Acute glomerulonephritis is an immune-inflammatory pathology that involves the structural units of the kidneys, nephrons, in the process of inflammation and affects the glomerular apparatus. As it progresses, the tubular structures and interstitial tissue of the kidneys are affected.
Etiopathogenesis consists of certain immune reactions explained by infection or progression of hypersensitivity.
The disease is accompanied by extrarenal (edematous and hypertensive) and renal (urinary) syndromes. It most often makes itself felt in children from 2 to 12 years of age, in adults - up to forty years. The incidence of pathology is higher among male patients. The peak incidence is observed in the cold season.
Detection of the disease requires laboratory tests of urine and blood, ultrasound scanning of the kidneys, and in severe situations, a biopsy of the kidney parenchyma. Correction includes proper nutrition, bed rest, drug treatment (steroids, diuretics, antihypertensives and other drugs as indicated).
Classification
According to etiopathogenesis, glomerulonephritis is distinguished:
- Primary. It is provoked by an infectious, allergic or toxic effect on the kidney parenchyma.
- Secondary. A consequence of systemic pathologies, the list of which includes systemic lupus erythematosus, hemorrhagic vasculitis.
- Idiopathic glomerulonephritis. Progresses for unknown reasons.
The nature of the disease determines its form.
Acute glomerulonephritis can be infectious-immune or non-infectious-immune. The volume of glomerular damage determines the division into focal and diffuse forms. Diffuse pathology according to ICD-10 is classified as acute nephritic syndrome.
Morphological variations in the development of acute glomerulonephritis:
- Proliferative endocapillary.
- Proliferative extracapillary.
- Mesangioproliferative.
- Membranous-proliferative.
- Sclerosing.
The clinical forms of the disease are:
- Classic extended (hypertension, swelling and urinary syndrome).
- Bisidromic (urinary syndrome is combined with either swelling or hypertension).
- Monosyndromic (urinary syndrome).
Types of glomerulonephritis
There are several classifications of the disease. In accordance with the nosological principle, primary and secondary glomerulonephritis are distinguished. In the first option, the cause of the pathological condition is unknown, and in the second, the disease develops due to systemic diseases, liver diseases, and the use of certain medications.
Taking into account the course of the disease, glomerulonephritis is divided into:
- For an acute form. With proper and timely treatment of glomerulonephritis, recovery occurs.
- For subacute form. It is characterized by a rapid, often malignant course. With such glomerulonephritis, acute renal failure may develop.
- For the chronic form. This type of disease is characterized by a progressive course leading to chronic renal failure.
Acute glomerulonephritis, in turn, is divided into post-streptococcal and post-infectious (classification by etiology), as well as epidemic and sporadic (classification by epidemiology). Chronic glomerulonephritis also has several forms:
- latent – changes are detected only in the urine of a sick person;
- hematuric – the presence of edema and arterial hypertension;
- hypertensive – changes in urine, arterial hypertension are observed;
- nephrotic – nephrotic syndrome is detected, there is no arterial hypertension;
- mixed - in this form, nephrotic syndrome can be combined with arterial hypertension, hematuria, and azotemia.
Causes
More often, acute glomerulonephritis occurs after an illness caused by a streptococcus-mediated infection. Such pathologies include:
- pharyngitis;
- sore throat or acute tonsillitis;
- scarlet fever;
- erysipelas.
In such situations, the etiological factor in the progression of inflammation is group A beta-hemolytic streptococcus.
The streptococcal genesis of the disease is confirmed by an increasing titer of antibodies to streptolysin-O and streptococcal hyaluronidase, an increase in circulating immune complexes, which include antibodies to streptococcus.
In other cases, inflammation of the glomerular apparatus of the kidneys can be triggered by an infectious disease of a viral nature from the following list:
- flu;
- chickenpox;
- mumps;
- rubella;
- mononucleosis;
- herpes;
- hepatitis.
In rare cases, glomerulonephritis is a consequence of the following pathologies:
- diphtheria;
- pneumococcal pneumonia;
- staphylococcal pneumonia;
- brucellosis;
- malaria;
- typhoid and typhus;
- infectious endocarditis.
Infectious-immune acute glomerulonephritis is listed above, but in addition to them, there are non-infectious-immune forms of the disease. They can be triggered by:
- vaccination and administration of serums;
- hypersensitivity to plant pollen;
- use of drugs that have nephrotoxic effects;
- snake and insect bites;
- alcohol intoxication.
The list of factors predisposing to the progression of the inflammatory process includes hypothermia and features of the anatomical structure of the glomerular apparatus in children.
At the present stage, urology believes that acute glomerulonephritis is an immune complex condition. That is, after the action of infectious or allergic factors, the body’s reactivity changes, as a result of which antibodies to antigenic structures are formed.
After the formation of antigen-antibody immune complexes, they are fixed on the basement membranes of the capillary network of the glomeruli. The structure of the vascular wall changes, vascular permeability increases, which creates conditions for the formation of blood clots.
As a result of malnutrition of the renal parenchyma in ischemic tissue, the renin-angiotensin-aldosterone system is activated. This leads to spasm of peripheral vessels and an increase in blood pressure. Because of this, disturbances in filtration and reabsorption processes are observed, water and sodium are retained, and pathological elements appear in urine.
Preventive measures
Prevention of acute glomerulonephritis includes prevention and early treatment of acute infectious diseases, elimination of focal infection. Experts recommend that people harden the body, avoid prolonged and sudden hypothermia, and not work in jobs that involve exposure to cold conditions or physical stress. After treatment, you should not plan a pregnancy for the next 3 years. It is advisable to periodically undergo medical examinations, have your urine tested, and monitor your blood pressure.
To prevent chronic glomerulonephritis, similar preventive measures have been established. Need to
- promptly eliminate foci of infection in the body;
- treat intestinal infections;
- avoid hypothermia and exposure to humid air;
- be under medical supervision;
- do not go on long business trips, do not get a job with night shifts, do not be exposed to harmful substances;
- regularly go to sanatorium-resort treatment;
- Healthy food;
- to refuse from bad habits.
In general, you should lead a healthy lifestyle.
In conclusion, it is worth noting that you need to be more attentive to your body, value your health and life. Only with this approach, as well as with timely consultation with a doctor and compliance with his clinical recommendations, can glomerulonephritis be avoided, like any other disease.
Symptoms
The classic picture of pathology is represented by three syndromes (symptom complexes):
- renal (kidney);
- extrarenal - hypertensive and edematous.
The development of the disease begins after one or two weeks after the action of one or another etiological factor - an infectious disease, hypersensitivity reaction and other provocateurs.
- The earliest sign of the acute form is the appearance of edema. In half of the situations, swelling is significant. The localization of swelling is in the face, it is more pronounced in the morning, and in the daytime the ankles and legs swell. Edema syndrome can develop to conditions such as hydroperitoneum, hydropericardium, hydrothorax, and widespread edema (anasarca). Visually noticeable swelling is not a mandatory symptom, but fluid retention is confirmed by an increase in body weight.
- Hypertension manifests itself moderately: in approximately 2⁄3 patients the pressure level is no more than 160/100 mmHg. Art. But you need to understand that prolonged persistent hypertension in the future gives a negative prognosis. In the case of acute damage to the glomeruli, hypertension is combined with a decrease (heart rate less than 60 beats per minute). It lasts for one or two weeks.
- When hypovolemia develops acutely, progression of left ventricular failure cannot be ruled out. Clinically, this is expressed in the form of pulmonary edema and cardiac asthma.
- Inflammation of the glomerular apparatus can be accompanied by pain of varying intensity. More often symmetrical pain occurs in the lumbar region. They arise as a result of overstretching of the kidney capsules and disturbances in urodynamic processes.
- The urinary syndrome of this pathology involves the early manifestation of oliguria, and in other situations, anuria. At the same time, there is pronounced thirst.
- The relative density of urine increases, and cylinders of hyaline and granular types begin to appear in it. Erythrocyturia (micro- or macrohematuria) and proteinuria are noted. In the case of gross hematuria, urine becomes the color of “meat slop.” Hematuria and proteinuria are especially intense on the first day of disease progression.
Quite often, cerebral disorders progress, which arise due to swelling of the brain. The list of manifestations includes:
- headache;
- vomiting and nausea;
- deterioration of visual function;
- the appearance of a “veil” before the eyes;
- deterioration of auditory perception;
- disturbances of psychomotor excitability.
The most severe manifestation of cerebral syndrome is eclampsia (angiospastic encephalopathy). It includes tonic-clonic convulsions, disturbances of consciousness, cyanosis of the facial and cervical area, swelling of the neck veins, decreased pulse rate and other symptoms.
In rare situations, the pathology progresses in a monosidromic form, which includes isolated urinary syndrome. There is no swelling and acceptable blood pressure levels are maintained.
Symptoms and course of acute glomerulonephritis
The acute form of the disease in many people begins with a simple sore throat. First, your throat hurts and your temperature rises. Unpleasant symptoms last for several days. Then recovery comes. It seems that the disease has subsided, but then the sore throat is replaced by acute glomerulonephritis (after about 1–2 weeks). It makes itself felt with high fever and deterioration in health. The amount of urine produced decreases, and it also takes on a reddish tint. Swelling appears quickly. Blood pressure also rises and headaches begin to occur.
Edema is one of the important symptoms of glomerulonephritis. A red tint to the urine may not be observed, but swelling occurs in 70–90% of cases. Very often they appear on the face. They indicate that the kidneys cannot cope with the function of excreting urine. The swelling is very noticeable in the morning. By evening they usually decrease. It is important to note that swelling is not always visible. Sometimes fluid accumulates in the pleural, abdominal, or pericardial cavities. Due to such hidden edema, body weight increases significantly.
Experts recommend that people have their urine tested after a sore throat or other illnesses. In adults, the picture of glomerulonephritis is not too bright. Sometimes the disease is indicated not by symptoms, but by changes in tests. Mostly in children and adolescents, the acute form of glomerulonephritis occurs with a rapid onset.
Diagnostics
Diagnosis of acute inflammation of the glomerular apparatus should take into account the clinical picture, complaints, changes in laboratory tests of urine and blood, the results of an ultrasound scan of the kidneys and the study of a biopsy specimen.
In the general analysis of urine, cylindruria, hematuria and proteinuria are noted. A Zimnitsky test is also performed: the volume of daily urine decreases and its relative density increases. The results of the Rehberg test indicate a deterioration in filtration function.
Changes in blood biochemistry parameters include hypoproteinemia, dysproteinemia (the ratio of albumin to globulins decreases). C-reactive protein appears. Increased levels of lipids, cholesterol, and blood nitrogen. Hypercoagulability syndrome is also characteristic.
It is advisable to conduct immunological studies:
- the titer of antistreptolysin-O increases;
- antistreptokinase titer increases;
- antihyaluronidase titer increases;
- the titer of antideoxyribonuclease B increases;
- the concentration of immunoglobulins G, M increases, less often - A;
- hypocomplementemia of C3 and C4 is noted.
Ultrasound scanning can reveal unchanged kidney sizes and decreased echogenicity.
In some situations, it is advisable to perform a biopsy. Indications for it are:
- Differentiation of acute and chronic forms of glomerulonephritis.
- Rapid progression of glomerular inflammation.
Nephrobiopsy has the following features:
- signs of cell proliferative processes;
- infiltration of the glomerular apparatus by neutrophils and monocytes;
- dense immune complexes.
In case of hypertension, it is advisable to examine the fundus and conduct an electrocardiographic study.
Diagnosis
CGN is diagnosed based on a set of clinical and laboratory studies, the scope of which is outlined in a similar section devoted to CGN. For diagnosis of the stages of chronic renal failure, see below. CGN should be suspected in any patient with “acute glomerulonephritis” if the disease occurs with nephrotic syndrome, hematuria and a persistent increase in blood pressure. In modern conditions, the diagnosis of CGN must be confirmed by morphological examination of the kidney.
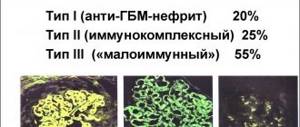
The point of a biopsy is to clarify the diagnosis, that is, to identify the morphological type of kidney damage, and hence to decide on the advisability of prescribing glucocorticosteroids and cytostatics (immunosuppressants). Light, electron and immunofluorescence microscopy of biopsy material also allow us to talk about the prognosis of nephropathy. Detection of hypoplasia and dysembryogenesis of renal tissue makes therapy with immunosuppressants practically pointless, since their damaging effect is great, and, of course, there will be no positive effect of treatment. In case of complications of GN with focal and diffuse sclerosis, lobular and extracapillary changes (clinically, such patients always have hypertension
), isolated administration of glucocorticoids is ineffective. Glucocorticoids are also contraindicated for amyloidosis, infections, and tumors.
Treatment
Therapy should be carried out in an inpatient setting in the urology department. Bed rest must be observed.
Medication
- Basic treatment involves prescribing steroids (dexamethasone, prednisolone). The course of therapy with them lasts up to one and a half months.
- In case of significant swelling and hypertension, antihypertensive drugs and diuretics are used in parallel.
- If there are signs of an infectious process, it is advisable to prescribe antibiotics.
- If glomerulonephritis has become the cause of progression of kidney failure, then anticoagulants and hemodialysis procedures can be used.
Diet
A salt-free diet is prescribed, in which the amount of animal proteins and liquids is limited. The diet includes fasting and “sugar” days. Fluid intake and diuresis should be monitored.
Stationary correction lasts up to one and a half months. After recovery, the patient should be observed by a nephrologist.
Prognosis for glomerulonephritis
The outcome of the disease depends on several factors - the morphological variant of glomerulonephritis, the frequency of exacerbations, and the development of chronic renal failure. In the acute form, the prognosis is favorable. However, it is worth remembering that only with treatment does recovery occur. Incorrect, untimely or completely absent therapy increases the likelihood of progression of the disease and the transition of the acute version to chronic.
With chronic glomerulonephritis, everything is much more complicated. The prognosis depends on the types of this disease. In the latent form of chronic glomerulonephritis, the prognosis is favorable, in the hypertensive form it is serious, and in the mixed form it is unfavorable.
Characteristic features of diffuse glomerulonephritis
Small renal vessels - capillaries, closely intertwined with each other, form glomeruli. They have a high filtering ability, as a result of which harmful substances are retained and released into the resulting urine. Under the influence of autoantibodies (hostile to the cells of one’s own body), the structure of the glomeruli is damaged with a gradual loss of their functionality.
According to the clinical course, two forms of pathology are distinguished, therefore, the modern ICD-10 classification is based on two encodings:
- Acute - N It is based on an infectious-allergic process - an attack of the glomeruli of an organ by immune complexes formed as a result of bacterial or viral damage.
- Chronic – N03. It is characterized by progressive diffuse damage to the structures of the glomerular apparatus, as a result of which their sclerosis and renal failure develop.
It is important to know! Diffuse glomerulonephritis is a type of disease that develops independently or against the background of certain systemic disorders - lupus erythematosus, hemorrhagic vasculitis, infective endocarditis.
Depending on the morphological changes, several types of acute forms of pathology are distinguished, and the existing code can have an additional order of numbers from 2 to 6:
- membranous glomerulopathy (diffuse thickening of capillary basement membranes);
- proliferative form (increase in cellular capillary structures);
- focal segmental glomerulosclerosis (sclerosation of individual vascular loops);
- mesangio-capillary (proliferative process in mesangial cells).
At the same time, a collective form of the disease is isolated, which combines symptoms of several types. Delayed therapy or its absence leads to chronicity of the process, which is much more difficult to treat.
Causes and pathogenesis
As mentioned above, the disease has two forms of clinical course, and each of them occurs for different reasons.
Chronic diffuse glomerulonephritis is a complication of an acute disease or is of autoimmune origin. Due to a violation of the permeability of the filtering membrane of the renal glomeruli, antigen-antibody complexes settle on the basal cells of the epithelium, provoking the development of a sluggish inflammatory process. It can last for several years, against the background of which kidney failure gradually increases and the organ itself dries out.
Acute diffuse type of glomerulonephritis develops against the background of a previous streptococcal infection. It could be tonsillitis, tonsillitis, pneumonia, scarlet fever, streptoderma. The disease is also considered a consequence of ARVI, chicken pox or measles. The development of pathology is affected by prolonged exposure to the cold in conditions of high humidity, since immune reactions are weakened.
The pathophysiology of the disease is immunoallergic. The incubation period is 2-3 weeks - this is exactly how long it takes after an infection and before the first signs of pathology appear. During this period, complexes are formed that enter the kidney structures. The glomeruli increase in size, and microscopic examination reveals signs of inflammation of the capillaries and the presence of protein exudate.
The acute inflammatory process develops rapidly, since immune complex compounds deposit in large quantities on the basal cells of the epithelium. The disease progresses and, in case of delayed treatment, enters the chronic stage. In pathological anatomy, the kidneys affected by the diffuse form of glomerulonephritis have reduced shapes and a compacted structure. Interstitial tissue is replaced by connective tissue, as a result of which the functionality of the organ decreases.
Symptoms of the disease depending on the form
For the acute diffuse form of the disease, three symptom complexes are considered characteristic: hypertensive, urinary and edematous. The main signs of the initial stage of the pathological process are:
- increased body temperature, sometimes to hectic levels;
- chills, fever;
- headache;
- decreased appetite;
- nausea, vomiting;
- pain in the lumbar region;
- general weakness.
In the first 3-5 days, oliguria develops, the patient experiences swelling, and the skin becomes pale. Later, the amount of urine excreted increases sharply, but its density decreases, and minor blood impurities appear - microhematuria. It occurs in 82-85% of cases. Much less often, in 12-15% of patients, macrohematuria can be noticed, which is characterized by the release of urine the color of “meat slop”, less often brown or black.
Acute glomerulonephritis has two types of course:
- cyclical, when the process develops rapidly and the symptoms are pronounced;
- latent – develops gradually, clinical manifestations are erased.
Symptoms of chronic diffuse lesions may vary depending on what form of course is inherent in it:
- nephrotic – oliguria and blood in the urine predominate;
- hypertensive – persistent arterial hypertension is noted;
- mixed - a combination of characteristics of the first two types;
- hematuric - detected during examination in the presence of red blood cells in the urine;
- latent – manifestations of all three symptom complexes are weak or absent.
It is important to know! Regardless of the form of the course, glomerulonephritis is characterized by the return of relapses. The risks of developing an acute episode increase in the autumn-spring period against the background of high humidity and low air temperature.
Description of complications
In severe cases and rapidly progressive development, diffuse glomerulonephritis can cause the following dangerous pathological conditions:
- acute heart failure;
- intracerebral hemorrhage;
- transient visual impairment;
- acute renal failure;
- chronic form of the disease.
Quite often, with rapid damage to the renal apparatus, preeclampsia or eclampsia develops - angiospastic encephalopathy caused by cerebral vasospasm and edema. The attack resembles an epileptic seizure and is characterized by lack of pupillary reaction to light, unconsciousness, increased blood pressure, and foam at the mouth. It can cause paralysis, paresis, and speech disorders. A cerebral hemorrhage can be fatal.
Establishing an accurate diagnosis
The diagnosis is made on the basis of the patient’s complaints, anamnesis described in the medical history, symptomatic manifestations, results of laboratory and instrumental studies.
The triad of clinical signs of acute glomerulonephritis is:
- swelling and pastiness of tissues;
- hematuria;
- high blood pressure.
Diagnostics is carried out to identify the form of pathology and involves performing the following manipulations:
- General and biochemical analysis of blood and urine;
- Ultrasound of the kidneys;
- Doppler ultrasound of renal vessels;
- radiography of the pelvic organs;
- MRI of the urinary tract and paired organ;
- kidney tissue biopsy;
- ECG.
These measures make it possible to differentiate inflammatory changes in the renal structures from cardiovascular diseases, disorders of internal secretion of hormones and metabolic processes, since swelling, especially in a child, may indicate problems in the vascular system, and not just in the excretory organs.