Acute glomerulonephritis - treatment and symptoms
You can determine whether you have this disease by the following symptoms:
- The most common sign of the disease is swelling. In the morning it appears on the face, and towards the afternoon it appears on the legs in the ankles and shins. A large amount of fluid begins to accumulate in the human body, which leads to an increase in body weight.
- High blood pressure. This can lead to heart failure.
- The amount and color of the secreted fluid changes (dirty red). But it happens that the color of the urine does not change, so it is necessary to take tests to check for the presence of red blood cells in it.
- Vision may be impaired.
- Headaches and dizziness.
If you notice the above symptoms, you should consult a neurologist or therapist.
Triad of symptoms in acute glomerulonephritis
Acute diffuse glomerulonephritis develops only after serious infectious diseases such as tonsillitis, otitis media, pneumonia, etc. During this period, unhealthy pallor of the skin and swelling of the entire body are observed. In some cases, patients experience acute pain in the kidney area.
Treatment of acute glomerulonephritis
There is a four-component treatment regimen.
- For two months you should take prednisolone 30 mg once a day. Gradually the amount of the drug is reduced until it disappears completely.
- Cytostatic until target remission.
- For a month, take five thousand units of heparin four times a day, gradually switching to aspirin.
- Dipiradamol 400 mg per day.
Be sure to consult your healthcare professional before using this regimen.
Prevention for acute glomerulonephritis
In order to avoid getting sick, you must constantly keep your body warm and avoid hypothermia. At the first symptoms of serious infectious diseases, you need to immediately begin intensive treatment, as well as eliminate foci of infection. Particular attention should be paid to the tonsils (tonsils).
Complications of acute glomerulonephritis
The most severe consequence of the disease can be kidney eclampsia. At this stage, seizures, severe headaches and high blood pressure may occur. The patient may also lose consciousness. After such attacks, irreversible consequences begin to develop, which lead to death.
Treatment of prostatitis with laser
Have you been struggling with PROSTATITIS and POTENTITY for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure prostatitis by taking it every day...
Read more "
Laser treatment has gained popularity relatively recently, but these days such therapy is being used more and more often. Moreover, this device is indispensable in cosmetology, for solving problems of skin imperfections, and for many other activities.
- What is laser therapy for prostatitis?
- How is the effect achieved?
- Is it possible to cure prostatitis with a laser?
- How is prostatitis treated with laser?
- Important points
Laser treatment of prostatitis is not just a modern therapeutic method, it is also quite effective. And the answers to all “how?”, “what?”, and “why?” - will be found below.
What is laser therapy for prostatitis?
Laser treatment is a physiotherapeutic method.
The device emits a luminous flux - this is a wave of a fixed length. The most commonly used optical radiation is in the infrared or red range. They can be generated in pulsed and continuous modes. The peculiarity of laser treatment of prostatitis is that the radiation penetrates directly into the tissues to any depth, where it has a healing effect on them. You also need to know that there are several types of laser therapy.
- Acupuncture - when the action is aimed at certain points.
- External - on the skin.
- Interactoral - this method involves the penetration of laser radiation directly into the rectum. It is especially effective for advanced forms of prostatitis.
How is the effect achieved?
Laser energy can work wonders. It improves blood supply to tissues, increases redox processes, stimulates the regeneration of damaged tissue areas, improves oxygen supply, and has anti-inflammatory and analgesic effects.
Thus, laser therapy in the complex treatment of prostatitis is an excellent tool in addition to medications.
Effect:
- Eliminating the possibility of developing an allergic reaction.
- Relieving pain
- Improving blood and lymph flow directly in the diseased organ.
- Reducing the likelihood of developing congestion in the prostate gland.
- Improving patency and increasing the effectiveness of antibiotics used.
- Stimulating the immune system.
Is it possible to cure prostatitis with a laser?
Laser treatment of prostatitis cannot be the only one in the fight against prostatitis for the simple reason that such a disease must be treated comprehensively, and therapy cannot take place without medications.
It is worth noting that if the patient consults a doctor in time, laser therapy is unlikely to be used. Usually, urologists prescribe it when prostatitis has become advanced, or to increase the speed of treatment of acute prostatitis (together with antibiotics).
The man feels improvement very quickly - after the first procedure. This therapeutic method is highly effective, that is, the laser cannot but give positive dynamics, and therefore it can be called a worthy “healer”.
Contraindications to laser therapy:
IT IS IMPORTANT TO KNOW! D. Pushkar told how to defeat prostatitis at home...
Such a pleasant treatment for prostatitis for 147 rubles...
- Tuberculosis.
- Diseases of the hematopoietic organs.
- Malignant tumors.
- The presence of serious illnesses.
- Photophobia.
- stroke/ischemia.
- Nervous system disorders.
When is laser therapy prescribed:
- Chronic prostatitis (congestive, bacterial, associated with infection of the genitourinary system).
- Prostatitis complicated by prostate adenoma.
- The need to supplement complex treatment with immunocorrective agents.
How is prostatitis treated with laser?
Treatment of chronic prostatitis with laser is carried out in a urology office on a special chair. In this case, the man should half sit and half lie on his back. This pose is necessary in order to completely relax the muscles of the lower body, in particular the muscles of the limbs and skeletal muscles.
The patient must first fill the bladder - without this, laser therapy is impossible. In addition to neon and infrared lasers, the doctor must also use a special gel that improves the passage of the rays. After the procedure is completed (and it does not last long), the physiotherapist performs breathing exercises with the patient.
Important points
The effectiveness of laser treatment for prostatitis depends on how comprehensive the program is developed by the doctor. And, as has already been written, if drug treatment is not carried out, the result from the laser, of course, will be, but you will have to wait much longer for it.
The age of the man and the degree of development of the disease are of great importance. The doctor must take into account other existing diseases and the results of studies. Of course, the diagnosis must be made as accurately as possible - a lot depends on this too.
The price of laser treatment for prostatitis ranges from 1000 rubles per session, depending on the clinic. Usually doctors prescribe several sessions of several minutes (from 5 to 10).
Priority problems of the patient in acute glomerulonephritis
Most often, the patient feels weak and unwell during illness. Over time, performance and appetite decrease. Fatigue increases. Fever may develop, accompanied by hot flashes.
Are they recruited into the army with acute glomerulonephritis?
If you are diagnosed with this disease, you will be able to avoid being drafted into the army. If, after your recovery, tests show that pathological changes persist in your urine, then you will be unfit for military service. A conclusion about your fitness category is made after a re-examination. In the absence of renal dysfunction, it will not be possible to avoid conscription into the army.
Urinary syndrome in acute glomerulonephritis
During the period of illness, the patient's urine volume decreases significantly. The daily amount of fluid released is usually no more than 700 ml. This process occurs due to inflammatory changes in the glomeruli. During uroscopy, you can notice that the urine is cloudy and has sediment due to the large number of red blood cells in it.
To prevent this disease, all preventive measures must be followed. If you find any of the symptoms described above, be sure to make an appointment with a therapist.
Chronic glomerulonephritis is a pathology when the kidney glomeruli become inflamed, and this process is sluggish. This disease has a very low prognosis for complete recovery; in fact, it is lifelong. Here the most likely consequences are kidney failure, a person needs hemodialysis on an ongoing basis, and there is often a need for a donor organ transplant. Chronic glomerulonephritis in children is no less common than in adults, which makes this disease even more dangerous. Symptoms and treatment of pathology should be studied and carried out only by experienced specialists, in view of its special danger, it must be said right away that no self-medication is completely unacceptable!
The complexity of the pathology also lies in the fact that it is not always possible to establish the exact causes of its occurrence. However, very often there is a direct connection between inflammation of the glomerular type, which has an infectious form and the nature of an allergy. Such an illness can be acute or chronic, but no matter what the illness is - acute or chronic, nature is always the same. First, acute glomerulonephritis is observed, and the chronic form occurs in most cases because ineffective therapy for the acute form of the disease is carried out or it is not carried out at all. The etiology of the disease has not yet been fully studied.
Another reason may be that there is a certain provocateur in the human body that acts on an ongoing basis. The process of inflammation in the kidneys occurs gradually, and there may not be an acute phase, since pathogens affect the body for a long time. Such infectious foci in a chronic form are most often streptococcal:
- they may be in the nasopharynx (here it could be tonsillitis, pharyngitis or sinusitis);
- also often observed in the oral cavity (caries occurs here);
- gastrointestinal tract (we are talking primarily about hepatitis and cholecystitis);
- in the genitourinary organs (cystitis often affects here).
There is another factor that can have a negative impact on immunological kidney damage; we are talking about sensitization of the body, which has a long-term form. This is most often observed in people suffering from various types of allergies, especially if there is a strong reaction to the allergen. And here we often see people who are affected by chronic intoxication (those suffering from alcohol dependence and constant consumption of nephrotoxic drugs).
There is a certain category of people who have a predisposition to glomerular lesions from birth. There is a congenital defect in the immune system that prevents the body from dealing with pathogens that enter it. Thus, immune complexes begin to be deposited in the nephrons, that is, protein-type formations that have a destructive effect on the glomeruli. Chronic glomerulonephritis and the classification of this disease imply different forms of the disease.
If chronic glomerulonephritis of a secondary form is observed, then everything goes together with ailments that are distinguished by an immunoinflammatory form: endocarditis, rheumatism, lupus erythematosus and some others. In the pathogenesis of pathology, the main role is played by the immune response mechanism. The formation of a protein type occurs, which causes disruption of microcirculation. Due to such influence, after some time the renal glomeruli undergo dystrophic changes. The kidney tissue begins to thicken and become fine-grained, as a result the organ becomes smaller in size and weight.
When the disease begins to progress, 2 stages are observed:
- If the kidneys retain the ability to function normally, then this is a compensated form.
- If the functions of the organ are impaired, chronic or acute renal failure is observed, then we are talking about a decompensated form.
It is noteworthy that the disease can progress very slowly, taking 10 years or more. And there is also moderate progression, then from the onset of the pathology it is observed for 2-5 years, and the disease can subside for a certain time, and then the period of exacerbation begins again.
Glomerulonephritis: choice of sanatorium treatment
Patients with glomerulonephritis can receive spa treatment. They are recommended resorts in their climatic zone.
Who can be treated in nephrology sanatoriums:
- Convalescents (recovered) after acute glomerulonephritis
- Patients with chronic glomerulonephritis in stable condition, without high arterial hypertension and edema, with normal blood protein levels
- Stable patients with moderate nephrotic syndrome
- Kidney transplant patients undergoing recovery.
Choosing a sanatorium with the appropriate conditions and procedures, selecting a suitable climate zone is a responsible matter and should be carried out by a nephrologist. Sanatorium treatment helps you recover much faster after therapy, however, if you want to go to a specific resort, be sure to consult your doctor.
Vaccination for glomerulonephritis: yes or no?
Unfortunately, children also suffer from this disease; pediatricians and pediatricians treat them. More often this is an acute form of post-streptococcal glomerulonephritis, which in 80% of cases ends in recovery. Concerned parents naturally have a question: is it possible to vaccinate for glomerulonephritis?
The question is not easy. According to Guidelines MU 3.3.1.1095-02 dated January 9, 2002, glomerulonephritis is not a contraindication for vaccinations according to the calendar. After recovery from acute nephritis, vaccination can be performed 6 months later; for nephrotic syndrome, after completion of treatment with corticosteroids. On the contrary, the Ministry recommends that patients be vaccinated against influenza, since all acute respiratory viral infections worsen the prognosis for renal pathology (this is a fact!).
On the other hand, if the function of the immune system is impaired and its “autoimmune mood”, the introduction of foreign proteins contained in vaccines and serums can provoke the development of glomerulonephritis. Here, no one can guarantee 100% safety, and even if the child is 7 years old, the risk of complications during vaccination still exists. With a progressive course of glomerulonephritis, children are not subject to vaccination.
Viral hepatitis and glomerulonephritis
Quite often there is a combination of viral hepatitis C and glomerulonephritis in one person. What should I do? The combination of these diseases is not favorable. Can hepatitis C virus be treated for glomerulonephritis? There may be a twofold situation here.
If a person had hepatitis C before glomerulonephritis was detected, then the virus can cause secondary kidney damage, as it persists and “harms” not only the liver, but also any organs, including the kidneys. In this case, it is necessary to treat viral hepatitis; after the virus is destroyed, the glomerulonephritis itself is treated with appropriate drugs.
What signs are observed?
Symptoms of the pathology should be determined by the clinical form; 50 percent of patients have a latent form of the inflammatory process. In the vast majority of cases, the disease expresses itself as an isolated type of urinary syndrome, while the amount of proteins and leukocytes in the urine is moderate. Chronic glomerulonephritis has symptoms that are often different, their nature is influenced by many factors - the individual characteristics of the human body, the severity of the disease.
If we talk about swelling and arterial hypertension, then they are not common with this disease. It is noteworthy that the latent form of the disease can occur completely without any symptoms for 10-20 years. And only when scar tissue begins to rapidly spread, instead of dead glomeruli, uremic signs begin to appear.
There is also a hematuric form of the disease, which has its own symptoms - anemia begins to actively develop, as red blood cells are constantly excreted in the urine. Moreover, this can sometimes be examined without any instruments when there are blood impurities in the urine. However, the kidneys are functionally quite normal, no swelling is observed.
If there is a hypertensive form, then there is arterial hypertension, and a weak expression of urinary syndrome is observed; hypertension is generally dangerous. In this case, there is a characteristic sign - the pressure is extremely unstable, it can change sharply during the day; the hypertensive form can have similar signs. Cardiac function may also be impaired, and suffocation may occur, so hypertension can lead to very serious consequences.
Almost 25 percent of patients experience nephrotic syndrome and there are certain symptoms:
- severe swelling, and this is most visible on the face and legs;
- swelling can be hidden, in which case it adds little weight to the person;
- an excess of cholesterol levels is observed in the blood.
However, it is necessary to say separately about the most severe version of this disease - the mixed form, which can very quickly lead to kidney failure. In this case, there are the following symptoms:
- pronounced swelling;
- blood and protein impurities are found in the urine;
- hypertension and anemia may occur;
- the specific gravity of urine decreases;
- the kidneys lose their ability to filter.
If the first signs of uremia appear, then renal failure begins, that is, the kidneys can no longer concentrate urine, metabolic products are poorly excreted. A large amount of urea begins to appear, which begins to poison the body with nitrogen-type substances.
If a person begins to develop uremia, it shows the following symptoms:
- the person feels very weak;
- nauseated, sometimes vomiting, and this does not alleviate the person’s condition;
- dizziness and pain;
- you are constantly thirsty, but water does not quench your thirst for long;
- the skin and mucous membranes are subject to dehydration;
- the person begins the process of exhaustion;
- an ammonia smell occurs;
- uremic coma.
Treatment of chronic glomerulonephritis
Anka, writes September 4, 2008, 01:55
- ← ctrl
- Page 3 of 5
- ctrl →
- 1
- 2
- 3
- 4
- 5
Hello dear fellow sufferers! I have been suffering from glomerulonephritis since 2002. 7 years. Before this, there were frequent sore throats with fever, otitis media, etc. But the doctors told me not to remove the tonsils - supposedly I would outgrow these problems, but it didn’t work out. And now I see that the attitude towards tonsillitis has changed: otolaryngologists unanimously declare that if tonsillitis occurs more than once a year, the tonsils must definitely be removed. Now I tell all my friends whose children often get sore throats to think about how potentially dangerous this is. They also cause complications for the heart - rheumatism is no better than glomerulonephritis.
I was probably lucky (if it is appropriate to say this in this case))))) - I have a sluggish form of hematuria. A biopsy was done in 2003 for membranous proliferative glomerular nephritis. Although now doctors say with confidence that the pathologists were mistaken - with such a bad form I should already be on dialysis, they do not recommend redoing the biopsy, since the treatment, in principle, will not change.
There are slightly red blood cells in the urine, with an exacerbation of 170, traces of protein in the general analysis, there are no changes in the blood, pressure and swelling do not bother. I have been taking Canephron for about 5 years, but I know that it is more indicated for pyelonephritis and urolithiasis. I try to drink chimes, but it gives me a headache. Of course, I try to follow a diet, but I admit that I’m a sinner: I love meat, chocolate, and coffee)))))) Although, of course, I limit myself, because I really love smoked perch, and I only allow myself to look at it)
I went to Bayram-Ali 2 times and developed urolithiasis. Apparently, there was a tendency in the body to form stones, and after the second trip there were countless numbers of kidney stones. I drank cystone for 2 years and was cured. I don’t want to go to Turkmenistan anymore, and those who have been going there for 20 years say that the climate there has already changed and the humidity is far from 3 percent - that is, the effect is no longer the same.
I know that the disease is autoimmune and incurable. I’ve already read everything I can and I understand the diagram of the disease well: the kidney consists of about two million nephrons, during each exacerbation of the disease (infection, hypothermia entering the body), thousands of them die (THEREFORE, COMRADES, BE AWARE, BE AWARE AND BE AWARE AGAIN). The process is irreversible. But about 5 years ago, sick friends told me that there is a sanatorium in Egypt, somewhere in the desert on the Nile River, where glomerulonephritis is treated. They take people there with favorable forms of disease (small protein, slight changes in urine) and supposedly people recover. I didn’t find out anything in detail then, because they didn’t take stones. And now there seem to be no stones) Maybe someone heard something? My nephrologist is very experienced and wonderful, but he doesn’t believe in this. And I think science is science, and there are plenty of miracles too)))) And one more thing: despite everything, you must sincerely believe that everything will be fine. point in getting ready for dialysis, because it seems to me that you can’t be ready for this anyway; in any case, it will be a colossal stress. So why darken the present for yourself, because this gloomy future may not come?)) But thoughts are material - believe me, friends)
I myself am not an optimist by nature. But just yesterday I was discharged from the hospital once again and a 33-year-old girl was lying with me. She had been on dialysis since September 1. She had subacute glomerulonephritis as a complication after pneumonia; within 2 months her kidneys stopped working. She is great, she doesn’t give up, doesn’t despair and doesn’t give up. I visited all the doctors and am sure that I will get out. Every day he tells himself: “I will get better. I will definitely get better. I simply cannot have it any other way - I will be healthy no matter what.” And you know, I won’t be surprised if her kidneys start working sooner or later)) Her belief in this is so strong) Moreover, her kidneys are of normal size and partially sclerotic. So I also decided to open the chakras))))), take up meditation and self-hypnosis)))
Diagnosis of the disease
When taking an anamnesis, it is necessary to especially highlight such factors as acute renal inflammation, whether there are foci of an infectious type, or systemic pathologies. Considering that latent pathology is often observed, a laboratory diagnostic method is most often used:
- First of all, you must do a general urine test;
- blood analysis;
- immunological tests.
However, such tests are not enough to make an accurate diagnosis, so it is still necessary to conduct diagnostic studies:
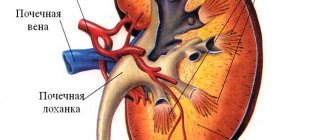
- renal ultrasound, since with such a disease the organs tend to shrink, since the tissues are sclerotic;
- in order to assess the condition of the kidney tissue, it is necessary to use an x-ray study;
- to identify hidden edema that may be in the internal cavities, it is necessary to do a cardiogram;
- the fundus of the eye is examined to determine arterial hypertension;
- If there are certain difficulties in diagnosis, a renal biopsy should be done.
Chronic glomerulonephritis, its diagnosis may involve other methods, it all depends on the specific situation.
Is it possible to cure glomerulonephritis forever?
Glomerulonephritis can occur in two forms : acute and chronic. The acute form is curable with timely diagnosis and correct treatment methods.
If time for drug treatment was missed, and the disease smoothly turned into a chronic form, then you cannot completely get rid of this disease, but you can maintain your body in a state where the disease cannot develop further and affect more and more kidney elements.
In this case, the doctor will prescribe a specific diet and tell you about following a special regimen that can protect the patient from developing a new relapse of the disease.
If a complete cure cannot be achieved, the doctor recommends following all established rules and preventive measures so that the symptoms become less noticeable. Sometimes, with successful therapeutic treatment, it is possible to achieve temporary disappearance of symptoms.
It is necessary to support the body for as long as possible before a new relapse occurs.
Treatment options
How to treat chronic severe glomerulonephritis? First of all, it is necessary to say about a strict protective regime for preventive measures; it is also necessary to promptly treat exacerbations and stop the progression of the disease:
- It is very important to adhere to a special diet when it is necessary to significantly reduce the consumption of salt, alcoholic beverages and spicy foods. All liquid that is drunk must be taken into account; if proteinuria is observed, then it is necessary to eat more protein foods;
- Do not overwork, expose the body to hypothermia, high humidity is dangerous;
- It is worth taking all measures to ensure that infections with infectious and viral diseases are kept to a minimum. Contacts with allergens should be minimal; you should not be vaccinated.
Chronic glomerulonephritis also implies treatment when drug therapy is actively used for pathology:
- immunosuppressive drugs;
- anti-inflammatory drugs that are non-hormonal;
- if hematuria is observed, then anticoagulants are used.
If there is edema, symptomatic treatment is used, diuretics are used, and the use of antihypertensive drugs helps normalize blood pressure. When an aggravated period is observed, it is better for the patient to be treated in a hospital setting, and when remission occurs, then supportive therapy is necessary; treatment in sanatoriums and resorts has proven itself to be excellent. And you need to regularly undergo the necessary medical examinations.
Herbs for glomerulonephritis: decoctions and inhalation
To provide assistance, in addition to drug recovery or folk remedies, an integrated approach is needed to treat such a disease, and herbal medicine must also be used. During the treatment period, it is necessary to completely abandon bad habits.
For inhalation, you can take birch and black currant leaves, lavender, nettle and strawberry leaves.
You should pour boiling water over it all and breathe in the steam, covering your head with a thick towel or any other cloth. With this method of treatment, the beneficial substances contained in the components have a beneficial effect on the entire body as a whole.
To help with glomerular nephritis, a decoction of herbs such as:
- Oregano;
- Centaury;
- Black currant;
- St. John's wort;
- Millennium.
Herbs, inhalations and traditional medicine can only remove severe symptoms. For glomerulonephritis, a visit to the doctor is mandatory.
About the prognosis of the disease
Is it possible to cure the disease? If we talk about the prognosis of the disease, then everything is directly dependent on the clinical form, as well as on how severe the disease is:
- If there is a latent form of the disease, then it can proceed for a very long time without any symptoms, then the disease begins to slowly progress. As for the hematuric form, a fifth of patients are completely cured when steroid drugs are used in treatment with medications that help reduce blood clotting;
- inflammation of an uncomplicated type, which is detected in children under the age of 6-7 years, can be cured in 80 percent of all cases. If adequate hormonal therapy is used;
- If hypertensive syndrome is observed, then it is necessary to take medications for blood pressure on an ongoing basis. Therapy must be adequate, otherwise heart failure may occur, atherosclerotic plaques will begin to form, and the person risks having a stroke;
- but the edematous form in most cases is associated with an unfavorable prognosis; the appearance of a necrotic form of the disease is evidence that the kidneys simply cannot fully carry out the filtration process, so in all likelihood, renal failure will soon occur;
- The mixed form of the disease has the most negative prognosis.
If there is no timely and effective treatment, there are predisposing factors, the disease progresses quickly, so that any of the forms can be such that a terminal stage will occur very soon. And here hemodialysis, as well as kidney transplantation, is necessary for the rest of his life. It is very important to start timely treatment, since complications of chronic glomerulonephritis can be irreversible. It is noteworthy that CG in a child, if detected in a timely manner, is often treated very successfully.
Is prostatitis curable? Treatment methods and prognosis
Faced with inflammation of the prostate gland, every man sooner or later wonders whether prostatitis can be treated. To assess the chances of complete restoration of organ function, it is necessary to accurately understand the mechanism of development of the disease.
Prognosis for acute prostatitis
Whether prostatitis can be treated depends, first of all, on the type of disease. According to the nature of the course, acute and chronic prostatitis is noted. Due to its development, the disease can be infectious or non-infectious.
The cause of acute inflammation is infection of the prostate gland. The infection usually enters the organ from the bladder or through the bloodstream. The causative agent of the disease can be both opportunistic microorganisms (Escherichia coli and Pseudomonas aeruginosa) and sexually transmitted pathogens (chlamydia, ureaplasma).
Bacterial prostatitis is curable if the disease is diagnosed in a timely manner. Treatment is carried out using antibacterial drugs. The drug is selected taking into account the causative agent of inflammation. As a rule, drugs of the penicillin or tetracycline group, fluoroquinolones, are used. Additionally, a number of drugs are prescribed for symptomatic therapy - anti-inflammatory drugs, antispasmodics, alpha-blockers for prostatitis, immunostimulants. It is possible to prescribe a course of physiotherapy after relieving acute inflammation.
Acute prostatitis is treated within several weeks, the course of treatment rarely exceeds two months. Then the patient is prescribed medications with herbal composition to normalize the function of the prostate gland, which should be used over a long course. As a rule, timely detected acute infectious prostatitis is successfully treated and does not cause complications such as impotence or infertility.
This form of the disease can be suspected by rapidly increasing symptoms. Characteristic signs of prostatitis are pain when urinating, incomplete emptying of the bladder, spasms in the perineum and lower abdomen.
Prognosis for chronic prostatitis
You should consult your doctor about whether chronic prostatitis is being treated. As a rule, this form of the disease develops as a result of incorrect treatment of acute inflammation of the prostate gland, or against the background of metabolic disorders in the pelvic organs.
Whether this type of disease can be cured depends on the following factors:
- patient's age;
- stage of the disease;
- severity of symptoms.
With age, the size of the prostate gland increases. This is due to the natural aging process of the body and changes in the hormonal background of a man. The older the patient, the more difficult it is to cure the disease.
Chronic prostatitis develops due to impaired blood circulation and lymph outflow in the pelvic organs. In most cases, it is diagnosed in obese men who lead a sedentary lifestyle.
Symptoms of this type of prostatitis include impaired urination, weakened erection and pain. The prostate gland swells, a thickening of the secretion of the organ is observed, which can cause the development of infertility in a man due to changes in the composition of the seminal fluid.
Whether prostatitis can be completely cured depends on how soon the disease is diagnosed. The chronic form of inflammation develops slowly; from the onset of disruption of blood microcirculation in the organ to the development of inflammation, it can take up to 7 years. At the initial stage, prostatitis can be successfully treated by normalizing the trophism of the organ. To do this, the patient is prescribed a number of medications and physiotherapeutic methods aimed at normalizing the tone of blood vessels and the muscles of the pelvic organs.
In the later stages of congestive prostatitis, irreversible changes occur in the organ. Drug therapy becomes ineffective with long-term use, so the only way to get rid of the disease is surgery. In this case, both partial and complete removal of the organ (prostatectomy) is practiced.
Treatment methods for chronic prostatitis
Whether chronic prostatitis in men is treated depends on when the man went to the doctor. At the initial stage of organ trophic disturbances, drug therapy is used. For treatment use:
- prostate protectors;
- drugs to improve blood microcirculation;
- alpha-blockers;
- immunostimulants.
To relieve inflammation, patients are advised to take non-steroidal anti-inflammatory drugs. The course of treatment rarely exceeds 10 days. Then the therapy continues with herbal preparations, the action of which is aimed at improving blood microcirculation in the inflamed organ. Since the disease is accompanied by urination problems, drugs from the alpha-blocker group are used. Their action is aimed at relaxing the muscles of the walls of the bladder and prostate gland. The medicine acts directly on the receptors that regulate muscle tone. This allows you to reduce the pressure of the prostate on surrounding tissues and normalize the outflow of urine by relaxing the bladder.
Chronic prostatitis is treated with immunostimulants. After removing inflammation and reducing swelling, it is important to prevent the development of an exacerbation of the disease, which is often observed with the slightest hypothermia or a drop in immunity.
Physiotherapy - treatment with electric current, magnetic field, ultrasound - allows you to restore blood circulation and metabolic processes in the cells of the organ. As a rule, with timely detected congestive prostatitis, a properly developed drug and physiotherapeutic treatment regimen can minimize the risk of disease progression in the future.
Radical treatment method
Having figured out whether prostatitis is curable or not, it is important to understand that in some cases medications will have to be taken for many years. Over time, the effectiveness of drug therapy decreases, so the only way to get rid of the disease is through surgery. Depending on the severity of inflammation and swelling of the organ, either partial removal of the organ or radical prostatectomy is practiced.
The first place among the methods of influencing the prostate is occupied by minimally invasive operations and laser treatment. During this procedure, layer-by-layer burning of small areas of the prostate gland is carried out, the tissue of which has changed as a result of prolonged swelling. The operation lasts no more than a few hours, rehabilitation takes several days. It will take no more than one month for complete recovery. The advantages of minimally invasive methods are the absence of risks of bleeding and complications. As a rule, such intervention does not affect reproductive function and erection in any way. Feedback from patients allows us to conclude that laser treatment of the prostate gland for prostatitis is the most effective and efficient way to treat chronic prostatitis.
Useful tips
Prostatitis imposes a number of restrictions on the patient’s life. The following will help speed up prostate recovery:
- balanced diet;
- rejection of bad habits;
- regular sex;
- moderate physical activity.
To get rid of the disease, an integrated approach is needed. In addition to drug treatment, physiotherapy, massage, and a set of exercises are practiced to normalize blood circulation in the pelvic organs. Additionally, patients are prescribed a diet; foods that are good for men's health are introduced into the diet - citrus fruits, nuts, pumpkin. It is recommended to take flaxseed and pumpkin oil as dietary supplements.
Chronic prostatitis requires careful attention to your own health, otherwise any hypothermia or stress can cause an exacerbation. Frequent exacerbations of prostatitis lead to progression of the disease and disruption of the functionality of the prostate gland. To ensure that the urge to urinate at night becomes a thing of the past and does not return, in addition to taking medications to relieve inflammation, it is necessary to take immunostimulants. To strengthen the nervous system, taking B vitamins, magnesium supplements, and sedatives is indicated.
It is important to remember: any disease can be successfully treated if diagnosed in a timely manner, and prostatitis is no exception. If the patient does not initiate the disease, follows the doctor’s recommendations and does not self-medicate, it is possible to get rid of prostatitis.
Preventive measures
All preventive measures are aimed at eliminating external pathogens:
- First of all, it is necessary to promptly and effectively treat ailments of the streptococcal type, since they are the most nephrotoxic. It is also necessary to combat other pathogens in a timely manner;
- all chronic lesions must undergo sanitation;
- if the body is hypersensitive, then it is necessary to minimize all contacts with the allergen;
- if there is a need to take nephrotoxic drugs, then this must be done with the utmost caution and everything must be monitored by a doctor:
- it is necessary to adhere to a healthy lifestyle, reduce the consumption of alcoholic beverages to a minimum;
- It is very important that the body is not exposed to hypothermia, overheating, or high humidity.
Particular attention to active prevention should be paid to people who have a predisposition at the genetic level. However, you should not think that if there is a hereditary defect in the body, then the person will certainly get sick; as a rule, other factors are also needed.
Chronic glomerulonephritis, regardless of its form, sooner or later leads to the development of a secondary wrinkled kidney and chronic renal failure.
Diagnostics
The diagnosis of chronic glomerulonephritis is made by a nephrologist. He directs the patient to general and biochemical blood tests, and a general urinalysis. Kidney ultrasound, kidney biopsy, excretory urography and nephroscintigraphy are also performed.
Treatment
Treatment of chronic glomerulonephritis is long-term and includes drug therapy, diet, and selection of the right physical activity. Most of the treatment takes place on an outpatient basis; the patient does not stay in the hospital for long. A person suffering from chronic glomerulonephritis must strictly adhere to a daily routine. A very important part of treatment is a diet that limits the amount of protein, salt and liquid.
For the treatment of chronic glomerulonephritis, anti-inflammatory drugs are prescribed, most often these are hormonal drugs and drugs that suppress the immune system. However, in the later stages of the disease such treatment is contraindicated. Blood thinners and diuretics are also prescribed to relieve swelling and remove fluid from the body. In case of exacerbation, antibiotics or antibacterial drugs are prescribed if the cause of the exacerbation is infection.
After the exacerbation subsides, treatment in specialized sanatoriums is indicated.
Treatment abroad
If you are not short of money, then it becomes possible for you to receive treatment in university clinics in Germany, which represent the highest standards of medical care for patients. Based on university bases, they have the most modern equipment and technologies, and qualified specialists. The university clinic in Freiburg is widely known; there are excellent and multidisciplinary centers in Baden-Baden, Tübingen, Munich, Frankfurt, Düsseldorf, and Hannover.
Quite often, patients also seek treatment in Israel, known for the high quality of medical services. In both Israel and Germany, in addition to therapeutic treatment, in later stages, dialysis and, if necessary, a kidney transplant are performed. When treated abroad, patients with glomerulonephritis sometimes achieve stable remission.
However, in order to go abroad for treatment, the patient first needs to choose a clinic and a doctor, then find out the cost of hospital stay (bed-day), examination (our tests will not work), the treatment itself, and pay for it. After this, an official invitation for treatment will be sent from the clinic, with which you can apply for a visa to enter the country (today, a visa to Israel is not required).
Traditional medicine and glomerulonephritis
Traditional methods of treatment primarily include medicinal herbs. It is recommended to use the following preparations for the treatment of glumerulonephritis at home:
- Collection No. 68: calamus root 1, oak bark 2, St. John's wort herb 5, calendula flowers 3, flax seed 2, peppermint leaf 2, kidney tea 3, knotweed herb 4, thyme herb 2, lingonberry leaf 3, rose hips 1, herb marsh cudweed 6 parts
- Collection No. 70: Marshmallow root 2, speedwell herb 5, sweet clover herb 3, St. John's wort herb 5, nettle leaf 4, peppermint leaf 2, motherwort herb 8, chamomile flowers 1, yarrow herb 2, rose hips 3 parts.
The use of the mixture can improve kidney function, general well-being, and reduce protein loss in the urine. But remember, treatment with folk remedies does not replace the main therapy for the treatment of glomerulonphritis, but only expands its capabilities.
Glomerulonephritis: alternative methods?
Ukrainian healer Bolotov B.V. and his follower, comrade-in-arms Naumov D.V., created their own methods of healing. Let us immediately make a reservation that these methods contradict the canons of modern medicine and the principles of treatment of glomerulonephritis both in Russia and abroad, and are not recognized by official science.
The method of Bolotov and Naumov suggests that patients “dissolve toxins” using table salt, 1 gram. after meals up to 10 times (!) a day and generally actively salt food, even fruits. Doctors, on the contrary, strongly warn patients with glomerulonephritis against consuming more than 4 g of salt per day (this includes salt naturally contained in food products).
As we see, this “treatment” largely contradicts medical recommendations on the nutrition of patients with glomerulonephritis, but a number of patients are still inclined to use unconventional methods in treatment. However, it is important to remember that kidney disease is a very serious illness, and it is not worth risking your health.
Homeopathic medicines and other non-traditional remedies
The most important thing to remember when using the following remedies is: they are not drugs as such and cannot be used as monotherapy (alone on their own)! Homeopathic treatment can only be used as an auxiliary treatment, against the background of the main therapy, and only after consultation with a nephrologist! The most popular drugs:
- produces complex homeopathic preparations of mild action, non-toxic, normalizing body functions, improving drug tolerance. Here is a complete list of Hel drugs for the treatment of glomerulonephritis: Albumoheel S (correction of albuminuria), Apis-Homaccord (for edema), Lymphomyosot (antitoxic effect, prevents the formation of edema), Reneel (for infection), Engystol N and Ren suis-Injeel (in recovery period after glomerulonephritis), Rauwolfia compositum (with increased blood pressure).
- Argo products are made from natural ingredients: medicinal plant extracts, natural minerals, vitamins, microelements. They belong to dietary supplements, are produced here in Russia and are approved for use by the Institute of Nutrition of the Academy of Sciences and the Ministry of Health. Patient reviews of these drugs are mostly positive.
You may be recommended other drugs for treatment, for example, Chinese medicine: Tianshi drug, amino acid concentrates from sports nutrition departments. For example, is it possible to take L-carnitine power system? Of course, you should not try to treat glomerulonephritis with them and compensate for protein deficiency in proteinuria; for this, there are special balanced preparations specifically for patients with kidney diseases, including those diagnosed with glomerulonephritis.
Preventive actions
Prevention of the hematuric form of chronic glomerulonephritis consists of following the recommendations:
- avoid hypothermia or overheating of the body;
- promptly treat infectious and other diseases;
- Healthy food;
- eliminate all existing chronic infectious foci;
- do not abuse alcohol;
- quit smoking;
- take any medications carefully, only with the permission of a doctor;
- avoid contact with poisonous and toxic substances;
- strengthen the immune system.
These preventive measures should be followed both during the period of remission of the disease and in the presence of a predisposition to the development of a pathological condition.
Symptoms
All chronic glomerulonephritis (and hematuric glomerulonephritis is no exception) have 3 stages, each of which has certain symptoms:
Recommended topic:
Treatment of glomerulonephritis with folk remedies
- Compensatory. It is distinguished by the absence of visual signs of disease. The operation of the natural filter is not impaired. The kidneys remain active and fully cope with their functions. There may be slight swelling towards the end of the day and a slight increase in blood pressure. A urine analysis according to Zimnitsky reveals a moderate presence of altered red blood cells and protein. The density of urine changes.
- Decompensatory. Associated with the progression of the disease and the appearance of the first signs of renal failure. The patient experiences weakness, headache, vomiting, and thirst. The skin becomes dry. Polyuria is observed (an increase in the daily volume of excreted urinary fluid), and blood pressure increases. In a general urine analysis, the presence of casts, altered red blood cells and protein is clearly expressed.
- Uremia. The stage at which the kidneys can no longer filter the blood. In this case, we can talk about the presence of chronic renal failure. The patient experiences severe migraines, confusion, and an unpleasant ammonia odor from the mouth. Coma may occur.
The hematuric form of chronic glomerulonephritis has another significant visual symptom - the detection of blood impurities in the urine. The clinical course of the disease can develop in two ways:
- Microhematuria (sluggish progressive hematuria). The increase in symptoms occurs gradually. Over time, they are accompanied by signs of kidney swelling and growing arterial hypertension. When this happens, the patient's condition deteriorates sharply.
- Recurrent macrohematuria. Its symptoms appear mainly after the patient has suffered viral infections. The presence of blood in the urine can be observed for a long time (from several months to several years). During the remission period, all tests are normal.
The hematuric form of chronic glomerulonephritis requires immediate contact with a qualified nephrologist to confirm the diagnosis and prescribe adequate treatment methods.
Causes
The causes of the disease are conventionally divided into two groups.
Inflammatory factor
Glomerulonephritis may appear after a person suffers from the following diseases:
- angina;
- tuberculosis;
- typhoid fever;
- flu;
- rubella;
- chicken pox;
- herpes.
Autoimmune factor
In this case, the disease manifests itself as a result of a malfunction of the human immune system, when the body does not correctly perceive kidney cells (as foreign). Most often, this pathology occurs after suffering an acute form of infectious or inflammatory diseases.
The following specific factors can also be attributed to the reasons:
- long-term presence of various infections in the human body;
- hereditary factor, predisposition of the body;
- severe hypothermia of the body;
- lack of vitamins in the body, which greatly reduces resistance to various diseases;
- presence of streptococcus on the skin;
- damage to the body by various toxins (mercury or lead);
- snake or bee venom may also pose a danger;
- the presence of an acute allergic reaction.
Causes of the disease in children
The causes of glomerulonephritis in children are not much different from adults. But among the many factors, we can highlight those that are most common in children:
- skin lesions, namely strepoderma and streptococcal dermatitis;
- the presence of a bacterial or viral infection in the body;
- neglect of allergic reactions;
- negative reaction to vaccinations.
Complications of glomerulonephritis
When the disease in question is diagnosed in the acute stage, it is completely cured without consequences in most cases. In rare situations, glomerulonephritis becomes complicated - symptoms and treatment may be determined incorrectly, or the pathology may be detected in a subacute or chronic form. The most severe consequence of glomerular damage is renal failure. It progresses over the years and leads to the replacement of normal connective tissue.
Other complications that diffuse glomerulonephritis provokes:
- thrombosis;
- persistent arterial hypertension;
- anemia;
- heart failure;
- eclampsia;
- visual impairment;
- intracerebral bleeding;
- uremia;
- pulmonary edema.
Glomerulonephritis - causes
There is a primary and secondary form of the described disease. The latter option arises as a consequence of serious systemic violations. For example, kidney glomerulonephritis can debut against the background of the following pathologies:
- rheumatoid arthritis;
- Alport syndrome;
- lupus erythematosus;
- Fabry disease;
- antiphospholipid syndrome;
- hepatitis C;
- vasculitis;
- endocarditis;
- Coxsackie virus, Epstein-Barr;
- periarteritis nodosa;
- amyloidosis;
- Goodpasture's syndrome;
- Henoch-Schönlein disease;
- malignant tumors.
The primary type of glomerular injury is an autoimmune disease. Poststreptococcal glomerulonephritis often develops, sometimes other bacteria or parasites act as the causative agent. To fight pathogenic microorganisms, the immune system secretes specific antibodies. If they are not eliminated on their own, these complexes accumulate in the glomeruli. Later, they provoke inflammatory processes, and the body’s defense system begins to attack its own kidney tissue.
Treatment with folk remedies
The use of traditional methods is possible only after consultation with your doctor.
Infusions that help relieve swelling and lower blood pressure
- 4 tablespoons of flaxseeds are mixed with 3 tablespoons of dried birch leaves and 3 tablespoons of dried steelhead root. The resulting mass is poured with 500 milliliters of hot water and left to infuse for 2 hours. Take 3-4 tablespoons before meals;
- Black elderberry flowers must be dried and poured with a glass of boiling water. The resulting mixture is cooled and taken 3 times before meals;
- 10 grams of dried fennel fruits are poured with a glass of boiling water and left to infuse for half an hour. The resulting infusion is taken 100 milliliters 20 minutes before meals.
Decoctions
- 10 grams of strawberry leaves are mixed with 2 tablespoons of birch leaves and 3 tablespoons of flax seeds. The resulting mixture is poured with 800 milliliters of boiling water and boiled for 5 minutes, then left for half an hour and drunk 1/2 cup before meals;
- 5 tablespoons of processed oats are poured into a liter of milk and boiled until the grain is ready. Take 100 grams three times a day;
- 80-100 grams of finely chopped and dried burdock root are poured with a liter of cold water and boiled until half of the water has evaporated. Then add 2 tablespoons of honey or sugar. Take 100 milliliters 3 times a day;
- 40-50 grams of lingonberries are poured with 400 milliliters of boiling water and simmered for 5-10 minutes. Then the broth is infused for 1 hour. Once ready, filter it and drink half a glass before meals and half after.
Be sure to read:
Signs of cholecystitis and treatment at home
Tinctures
- 40 grams of crushed dandelion leaves are poured with 100 milliliters of vodka and left in a dark place for 12 hours. Once ready, take 1 teaspoon three times a day;
- dilute 30 drops of hawthorn tincture in a glass of cold water and drink this remedy 3 times a day.
A very useful remedy for glomerulonephritis is freshly squeezed celery, birch or pumpkin juice.
Baths
- finely chopped pine branches and fir cones are poured into 3.5 liters of water and boiled over low heat for half an hour, then the broth is infused for an hour, filtered and poured into a warm bath;
- you can take a bath in which 350 grams of horsetail are placed, the duration of the procedure is usually 30-60 minutes;
- 100 grams of birch leaves, 100 grams of knotweed herb and 100 grams of sage are poured with 500 milliliters of boiling water and left for exactly 24 hours. Then the mixture is filtered and a bath is poured, which must be taken for 15-20 minutes.
Folk remedies for kidney cysts.
How to treat urinary incontinence in women.
Learn more about the treatment of pyelonephritis with folk remedies.
Prevention
To avoid the occurrence or exacerbation (in the chronic form) of glomerulonephritis, you must adhere to some rules:
- it is necessary to treat viral and infectious diseases in a high-quality and timely manner;
- you need to be careful about vaccinations and monitor your health after this procedure;
- Quitting smoking and drinking alcohol will be mandatory;
- all physical activity should be gradual, overexertion should be avoided;
- you need to adhere to a special diet;
- It is best to avoid hypothermia;
- A mandatory measure will be routine examinations by a nephrologist and a urine test.
Glomerulonephritis is a very dangerous disease; in the early stages it responds well to treatment, but in advanced forms it can develop into kidney failure. Most often, children suffer from it, so you need to carefully monitor the child’s health.
Treatment is carried out using a large number of different medications, and the patient is also prescribed a diet and bed rest.
Treatment
Treatment of hematuric glomerulonephritis includes a whole range of measures.
The doctor prescribes a special diet that excludes highly salted, smoked and spicy foods. It is also advisable to limit the amount of animal protein in the diet.
To treat the disease, drugs of different groups are used. First of all, medications that improve blood circulation (dipyridamole, ticlopidine, heparin) are used. They prevent the formation of blood clots in the vessels and their sedimentation in the kidneys. Non-hormonal anti-inflammatory drugs are also used.
Immune suppressants are often used to prevent the destruction of the renal glomeruli by the body's immune system, these include steroid and cytotoxic drugs.
Together with this complex, antibiotics (selected by the attending physician), diuretics (hypothiazide, furosemide, uregit) and blood pressure lowering agents (captopril, enalapril, ramipril) are used.
Patients are recommended to rest in bed and reduce the overall load on the body. This is due to the fact that with high activity, the body’s metabolism increases, more fluid is released, and therefore the load on the kidneys is higher.
It is recommended to limit your liquid intake throughout the day. This also helps reduce the load on the kidneys.
Glomerulonephritis - diagnosis
First, the specialist carefully examines the patient and interviews him, establishing the presence of specific signs of the disease. To make a final diagnosis, tests are required - in case of glomerulonephritis, urine and blood (biochemistry) must be taken. Additionally, the following studies are prescribed:
- computed tomography or magnetic resonance imaging;
- X-ray;
- ultrasound diagnostics;
- kidney biopsy.
Glomerulonephritis - classification
The disease in question is differentiated by the nature of its course. Specialists diagnose subacute, acute and chronic glomerulonephritis. The first form of pathology is also called rapidly progressive or malignant; it is considered the most dangerous type of glomerular damage. It is rarely possible to stop such glomerulonephritis - the symptoms and treatment do not depend on each other, the condition worsens even with timely specific therapy. This type of disease ends in death in 80% of cases.
Acute glomerulonephritis is characterized by a rapid onset with severe symptoms. With early diagnosis and the correct medication approach, it can be completely cured without consequences. If the therapy was chosen incorrectly or the pathology progressed for too long, the disease becomes chronic. This type of disease has several variations.
Latent glomerulonephritis
Other names for the described type of damage to the renal glomeruli are hidden, urinary. With the development of the presented form of glomerulonephritis, the person feels well, no specific symptoms are observed. Only a urine test helps to identify the latent type of disease. It contains traces of protein compounds and blood components.
Glomerulonephritis – hematuric form
This variant of pathology is also called Berger's disease. At first, the state of health also remains satisfactory, but later hematuric glomerulonephritis provokes swelling of the soft tissues and increased blood pressure. The symptoms of the disease are nonspecific, so laboratory tests are required. It is necessary to examine the urine to diagnose such glomerulonephritis - symptoms and treatment are confirmed when blood components are detected in the biological fluid:
- red blood cells;
- protein fractions;
- platelets.
Glomerulonephritis – hypertensive form
One of the most common types of pathology, accounting for about 25% of all glomerular damage. A urine test will not help determine the specified chronic glomerulonephritis - the hypertensive form does not affect the composition of the biological fluid. Experts call the only pronounced symptom of the disease in question a steady increase in blood pressure. Hypertension is observed from the first days of progression of the pathology and continues until remission. Diastolic indicator (lower pressure) more than 95 mm Hg. Art.
Nephrotic glomerulonephritis
This variant of the disease occurs with pronounced clinical manifestations. There is both chronic and acute glomerulonephritis with nephrotic syndrome. It is characterized by severe swelling of the subcutaneous tissue (anasarca), limbs and soft tissues, and sometimes ascites (dropsy) is observed. It is easier for specialists to diagnose the described glomerulonephritis - symptoms and treatment are confirmed even on the basis of examination. Additional studies reveal a high concentration of protein in the urine, and a deficiency of albumin in the blood.
Mixed form of glomerulonephritis
This type of disease is a combination of hypertensive and nephrotic syndrome. Mixed glomerulonephritis occurs with signs characteristic of both forms of pathology. It progresses very quickly and can lead to severe complications, so it requires intensive therapy. The combined type of damage to the renal glomeruli always provokes changes in the composition of urine (proteinuria and hematuria).
Diagnostics
This disease is treated by a nephrologist who, through special diagnostic measures, is able to correctly determine the presence of glomerulonephritis and prescribe treatment appropriate to the form of the disease.
Oral interview with the patient
- it is determined whether kidney disease was present previously;
- is there a hereditary predisposition;
- whether you suffered an infectious or viral disease, and what period of time passed after recovery;
- when did the first signs of glomerulonephritis appear;
- how quickly the symptoms of the disease increase;
- whether the patient took any medications on his own and what the body’s reaction was.
External examination of the patient
- the presence and strength of manifestation of external symptoms (edema, etc.) is examined;
- doctor measures blood pressure.
Laboratory research
- urine - the amount of blood and protein is assessed;
- blood - a study is carried out to determine the number of leukocytes and the erythrocyte sedimentation rate;
- biochemical blood test - check for cholesterol and protein;
- immune blood test - taken when the doctor suspects an autoimmune development factor.
An ultrasound (ultrasound examination) is also required, which reveals an increase in the size of the kidneys.
Diagnostic methods
To make a diagnosis, the patient is interviewed and examined, and clinical, laboratory, and instrumental studies are prescribed:
- a general urinalysis, which allows you to detect the presence of red blood cells, protein, leukocytes, casts, fibrins. There is a change in the density of urine, a decrease in specific gravity;
- blood biochemistry to monitor ESR, the presence of leukocytosis, and check hemoglobin. With glomerulonephritis, cholesterol levels increase and protein concentration decreases;
- Kidney ultrasound, CT;
- immunological tests;
- X-ray of the pelvic organs;
- glomerular biopsy;
- fundus examination.
To make a diagnosis, the patient is interviewed and examined, and an examination is prescribed
To make a diagnosis, it is necessary to carry out differential diagnosis. This is necessary; some diseases have a similar clinical picture. These include urological diseases and oncology.
Treatment of rapidly progressive glomerulonephritis
This form of the process is considered the most unfavorable, and the effectiveness of the therapy is low. This condition is treated with high doses of glucocorticoid hormones in combination with cytostatics (pulse therapy is used, often repeated after 2-3 days).
Non-drug therapy methods such as plasmapheresis and hemodialysis are widely used, the main task of which is to maximally cleanse the patient’s body of toxic substances accumulated in it and remove immune complexes.
In some cases, organ transplantation is resorted to, but the mortality rate among such patients remains extremely high.