Infectious-allergic, or autoimmune, kidney disease is called glomerulonephritis. This pathology often appears after a recent (2-3 weeks ago) cold infection, nasopharyngitis, or repeated sore throat.
Hypothermia in combination with chronic foci of infection, such as chronic tonsillitis, caries, sinusitis, significantly (60%) increases the risk of acute glomerulonephritis.
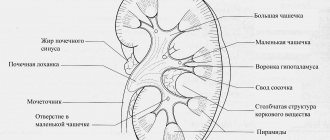
With glomerulonephritis, extensive inflammation of the kidneys is observed with damage to the main filtration device - the glomeruli, the renal glomeruli. It is thanks to the glomerular apparatus that the blood is purified, followed by the release of “slags” into the urine, that is, substances that the body does not need. With glomerulonephritis, the glomeruli are most affected, which immediately affects the characteristics and indicators of urine analysis.
Urinary syndrome
The clinical picture of diseases is characterized by the presence of a set of symptoms, that is, a syndrome.
Urinary syndrome is a sign of an increasing inflammatory reaction of the glomeruli (glomeruli), that is, a sign of dysfunction of the renal glomeruli and kidney function, respectively. The syndrome is characterized by the presence of a main triad of symptoms:
- Decreased amount of urine excreted (oliguria). With the development of acute glomerulonephritis, in the first 3 days, there is a sharp decrease in the amount of daily diuresis (up to 500 ml/day). That is, the patient visits the toilet less often, and during emptying the bladder, a relatively small amount of urine is released. When conducting a urine test (general analysis), during the period of oliguria, an increase in specific gravity is noted (over 1.040). After 3 days, the opposite symptom appears, that is, polyuria (increased volume of waste diuresis). At the same time, the density of urine decreases (below 1.010). A long period of oliguria, which lasts more than 3-4 days, is a dangerous symptom, indicating a high likelihood of developing acute renal failure (ARF).
- The appearance of protein in the urine (proteinuria). This symptom indicates a malfunction of the renal glomeruli and tubules. A companion to proteinuria is the appearance of hyaline casts in urine analysis. With glomerulonephritis, an insignificant (up to 1 g/l) or moderate (up to 3 g/l) amount of protein in the urine is often observed. However, with a severe, nephrotic form of the disease, massive proteinuria (over 3-4 g/l) may develop. The peak increase in protein in urine occurs in the first 2 weeks, from the moment of development of glomerulonephritis. With proper treatment. There is a gradual decrease in the level of proteinuria, and the last traces of protein disappear by 6-8 weeks, from the moment of illness.
- Blood in the urine (hematuria). Red blood cells in the urine with glomerulonephritis are present in a single quantity, from 5 to 99 in the field of view. At the same time, there are no visible changes in the color of urine. However, there is a possibility of developing macrohematuria, that is, the appearance of a large number of blood cells in the urine. At the same time, urine acquires the characteristic color of “meat slop”, a cloudy red tint - a fairly classic sign of acute glomerulonephritis. The appearance of blood in urine is associated with increased permeability and an increase in the diameter of the pores of the basement membranes, glomeruli (septa and vessels of the renal glomeruli). The level of red blood cells in the urine with glomerulonephritis reaches a peak in the first days of the disease, gradually decreasing and completely disappearing by 2-6 weeks.
It should be noted that the level of leukocytes in the urine with glomerulonephritis increases slightly, reaching 12-25 units in the field of view. Leukocyturia is a typical symptom of pyelonephritis, while hematuria is a typical symptom of glomerulonephritis.
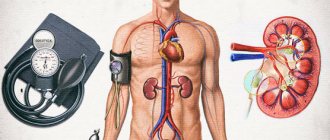
Urinary syndrome, in the typical course of the pathology, is accompanied by edema and increased blood pressure (hypertension). The development of such symptoms is directly dependent on the urinary syndrome itself.
- Swelling, first of all, appears on the eyelids, and the skin acquires pronounced pallor (a typical face of a “nephrotic”). Gradually, swelling can take over the entire area of the face and spread to the limbs. In severe forms of pathology, fluid accumulation in the natural cavities of the body (abdominal, pleural, etc.) is possible.
- Blood pressure rises moderately, rarely very strongly. With timely treatment and treatment, normalization of blood pressure is noted by the 10th day from the onset of the disease. In addition, a short-term, one-, two-day, or one-time increase in blood pressure is possible.
In some cases, it is possible to develop isolated urinary syndrome, that is, there are changes in urine that are not accompanied by the appearance of edema and an increase in blood pressure.
Acute glomerulonephritis: treatment, symptoms, complications, diagnosis, classification, forms, causes
The causes of acute glomerulonephritis can be various factors. An infectious etiology of the process is usually diagnosed. Acute post-streptococcal glomerulonephritis is identified as a separate form, since it occurs most often and serves as a model for the study of glomerulonephritis.
Non-streptococcal species provoke the following microbes:
- bacteria - meningococci, pneumococci, Staphylococcus aureus;
- viruses that cause chickenpox, mumps, viral hepatitis B and C.
In addition, the following reasons can cause kidney damage:
- systemic diseases, including collagenosis;
- primary kidney pathology, often congenital, autoimmune or genetic;
- exposure to other factors - radiation for cancer problems, taking certain medications, administration of serums or vaccines.
The pathogenesis of the acute variety of glomerulonephritis can be most clearly explained using the example of post-streptococcal lesions. In its development it goes through the following stages:
- The appearance of a focus of infection (usually hemolytic streptococci of group A) in the area of the tonsils, middle ear, and skin.
- Production of antistreptococcal antibodies to microbial antigens and their combination.
- Deposition of formed immune complexes on the walls of glomerular capillaries and damage to renal tissue.
The pathogenesis of acute glomerulonephritis also includes the development of typical syndromes, the main of which is urinary. This syndrome involves a symptom complex consisting of a number of urinary changes:
- oliguria - a decrease in the amount of urine excreted is due to a decrease in the mass of functioning glomeruli, while the specific gravity of urine increases;
- proteinuria - the appearance of albumin, proteins with low molecular weight, in the urine due to inadequate filtration;
- hematuria - blood in the urine due to inflammatory damage to the vessels of the kidneys and increased capillary permeability;
- the appearance of leukocytes and casts in tests is explained by inflammation of the renal tubules and organ parenchyma.
Since the filtration function of the kidneys is reduced, fluid is retained in the bloodstream, swelling and increases in blood pressure appear.
Classification
The medical literature provides several variants of pathology classifications, which are based on different criteria.
Thus, there is a classification that divides the forms of the disease depending on the background on which the kidney damage was formed. The following types are distinguished:
- primary disease - damage occurred due to direct effects on the kidney tissue of infectious agents, poisons, allergies, autoimmune complexes;
- secondary glomerulonephritis - the development of pathology against the background of serious disorders of other organs;
- idiopathic variety, when the cause cannot be determined.
A classification has been developed that allows a correct diagnosis to be made based on the analysis of histological samples of the renal parenchyma. According to pathomorphology, varieties are distinguished with a predominance of sclerosis of the kidney elements, pathological proliferation of the glomerular epithelium, and damage to the capillary network.
Classification of acute glomerulonephritis based on the extent of the lesion:
- focal acute process, in which isolated and scattered areas of renal tissue are inflamed;
- acute diffuse glomerulonephritis, which is characterized by damage to more than half of all renal glomeruli and areas of inflammation merge with each other.
Varieties of acute forms, depending on clinical manifestations:
- expanded - a combination of urinary syndrome with edema and hypertensive;
- bisyndromic - urinary syndrome along with only high blood pressure or severe edema;
- monosyndromic - only urinary syndrome or acute glomerulonephritis with nephrotic syndrome.
In addition, there are types of pathology with a typical clinical picture and those with a long latent course.
Symptoms
It is customary to distinguish the following main syndromes of acute glomerulonephritis:
- urinary - pronounced changes in urine;
- edematous - the appearance of edema;
- hypertensive - persistent increase in blood pressure.
As a rule, the clinic unfolds against the background of severe intoxication. Symptoms of acute glomerulonephritis appear 1-2 weeks after an infection of the upper respiratory tract or ENT organs, most often caused by streptococcus. A person’s general condition suddenly deteriorates, fever, nausea, weakness return, and appetite disappears.
But the main sign by which acute post-streptococcal glomerulonephritis can be suspected is changes in the urine. Reddish urine (macrohematuria) is observed in 15-30% of patients, and microhematuria is detected in the majority. Diuresis (the amount of urine excreted per day) sharply decreases.
Sometimes hematuria is the only sign of kidney damage ; there are no other clinical manifestations. This is typical for the latent form.
Almost 8 out of 10 patients experience swelling. Typical localization is the face, eyelids. They increase in the afternoon, and in the evening there is a pastiness of the legs and feet.
Arrhythmias, attacks of angina pectoris, shortness of breath, abdominal pain are possible, which is explained by the accumulation of fluid in the pericardial area, the formation of ascites, and pleurisy.
In addition, a clinic for arterial hypertension is gradually being formed. In this case, rises in pressure are accompanied by chest pain and headaches, dizziness, the appearance of weather dependence and irritability.
In children, acute diffuse glomerulonephritis manifests itself very clearly and is characterized by severe intoxication. Adult patients often notice moderate disturbances in their general condition and consult a doctor due to changes in the color of urine.
Diagnostics
If, after suffering from tonsillitis or otitis, a person again develops fever and other warning signs, he or she should undergo a general urine test. Sometimes blood in the urine can only be determined by laboratory testing.
To identify kidney damage, the doctor carefully collects anamnesis and examines the patient. But basically, the diagnosis of acute glomerulonephritis is based on laboratory examination data. A general urine test records pathological changes characteristic of urinary syndrome.
Feature: in urinary sediment, erythrocytes always prevail over leukocytes. Special urine tests and urine culture are also carried out.
A general blood test reveals the following:
- leukocytosis;
- decrease in hemoglobin and red blood cell count;
- increase in erythrocyte sedimentation rate.
There may be an increase in cholesterol, fibrinogen, creatinine and urea in the blood. Characterized by a high content of antibodies to streptococcus, an increase in the concentration of globulins.
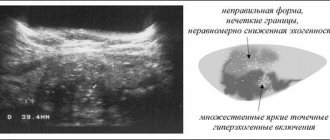
To make a diagnosis of acute glomerulonephritis, the following instrumental methods are most informative:
- ultrasound examination of the kidneys;
- isotope renography;
- Kidney tissue biopsy is the most accurate, but rarely performed, method of examination.
Such popular techniques in nephrology as excretory urography and endoscopy of the bladder are not always indicated for suspected acute diffuse glomerulonephritis. In difficult cases, magnetic resonance imaging or examination using nuclear magnetic resonance is prescribed.
Treatment
Acute diffuse glomerulonephritis can only be treated in an inpatient setting. The patient is urgently hospitalized in the nephrology department.
Therapy includes etiotropic and symptomatic agents. For post-streptococcal glomerulonephritis, antibacterial drugs are prescribed, usually penicillin.
Representatives of the cephalosporin group (Cefazolin) are effective. Before choosing a medicine, the sensitivity of the microbe to various antibiotics is determined.
Antistreptococcal plasma and immunoglobulin are sometimes administered as additional therapeutic agents.
If the pathology is of viral origin, antiviral treatment is carried out - Cycloferon, Ribaverin. It is also necessary to treat the underlying disease that caused kidney damage.
Treatment of acute glomerulonephritis involves combating the underlying syndromes. For this, the following groups of drugs are used:
- diuretics (Furosemide, Mannitol);
- antihypertensive drugs (Enalapril, Capoten, Obzidan);
- anticoagulants (Heparin, Curantil);
- immunomodulators (Levamisole, Timalin);
- antioxidants (Oxylic, Tocopherol acetate);
- vitamins (ascorbic, nicotinic acid, B vitamins).
Acute diffuse glomerulonephritis, complicated by renal failure, makes hemodialysis sessions necessary.
To determine the dynamics of the condition and the effectiveness of therapy, tests are taken regularly: urine - every 3 days, blood - once a week. During treatment, the decrease in the level of streptococcal antibodies is monitored every 5-7 days. Diuresis is measured daily in relation to the amount of fluid drunk. It is necessary to take an ECG, monitor blood pressure, and monitor the condition of the fundus vessels.
In addition, a special therapeutic diet No. 7a is prescribed, which involves the following points:
- drinking regime - no more than 1 liter of water per day;
- sodium chloride intake should not exceed 2 g;
- exclusion of rich meat broths and soups;
- consumption of vegetables, fruits, eggs and cottage cheese.
Forecast
The rehabilitation process proceeds faster with minor renal damage and the absence of serious concomitant health problems. With timely treatment and adequate treatment, acute glomerulonephritis does not cause complications, the person recovers.
In advanced cases, there can be dire consequences for health. The transition of the acute stage to the chronic phase is possible.
The following life-threatening complications of acute glomerulonephritis may also develop:
- transformation into a rapidly progressive form that threatens acute renal failure;
- eclampsia, characterized by the sudden development of a coma and the appearance of convulsive seizures, develops in particularly difficult cases;
- slow progression of the process leading to chronic renal failure.
Prevention
The disease can be prevented by taking the following measures:
- strengthening immunity from an early age;
- combating foci of chronic infection in the body;
- timely treatment of any acute conditions;
- avoiding hypothermia, especially of the legs.
In the presence of a burdened allergic history, preventive vaccinations are given only according to strict indications and against the background of hyposensitizing therapy.
The acute form of glomerulonephritis is a dangerous disease, the complications of which threaten human life. Therefore, it is so important to be attentive to your health and consult a doctor at the first warning signs.
Olga Shchepina, doctor, specially for Nefrologiya.pro
about acute glomerulonephritis
Source: https://nefrologiya.pro/pochki/glomerulonefrit/ostriy-vid/
Creatinine level
Creatinine is a product that appears as a result of the energy metabolism of body tissues, including muscle. The rate of its content in the body depends on the gender, age, muscle mass of the patient, physical activity and type of nutrition. Accordingly, a man who plays sports or works in production will have a higher creatinine level than a woman or child.
Creatinine is excreted by the kidneys, that is, with urine.
A blood or urine test is often prescribed to assess kidney function in general and glomerular filtration in particular. This kind of research makes it possible to detect even latent kidney pathologies (chronic processes, etc.), diseases of the muscular system.
Determining the level of creatinine is important in the presence of chronic glomerulonephritis; it allows identifying the development of chronic renal failure (CRF) in the early stages.
Both blood (biochemical analysis, Rehberg test) and urine (Rehberg test) are suitable for testing. The Rehberg test, or creatinine clearance, is necessary to more accurately determine the level of creatinine in human biological fluids.
Creatinine is not processed in the body, but is excreted in the urine! Therefore, the slightest disturbances in the functioning of the filtration systems (kidneys, liver) lead to the accumulation of creatinine, which, as it concentrates, aggravates the course of the underlying disease.
An increase in the level of creatinine in the blood is observed in chronic glomerulonephritis. Such symptoms may indicate the development of chronic renal failure. A very high level of creatinine (more than 180 mmol/l) indicates the need for forced cleansing of the body - a hemodialysis procedure.
↑ Etiology. Pathogenesis
The disease occurs most often after tonsillitis, tonsillitis, upper respiratory tract infections, and scarlet fever. An important role in the occurrence of glomerulonephritis is played by the 12th strain of B-hemolytic streptococcus of group A. Glomerulonephritis may occur under the influence of bacterial infections: pneumonia (staphylococcus, pneumococcus), as well as other infections - diphtheria, typhus and typhoid fever, brucellosis, malaria, infectious mononucleosis , hepatitis B, enteroviruses. It is possible to develop glomerulonephritis after administration of vaccines and serums. The development of the disease is facilitated by hypothermia, high humidity, surgery, injury, physical activity, and alcohol. Cooling causes a reflex disorder of the blood supply to the kidneys and affects the course of immunological reactions. Streptococcal toxins, damaging the structure of the basement membrane of the glomerular capillaries, cause the appearance of specific autoantigens in the body, in response to which antibodies of the immunoglobulin U and immunoglobulin M classes are formed. Under the influence of a nonspecific resolving factor, most often cooling, a new exacerbation of the infection, a violent allergic reaction of the antigen compound occurs with the antibody, the formation of immune complexes with the subsequent addition of complement to them. Immune complexes are deposited on the basement membrane of the glomeruli of the kidney, damaging them. There is a release of inflammatory mediators, damage to lysosomes and the release of lysosomal enzymes, activation of the coagulation system, disturbances in the microcirculation system, increased platelet aggregation, resulting in the development of immune inflammation of the glomeruli of the kidneys.
Changes in urine
With glomerulonephritis, there are changes in urine visible to the naked eye.
- Transparency. Due to proteinuria, turbidity, sediment, and flakes appear in the urine. Urine loses transparency. There may be foam in the urine.
- Color. Urine in acute glomerulonephritis takes on the characteristic “color of meat slop,” that is, water in which red meat was washed. This is a specific red-brown shade. In a chronic process, periodic relapses are observed, respectively, urine during this period has a similar color. Urine may be dark, deep yellow, or cloudy pink.
Changes in laboratory tests:
- Red blood cells: from 5 to 100 or more units in the field of view.
- Leukocytes: from 12 to 25 units in the field of view (there are always fewer leukocytes than red blood cells).
- Protein: from 0.033 to 3 g/l (in severe cases: more than 3 g/l).
- Specific gravity: at the beginning of the disease there is an increase (over 1.040), then a decrease in indicators (less than 1.010).
- Cylinders: hyaline, erythrocyte (acute glomerulonephritis). In the chronic process, granular, waxy cylindrical cells often appear. Normally, the content of cylindrical cells is single, with the development of acute or chronic glomerulonephritis, the indicators exceed 20 units in the field of view.
The results of the studies depend on the form of glomerulonephritis (acute, chronic), the type of clinical syndrome (nephritic, nephrotic, mixed, hematuric), and the severity of the pathology.
Treatment of the disease
Timely detection of pathology allows treatment with conservative methods. In this case, hospital therapy is required. To suppress the autoimmune reaction, a course of immunosuppressants is prescribed. Typically, cytostatics, glucocorticosteroids and selective immunosuppressants are used. Among other things, diuretics are used to stabilize the condition and reduce swelling. Additional medications may be prescribed to correct symptoms that have developed against the background of the underlying disease.
During the treatment of this pathological condition, it is very important for patients to support the body with a special diet, primarily aimed at increasing the daily dose of protein
It is very important that food contains at least 1.4 g of this substance per 1 kg of human weight. Animal proteins should make up at least 2/3 of the total
Typically, patients are recommended to follow diet plan No. 7 with the consumption of egg whites, cottage cheese, lean fish and meat. If, against the background of such a diet, a decrease in kidney function is observed, it is necessary to reduce the amount of protein intake. It is very important that the patient avoids high-fat foods throughout the treatment period. Against the background of the disease, an increase in the level of triglycerides and cholesterol is observed in the blood.
To compensate for potassium deficiency, potatoes, bananas, honey, legumes, and greens are introduced into the diet. Given the severity of edema, salt intake should be completely eliminated or limited. Patients suffering from glomerulonephritis with nephrotic syndrome should not consume marinades and salty sauces.
Among other things, to reduce swelling, it is necessary to significantly reduce the daily dose of water consumption; it is recommended to consume no more than 1 liter. Throughout the entire period of treatment, patients suffering from this pathological condition are strictly prohibited from consuming mushroom broths, bread, offal, fatty meats, spicy and salty dishes, smoked meats and cheeses. A gentle diet should be followed until complete remission occurs.
Hematuria
Isolated glomerular hematuria can occur with primary and secondary glomerulonephritis, lesions of the renal vessels, tubulointerstitial disease and necrosis of the renal papillae. There is tubular and extrarenal hematuria, which develops with malignant tumors of the kidneys and urinary tract, kidney cysts, prostate adenoma, and urolithiasis. Hematuria occurs in IgA nephropathy, thin membrane disease, and less commonly in Alport syndrome.
IgA nephropathy
IgA nephropathy can develop with cirrhosis of the liver, Crohn's disease, adenocarcinoma of the stomach and colon, bronchitis obliterans, dermatitis herpetiformis, fungal mycosis, ankylosing spondylitis and Sjögren's syndrome, in which there is no inflammation in the glomeruli. A pathognomonic sign is IgA deposits in the mesangium, which can be combined with C3 deposits.
Clinical manifestations of IgA nephropathy are minimal. Gross hematuria, which occurs 24–48 hours after a sore throat, gastrointestinal infection and heavy physical activity, is the main manifestation of nephropathy. In some patients, during a routine examination, microhematuria is detected. Arterial hypertension occurs in 20–30% of patients and nephrotic syndrome – in 10%.
IgA nephropathy lasts for years. End-stage renal failure develops within 20 years in 30–50% of patients. The prognosis is worse in older men, with high proteinuria, renal failure at the onset of the disease, glomerulosclerosis and arteriolar hyalinosis. Microscopic examination reveals deposits of IgA and C3 in the kidney, expansion of the mesangium due to accumulation of the matrix and an increase in the number of glomerular cells, in severe cases - crescent, inflammatory infiltration of the interstitium and foci of glomerulosclerosis.
There is no treatment. In severe cases (rapidly progressive course, nephrotic and nephritic syndrome), high doses of immunosuppressants are recommended, with mandatory consideration of the underlying disease that led to the development of IgA nephropathy.
Thin Membrane Disease
Thin membrane disease, an autosomal dominant hereditary disease, usually begins in childhood and manifests as persistent or intermittent hematuria after acute respiratory infections. A morphological sign - a thin basement membrane (less than 275 nm in children and less than 300 nm in adults) - is detected by electron microscopy. The prognosis is good.
Alport syndrome
Alport syndrome is a hereditary nephropathy. The type of inheritance is dominant, linked to the X chromosome. It develops more often in men and is characterized by hematuria, proteinuria and progressive renal failure. In addition to kidney damage, 60% of patients have sensorineural deafness and 15–30% have eye damage - bilateral anterior lenticonus. In heterozygous women, the disease occurs in a mild form without renal failure. Microscopy reveals mesangial proliferation, focal segmental nephrosclerosis, tubular atrophy, and foam cells. Electron microscopy reveals a deformed and thickened basement membrane. The progression of the syndrome in men leads to the development of chronic renal failure, in which dialysis and kidney transplantation are indicated.
Isolated proteinuria
Isolated proteinuria without any underlying renal disease is found in 1–10% of the population. It may be benign or permanent.
Benign isolated proteinuria
Benign isolated proteinuria can have the following options:
- Transient idiopathic proteinuria is detected in young people with a single urine test during routine examinations (in a repeated urine test, protein is usually no longer present).
- Functional proteinuria - occurs with fever, hypothermia, emotional stress, heart failure (presumably due to increased intraglomerular pressure and glomerular filter permeability).
- Orthostatic proteinuria - caused by prolonged standing (usually does not exceed 2 g/day).
In all types of benign isolated proteinuria, a biopsy either does not reveal any changes or reveals minor changes in the mesangium and podocytes. The prognosis is favorable.
Persistent isolated proteinuria
Persistent isolated proteinuria is characterized by the constant presence of protein in the urine, regardless of external conditions and the condition of the patient. A biopsy reveals the morphological picture of any glomerulonephritis. Mesangioproliferative glomerulonephritis and focal segmental glomerulosclerosis are most often found. The prognosis for this syndrome is less favorable than for benign isolated proteinuria. Chronic renal failure develops in 20–30% of patients within 20 years, but it usually does not reach the terminal stage.
Glomerulonephritis is a lesion of the glomeruli in the kidneys, which are responsible for the transformation of blood plasma into primary type urine. The most common types are acute and chronic, occurring in different variants.
The causes of the disease and its severity vary, in some cases the changes are visible only in the field of view of a conventional microscope, in other cases an electronic one with high magnification is required. But regardless of the morphology, the doctor suspects glomerulonephritis in cases of high blood pressure, protein and red blood cells in urine tests, as well as general swelling.
Folk remedies
Here are some effective remedies that will help quickly restore kidney function:
- Take one tablespoon of dried black elderberry flowers, pour a glass of boiling water, leave until it cools completely. Take the medicine 1/3 cup three times a day before meals. The duration of taking elderflower infusion is 3-4 weeks, until complete cure.
- Healing collection for swelling. Mix flaxseed (4 parts) with dry birch leaves (3 parts) and field steel root (the same amount). Pour boiling water over it and leave to steep for a couple of hours. Then strain and consume a third of a glass three times a day. And so - for a week. After this time, you will forget what swelling is, get rid of pressure and heart pain.
- Mix 1 teaspoon of corn silk and the same amount of cherry tails, pour in 500 ml of boiling water and leave to steep until the medicine cools to room temperature. You need to take the infusion ¼ glass three times a day half an hour before meals. Treatment should be continued until the symptoms of glomerulonephritis disappear.
To boost immunity and help the body quickly cope with the pathological process, you need to take the following medicine every day, a teaspoon: a glass of honey, a tablespoon of walnuts, a tablespoon of hazelnuts, the peel of one lemon. Mix everything and store in a warm place.
Types of glomerulonephritis
Depending on the degree of predominance of certain symptoms and their severity, there are several clinical variants among the types of glomerulonephritis.
Chronic glomerulonephritis with isolated urinary syndrome
Chronic glomerulonephritis with isolated urinary syndrome is more common than other variants, and, as a rule, is discovered completely by chance. The patient has no complaints about the condition, no swelling or high blood pressure, the color of the urine is unchanged and within normal limits. And only during a routine medical examination, urine tests accidentally reveal protein and red blood cells up to 2g per day.
The course of this type of glomerulonephritis (CGN) is benign and does not require the use of aggressive treatment regimens. Because patients cannot detect symptoms, the onset of the disease is often missed and they consult a doctor only at the stage of development of renal failure.
Experts note that in some cases patients experience increased fatigue, weakness and morning facial pastiness. During the examination there are no signs of left ventricular hypertrophy, the fundus of the eye is not subject to changes.
Exacerbation of this form of the disease occurs during infection, hypothermia or pregnancy. An exacerbation is accompanied by an increase in hematuria and proteinuria by a factor of two or more. In this case, the glomerular structure in the kidneys is damaged and immunocomplex pathology develops. At this stage, swelling and high blood pressure levels may appear.
Relapses are quite rare, but lead to the transformation of this type into hypertensive or nephrotic. This type of glomerulonephritis lasts up to 25 years. Patient survival rate is 90%. Differentiation of the disease occurs with chronic pyelonephritis; urine tests using the Nechiporenko method reveal active leukocytes, unchanged erythrocytes, and extraglomerular microhematuria.
Nephrotic appearance
Neurotic glomerulonephritis occurs in 22% of all cases of the disease, and it is very difficult to miss its onset. Nephrotic syndrome is characterized by the following factors:
- protein excretion in the amount of 3 grams per day along with urine, and a diagnosis of proteinuria is made;
- severe swelling of the entire face and legs, as well as internal cavities, with pleurisy occurring in the lungs, ascites in the peritoneal cavity, and hydropericarditis in the heart sac;
- the protein in the blood plasma sharply decreases, a diagnosis of hypoproteinemia is made;
- Albumin, the lighter parts of protein cells, are lost along with the urine, the diagnosis sounds like hypoalbuminemia;
- detection of hyperlipidemia, when cholesterol reaches 12 g per liter or higher. Low-density lipoproteins also increase along with triglycerides.
This variant of glomerulonephritis requires serious and long-term treatment, since in addition to the listed symptoms, the patient experiences the following conditions:
- the immune system and resistance to penetrating infections are reduced, since copper and zinc are excreted along with the urine;
- the risk of thrombosis and osteoporosis increases, since the body loses vitamin D along with protein;
- symptoms of initial hypothyroidism appear due to the loss of thyroid-stimulating hormones;
- due to the resulting hyperlipidemia, atherosclerosis is complicated and the risk of stroke or heart attack increases;
- The most dangerous of all complications in nephrotic syndrome is hypovolemic shock and cerebral edema.
Hypertensive appearance
The most striking symptom of this disease is high blood pressure. Urine tests show slight proteinuria and an increase in red blood cells. If the disease is detected, treatment should be started as soon as possible, using antihypertensive drugs in the correct dosage.
Forecast
For glomerulonephritis, the prognosis depends on the form of the disease and the degree of spread in the body:
| № | Helpful information |
| 1 | Latent glomerulonephritis with isolated urinary syndrome does not manifest itself for many years and progresses quite slowly. In 20% of patients, the hematuric form can be cured with a combination of steroid drugs and medications - coagulators |
| 2 | inflammation without complications, which are detected in a school-age child, when carrying out gentle hormonal therapy in combination with cytostatics, allows success to be achieved in 80% of cases |
| 3 | Hypertensive glomerulonephritis is treated with drugs of various dosages that lower blood pressure. If therapy is prescribed incorrectly, heart failure, atherosclerotic plaques and an increased risk of stroke may occur. |
| 4 | With the edematous variety of the disease, the prognosis is most often unfavorable. Nephrotic types are evidence of kidney dysfunction and lack of filtration. The development of renal failure occurs quite quickly |
| 5 | mixed form of glomerulonephritis is marked by the most negative prognoses |