Prolapse of the wall through the hernial orifice is called a bladder hernia. The disease occurs in women and men. A hernia is manifested by painful and frequent urination, a feeling of incomplete emptying of the bladder. This disease brings a lot of inconvenience to the patient’s life and also leads to dangerous consequences. Therefore, if the first manifestations of the disease occur, it is necessary to contact a medical institution, undergo examination and begin treatment.
A bladder hernia can occur for various reasons and this phenomenon is very dangerous if complications develop.
Bladder hernia: symptoms and diagnosis
In patients with this pathology, two-stage urinary bowel movements are observed. The urine itself is cloudy in color, and signs of cystitis may be observed. The hernia itself increases in size before going to the toilet due to the accumulation of urine in the bladder, part of which bulges out.
Diagnosis of the disease is carried out using modern medical equipment:
- cystoscopy;
- cystography.
Any bladder hernia must be removed surgically. This is the only effective treatment for this pathology. Most often, this disease occurs in older men. It significantly worsens the quality of life of an elderly person and is a risk factor for the development of dangerous inflammatory diseases.
Treatment of bladder hernia: surgery at the First Surgery clinic
A successful operation to remove a urinary hernia of any location can be performed at the First Surgery clinic. Experienced specialists, using modern laparoscopic techniques and the latest medical equipment, will quickly set the bladder to its original place and strengthen the hernial orifice. Carrying out an operation in this clinic guarantees a complete cure for such a dangerous pathology.
A bladder hernia is a pathological process marked by the loss of any part of its wall.
This is possible in the presence of weak (thin) walls of the organ, which are also called “hernial orifices”.
The reasons why such a serious disease occurs are reflected in many medical sources. But it is impossible to say that the list is complete, since the disease and its causes have not yet been fully studied.
Extreme stretching of the bladder can contribute to the appearance of a hernia. This happens because the diameter of the urethra sharply narrows, affecting the decrease in the tone of the organ.
In men, a significant reason may be an adenoma, which is a serious obstacle to the timely outflow of collected urine.
The cause may be weak muscles, most often this condition is typical for women whose abdominal muscles have fallen into complete decline during pregnancy.
Not only men, but also women suffer from difficulty urinating due to diseases of the female genitourinary system.
The hernia leads a secretive existence, not showing any characteristic signs, not making itself known at first.
The patient can only find out about its presence when undergoing an ultrasound or other instrumental diagnostic measures.
And, nevertheless, there are symptoms that help predict the development of a hernia and, accordingly, allow you to consult a doctor in a timely manner and undergo an examination.
Bladder hernia is characterized by symptoms:
- changes in the size of the protrusion;
- incomplete emptying in one act;
- severe pain when urinating;
- frequent urge;
- urinary incontinence in rare cases.
Very often, patients name characteristic symptoms that indicate the presence of a problem. They claim that the process of emptying the bladder is faster and easier if at this moment you press on the area of the protrusion.
Naturally, direct pressure on the hernia causes urine to flow out of it, heading initially into the bladder, and then further out.
Due to the fact that urine accumulates in the hernia for a long time, infection occurs, which subsequently turns into purulent stagnation, worsening the patient’s condition.
The hernia has different sizes. With small sizes, a person can feel it only in a state of extreme tension, and with excessively large sizes, it is observed even in a complete state of rest.
Inguinal hernia in boys
A congenital inguinal hernia in boys can be diagnosed in the first weeks of life. It is manifested by the appearance of a tumor-like protrusion in the groin area, which increases when the child cries and strains, and when the baby sleeps, in a relaxed state, it almost completely disappears.
With an inguinal-scrotal hernia in boys, there is an asymmetry in the structure of the scrotum due to a clear increase in one half of it.
According to the characteristics of the clinical course, inguinal hernias can be uncomplicated or complicated.
Strangulation of an inguinal hernia in boys threatens the development of serious complications (peritonitis, intestinal obstruction). In approximately 5-7% of boys, strangulation of the inguinal hernia leads to testicular atrophy and a decrease in reproductive abilities in adulthood, including the development of infertility. Therefore, it is very important to promptly identify and treat inguinal hernias in boys, preventing them from being strangulated.
Diagnosis and treatment
The process of diagnosing a hernia is absolutely simple and does not present any difficulties.
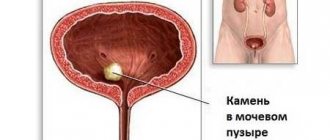
Bladder pathologies
Modern medicine uses ultrasound, cystography and cystoscopy for diagnostic purposes.
Cystoscopy allows you to see the location of the hernial sac, determine the degree of depletion of the walls, and also determine the condition of its mucosa.
Cystography is carried out using a radiopaque substance, which is injected into the bladder before using the device.
Such a study allows us to determine the nature and level of protrusion.
A timely examination allows the treatment process to begin in a timely manner, since a hernia is not as harmless as it seems at first glance.
Due to its presence, a person may acquire additional problems in the form of pinching, neoplasms or the formation of stones.
Treatment consists almost exclusively of surgical intervention.
Cystoscopy
In cases where all symptoms indicate the presence of a small hernia, and the patient’s health does not allow surgical intervention, wearing a bandage is recommended.
If a hernia was identified during the operation, the doctor removes it, with the obligatory installation of a catheter in the bladder in order to ensure a calm outflow of urine without overstraining the walls of the urinary organ.
Otherwise, the sutures placed during surgery may simply come apart.
The most complex operations that require special skills from the surgeon are operations to remove recurrent hernias.
The situation is even more complicated if such hernias have a wide gate. The removal site is carefully sutured and drains are installed, since ignoring this step can lead to disastrous results, even death.
In order not to aggravate the situation, only after identifying the symptoms characteristic of bladder hernias, you should immediately consult a doctor.
A timely operation and compliance with all recommendations will allow you to forget about problems and continue to live a healthy and happy life.
The disease hernia of the bladder is associated with a protrusion of a section of the wall of this organ. This prolapse occurs through the hernial orifice - weak areas of the abdominal wall. Such gates can be the inguinal fossae, the umbilical ring, postoperative scars, areas whose integrity is compromised as a result of various injuries or pathologies.
It should be noted that in males such hernias develop approximately four times more often than in females.
Experts distinguish these types of hernias, depending on the location of the bladder prolapse:
- Inguinal;
- Perineal;
- Femoral;
- Obturator;
- Hernia of the white line of the abdomen.
In addition, protrusions are also usually divided depending on their location relative to the peritoneum:
- Intraperitoneal, which are located in the hernial sac formed by the peritoneum;
- Periperitoneal, which are in contact with the peritoneum;
- Extraperitoneal, not in contact with the peritoneum (see photo).
Statistics show that peritoneal hernias account for half of all registered pathologies.
The picture shows a diagram of a bladder hernia
Recipes
Prickly tartar. You need to take 20 grams of raw material, pour boiling water over it (1 glass). Leave for about forty minutes. Drink a tablespoon three times a day. In addition to the infusion, you can also take the powder of this plant. Tatar leaves are famous for their diuretic effect, as well as their ability to relieve inflammation.
Dill seed + Tartar. To obtain this miraculous mixture, you should use 1/3 tablespoon of tartar seeds and leaves. The mixture is poured with boiling water directly into the thermos. Leave for about one hour. Take 4 times a day, ¼ cup. The course lasts a month. No more than six such courses can be conducted per year.
Mint. This aromatic herb, beloved by many, can cope even with advanced inflammation. It is collected during flowering. You will need 20 grams of dried herb. Fill it with boiling water in the amount of one and a half liters. Boil for no more than ten minutes. Drink mint one glass 3 times a day for a month.
Birch bark. Folk remedies for bladder inflammation can cure even if you take them as a drink. In this case we are talking about birch bark. They remove it from the branches in May. Then infuse for about six hours in drinking water. Cut a tablespoon and pour over boiling water in a volume equal to one glass. The mixture should boil for about twenty minutes. After this, let it sit for half an hour and filter. Drink as desired throughout the day.
A mixture of herbs. You need to mix in equal proportions juniper, arnica (flowers), steelhead (root), calendula (flowers), St. John's wort, bearberry and pear leaves. Then take a teaspoon of the resulting potion, pour a glass of water and bring to a boil. Let it brew for ten minutes. Strain and the infusion is ready for use.
Spurge. If you drink a decoction of this herb at the first sign, the effect will be noticeable immediately. For complex pathologies, courses must be repeated every ten days. The duration of the course itself is thirty days. The decoction is prepared like this. Take six tablespoons of the herb and pour it with a liter of hot water. Insist for an hour. You need to drink the entire prepared infusion within a day.
Corn silk. Folk remedies for bladder problems in women involve brewing corn silk. They will be effective at the first symptoms. To prepare a medicinal drink, you need not only stigmas, but also berry stems from cherries. You need to brew them in different containers. Then combine and add honey. This drink can be drunk instead of tea.
Fresh dill. And again about dill. This time you need fresh herbs. Pour a tablespoon with a glass of water. Boil and strain through cheesecloth. Drink on an empty stomach. The quantity of this decoction is unlimited.
Causes of bladder hernia and its symptoms
It must be said that modern medical science has not yet fully determined the circumstances due to which the disease occurs. The main factors contributing to the manifestation of a hernia include the following:
- Stretching of the walls of the bladder and its low tone due to narrowing of the urethra;
- Prostate adenoma, which prevents normal urine flow;
- Flabbiness of the abdominal wall;
- Weakening of the abdominal muscles as a result of pregnancy;
- Diseases of the female genitourinary area associated with difficulty urinating.
Most often, a bladder hernia does not manifest itself with any characteristic features, which would make it possible to distinguish it from other hernias (inguinal, femoral, and others). As a rule, such a pathology is diagnosed only during ultrasound, cystoscopy, cystography or surgery. Moreover, there are still a number of certain signs that indicate precisely this pathology.
These are the following symptoms:
- An increase in hernial protrusion when the bladder is filled and a decrease after it is emptied;
- Inability to completely empty the bladder at one time;
- Frequent and painful urination;
- Partial urinary incontinence.
In addition, patients pay attention to the fact that it is easier for them to empty their bowels if at this moment they press the hernia with their fingers, forcing the urine in it to flow into the bladder. Very often the pathology is accompanied by various urinary tract infections due to congestion.
The degree of protrusion may vary. In mild cases, the hernia is detected only during physical exertion, but in severe cases, the protrusion is present even at rest.
In men and women
The structure of the bladder is the same in representatives of different sexes. In men, the prostate is adjacent to the lower outer part of the bladder, and the seminal ducts are located on its sides. In women, the back of the bladder borders
and vagina.
A significant difference is observed in the length of the urethra. So, in men it is 15 centimeters or more long, and in women it is only 3 centimeters.
The female half of the population suffers from this disease several times less often than representatives of the opposite sex. This pathology is more common in women who have given birth, who gave birth by caesarean section, or when the abdominal muscles are severely stretched and weakened during pregnancy.
The cause of the development of such a disease in women can be other operations performed in the lower part of the peritoneum, as well as diseases of the genitourinary system associated with difficulty in the urinary process.
It is known that representatives of the stronger half of humanity suffer from bladder hernia much more often than representatives of the weaker sex - as a percentage, the incidence rate of both is 90% to 10%.
The reason for this trend is the peculiarities of male physiology and the anatomical structure of the groin region in men. The main causative agent of the pathology in this case is an exclusively male disease - prostate adenoma, which prevents the full and timely release of urine.
In old age, the risk of developing a hernia increases due to sagging abdominal muscle tissue.
Treatment methods for bladder hernia
Treatment of such a hernia is only possible through surgery. However, if the patient’s condition for some reason excludes the possibility of surgery, and the protrusion is small in size, then wearing a special support bandage is recommended.
The choice of surgical procedure will depend on the type of pathology, age and health status of the patient and the qualifications of the surgeon.
During the operation, the protrusion must be carefully separated from the hernial sac and sutured using a special suture. After this, a catheter is placed in the bladder for 5-7 days.
The video talks about foods that are good for the bladder:
You should absolutely not delay contacting a doctor, since the disease can be complicated by undesirable consequences, among which the most severe can be considered a strangulated hernia. It is much better to calmly perform the necessary operation as planned than to end up on the operating table in an emergency with the risk of developing necrosis of the bladder wall.
Rice. 3. Inguinal-scrotal hernia of the bladder
(cystogram).
A hernia of the bladder is called its prolapse through the hernial orifice (Fig. 3). More often there are inguinal, inguinal-scrotal and femoral hernias of the bladder, less often sciatic and perineal. Symptoms: hernial protrusion, changing its size depending on the degree of filling of the bladder, urination
in two doses, urinary retention, dysuria, pyuria.
Bladder
hernias are detected using cystoscopy (see) and cystography. Treatment is surgical. Wearing a bandage is contraindicated.
Circulatory disorders
There are arterial and venous (congestive) hyperemia of the bladder
.
Arterial is observed in diseases of the internal genital organs. Arterial hyperemia is most often localized in the area of the neck and triangle of the bladder. With arterial hyperemia, temporary urination disorders are observed without the presence of pathological elements in the urine. Venous (congestive) hyperemia in the bladder can be observed during pregnancy, prostate adenoma, pelvic vein thrombosis, and cardiovascular failure. During cystoscopy, the mucous membrane of the bladder
in the area of the neck and bladder triangle is bluish in color.
Sometimes you can notice multiple hemorrhages, the veins of the bladder are dilated and appear in the form of varicose veins. Urination
is impaired , and blood may appear in the urine.
The prognosis is usually favorable. Treatment of bladder circulatory disorders depends on the underlying disease. Bed rest is required. Anticoagulants, antibiotics, and sulfonamide drugs are prescribed for venous diseases (per os or parenterally). Bladder lavage is contraindicated in the acute period. In case of threatening bleeding, surgery with a high section of the bladder, hemostatic drugs, and blood transfusions are indicated. Gangrenous cystitis is manifested by acute pain in the bladder area, constant urge to urinate
, and hematuria. Subsequently, the temperature rises to high levels, difficulty urinating or complete urinary retention appears, intoxication increases, and the general condition progressively worsens. Recognition is facilitated by the presence of foul-smelling urine and the discharge of dead areas of the bladder wall. In severe cases, bladder rupture and peritonitis may develop. The latter can also develop in the absence of perforation of the cystic wall by contact or hematogenous means. The disease is complicated by paracystitis (see Cystitis), ascending purulent pyelonephritis (see). Treatment: application of a suprapubic fistula and removal of dead tissue. At the same time, measures are taken to eliminate intoxication and the causes that contributed to the onset of the disease. The prognosis is unfavorable. In cases of recovery, deformation of the bladder remains, wrinkling of the orifices of the ureters with disruption of their neuromuscular system and the development of vesicopelvic reflux (see).
Unfortunately, many women at a certain stage of life have to deal with such an unpleasant problem as cystocele. What it is? This is a hernia of the bladder that occurs when the supporting tissue between the bladder and the vaginal wall stretches, causing the bladder to protrude down into the vagina.
The main reason for this problem is stretching of the muscles that support the pelvic organs. Sprains can be caused by vaginal childbirth, chronic constipation, prolonged severe coughing, or heavy lifting. In addition, menopause, when estrogen levels in the body decrease, is considered an additional risk factor.
If a woman is diagnosed with a mild or moderate bladder hernia, doctors usually prescribe conservative treatment. In more severe cases, surgery may be required to keep the vagina and other pelvic organs in the correct places.
Forms of the disease
Inguinal hernias in men, depending on the characteristics of the anatomical structure, are divided into several types:
- Oblique. They can be either congenital or acquired. The hernial contents are located inside the structures of the spermatic cord along the inguinal canal. Oblique inguinal hernias, in turn, are divided into inguinal-scrotal (the hernial protrusion descends into the scrotum), cordial (the hernial sac is located in the inguinal canal at the level of the spermatic cord) and canal (the hernial sac is located at the level of the outer ring of the inguinal canal).
- Direct. This type refers to acquired hernias. They are characterized by the passage of a protrusion outside the spermatic cord through the inguinal space.
- Combined. They are quite anatomically complex formations, which consist of two or more hernial sacs passing through different hernial openings.
- Direct interstitial (subcutaneous). The hernial sac is located in the subcutaneous tissue of the aponeurosis of the external oblique muscle, without descending into the scrotum.
Inguinal hernias in men can be reducible or irreducible. With reducible hernias, the hernial protrusion may disappear, slipping back into the abdominal cavity. If the hernial sac becomes fused with the hernial contents, then the hernia becomes irreducible.
In men, the inguinal canal is wider and shorter than in women, so inguinal hernias in men are several times more common than in women.
Sliding inguinal hernias are also isolated. In this case, not only the parietal, but also the visceral layer of the peritoneum takes part in the formation of the hernial sac. Most often, the hernial contents of such inguinal hernias in men include the wall of the bladder.
If, after removal of an inguinal hernia in a man, the protrusion appears again, then such hernias are called recurrent.
According to the characteristics of the clinical course, inguinal hernias can be uncomplicated or complicated.
Symptoms
It is possible that with mild bladder prolapse, you will not even feel the development of a cystocele. Symptoms and signs of pathology can be expressed in different ways and usually include:
- a feeling of fullness or pressure in the pelvis and vagina;
- increased discomfort when straining, coughing, pushing, or lifting heavy objects;
- a feeling that you haven't completely emptied your bladder after going to the toilet;
- recurrent urinary tract infections;
- pain or mild urinary incontinence during sexual intercourse.
In severe cases, a piece of tissue may become noticeable protruding through the vaginal opening, and it may feel like you are sitting on a chicken egg.
Signs of pathology are especially noticeable after standing for a long time and may disappear after taking a lying position.
Characteristic symptoms
At an early stage, cystocele does not show symptoms at all, so it is extremely difficult to identify it. Patients often find out about the presence of a hernia during a routine ultrasound examination of the pelvic organs. As the hernia increases, the patient will begin to experience the following symptoms:
- urinary incontinence, which worsens when laughing, lifting weights, sneezing, coughing, as well as during various stressful situations;
- frequent urge to go to the toilet, often completely unexpected, which is difficult to control;
- difficulty urinating, accompanied by pain;
- a constant feeling of discomfort and insufficient bowel movements of the bladder, even with frequent visits to the toilet.
As it develops, the symptoms will worsen and become more pronounced. It is important to listen to your body, and at the slightest deviation, consult a doctor to establish an accurate diagnosis.
Causes
The pelvic floor is made up of the muscles, ligaments, and connective tissues that support the bladder and other pelvic organs. The connections between muscles and ligaments can weaken over time as a result of birth trauma or chronic strain of the pelvic floor muscles. When this happens, the bladder can drop below normal and literally fall out into the vagina. This condition is called a vesical hernia - cystocele (photo).
Possible reasons include the following:
- pregnancy and natural childbirth;
- overweight or obesity;
- frequent lifting of weights;
- problems with bowel movements, constipation;
- chronic cough or bronchitis.
Risk factors
It is quite possible to prevent the development of pathology if you have only recently learned about the existence of the term “cystocele”. What is this and how to prevent the problem? Pay special attention to risk factors that increase your likelihood of developing a bladder hernia. This:
- Childbirth. Most often, cystocele is found in women who have given birth to more than one child naturally.
- Aging of the body. The risk of urinary hernia increases in direct proportion to the patient's age. The postmenopausal period is especially dangerous, since after menopause the production of estrogen, which maintains the elasticity of the pelvic floor, decreases.
- Surgical removal of the uterus.
- Genetic features. An increased risk of pathology is observed in women born with weak connective tissues.
- Obesity. Cystocele also poses a danger for patients diagnosed with obesity and simply being overweight.
Diagnostics
The doctor must diagnose the problem before prescribing treatment based on the signs of cystocele alone - only a specialist can determine what it is and what kind of disease the discomfort is tormenting you. For this purpose, appropriate studies and analyzes are carried out, including:
- Pelvic examination. Such an examination can take place in two positions of the patient: standing and lying down. The doctor will look for obvious signs of a hernia, including a piece of tissue protruding into the vagina. Most likely, the specialist will ask you to push, as when visiting the toilet, to determine: how much such pushing affects the degree of the cystocele; What is it - a variation of the norm or an obvious pathology. To test the strength of your pelvic floor muscles, your doctor will ask you to contract them, as if you were trying to stop urinating.
- Urine and bladder function tests. If a severe cystocele is detected, you will be prescribed a study of bladder function, that is, the quality of emptying the organ during urination. A urine test will be needed to identify possible infectious diseases if it turns out that more urine remains in the body after a bowel movement than it should.
Prevention
Specific preventive measures include following simple recommendations:
- Correction of body weight. But without sudden changes. Therefore, no aggressive diets or other extreme methods of losing weight. All the more efficient ones.
- Optimal level of physical activity. Physical inactivity and excessive physical activity are almost equally harmful.
- Timely contacting doctors regarding third-party diseases. Including prostate adenomas.
- Careful monitoring of your well-being during pregnancy. It makes sense to regularly visit a leading obstetrician-gynecologist and report any problems to him. If necessary, consultation with an endocrinologist is indicated.
- An important point is muscle training. Perhaps doing some light sports, if your health allows. Or physical therapy, if there are contraindications to more intense activity.
If you follow the recommendations presented, there is every chance of not encountering a hernia, even if there is a tendency to develop one.
Treatment
If your diagnosis is cystocele, treatment will depend on the degree of bladder prolapse and the presence or absence of associated pathologies, such as prolapse of the uterus into the vagina (uterine prolapse).
Small hernias with mild or no symptoms usually do not require treatment. Experts recommend simply visiting a doctor from time to time to monitor the progression of the hernia and take independent treatment measures, namely, strengthening the pelvic floor muscles with the famous Kegel exercises. If independent measures do not help, treatment may include the following:
- Installation of a support device (pessary). A vaginal pessary is a plastic or rubber ring that is inserted into the vagina to hold the bladder in place. Installation is carried out by a specialist who will show you how to remove, clean and reinsert the ring. Many women use a pessary as a temporary alternative to surgery.
- Use of estrogen. Your doctor may recommend using estrogen-containing medications in the form of vaginal ointment or tablets specifically to treat cystocele. Reviews about specific medications can be read in advance on thematic forums. This therapy is especially useful after the patient reaches menopause.
Surgery
If you experience significant discomfort due to the symptoms of a bladder hernia, surgery may be necessary to correct the problem.
The operation is usually performed inside the vagina and involves returning the bladder to its normal position, removing excess tissue and tightening the muscles and ligaments of the pelvic floor. It may be necessary to use special tissue flaps (grafts) to strengthen and provide additional support to the vaginal tissue.
Peculiarities
If you have been diagnosed with uterine prolapse, in addition to pelvic tissue surgery, your doctor will recommend removing the uterus.
If you are planning a pregnancy but suffer from the telltale signs of a cystocele, surgery may be delayed until you decide you no longer want to have children. Symptomatic treatment at this time is carried out by installing a pessary.
The effect of competent surgical intervention can last for many years, however, unfortunately, no one is immune from relapse of the pathology. In this case, experts will advise you to undergo another operation.
fb.ru
The bladder may be adjacent to the hernial sacs of inguinal and femoral hernias or may protrude into the cavity of the hernial sac, constituting its contents. According to V.R. Braitsev, bladder hernias occur in 0.5-6.3%, according to R.S. Simovsky-Veitkov (1958), in 0.33-6.4% of cases. In 700 operations on hernias, inguinal, femoral and linea alba, M. G. Burlakov (1934) observed bladder hernias in 2.7% of cases, and they were recognized before surgery in only one case.
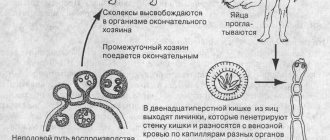
It is practically important to note that the bladder descends through the hernial orifice according to the type of sliding hernia. Significant displacement of the peri-vesical tissue, especially with a flabby abdominal wall, wide hernial orifices, leads during surgery when the hernial sac is overly stretched to the so-called artificial, or surgical, hernia of the bladder (Fig. 95).
There are three types of anatomical proximity of the bladder to the hernial sac: 1) intraperitoneal hernias, in which the bladder enters the hernial sac as a diverticulum covered with peritoneum (the wall of the hernial sac); 2) extraperitoneal hernias, when a part of the bladder not covered by peritoneum is adjacent to the hernial sac; 3) paraperitoneal hernias, in which the bladder, partially covered with peritoneum, is adjacent to the hernial sac. The most common hernias are paraperitoneal, then extraperitoneal, and much less often intraperitoneal.
Predisposing causes for the occurrence of bladder hernias are weakness of the anterior abdominal wall, especially pronounced in the lower abdomen, the presence of bladder diverticula, and a progressive increase in hernial protrusion. The role of fat plugs (lipoceles) near the wall of the bladder is also noted, which, increasing, draw it into the hernial orifice (L. N. Kenarskaya, A. F. Lukanov). Diseases of the prostate gland, narrowing of the urethra, and constipation can contribute to the displacement of the bladder towards the hernial orifice and hernial sac.
Rice. 95. Operative (artificial) hernia of the bladder (Kirschner).
Recognition of bladder hernias. The complaints of patients are reduced to difficulty urinating, frequent urge, urine retention, excretion in small portions, sometimes drop by drop. In some cases, the patient cannot urinate without pressing on the hernial protrusion, or the act of urination can only be performed by pressing on the scrotum and lifting it upward. When examining the patient, it is necessary to pay attention to the periodic increase in hernial protrusion, which is associated with an overfilling of the bladder. In unclear cases, you can recommend that the patient drink two glasses of water or tea and re-examine him before and after urination. When the bladder is emptied, the hernial protrusion decreases in size and the dull sound, previously detected by percussion, disappears. With moderate compression of the hernial protrusion, the patient feels the urge to urinate. It is necessary to check the condition of the prostate gland, especially in elderly patients.
In addition to a thorough history taking and repeated examinations of patients, additional studies (radiography, cystoscopy, cystography) are also necessary, which significantly improves the quality of preoperative recognition and reduces errors during surgery. L. I. Dunaevsky (1959) recommends cystoscopy for large, especially recurrent, hernias, which can show deformation of the bladder, retractions and funnel-shaped openings, hyperemia of the mucous membrane. The radiograph given by L.I. Dunaevsky is very indicative, which shows the asymmetry of the bladder, a protrusion of a diverticulum-like nature, extending from the shadow of the bladder (see Fig. 6).
By comparing two images taken after filling the bladder with a contrast agent and after urination, it is possible to determine the degree of emptying of the bladder and the presence of an unemptied diverticulum.
Privitera (1962) described an operation performed for a suspected inguinal hernia in the presence of a calculous cystocele in a 72-year-old man who, for 2 years, felt heaviness in the right groin area, pain during urination and after physical exertion. Upon palpation, an elastic formation (diverticulum) was determined, containing numerous dense bodies that moved noisily when palpated. The X-ray revealed many small, circular shadows; no stones were found in the bladder (Fig. 96).
Rice. 96. Bladder hernia. The diverticulum extending into the scrotum is filled with stones (Priviera).
In the differential diagnosis of sliding hernias, both inguinal and femoral, it is necessary to take into account the possibility of the bladder adhering to the hernial sac or the diverticulum protruding into the sac of the obturator hernia. P. A. Milonov (1962) gives a rare observation of an obturator hernia with a diverticulum of the bladder. The preoperative diagnosis was a right-sided sliding femoral hernia of the bladder. N.A. Kudryavtseva (1956) reports complete prolapse of the bladder into the scrotum in a 54-year-old patient with a bilateral inguinal-scrotal hernia. Direct adherence of the bladder or its protrusion into the lumen of the hernial sac, as well as protrusion of the bladder wall into the hernial orifice are accompanied by a real danger of damage to the bladder during surgery. During surgery for inguinal and femoral hernias, special attention is paid to the fatty tissue located in front of the hernial sac. The frequency of finding an excess amount of adipose tissue in the hernial orifice, according to V.
Braitsev is determined in 27%, and according to Lejars - in 63%. The atypical location of fatty tissue in the hernial orifice, at the neck of the hernial sac, should be considered a danger signal indicating the possible proximity of the bladder. The fatty deposit, which may be connected to the bladder, is usually located on the medial wall of the bladder. When isolating the hernial sac, the surgeon must palpate the tissue being divided. When the bladder is directly adjacent to the hernial sac, a greater thickness of the medial wall of the sac is noted. The patient should be asked about his sensations when stretching the hernial sac; The patient's statements about the urge to urinate should be immediately taken into account by the surgeon.
The surgeon cannot always determine whether the wall of the bladder is really in front of him; in doubtful cases, insertion of a catheter is indicated, which can be clearly palpated. Damage to the bladder during operations for hernias occurs in 0.4% of all hernia repairs (M. V. Dunye, 1948). V.I. Farberman (1930) analyzed 190 cases of bladder injury during surgery: the bladder was mistaken for a hernial sac 43 times, for a second hernial sac - 17 times, for a lipoma - 18 times, and for the colon - 3 times.
According to A.I. Baryshnikov (1961), out of 3296 operations for inguinal hernias, 12 bladder injuries were noted (0.37%).
Insufficient isolation of the hernial sac at the neck with subsequent suturing of the bladder wall is a consequence of non-compliance with the surgical technique. High discharge and high ligation of the neck of the hernial sac should not be accompanied by excessive tightening of it.
If a bladder injury is recognized during surgery, it is necessary to carefully isolate the area of the surgical field corresponding to the bladder wound and dry the surgical field. When applying forceps to the edges of an incision or rupture of the bladder wall, unnecessary trauma should be avoided. Excision of the edges of the defect is indicated for wounds with uneven edges. A double-row suture is applied without capturing the mucous membrane of the bladder. A change of linen and subsequent hand cleaning are required. The operation ends with plastic surgery followed by the administration of antibiotics.
If a bladder injury is detected immediately after the end of the operation, all sutures placed on the skin are removed and the surgical wound is inspected, since it is not always easy to detect the location where the integrity of the bladder has been damaged. On the recommendation of L. I. Dunaevsky, a solution of methylene blue can be injected into the bladder, which will make it possible to find the site of damage. The detected defect is treated in the usual way, cutting out the edges and suturing the defect with a double-row suture. The anatomical relationships of plastic closure are restored, a thin drainage tube is inserted, and antibiotics are administered. A soft catheter is inserted into the bladder for 1-2 days. In the postoperative period, attention is paid to all symptoms that may reveal an unrecognized violation of the integrity of the bladder: increased temperature, swelling in the area of the operation, swelling of the scrotum, spermatic cord, abdominal pain, dysuric phenomena, blood in the urine, pain in the depths of the pelvis with light sipping of the spermatic cord. cord (symptom of I.I. Sobolev, 1954). The prognosis depends on timely recognition of the first signs of tissue reaction to bladder damage.
In these cases, all skin sutures are removed and previously sewn tissues are separated layer by layer; Double-row sutures are applied to the detected area of bladder damage. A thin drainage is placed at the site of bladder damage, and a soft catheter is inserted into the bladder. The patient is carefully monitored with examination of the anterior abdominal wall, lumbar region, and digital examination of the rectum. At the same time, measures are being taken to combat intoxication. When a urinary fistula forms, if there are no indications for surgical intervention, L. I. Dunaevsky recommends inserting a permanent catheter into the bladder for 7-10 days, which often leads to closure of the fistula. If the fistula does not heal, radical surgery is indicated.
The mortality rate for unrecognized bladder injuries is high, amounting to 27% according to A. M. Gasparyan (1928) and 16.5% according to V. I. Farberman (1930).
Sliding of the ureter to the hernial sacs of inguinal and femoral hernias is very rarely observed. According to data collected by A.P. Krymov, 29 cases of ureteral hernias were observed, more often in women with femoral hernias. A.P. Krymov (1950) gives his observation of a 46-year-old patient with a large inguinal hernia. During the operation, a ureter was discovered behind the hernial sac, which the assistant mistook for a blood vessel. The ureter is often adjacent to the hernial sacs of direct inguinal hernias; simultaneously with the ureter, the bladder may also be adjacent to the hernial sac. If the wall of the ureter is damaged, side sutures are applied; if its integrity is completely damaged, it is sutured end to end. If ureteral injuries are not recognized during surgery, severe symptoms of urinary leakage develop with fever, chills, infiltration of the abdominal wall, and urine leakage from the wound. Timely opening of the wound is necessary to prevent urinary leakage, phlegmon, and sepsis. The question of further tactics is decided after a complete analysis of the entire clinical picture.
med-tutorial.ru
Etiology
Regardless of where the pinched hernia is localized, the mechanism of development of the pathology will be similar for all options. In such situations, a process of compression of the tissues of the internal organs that enter the cavity of the hernial sac occurs.
All hernias include the following components:
- gate - is a weakened hole in the ligaments or muscles;
- the bag is the cavity into which the internal organs directly fall;
- hernial contents are part of the organs penetrating the pathological opening that forms between the ligaments. In the vast majority of situations, the constituent parts of the hernial sac are intestinal loops, the greater omentum, as well as part of the stomach or bladder, which cannot independently return to their normal anatomical location.
Components of a hernia
The main reason affecting the strangulation of a hernia is an increase in intra-abdominal pressure, which, in turn, can be caused by:
- severe straining during bowel movements;
- coughing or sneezing;
- sudden lifting of weights;
- disturbance of the urination process;
- weakness of the abdominal muscles;
- traumatic injury to the abdomen;
- a sharp decrease in body weight;
- intestinal atony, esophagitis and other gastroenterological diseases;
- intense crying or loud screaming - these are the fundamental sources of strangulation of the abdominal hernia in the navel area in children;
- difficult course of labor;
- the patient has any stage of obesity;
- wearing excessively tight belts or belts.
After intra-abdominal pressure returns to normal, a decrease in the size of the hernial orifice is observed, against the background of which the process of pinching of internal organs that extend beyond the hernia occurs. It is worth noting that the probability of the formation of such a process does not depend on the diameter of the gate of the pathological protrusion and its size.