleasant symptoms appeared and the presence of chronic diseases. For small tumors, there are no symptoms for a long time; they appear with the growth of the cyst and secondary infection. The patient complains of pain in the lower abdomen, in the navel area, discomfort and frequent urination. The feeling of incomplete emptying after urination occurs due to an obstruction to the outflow of urine. If the cyst exerts a compressive effect on the intestines, flatulence, constipation, and cramps occur. During palpation examination of the abdomen below the navel, a dense elastic round formation may be detected, painful when pressed. Hyperemia of the skin over it and severe pain indicate infection.
When a fistula tract forms, serous fluid is released from the navel (if infected, purulent discharge with an unpleasant odor and blood). Excessive maceration leads to the development of dermatitis. The breakthrough of a cyst deep into the bladder is manifested by the clinical picture of acute cystitis: pain with frequent urination, increased temperature, change in the nature of urine excreted (fetid odor, admixture of blood and pus). In adults, a urachal cyst is often diagnosed during examination for gross hematuria. Dyspareunia (pain and discomfort during and after sexual intercourse) is reported less frequently.
Treatment
Anti-inflammatory drugs, antibiotics or other drugs are prescribed to combat the provoking agent, antiseptics, diuretics with a mild effect, preferably based on herbal components (herbal preparations).
Forecast
Mostly favorable. Classic cysts do not tend to create big problems for the patient or provoke dangerous complications.
However, with mechanical impact, it is quite possible for the capsule to rupture and the contents of the sac-like formation to escape into the structures of the bladder and the abdominal cavity.
This is fraught with the development of an infectious lesion, even sepsis, since the contents are not sterile. In such a situation there is a risk to life and health.
Prevention
No specific preventive measures have been developed, since the cause of the pathological process is unknown to doctors. Based on the expected risk factors, the following recommendations can be made:
- Timely treatment of infectious diseases of the bladder and excretory structures. Under the supervision of a doctor, independent treatment is impossible.
- Regular preventive examinations with a urologist/nephrologist or several specialists at once.
It is important to closely monitor your health. The slightest deviations are grounds for visiting a specialist.
A bladder cyst is a relatively rare condition; it has few symptoms or no symptoms at all, making it difficult for targeted diagnosis. Usually, the problem is discovered by chance, during diagnosis for other diseases.
Treatment is not always required, depending on the case. In any case, it is recommended to adhere to the doctor's advice and follow the recommendations. What a specialist decides depends on his approach to the management of such patients. As a rule, this is dynamic regular observation. The operation requires compelling reasons and indications.
Sources
There are several types of bladder cysts, most of which are not cancerous.
Bladder cysts usually do not cause symptoms. However, a person may experience painful or frequent urination. In such situations, cysts are often mistaken for cystitis.
In this article, we will describe the types, causes, symptoms, diagnosis and treatment of bladder cysts.
articles: 1. What are bladder cysts? 2. Bladder cysts and cancer 3. Symptoms of bladder cysts 4. Diagnosis of bladder cysts 5. Causes of formation of cysts in the bladder 6. Treatment of bladder cysts 7. Complications of bladder cysts 8. Conclusion
Symptoms of bladder cysts include urinary urgency, excessive urination at night, and pain while urinating.
A cyst is a tissue shell, which inside is filled with gases, liquid or semi-solid substance. Cysts can appear in any area of the body, both inside and outside the body. Bladder cysts most often occur in the mucous membrane of the organ.
They are relatively rare in people whose urinary system functions normally. Such cysts are usually small, non-cancerous in nature and go unnoticed. As a rule, they are identified when doctors examine other problems of the pelvic cavity.
In the bladder, cysts can cause the same symptoms as polyps. The latter appear as a result of abnormal cell growth and, unlike cysts, do not have other materials inside. Polyps can be either benign or cancerous.
In most cases, bladder cysts are benign, meaning they are not cancerous.
The doctor must determine whether the new growth is a cyst or a tumor. Much more often tumors are associated with cancer.
American doctors believe that chronic infections or irritations of the bladder increase the risk of developing cancer. If a person has such a problem, he needs to discuss it with a doctor, who will give recommendations on reducing risk factors and can ensure regular monitoring of the patient's condition.
Most bladder cysts do not cause symptoms. People usually begin to experience symptoms when cysts grow too large or rupture and become infected. Conditions that underlie the appearance of cysts may cause associated symptoms.
If symptoms occur, they may include the following:
- pain during urination;
- blood or colored streaks in the urine;
- pain when needing to urinate;
- continued urinary urgency;
- inability to control the bladder, i.e. incontinence;
- excessive urine output at night;
- pain in the lower back or pelvic area;
- unpleasant or sour urine odor.
A person may experience similar problems if they have other bladder problems, such as kidney stones or urinary tract infections (UTIs).
These symptoms may also be a consequence of interstitial cystitis, a chronic bladder disease, the cause of which is currently unknown. This condition leads to severe pain during urination and frequent urination, which can occur in a person every ten minutes.
Symptoms
Causes
A bladder cyst is located in the bladder, or more precisely in its duct – the urachus.
Pregnant
In this regard, you can find other medical terminology associated with such pathology.
Very often it is called a “urachal cyst”. Human organs are formed, as is known, even in the prenatal period. The urinary duct plays an important role until the fifth month of this period.
It connects the bladder with amniotic fluid. After the fifth month, the expected changes occur, due to which the walls of the bladder duct begin to close and it closes.
According to the rules, it should be completely closed, but sometimes developmental anomalies occur. As a result, only the ends of the bladder duct fuse (completely close), while its middle part remains hollow.
This is what provokes the formation of a urachus cyst.
It is filled with mucus, primary feces and urine. It can exist in this state for a long time without showing any symptoms, since its size is small.
But when microbes or bacteria enter the cyst, the size increases, reaching almost 15 centimeters.
This type of bladder cyst is more often diagnosed in men, and the frequency of anomalies in them is almost three times higher than in women.
Despite the highest level of development of modern medicine, it is not possible to fully determine the true causes of duct abnormalities in the bladder.
Therefore, most doctors believe that this pathology is caused by disturbances in embryonic formation.
Due to the fact that the true cause remains unclear, it is also impossible to develop a set of preventive measures to prevent the development of such cysts in the bladder.
Classification
An excretory duct cyst can have different sizes, its volume varies - from 5-10 ml to 100 - 150 ml. There are giant cystic cavities that cause compression of neighboring organs. There are complicated and uncomplicated urachal cysts. The urinary duct is conventionally divided into three parts: proximal, median and distal. When regression processes are disrupted in various parts of this embryonic formation, four known defects arise, including the urachus cyst (some authors include in the classification the alternating sinus - a defect when the cyst is drained alternately through the umbilicus and into the bladder):
- Umbilical fistula (incomplete). The absence of obliteration maintains communication with the umbilicus (distal cleft), leading to the formation of a fistula, or sinus (this name is often used in the English-language literature). Occurs in 36.5% of cases.
- Vesico-umbilical fistula (complete). Urine comes out of the bladder through the navel, since the embryonic duct is completely open. Diagnosed in 20% of cases of all urachus pathologies.
- Diverticulum. Its formation is caused by a non-closure of the duct in the area of the apex of the bladder (proximal section). The detection rate of diverticulum is 1.6%.
- Urachal cyst. The cyst is isolated from the navel and bladder, i.e., the distal and proximal ends of the urinary tract are closed. Cystic formations are most often located in the middle, but can be localized at any level of the urachus. This pathology is recorded most often - in 42% of cases.
Diagnostic measures
If the bladder cyst reaches a large size, it can be easily felt through the abdominal wall between the navel and the pubic bone. In other cases, instrumental research is carried out.
Instrumental diagnostic methods include:
- CT scan . On a computed tomogram, a cyst will be identified as an expansion or cavity in the area of the vesico-umbilical duct in the thickness of the anterior abdominal wall.
- Ultrasound. During an ultrasound examination, its area is visible as an area of increased echogenicity. The boundaries of such formation are unclear. If it is filled with exudate, it takes on a round or oval shape.
- Cystoscopy. An endoscopic examination allows you to evaluate the condition of the bladder wall from the inside. If the cyst communicates with the bladder or protrudes into it, which happens with a cyst in the bladder in men, it is easily detected visually.
- Cystography. X-ray technique in the form of cystography allows you to identify only a cyst communicating with the bladder. To do this, the bubble is filled with a special contrast and a series of photographs are taken.
- Fistulography. During fistulography, a contrast agent is injected into the lumen of the fistula from the navel, then an X-ray is taken. This study makes it possible to assess the length and width of the lumen of the unclosed germinal duct. If there is a cyst, the contrast agent will accumulate in it and make it visible.
There is a simpler method in which a solution of methylene blue is poured into the fistula from the navel through a cannula. If the cyst communicates with the bladder, the urine turns blue after some time.
Prevention
Specific measures to prevent the formation of cysts in the bladder have not been developed, since doctors do not reliably know the cause of the problem. Urologists give preventive recommendations based on factors predisposing to the disease. These include timely elimination of infectious diseases of the urinary system and regular examinations by a nephrologist in case of hereditary predisposition to urolithiasis.
Bladder cysts are a rarely diagnosed disease. It manifests itself with vague symptoms, which creates difficulties for timely diagnosis of the disorder. Removal of a bladder cyst is not required in all cases. The treatment regimen depends on several factors: the severity of symptoms, the size of the lump and the age of the patient.
- In the case of purulent inflammation, there is always a risk of the cyst breaking into the abdominal cavity. The wall of the cyst is separated from the abdominal organs only by a thin serous membrane. When the parietal peritoneum ruptures, infected contents can get inside and cause diffuse purulent peritonitis.
- When a cyst communicates with the bladder, it causes the clinical picture of chronic cystitis. In the future, this condition can lead to an ascending infection with purulent kidney damage.
- If an inflamed cyst occurs in a woman, this pathology can lead to inflammation of the nearby fallopian tube and ovary.
- A long-existing festering cavity is a source of chronic infection. This can lead to severe degeneration of internal organs or to a life-threatening septic condition.
The prognosis for bladder cysts is ambiguous. In the case when the formation is not complicated by fistulas or inflammation and is small in size, it does not affect the state of health in any way. Meanwhile, it should be remembered that during infectious diseases, injuries and stress, this cavity adjacent to the bladder can become inflamed and lead to the development of complications.
Share the article on social media. networks:
It is important to follow prevention regardless of whether a cyst appears on the bladder of a woman or a man. It is important to have regular medical examinations. In addition, the following measures are required:
- Do not overcool the body, especially the lower part.
- Maintain personal hygiene: wash regularly, change underwear.
- Eat a balanced diet.
Cysts of the bladder, including urachus, are often benign and do not cause discomfort. However, if the infection is not treated in time, it can lead to the degeneration of the neoplasm into a malignant one and the development of cancer. It is important to seek medical help promptly and follow preventative measures.
Candidate of Medical Sciences, mammologist-oncologist, surgeon
More articles
To prevent postoperative complications, after surgery for urachal cysts, tests are performed: CT scan, cystoscopy, urine cytology. The patient is under the supervision of a doctor throughout the recovery period and must strictly follow all medical recommendations.
If the root cause of the urachus cyst is unclear, prevention is difficult. General recommendations include:
- Strengthening the immune system (adequate physical activity, proper rest, compliance with nutritional rules, intimate hygiene, taking vitamin complexes);
- Prevention of infectious diseases of the genitourinary system.
Sources
The prognosis for timely surgical treatment is favorable, since it avoids complications. No preventive measures with proven effectiveness have been developed. Considering the potential teratogenic effects of alcohol, nicotine and narcotic drugs on a woman’s body and fetus, one should adhere to a healthy lifestyle not only during pregnancy, but throughout life.
Symptoms of cystitis in women
Every woman encounters cystitis - inflammation in the bladder - at least once during her life. Because the female urethra is wide and short, infection easily enters the bladder. Cystitis is bacterial and viral in nature. Trichomonas, Candida fungi, staphylococcus, streptococcus, and E. coli bacteria cause inflammation. Sometimes cystitis develops against the background of inflammation of the urethra after sexual intercourse. In this case, symptoms appear within 12 hours after sex. Risk factors are impaired urine outflow, active sex life, hypothermia, infections in the pelvis, pregnancy and childbirth, hormonal imbalance, pyelonephritis.
Main signs of cystitis:
- frequent and painful urination;
- the appearance of nocturia, that is, the urge to urinate at night;
- change in the color of urine, the appearance of a cloudy shade;
- increased odor of urine;
- hematuria - the appearance of blood in the urine;
- pain in the lower back and lower abdomen;
- burning sensation;
- fever and chills;
- nausea and vomiting.
The listed symptoms are characteristic of acute cystitis. With timely and competent treatment, the mucous membrane of the bladder is restored, and complete recovery occurs. If the root cause has not been identified and eliminated, and complex therapy has not been carried out, the disease may progress to the chronic stage. With chronic cystitis, unpleasant symptoms may reappear. The course of treatment for the disease is prescribed by a urologist and usually includes antibiotic therapy, analgesic therapy, and immunotherapy. Patients are recommended to drink plenty of fluids and correct sexual and hygienic factors.
Surgical intervention
A radical method of healing for a bladder cyst is its excision. If there is an accumulation of purulent inflammatory exudate in the cyst cavity, the abscess is initially opened and drained. Later, when the acute period has passed, surgery is performed.
For radical healing, complete excision of the embryonic vesico-umbilical duct along with the umbilical ring is performed. It is recommended to carry out the operation as planned. Most often it is performed after the child reaches 6 years of age.
In case of complete non-closure of the urachus, its excision should be carried out in the first years of life.
Surgical treatment is carried out only in a hospital setting , preferably in a specialized department. During the operation, an incision is made in the anterior abdominal wall along the midline of the abdomen. The urachus together with the peri-vesical cyst is separated. An important point of the operation is to preserve the integrity of the serous membranes of the abdominal cavity.
With a cyst located near the wall of the bladder, you need to be especially careful. This arrangement may cause damage to the ureter.