Cystectomy is a complex surgical operation, the essence of which is the removal of the bladder. In the case of a radical cystectomy, the man's seminal vesicles and prostate gland are removed along with his bladder. In addition, urethral resection is performed.
During this procedure, the proximal, i.e., is removed. the one located directly after the bladder, the section of the urinary canal. The pelvic lymph nodes on both sides are also removed. Typically, cystectomy is used to treat bladder cancer. In addition to surgery, other existing methods can be used to treat this disease.
Indications for TOUR
Radical cystectomy is prescribed:
- with progressive malignant growth of a bladder tumor, if other treatment methods, including chemotherapy, are unsuccessful;
- tumors emanating from neighboring organs (prostate gland in men, ovaries, cervix and endometrium in women, rectum) with growth into the bladder;
- significant deformation of the cavity, a sharp decrease in size due to the consequences of severe chronic cystitis, trauma, large size of a benign tumor;
- severe bleeding;
- recurrent cancer growth after economical transurethral resection (using endoscopic equipment);
- multiple papillomas on the mucous membrane inside the organ to prevent degeneration into a malignant tumor.
If the detected tumor is not characterized by rapid progressive growth and does not produce symptoms, then there is the possibility of partial cystectomy of the part of the bladder where the tumor is located.
Absolute contraindications that make surgery impossible are:
- the patient's serious condition due to cancer intoxication or concomitant diseases (stroke, heart failure, paralysis with dysfunction of the pelvic organs);
- detection of distant metastases in the brain, liver, lungs;
- stress urinary incontinence;
- blood diseases with reduced coagulability.
Weakness of the sphincter in older people disrupts the process of urinary regulation.
Relative contraindications include:
- a state of insufficiency of the internal sphincter of the bladder neck, if the examination establishes the maximum obturator pressure value is less than 30 cm of water. Art.;
- detection of a single metastasis in a patient in a neighboring lymph node with a diameter of 5 cm or less;
- detection of several similar metastases in the regional zone of lymph nodes;
- localization of the tumor in the area of the vesical triangle.
In case of relative contraindications, the use of other treatment methods, complex radiation and chemotherapy is considered.
This treatment method is used when there is a suspicion of the presence of altered cells in the tissues of the bladder. TUR is prescribed to detect bladder tumors and chronic inflammatory processes.
When performing a TUR, a biopsy of bladder tissue is performed to examine the cells of the affected area of the organ.
Resection is used only at the initial stage of development of a malignant neoplasm, when it has not yet affected neighboring tissues. At this stage, pathological cells are found on the mucous membrane and do not affect the muscles. If the cancer has spread to neighboring tissues and organs, resection will not have the desired effect.
Among the advantages of this type of surgical treatment are the following:
- minimal degree of injury to the mucous membrane and tissues;
- reducing the risk of bleeding;
- reducing the likelihood of developing an infection;
- maintaining the integrity of the skin;
- relative stability of the patient’s condition at all stages of treatment (subject to the doctor’s recommendations).
TUR is a reliable method of treatment in cases where superficial cancer is suspected.
The patient may have contraindications to TUR of the bladder due to the characteristics of the body’s condition. The operation is not performed if the patient has the following pathologies:
- narrowing in the urethra;
- any infectious diseases;
- diseases of the cardiovascular and genitourinary systems;
- kidney disease;
- liver failure;
- problems with blood clotting.
Each planned surgical intervention involves a thorough diagnosis aimed at identifying contraindications and determining the stage of development of the tumor. If surgery is not possible, another treatment method is used.
The patient is positioned on the surgical table, lying on his back. Legs bend at the knees and spread apart. Transurethral resection of the bladder (TURP) requires anesthesia.
When performing resection, a special device is used - a cystoscope. It is inserted into the bladder through the urethra. In order not to damage the mucous membrane of the organ, it is necessary to inject a sterile saline solution. It completely fills the bladder. This provides a good overview for surgical procedures. The device, which is inserted inside, is also equipped with a camera and lighting, which allows the operation to be performed remotely. All actions are displayed on the monitor.
Using a loop on the cystoscope, the tumor and surrounding tissue are removed. If the tumor is large, it is removed in parts - gradually, in several stages. The cut surface is immediately cauterized to avoid inflammation and bleeding. During a TUR, tissue samples are taken for biopsy. The results of the histological analysis will be ready in a week. It allows you to determine the nature of the tumor and choose a further treatment regimen.
To prevent the surface of the wound from bleeding over time, a catheter is inserted into the urethra in place of the cystoscope. A system for administering medications, which has two channels, is connected to it. The drug solution enters through one channel, and it is removed through the other. This two-channel system ensures cleansing of the organ from blood clots.
Carrying out surgical intervention requires serious preparation and careful diagnosis of the patient's condition. The uniqueness of TUR is that the procedure allows you to examine the diseased organ instrumentally with visual control at each stage of the examination. The entire operation process is broadcast on the monitor.
The use of one or another method of surgical treatment of bladder cancer (BC) depends on the location of the malignant tumor and the degree of its prevalence. Currently, the following surgical techniques are used for bladder cancer:
- radical cystectomy;
- partial cystectomy;
- TUR (transurethral resection).
Radical surgery, or cystectomy, that is, complete removal of the bladder for cancer, is the method of choice when the tumor has already spread deeper or is detected in late stages. Those. when the risk of relapse or the appearance of a secondary tumor is high, in Germany there is a clear preference for complete removal of the entire bladder. In fact, surgery to completely remove the bladder is recommended for stage 2 through 4 bladder cancer.
Now in German clinics, operations to remove the bladder, even in late stages of cancer, are performed through minimally invasive intervention - laparoscopy, which reduces the length of hospital stay and speeds up recovery. Compared to open surgery, the method of operating through a laparoscope, using a small hole in the abdominal cavity, is more gentle.
The operation allows you to save the bladder (organ-preserving), since only the part of the organ affected by the tumor is removed. Performed for small superficial tumors. Superficial tumors are those that do not affect the muscle layer of the bladder wall, but only the mucous membrane.
After such an operation, the bladder will certainly decrease in size and you will have to visit the toilet more often. However, this is probably more convenient than restorative plastic surgery: the urination function remains natural.
The method of treating bladder cancer using organ-sparing surgery is possible in a small percentage of cases, since bladder cancer is not often diagnosed in the early stages. To increase the success of bladder cancer treatment by partial cystectomy, additional treatment may be prescribed - brachytherapy (internal radiation therapy).
Operation TUR
For superficial small malignant tumors, transurethral resection (TUR) is also performed - removal of part of the bladder. In fact, this is a partial cystectomy operation, only not through laparoscopic access in the abdominal cavity, but through the urinary canal (urethra). More often, this type of surgery is used to remove benign types of bladder tumors and bladder polyps.
After such a procedure, chemotherapy or brachytherapy is often prescribed to prevent relapse and the formation of metastases, since this is an organ-conserving operation. If several malignant cells were not removed, chemotherapy or radiation therapy should destroy them.
With the help of such a cyber-assistant, radical and partial cystectomy is performed using the laparoscopic method. In Germany, operations using the da Vinci robot are performed not only to treat bladder cancer, but more often to remove prostate cancer and colon cancer, as well as other cancerous tumors.
- the surgical field is enlarged 10 times through images from several video cameras (3D);
- scaling of the surgeon's movements: a movement of the doctor's hand of 4 mm is transmitted as a movement of the robot's hand with an amplitude of 1 mm. This increases the thoroughness and accuracy of manipulations during surgery;
- greater freedom of movement: a conventional laparoscope has 3 degrees of freedom, the da Vinci robot has 7 degrees;
- the slightest random trembling of the surgeon’s hand is filtered, literally, by the robot’s hand;
- miniature size of scalpels - a few millimeters;
- the diameter of the punctures for instruments is even smaller: the muscles are not damaged, because the muscle fibers simply move apart; Only the skin and subcutaneous tissue are pierced;
- operation time is reduced;
- Recovery after bladder cancer removal is also faster.
In addition, there is additional protection: the robot's manipulator arms are active only if the surgeon's head is precisely positioned in relation to the monitor - behind the control panel. Thus, if the doctor turns away from the monitor, the da Vinci robot's manipulators will become inactive.
Preparatory stage
Before issuing a referral for transurethral intervention, the doctor will necessarily send the patient to undergo related tests. This makes it possible to identify previously undetected chronic diseases, information about which is not in the patient’s medical record.
During preparation, it will not be possible to do without an external examination, studying the victim’s complaints, questioning for the presence of congenital pathologies or bad heredity. At the same time, traditional external examination is usually carried out in two ways, depending on the gender of the applicant:
- women have the potential affected area examined through the vagina;
- men are examined through the rectal opening.
Such a superficial examination helps to establish the approximate diameter of the formation, as well as determine the stage of its progress.
If a lump is nevertheless found in the bladder area, then the victim is assigned to undergo a series of minor differential tests:
- biopsy of the extracted sample;
- urine cytology;
- clinical study of flushing from the area of the affected organ;
- cystoscopy;
- scyptigraphy of dynamic and statistical type;
- Ultrasound examination of the bladder and surrounding organs.
Separately, the feasibility of organizing the inoculation of biological material from the urethra with transfer to a nutrient medium in the laboratory is considered.
Blood parameters are also taken into account during the general analysis. With their help, it is possible to accurately determine the quantitative and qualitative value of platelets, red blood cells and the hemoglobin threshold.
If we are talking about a tumor of relatively modest dimensions, then it often chooses the mucous membrane as its location. Due to this, TUR can be carried out quickly and with minimal risk of possible negative consequences.
To prescribe a more effective format of care, doctors have introduced a special classification of all bladder tumors. Thanks to her, it is possible to quickly understand what preparation suits a particular patient best. But if the formation has grown very large, simultaneously damaging the internal organs located next to the bladder, then this aggravates the clinical picture. In addition to the analyzes described above in the preparatory phase, the following is added:
- magnetic resonance therapy;
- computed tomography;
- X-ray examination.
You will have to come to terms with the fact that the operation must be postponed if biochemical tests have demonstrated the presence of pathogenic pathogens of an infectious type. First you will have to rid the genitourinary system of their presence, and then enjoy the privileges of the transurethral method.
To correct the situation, you will need to undergo a course of treatment with antimicrobial medications and antibiotics. They are prescribed by a urologist based on the individual characteristics of the patient’s body. That is why it is forbidden to change the dosage of medications, the dosage schedule, or try to change the dosage on your own.
People with chronic illnesses deserve special attention at the preparatory stage. They will need to consult with their doctor ahead of time about temporarily stopping their usual medications if they are working on a blood thinner. But without obtaining the doctor’s approval, quitting the course of treatment on your own is strictly prohibited.
The last meal should take place no later than the evening before. And on the day of the operation you will need to give up breakfast and even drinking drinks. If you ignore this rule, you may run into risks of improper action of anesthesia.
It would be useful to conduct an allergy test in advance for the composition of the anesthesia if the person has not previously been exposed to it. This will prevent sudden anaphylactic shock from developing.
What is transurethral resection of the bladder
If disorders associated with the occurrence of pathological neoplasms are diagnosed in the bladder, and the organ ceases to perform its functions, it is important to determine in time what caused this condition.
Transurethral resection of the bladder is a universal operation, during which not only the tumor is eliminated, but also tissue samples are taken for analysis to make an accurate diagnosis. Modern technologies make the operation quick and efficient. Let's consider what a TUR of the bladder is and what are the features of this type of treatment.
The patient must be carefully prepared for bladder surgery using the resection method. Training is carried out in a hospital setting under the supervision of a specialist.
The patient goes to the hospital 5-7 days before the planned operation. During this time, he passes all the necessary tests. Both tumor cells and tissues from other parts of the organ are examined. If there is a suspicion of an invasive type of neoplasm, when the affected cells penetrate through the surrounding tissues and spread to healthy areas of the organ, then the patient is prescribed an MRI with contrast. This examination will provide a detailed picture of the condition of the damaged bladder and neighboring areas.
Additional diagnostic methods are used: chest X-ray examination and electrocardiogram.
At each stage, the operation is supervised by an anesthesiologist (anesthesia is necessary due to the pain of the procedure itself). He selects the appropriate type of anesthesia based on the patient's general health.
If the operation is planned in the morning, the patient is given an enema the night before and the hair in the groin area is removed. The consumption of any products is prohibited.
Before the operation in the morning, the patient must be given intravenous antibacterial drugs to prevent the development of infection.
On the eve of the procedure, the patient signs consent to undergo surgery. The doctor explains in detail what kind of process the patient will undergo, how the operation is performed and what complications are possible.
This is a cystoscopic resection most commonly used to treat superficial tumors. It is sometimes used when there is minimal invasion of the bladder wall or to remove most of the growth before other treatment is involved. TUR with fulguration is performed using local, spinal and general anesthesia.
The surgeon inserts the cystoscope through the urethra and into the bladder. Removes the tumor using a special instrument inserted through a cystoscope. Some healthy tissue around the tumor is also resected. The doctor takes a sample of the bladder wall for testing to see if the cancer has invaded the muscles of the organ.
The base of the tumor is treated with high-energy electricity (fulguration) or laser to destroy any remaining abnormal cells.
This is an operation for bladder cancer, during which the tumor and part of the bladder around it are removed. It is performed under general anesthesia. Segmental cystectomy may only be an option for some patients. Contact her if:
- The low-grade tumor had invaded only one area in the bladder wall.
- The small, solitary mass is located in a location where it can be easily removed with clear surgical margins. There is no carcinoma in situ in other parts of the organ.
- The tumor occurs in a diverticulum, an abnormal protrusion of the wall of the bladder.
- The patient is not in good enough shape to undergo more extensive surgery for bladder cancer.
The functioning of the organ is preserved, the patient will be able to urinate in the usual way. But its size will decrease, and you will have to visit the toilet more often.
This surgery for bladder cancer involves complete removal of the bladder and resection of the surrounding fatty tissue and adjacent lymph nodes. Performed under general anesthesia. In addition, in men, the prostate, seminal vesicles, and part of the urethra are also removed - radical cystoprostatectomy. In women - the uterus, cervix, fallopian tubes, ovaries, anterior vaginal wall and urethra - anterior exentaration of the small pelvis.
Cancer grows into the muscle layer of the bladder wall. Frequent recurrence of superficial tumors, despite transurethral resection and intravesical therapy. The malignant tumor has invaded the muscular layer of the organ and cannot be removed by partial cystectomy, since the main part of the bladder is involved, or there are several pathological foci.
When the bladder is removed, reconstructive surgery is used to create a new organ to hold and drain urine.
It is also possible to perform surgeries for bladder cancer using a laparoscopic approach (minimally invasive), as well as using robotic technology - the da Vinci robot.
Request a free call
Surgery for cystocele
In women during menopause, the concentration of estrogen and their effect on the body decreases. Receptors for hormones are found in adipose and connective tissue, skin, and vagina. Their deficiency leads to the appearance of wrinkles, sagging skin, and a decrease in the tone of the pelvic muscles. The result is prolapse of the bladder or its displacement.
The indication for intervention would be complete loss. To restore the functions of the pelvic floor muscles, a bioinert mesh is used, which is sutured laparoscopically. After the operation, the patient is under observation for 1–2 days and can return to a full life. At home, she is advised to take a course of antibiotics.
Planned preparation for surgery
Operating urologists know that the postoperative course, and often the success of the operation itself, depends on the patient’s preparation. Therefore, much attention is paid to the interpretation of tests and expert opinions regarding concomitant pathologies.
For a month it is proposed to give up alcoholic beverages, strong coffee and tea, and stop smoking.
Some patients require a 7-day course of antibiotic therapy or other anti-inflammatory drugs to ensure that there is no pathological flora in the urinary tract. For others, on the contrary, stop taking medications, for example, those with a thrombolytic effect (Cardiasc, Cardiomagnyl).
For 3 days, a semi-liquid diet is proposed, without foods containing fiber. On the last preoperative day, you are only allowed to drink water. Typically, the proposed procedure for the operation is known to the attending physician. He should explain all the steps to the patient in detail. Only after this is consent signed.
In cases of simultaneous formation of ducts for excretion of urine through the ureters into the intestine, isolation of part of the intestine for bladder repair, or creation of artificial fistula tracts, special attention is paid to intestinal preparation:
- siphon enemas are done for three days in a row for the purpose of maximum cleansing;
- a tincture is prescribed that inhibits intestinal motility.
Some doctors use prophylactic medications with bifidobacteria and lactobacilli with good results.
Before surgery, it is important to cleanse the intestines of toxins.
The evening before the operation, the nurse prepares the “operative field”: she shaves the hair in the perineum, in the genital area, above the pubis. You are not allowed to drink liquid at night or in the morning.
Since surgery requires general anesthesia, the patient is examined by an anesthesiologist who:
- determines the working blood pressure;
- checks ECG results;
- asks again about previous reactions to medications.
All cases of allergies or suspected allergies should be reported to your doctor. If you have removable dentures, they are removed from your mouth.
Preoperative preparation
It is necessary to carefully examine the patient in order to reduce the risk of death and postoperative complications. The activities are typical for preparing for any surgical intervention, but there are some specifics.
Research and analysis
Recommendations on the necessary studies, tests and preparation for surgery can only be given by the attending physician!
General and biochemical blood tests. They make it possible to identify infectious and inflammatory processes.
Direct preparation
- two weeks before it is necessary to stop taking certain medications: Aspirin and others;
- a week before surgery, the patient is switched to a low-fiber diet;
- for two days it is forbidden to eat and it is recommended to drink more;
- hygienic treatment of the groin area is mandatory;
- a day before, a cleansing enema and diuretics are prescribed in order to “drive” excess fluid from the body;
- Smoking and drinking alcohol are prohibited 12 hours before;
- You should not drink liquids the evening before surgery.
The preparation doesn't end there. Almost two weeks later, the doctor prescribes the man a course of antibiotics to prevent secondary infection and prebiotics to normalize the intestinal microflora. In addition, such measures are necessary to prepare the gastrointestinal tract: it is possible to use part of it to drain urine.
What is taken into account during emergency intervention?
Most often, bladder tumors are detected in men after 60 years of age. Examination and treatment are carried out as intensively as possible. This is necessary to preserve the surgical method as a backup option. It happens that during therapy massive bleeding begins. Therefore, in order not to reduce the patient’s blood loss, a decision is made on emergency surgery.
Bladder resection
There is no time to carry out full preparation. The patient ate regular meals without following a diet. To cleanse the stomach, it is lavaged using a gastric tube. The enema is given in a “soft” version with a small amount of liquid so as not to increase bleeding.
It is mandatory for the patient to have an ECG taken, examined by a therapist, and checked:
- general blood and urine analysis;
- blood type and Rh factor;
- electrolytes;
- liver tests;
- residual nitrogen indicators.
The anesthesiologist examines the patient, clarifies all questions, and, if necessary, recommends prophylactic administration of medications.
Cystolithotripsy
The crushing of stones is called cystolithotripsy. The intervention is often combined with cystolitholapaxy - stone removal. The procedure is performed if the stone creates an obstruction to the outflow of urine.
Sometimes stone removal is the first step in surgery on the bladder neck or urethra. For older men, this procedure serves as preparation for transurethral resection of prostate adenoma. It can also be performed if surgical treatment is refused.
Cystolithotripsy is contraindicated:
- inflammatory diseases of the genitourinary organs;
- stones are fixed with a ligature or in a diverticulum;
- inability to insert instruments through the urethra;
- bladder tumors;
- large stones more than 4 cm.
Anesthesia, parabulbar or presacral anesthesia, and local anesthesia are used as anesthesia.
The patient is placed on a urological chair. The bladder is flushed through the catheter. A cystolithotripter with an obturator at the end is inserted through the urethra. The obturator is then removed and the endoscope is advanced. Up to 350 ml of liquid is injected into the bladder. Be sure to inspect the cavity from the inside and determine the location of the stone. It is then captured and brought to the center of the bubble, where fragmentation is carried out.
During manipulation, you constantly have to rinse the cavity of the bladder, as the liquid becomes cloudy. After crushing is completed, a control cystoscopy is performed to make sure that there are no stones left and there is no damage to the walls.
Progress of bladder removal surgery
The cystectomy technique is followed consistently:
- A permanent catheter is installed in the bladder.
- An arcuate or anchor-shaped skin incision is made above the pubis (if necessary, with an anchor-shaped one, it is possible to quickly ligate the internal iliac arteries to stop bleeding).
- The covering part of the peritoneum is peeled off or removed, the cavity of the bladder is opened and its revision is carried out. The vessels are ligated.
- The back and side walls are distinguished. In male patients, the posterior surface of the seminal vesicles and prostate gland are released from adjacent tissues.
- The ureters are cut 2.5-3 cm above the cancerous tumor and fixed with special holders. Special catheters are inserted inside the ureteral tubes.
- The vas deferens are ligated. The bladder is moved up and back and bandaged.
- The puboprostatic and pubovesical muscles and ligaments are transected on both sides, and the portion of the urethra lying below the prostate is removed.
- The bladder is removed.
The intervention is carried out by qualified specialists after preparing the patient
In the peritoneal cavity, bleeding is stopped by ligating the vessels, and the peritoneal defect is sutured. Layer-by-layer sutures are applied to the muscles and skin. Ureteral catheters are brought out. A drain (tube) is left in the abdominal cavity and pelvis for postoperative observation and administration of antibiotics.
Traditional method
A radical type of bladder removal in men involves, in addition to excision of the bladder itself, removal of other organs of the genitourinary system. As for a similar procedure in women, it also includes excision of part of other organs that form the reproductive system and urinary system.
The procedure begins with the use of anesthesia. Next, the patient is placed in a certain way on the operating table. Men are simply placed on their backs, while women must assume a supine position with their legs positioned on a special stand. At the next stage, a catheter is inserted into the bladder and an incision is made from the pubis to the navel.
When performing a radical cystectomy, the surgeon adheres to several simple principles:
- Adherence to the radical principle. In one fell swoop, the entire urinary cavity and nearby lymph nodes are excised.
- Compliance with the principle of ablistics. Surgeons do not allow the possibility of cancer cells spreading to other body systems.
- Compliance with the anti-blast principle. Surgeons completely excise the entire malignant tumor and treat the wound with an alcohol solution.
After complete excision of the urinary tract, specialists will begin to form a new pathway for urine excretion. Next, the surgical team closes all the incisions and leaves the catheters. After the operation is completed, the patient will be sent to the ward, where he will spend about a week until the end of the initial recovery.
What complications can you expect?
The most dangerous complications of cystectomy are:
- bleeding from pelvic vessels;
- rectal damage;
- infection in the abdominal cavity with the development of peritonitis;
- ureteral obstruction with urine retention;
- development of fistula tracts;
- tumor recurrence.
Bleeding is eliminated by local ligation of blood vessels. If this measure is not possible, ligation of the trunk of the internal iliac artery is performed. Apply 2 ligatures with a distance of 0.5 cm between them.
Undesirable consequences are determined by the type and location of surgery, the general physical fitness and health of the patient, and the effects of other therapies (for example, tissue exposed to radiation may not heal properly after surgery).
- Pain is a consequence of tissue injury. Painkillers are used to control it. It may take some time for the pain to subside, depending largely on the procedure performed and the patient's pain threshold.
- Vomiting and nausea are consequences of general anesthesia. Medicines are often used to eliminate them.
- Hemorrhage or bleeding may rarely occur after surgery. It is normal to have a small amount of blood in the drain.
- After surgery for bladder cancer, problems with the urinary tract are possible. Some drugs used in anesthesia and pain medications may cause the inability to urinate. Repeated TUR can cause scarring in the bladder and lead to incontinence. After a partial cystectomy, due to a decrease in the size of the organ, more frequent urination is observed. After radical cystectomy and reconstruction, side effects such as urinary incontinence, blockage of the ureters, and backflow of urine into the ureters (reflux) are possible.
- Surgery in the pelvic area sometimes provokes intestinal irritation, causing various disorders. Paralytic intestinal obstruction occurs as a result of anesthesia, when the contents of the organ do not move. Food and fluid intake is gradually resumed after surgery. Narrowing (stricture) of the rectum is possible and is treated with dilatation (widening) and, in serious cases, surgery.
- With any type of surgery, wound infection is possible. A drain is placed in the wound area to drain excess fluid. Urinary tract infections after surgery for bladder cancer can be a complication. Such repeated infections develop with obstruction or reflux of the ureters and can provoke chronic pyelonephritis. To prevent and treat them, they resort to antibacterial therapy.
- After surgery for bladder cancer, stones may appear in the kidneys or the reconstructed bladder. It is important to drink plenty of fluids. If the condition does not improve, surgery may be necessary.
- Stenosis or narrowing of the stoma is a late complication that occurs as a consequence of ileal conduit. The disease is treated with dilation (widening) of the stoma.
- The formation of a hernia around the stoma can also be a late complication of ileal conduit. Surgery will be required to eliminate it.
- After reconstructive surgery, metabolic disorders are possible, for example, an imbalance of electrolytes - potassium and sodium. If necessary, supplements are prescribed to bring their levels back to normal.
- Reproductive disorders are a consequence of radical cystectomy, which changes the functioning of the reproductive system - infertility in women and erectile dysfunction in men. As the size of the vagina decreases in women and sensations during sex change, it happens that sexual intercourse is no longer possible.
After resection, various complications are possible that require medical consultation. These include:
- prostatitis;
- damage and inflammation of the bladder neck;
- cystitis;
- purulent urethral infection;
- narrowing of the urethra (stricture), interfering with the normal flow of urine.
After resection, the patient must be constantly monitored by a doctor and examined to monitor the condition of the operated area. The first postoperative examination is carried out three months later, subsequent ones - on the recommendation of the doctor. If the tumor is malignant, other specialists are involved in the treatment.
Complications and consequences
If left untreated, OAB syndrome can lead to negative consequences:
- Reducing or completely abandoning physical activity.
- Problems in personal life, lack of sex.
- Complexes due to the need to take additional measures to maintain hygiene.
- Refusal of social contacts, isolation, depression.
OAB syndrome leads to severe psychological disorders, which gradually affect the physical condition.
How does the postoperative period proceed?
After radical cystectomy, the patient is in the intensive care unit and then transferred to the urology department. You are allowed to get up and walk from the second day. Breathing exercises are recommended to prevent congestive pneumonia. If necessary, the doctor prescribes antibiotics intramuscularly.
For three weeks, urine is drained through a catheter. The drainage tube is removed after a few days if there is no discharge in it. The patient receives nutrients and fluids through intravenous systems. The intestines do not work for the first days. When peristalsis (motor activity) is restored, the patient is allowed to feed on his own.
Normal hospitalization requires 12 days. The patient is discharged with a urinary catheter. Its removal is carried out after 10 days, for which the patient returns to the department.
You can buy urine collection bags at the pharmacy.
The postoperative recovery period is of great importance for the patient's health. Failure to follow the doctor's recommendations can lead to relapse and complications.
The patient is treated for three days with special disinfectant solutions injected through a catheter into the bladder. The time to use the catheter is determined individually - from several hours to several days, as long as there is blood in the urine.
If after the operation the patient’s condition is stable, there is no vomiting, no feeling of nausea, and no severe pain, you can drink a little liquid - still water (about 1.5 liters during the day).
Eating is allowed the next day. The patient must adhere to a diet after bladder surgery, observing some restrictions. Dishes prepared by smoking and frying, as well as spicy and salty foods are prohibited. A large amount of liquid, on the contrary, is recommended: you can drink 2-3 liters per day. If the patient has concomitant diseases, the diet can be adjusted.
Taking antibiotics is a mandatory component of therapy in the postoperative period. Before prescribing medications, it is necessary to take into account possible side effects from taking the drugs, as well as the presence of individual intolerance. After the catheter is removed, the patient may experience urinary problems:
- burning and pain;
- urination in fractional portions;
- imperative urges.
These symptoms should disappear within a week. If symptoms do not disappear, this is a serious cause for concern.
Biopsy results are ready 7-10 days after surgery. If the tumor turns out to be malignant, the patient must continue treatment with an oncologist. The doctor will advise you on further actions.
Rehabilitation after a TUR of the bladder ends when the patient is already at home. During this time, he must follow all the doctor’s recommendations, eat properly according to the diet, do not lift weights, and refuse intimate relationships during recovery.
The time it takes for the bladder to heal after TURBT surgery is individual in each case. For men, the rehabilitation period lasts longer.
Symptoms
The predominant signs of OAB are increased daytime and nighttime urination (“dry” OAB). The urge is so strong that it is almost impossible to endure. As a result, a person goes only to those places where there is a toilet, since he has to look for it every 1-2 hours.
A more severe manifestation is urge incontinence - involuntary loss of urine immediately after the urge (“wet” OAB). In approximately 1/3 of patients, OAB symptoms spontaneously subside and also recur for no reason. The most persistent symptom is frequent urination, which reaches several dozen times a day.
Urologist, dermatovenerologist Sergey Gennadievich Lenkin learn more about how OAB manifests itself in men
Symptoms of OAB become more pronounced after drinking large amounts of liquid or alcohol, as well as when overeating, obesity, and taking certain medications.
Methods for forming urinary diversion
The next stage of surgical treatment is the formation of urine excretion pathways. To do this, one of the methods is used in each specific case. The choice of operation depends on:
- on the age of the patient;
- surgeon experience;
- the patient's wishes;
- general condition after radical cystectomy;
- complications of radiation or chemotherapy;
- prognosis of the course of the tumor.
The greatest success in the practice of urologists is characterized by two urinary diversion operations:
- according to Bricker - the application of an external urostomy or its connection to the intestine;
- according to Studer - the formation of an artificial bladder.
The advantages and disadvantages of the methods are visible from the table
| Type of operation | The essence | pros | Minuses |
| according to Bricker | The ureters with inserted stents (so as not to collapse) are sutured to the intestine using a section of the small intestine, the other end is brought out to the skin near the navel and a stoma is formed. |
|
|
| according to Studer | A urinal bag is formed from a 65 cm long section of the ileum on a “vascular pedicle”. A catheter is inserted into it through the urethra. The ureters with stents are sutured to the “new” bladder. After 2 weeks, all catheters, drains and stents are removed. |
|
|
This is how the ureters are sutured to a section of the intestine from which a urinal is obtained.
The Studer procedure is more modern and preserves the patient's quality of life, but it is not suitable for everyone. Contraindications are:
- addition of chronic renal failure;
- liver failure caused by cirrhosis or chronic hepatitis;
- intestinal diseases accompanied by dysfunction;
- partial or complete removal of the urethra with damage to the sphincter;
- dysfunction of the anal sphincter;
- decreased intelligence of an elderly person;
- undergone course of radiation therapy;
- the presence and consequences of neurological diseases.
In these cases, only the Bricker method is used.
Artificial bladder surgery is not recommended for older people over 70 years of age due to age-related sphincter weakness and an increased likelihood of persistent urinary incontinence. For women, a radical cystectomy removes the entire urethra. This makes it difficult to create an artificial reservoir.
Classification of surgical interventions
Bladder surgeries (UB) include:
- Bladder drainage operations (trocar and open cystostomy).
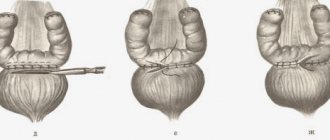
Trocar epicystostomy is performed from a small incision above the pubis, under ultrasound guidance. To insert a catheter into the cavity of the bladder, a special stylet with a mandrel is used: after puncture of the bladder, the stylet is removed, and a catheter is inserted into the lumen of the bladder along the mandrin (Fig. 1).
Rice.
1 – Placement of trocar epicystostomy. Source - [1] Open epicystostomy is performed when the surgeon has no experience in performing a trocar cystostomy, the necessary tools, or an ultrasound sensor.
Indications for epicystostomy:
- 1Acute urinary retention in combination with the impossibility of transurethral placement of a catheter into the bladder cavity.
- 2For chronic urinary retention - for long-term urine diversion, or when preparing the patient for surgery.
- Operations for drainage of the paravesical space. Depending on the severity of the bladder injury, it may be necessary to place drains in the paravesical space. The number of drains and the method of their installation depend on the nature of the operation, its volume and the likelihood of postoperative complications (bleeding, urine leakage).
- Operations to remove stones and foreign bodies from the bladder. Often operations are performed through cystoscopy (a cystoscope with the necessary instruments is inserted through the urethra into the cavity of the bladder). In rare cases, open surgery is required.
- Operations for removing diverticula and hernias of the bladder. These interventions are increasingly performed laparoscopically.
- Prompt repair of damage to the bladder wall. Depending on the patient’s condition and the severity of the injury, suturing of the bladder defect can be performed either openly or laparoscopically.
- Operations to remove tumors of the bladder. Removal of neoplasms of the bladder wall can be carried out by all available methods: transurethral, open and using laparoscopy. The choice of one or another technique depends on the nature of the neoplasm, localization and prevalence of the process. Often, tumors may require resection of the organ wall or its complete removal.
- Operations to close vesical fistulas.
- Reconstruction of the urine reservoir from a segment of the intestine is performed during extirpation of the bladder.
- Surgical treatment of neurogenic MP.
Based on invasiveness, surgical interventions are divided into:
- 1Open operations. Open operations are traumatic, as they require large incisions in the skin and muscles of the anterior abdominal wall. Increasingly, minimally invasive methods are being used instead of open surgical interventions.
- 2Minimally invasive operations (laparoscopy, transurethral surgical interventions).
Forecast
TUR is a complex procedure, after which the patient's condition may worsen. The following phenomena may be of concern:
- in the first days after resection, pain occurs in the area of the urethra;
- blood appears in the urine.
These symptoms are not dangerous. This is a normal reaction of the body to surgical procedures.
You should see a doctor if:
- body temperature stays around 38 °C and above;
- severe pain does not go away;
- discomfort occurs during urination;
- For more than a week, blood clots appear in the urine, it is cloudy and smells unpleasant.
During the procedure, there is a possibility of bleeding, venous blood clots, wounds and damage to the urethra and bladder walls. This risk is minimal if all the rules of the operation are followed and there are no concomitant chronic diseases.
The effectiveness of bladder surgery and the possibility of relapse are influenced by many factors:
- degree of organ damage;
- the occurrence of complications;
- patient's age;
- general health;
- the technique underlying the therapy used.
Life after surgery
To avoid unpleasant consequences, you need to drink plenty of fluids after surgery. The diet should be balanced, but you should avoid eating the following foods:
- sorrel and spinach;
- fruit juices;
- dairy products;
- marinades.
The diet immediately after open access surgery is chemically and thermally gentle; fried and spicy foods are avoided. Preference is given to slimy porridges, steamed lean meats, and boiled vegetables.
After the bladder is removed, the ureters can be drained out and the urine is collected in a urinal. In this case, careful personal hygiene is necessary to avoid infection of the kidneys through the ascending route and the appearance of the accompanying unpleasant odor of urine. Sometimes they resort to restoring the bladder through plastic surgery from the intestine. In this case, the patient does not lose the ability to urinate in the traditional way.
Other types of cystectomy
In specialized clinics with high-tech equipment, the classic version of cystectomy is replaced by radical laparoscopic surgery. Laparoscopic radical cystectomy is performed under general anesthesia through several punctures in the abdominal cavity. A laparoscope with a video camera is inserted into them.
Special surgical instruments allow you to carefully ligate the vessels, isolate, and then cut out the bladder. A drainage tube is left in the pelvic cavity for monitoring. Preparation and postoperative management do not differ from the classic version. To restore the outflow of urine, the already listed interventions are carried out according to indications.
Nerve-sparing cystectomy is characterized by careful control of the nerve endings responsible for connecting the spinal cord with the genital organs and sexual function in men. Young people without tumor metastasis most often undergo this intervention. The operation prevents subsequent impotence and preserves the nerves of the cavernous bodies.
What anesthesia is the operation performed under?
The most commonly used general anesthesia is endotracheal (intubation) anesthesia. With this anesthesia:
- The patient's airway will be completely patent, regardless of the position on the operating table;
- Prevents stomach contents from entering the airways;
- Despite prolonged anesthesia, the toxic effect of the drugs on the patient is minimal;
- The operation is facilitated by relaxing the muscles of the anterior abdominal wall (it becomes easier for surgeons to reach the bladder).