Etiology
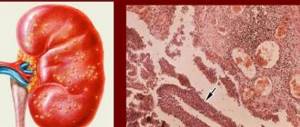
With chronic pyelonephritis, the kidneys decrease in size and their surface becomes lumpy. Leukocyte infiltration with damage to the renal tubules is observed in the interstitium. In the later stages of the disease, the kidneys shrink, and interstitial necrosis occurs during this period. Morphological changes develop in the direction from the pelvis to the cortex.
When the disease is chronic pyelonephritis, the symptoms are quite varied. The inflammatory process in the kidneys may resemble other diseases in its course.
- anemic,
- azotemic,
- leukocyturia,
- microhematuria,
- examination of urinary sediment (Addis-Kakovsky test);
- quantitative determination of cells according to Stenheimer-Malbin;
- biochemical blood test to determine the level of residual nitrogen, creatinine and urea;
- determination of electrolytes in blood and urine;
- kidney biopsy (process activity, inflammatory infiltration, degree of damage to renal tissue).
- kidney amyloidosis,
- diabetic glomerulosclerosis.
The latent form of the disease is characterized by minor clinical manifestations. The patient may experience general weakness, fatigue, headache, and sometimes the temperature may rise slightly. As a rule, there is no lower back pain, swelling or dysuria, although some experience a positive Pasternatsky symptom (pain when tapping the lumbar region).
A general urine test reveals slight proteinuria; leukocytes and bacteria may be excreted in the urine periodically. With a latent course, the concentrating ability of the kidneys is usually impaired, so a decrease in urine density and polyuria are characteristic. Mild anemia and a slight increase in blood pressure can sometimes be detected.
The azotemic form is considered chronic pyelonephritis, which began to appear only at the stage of chronic renal failure. The azotemic form may include the further development of latent pyelonephritis, which was not diagnosed in a timely manner.
Changes in urine analysis during an exacerbation are as follows:
Clinical diagnosis of chronic pyelonephritis has some difficulties due to the variety of clinical manifestations and, in many cases, the latent course of the disease. The diagnosis is usually made taking into account the history, characteristic clinical picture and results of laboratory and instrumental studies. The following diagnostic methods are usually used:
It should be said that even with an asymptomatic, latent course of pyelonephritis, a detailed questioning of complaints and anamnesis often reveals signs of the development of the disease. For example, patients may be bothered by “unreasonable” chills that periodically occur over many months or even years.
Another important symptom is nocturia (more urine is produced at night than during the day), especially if it is not associated with an increase in fluid intake and bothers you for a long time. Nocturia indicates a violation of the concentrating ability of the kidneys.
Chronic kidney pyelonephritis should be differentiated from the following diseases:
Kidney amyloidosis is characterized by the presence of chronic foci of infection in the body, scanty urinary sediment, the absence of bacteria in the urine and radiological signs characteristic of pyelonephritis.
Chronic glomerulonephritis is characterized by the predominance of red blood cells in the urinary sediment, the absence of “active” leukocytes and bacteria.
Unilateral pyelonephritis: features
This disease is characterized by dull pain in the lumbar region on one side (where the source of infection is localized). The pain is constant. There is usually no dysuria. During an exacerbation, fever is observed in every fifth patient. There are more leukocytes in urine sediment than other structures. When the diseased kidney shrinks, the urinary syndrome becomes less pronounced. The density of urine does not change.
When making a diagnosis, it is important to determine the concentration of active leukocytes. In case of a latent form of the disease, it is necessary to perform a test with prednisolone. 30 mg of the substance is dissolved in 10 ml of liquid and injected into a vein within five minutes, after which several portions of urine are taken for examination - an hour after the procedure, two and three hours later. Such a test is considered positive if after an hour there are 400 thousand or more leukocytes in the urine, the main percentage of which are active. If Sternheimer-Malbin structures are detected, the focus of inflammation can be confidently diagnosed, although this is not an indisputable indication of pyelonephritis.
Course of chronic pyelonephritis
Chr. pyelonephritis, as a rule, lasts a long time (15 or more years) and ultimately leads to shrinkage of the kidneys. This disease is characterized by uneven wrinkling and the formation of rough scars on the surface of the kidneys. In cases where the process is unilateral, compensatory hypertrophy of the healthy kidney and its hyperfunction are observed.
In chronic pyelonephritis, uremia develops slowly; as a result of treatment, it can be easily reversed.
Latent chronic pyelonephritis is characterized by long-term preservation of patients’ ability to work. This cannot be said about the hypertensive form, which occurs with high arterial hypertension; in its malignant course, patients lose their ability to work. A serious prognosis also occurs with the azotemic form of the disease. Recently, the prognosis has improved significantly due to the introduction of modern methods of treating pyelonephritis.
In all forms and stages of the disease, adherence to a certain diet plays an important role in therapy. It is necessary to exclude spicy foods and spices, coffee, alcoholic beverages, meat and fish broths from the diet. At the same time, food should be fortified and sufficiently high in calories. You can eat almost all fruits and vegetables, especially those containing a lot of potassium, as well as eggs, boiled lean meat and fish, milk and dairy products.
Diet for pyelonephritis
In the anemic form of the disease, food includes foods containing a lot of iron and cobalt (strawberries, wild strawberries, pomegranates, apples). Also, for almost all forms of pyelonephritis, it is recommended to eat grapes, watermelon, and melons, which have a diuretic effect.
It should be noted that drug therapy can only be effective if the unimpeded outflow of urine is ensured. Antibacterial agents (antibiotics, sulfonamides, uroseptics) are usually used as drugs. Antimicrobial treatment is prescribed taking into account the sensitivity of the microorganisms that caused the inflammation. For chronic pyelonephritis, treatment is long-term; a combination of antibacterial drugs with different mechanisms of action is usually used. Antibacterial treatment must be continued until leukocyturia is completely eliminated and urine is sterilized.
When the exacerbation subsides, anti-relapse treatment is carried out, which consists of long-term, months-long use of minimal doses of antimicrobial agents with periodic changes of drugs. Along with drug treatment, herbal medicine is important. A good effect is observed when using decoctions and infusions of various plants that have diuretic, anti-inflammatory and antibacterial effects. Usually juniper berries, horsetail herb, bearberry leaf, and kidney tea are used.
AMUR STATE MEDICAL ACADEMY
Higher education
Home address: ******
Work performed and position: instructor in the company
COMPLAINTS.
At the time of examination: the patient complains of a mild aching pain in the lumbar region. Frequent urination in small quantities.
A
NAMNESIS MORBI:
In 1989, minor aching pains, frequent painful urination, and facial pastiness appeared. The patient was offered sanatorium-resort treatment in Anapa, which gave positive results.
09/25/2000 severe paroxysmal pain appeared in the lumbar region, which radiated down the abdomen. Urination is frequent and painful. I went to the clinic and was sent for an ultrasound of the kidneys, where salts were found in both kidneys. The patient was sent to the 3rd city hospital for examination and treatment.
Higher education. Works as an instructor. There are no occupational hazards. The working day and working week are standardized.
Menstruation began at the age of 12, regular, painless, five days, after 28.
Marital status: not married, no children.
Family history and heredity data: Heredity is not burdened.
Financially secure. Meals are regular, varied and nutritious. Complies with hygiene standards.
Bad habits: Doesn't smoke. Drinks alcohol on holidays.
ALLERGOLOGICAL HISTORY:
There is an allergic reaction to penicillin, in the form of swelling at the injection site. He denies reactions to other allergens.
EPIDANAMNESIS.
I gave myself injections of antispasmodics. Blood type III Rh+
S
TATUS PRAESENS OBJECTIVUS .
Body temperature 36.7 C.
The skin is not changed, normal color, clean, moist. The nails are oval in shape, brittle, and there is no deformation of the nail plates. Visible mucous membranes are pale pink. Subcutaneous fatty tissue is moderately developed. Swelling on the legs, pasty face.
Peripheral lymph nodes: subpharyngeal, jugular, inguinal, cervical, occipital are not palpable
Muscular system: Well developed. There is no pain on palpation.
Osteoarticular apparatus: No visible changes.
Breathing type: chest. Breathing is rhythmic with a frequency of 16 respiratory movements per minute. The chest is painless and elastic. The collarbones are located symmetrically. The course of the ribs is oblique. The epigastric angle is straight.
The spine is not deformed. shoulder blades are located at the same level
Topographic percussion of the lungs.
Source: https://studentmedic.ru/history.php?view=231
What is the danger of the disease
After each attack of acute pyelonephritis, a scar remains on the kidneys. The amount of functioning parenchyma decreases, the work of the organ becomes less and less active. The load on operating nodes increases. The result is serious kidney disease.
The presence of purulent bacteria in the blood during a descending route of infection contributes to the formation of apostenomatous pyelonephritis. When the cortical surface of the kidney becomes covered with ulcers. When several small abscesses coalesce into one, a kidney carbuncle is formed, which can only be eliminated surgically.
Chronic pathology characterized by nonspecific inflammation of kidney tissue
As a result of chronic pyelonephritis, patients experience swelling of all tissues and intoxication of the body, since the kidneys are not able to purify the blood plasma and harmful substances remain in the tissues. Over time, a rash appears on the skin - sepsis, as a result of poisoning the body with toxins.
Reverse infection of the bladder and urinary tract leads to inflammatory processes in the genitourinary system. This, in addition to pain when urinating, is noticeable by the color of the urine and its unpleasant odor. Blood and pus appear in the urine.
Chronic pyelonephritis (case history)
Russian nationality
Profession: teacher
Clinical diagnosis: Chronic pyelonephritis, primary, right-sided, in the phase of active inflammation.
At the time of admission: the patient complains of nagging pain in the lumbar region. Frequent, painful urination in small quantities.
A
NAMNESIS MORBI:
In 1998, severe paroxysmal pain appeared in the lumbar region, which radiated down the abdomen. Urination was frequent and painful. She called an ambulance, which took her to City Hospital No. 3. An examination was carried out, the results of which were normal. The patient was sent home and prescribed antispasmodics.
A
NAMNESIS VITAE:
GYNECOLOGICAL HISTORY:
Financially secure. Meals are regular, varied and nutritious. Complies with hygiene standards.
There is an allergic reaction to penicillin, in the form of swelling at the injection site. He denies reactions to other allergens.
HAEMOTRANSFUSION HISTORY.
There was no blood transfusion.
Viral hepatitis, tuberculosis, veins. Denies illness, typhoid and typhus.
Over the past 6 months I have not traveled outside the city. There was no contact with infectious patients. Stools are formed, regular, once a day.
The chest is of normal shape. The joints are of normal configuration, painless on palpation, active and passive mobility is preserved.
RESPIRATORY SYSTEM.
Source: https://mirznanii.com/a/147737/khronicheskiy-pielonefrit-istoriya-%3Cb%3Ebolezni%3C/b%3E
Pediatric gastroduodenitis
This disease in children involves nonspecific inflammation of the mucous membranes of the stomach and duodenum. Chronic and acute gastroduodenitis occurs. Pediatric medical history and its diagnosis are not always accurate, since this disease can be confused with gastritis. They have similar symptoms. The acute manifestation looks like this: pain and heaviness in the upper abdomen, dry mouth and thirst, sour belching, headaches and nausea. Chronic gastroduodenitis combines many more symptoms:
Source: https://fb.ru/article/158079/istoriya-bolezni-po-pediatrii-detskie-bolezni
Abstract: Chronic pyelonephritis (case history)
Type: abstract Added 10:06:07 July 23, 2005 Similar works
Blagoveshchensk 2000
Date of admission: 09/05/2000
Date of discharge: 09.26.2000
She considers herself sick since 1980, when the patient first developed acute pyelonephritis, the cause of which she does not know. Treatment was carried out and in the next 2 years after observation in the clinic, a diagnosis was made: chronic pyelonephritis.
She was born in Skovorodino, the first child in a working-class family. She did not lag behind her peers in development. I went to school at age 7 and studied well. She started working at the age of 22.
Past illnesses: In 1984, she suffered from Botkin's disease. In 1989, she suffered from tonsillitis. There are no complications after the illnesses suffered.
Menstruation began at the age of 12, regular, painless, five days, after 28.
Marital status: not married, no children.
Family history and heredity data: Heredity is not burdened.
Bad habits: Doesn't smoke. Drinks alcohol on holidays.
ALLERGOLOGICAL HISTORY:
S
TATUS PRAESENS OBJECTIVUS.
The patient's condition is satisfactory. Consciousness is clear. Position active. Behavior is appropriate.
Anthropometric data: height 175 cm. weight 64 kg. Normosthenic type of constitution.
Breasts: regular shape, nipples are symmetrical, lumps are not palpable.
The chest is of normal shape, symmetrical. Both halves of it evenly and actively participate in the act of breathing.
Source: https://www.bestreferat.ru/referat-66809.html
Chronic pyelonephritis means chronic nonspecific inflammation of the interstitial tissue of the kidney, leading to damage to the mucous membrane of the pelvis, renal vessels and parenchyma.
Chronic pyelonephritis is usually bilateral, but the degree of kidney damage varies. More often the disease affects women.
Pyelonephritis is caused by bacteria:
L-forms of bacteria play a certain role in the occurrence of chronic pyelonephritis, which can persist in the body for a long time and enter the kidneys with the blood.
Pediatrics and childhood diseases
Pediatrics is a separate field of medicine that studies the developmental characteristics of children, their diseases, and issues of caring for a newborn, healthy and sick child. Initially, the subject of pediatrics was only early childhood diseases and the fight to eliminate them. Today, this science combines a variety of aspects that are closely related to the normal development and diseases of children from birth to puberty. Such areas include hygiene, physiology, dietetics, childhood diseases, their prevention and treatment.
The child’s body is constantly growing and developing, has a number of anatomical and physiological characteristics, emotional and physical immaturity, thereby determining the specific course of diseases. For example, certain childhood diseases go away much easier until they grow up, such as rubella and chickenpox, but diseases of the upper respiratory tract are difficult for children.
Clinic
Forms of chronic pyelonephritis:
The anemic form of pyelonephritis is characterized by the predominance of anemic symptoms in the clinic: shortness of breath, weakness, fatigue, pallor, heart pain. Changes in urine are scanty and inconsistent.
In the hypertensive form, arterial hypertension predominates in the clinic. Headache, dizziness, sleep disturbance, stabbing pain in the projection of the heart, frequent hypertensive crises, and shortness of breath occur. Changes in urine are subtle and not constant. Hypertension with pyelonephritis is often malignant.
The recurrent form of pyelonephritis is characterized by alternating periods of exacerbation and remission. The patient may experience discomfort in the lower back, chills, and fever. Dysuric phenomena appear (frequent urination, sometimes painful).
Exacerbation of chronic pyelonephritis clinically resembles the picture of acute inflammation. As the process progresses, the leading syndrome becomes hypertensive, which is manifested by headache, dizziness, visual impairment, and pain in the heart. Sometimes, as a result of long-term pyelonephritis, anemic syndrome develops. The outcome of the disease is chronic renal failure.
Blood tests show anemia, increased leukocyte count, increased ESR.
Nuances of clinical practice: chronicle
Particular difficulties are associated with clarifying the condition: chronic pyelonephritis is in many ways similar to glomerulonephritis, which occurs in a chronic form. To clarify the condition, it is important to carefully analyze the urinary syndrome, evaluate the content of various components in urine, and also identify all the features of the functioning of the organ through urography. Nephrotic syndrome indicates glomerulonephritis.
If blood pressure is elevated, the possibility of hypertension, renovascular hypertension, and renal disease in question should be considered. In order for the differential diagnosis to give the most correct result, it is necessary to analyze the urinary syndrome, an x-ray, and the results of a radionuclide study. Pyelonephritis will be indicated by asymmetry in the excretion of the coloring component during chromocystoscopy.
The pathological condition can be distinguished from renovascular hypertension by means of urography, renography, and aortoarteriography.
Diagnosis and differential diagnosis
- general urine analysis (leukocyturia, sometimes erythrocyturia, proteinuria, decreased urine density);
- general blood test (anemia, neutrophilic leukocytosis, increased ESR);
- bacteriological examination of urine;
- X-ray examination of the kidneys (changes in the size of the kidneys, deformation of the calyces and pelvis, impaired tone of the urinary tract);
- radioisotope renography (the functional state of the left and right kidneys is determined separately);
Kidney biopsy
To diagnose the disease, retrograde and intravenous pyelography, scenography and renography are used. To identify unilateral chronic pyelonephritis, catheterization of the ureters is performed and the presence of protein and blood cells in the urinary sediment is determined.
Advice: if you notice these symptoms, you should not ignore them. It is necessary to consult a doctor so as not to miss the development of chronic pyelonephritis and start treatment in a timely manner.
Hypertension is more common in older people, occurring with hypertensive crises and pronounced sclerotic changes in the cerebral, coronary vessels and aorta. Also, patients do not have changes in urine and blood characteristic of pyelonephritis.
Diabetic glomerulosclerosis is characterized by a history of diabetes mellitus and the presence of other manifestations of angiopathy (trophic leg ulcers, retinopathy, etc.). In the most difficult cases, a histological examination of kidney biopsies is performed.
When both kidneys are affected in the final stage of pyelonephritis, chronic renal failure appears. First, the concentration function of the kidneys decreases and polyuria occurs, and then the filtration capacity is impaired. This leads to retention of nitrogenous waste in the body and uremia.
Forecast
Features of symptoms
Often, doctors record in the medical history of gestational pyelonephritis (as, indeed, any other) that a high concentration of bacteria is detected in the patient’s urine. If the number of microorganisms per 1 ml of liquid is 100 thousand or more, samples of the liquid should be taken to determine resistance to antimicrobial agents and chemotherapy.
Often, increased pressure in the arteries indirectly indicates pyelonephritis. To a greater extent, this is characteristic of a bilateral process, a chronic form.
To identify the characteristics of the condition, it is necessary to do chromocystoscopy, urography, and evaluate creatinine clearance for each of the kidneys. An X-ray is taken using hippuran and the kidneys are scanned. With chronic conditions, the organ’s concentration ability is quickly impaired, but nitrogen release can last for a long time.
Since with pyelonephritis the tubules of the organ cannot work normally, acidosis is gradually observed. In some patients, pyelonephritis is indicated by parathyroidism and renal osteodystrophy, which are explained by the leaching of phosphate compounds and calcium from organic tissues.
Treatment
Treatment of chronic pyelonephritis includes a gentle regimen, diet and drug therapy. Patients should avoid hypothermia and colds. Any infectious diseases that occur against the background of pyelonephritis require adequate therapy and monitoring of urine tests.
Diet
In addition, it is necessary to drink a sufficient amount of fluid (about 1.5 - 2 liters per day) to prevent excessive concentration of urine and to flush the urinary tract. It is very useful to drink cranberry juice, which contains natural antibacterial substances. During an exacerbation of the disease, fluid intake, on the contrary, should be reduced, since the outflow of urine is disrupted. Also, during an exacerbation and in the hypertensive form of pyelonephritis, it is necessary to limit table salt to 2-4 g per day.
Drug treatment
Important: herbal medicine cannot replace drug treatment. Decoctions and infusions can improve the effect of antibacterial or diuretic agents. Their use must be agreed with your doctor.
Vitamin therapy is of no small importance. During treatment with antibiotics, the prescription of antihistamines and anti-inflammatory drugs is justified. In the hypertensive form of pyelonephritis, antihypertensive and antispasmodic drugs are widely used. Anemia resulting from the disease is difficult to treat. To eliminate it, iron supplements and vitamins are prescribed.
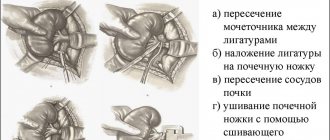
In some cases, nephrectomy is resorted to. The operation is indicated for advanced chronic unilateral pyelonephritis, which is not amenable to therapy, as well as for shrinkage of one kidney, complicated by severe arterial hypertension. To treat developing uremia, an appropriate diet with limited protein and salt is prescribed. Peritoneal dialysis or hemodialysis is performed. If kidney function is significantly reduced, then the issue of transferring the patient to chronic hemodialysis is decided.
How to help?
When a patient’s chronic pyelonephritis in the acute stage is detected in the medical history, the doctor not only records all the patient’s complaints and test results, but also specifies which treatment program is chosen for a particular case. In particular, this is specialized nutrition. The acute stage of the disease calls for eating according to the seventh table (subtype A). You need to drink at least two liters of fluid per day, more if possible. The doctor monitors the patient’s condition and, as it improves, expands the diet, increasing the protein saturation and fat content of the diet. If metabolic acidosis is observed, sodium bicarbonate should be used. Take up to 5 g orally or inject into a vein up to 60 ml of solution (not more saturated than 5%).
All selected activities, medications, and their dosages must be recorded in the medical history. Therapy for pyelonephritis requires taking measures to stimulate blood flow in the kidneys and relieve pain. Thermal procedures are shown. The doctor will explain how to make compresses and heating pads. A popular procedure is diathermy. If the pain is still severe and the heat does not relieve it, it is necessary to take medications. Antispasmodics - Papaverine and Platifillin - will help. They are intended for short-term use, they help alleviate the condition, but you cannot take such drugs constantly - they are characterized by side effects.