The inflammatory process in the kidneys is sometimes not bacterial in nature, but occurs due to stagnation of urine caused by obstruction of the elements for the production and excretion of urine into the bladder.
Later, against the background of stagnation, a bacterial infection joins and complicates the course of the pathology.
Chronic obstructive pyelonephritis is a common type of pathology; when the situation worsens, the disease becomes acute and requires immediate surgical care.
Differences
These two types of disease have characteristic differences.
| Sign | Obstructive pyelonephritis | Non-obstructive pyelonephritis |
| Disturbance of urine outflow | Eat | No |
| Formation of stones in the kidney | Often. Sometimes the disease itself occurs due to the formation of stones | Rarely. Possible in the case of a long latent course of the disease |
| Character of fever | A sharp increase in temperature to critical values. Poorly or not at all affected by antipyretics | Slow rise in temperature to critical values with episodes of decrease without taking antipyretics |
| Painful sensations | Renal colic, very severe sharp pain | Pressing or dull aching pain in the lumbar region, radiating to the abdomen |
| Formation of purulent infiltrates | A common complication of the disease | Almost never found |
| Etiology | The disease is secondary. The main reason lies either in congenital anomalies of the structure of the urinary tract, or in the long-term course of a chronic inflammatory process or urolithiasis | The disease is primary in nature and occurs when pathogenic microorganisms enter the tissue and mucous membranes of the kidneys. |
| Surgical intervention | Required frequently. Defects that interfere with the flow of urine and stones are eliminated surgically. Nephrostomy is sometimes necessary to preserve kidney function | No surgery required |
Both obstructive and non-obstructive pyelonephritis can occur with ascending (from the bladder and urethra) and descending (with the bloodstream) infection of kidney tissue by pathogens, but in the first type of disease it is characterized by severe congestion and destruction of kidney tissue.
Causes
The source of development of pyelonephritis is most often an infection caused by microorganisms. Reducing the lumen of the ureter leads to serious consequences. The main causes and principles of treatment of obstructive pyelonephritis are well known. Both men and women suffer from this disorder of the urinary system. There are a large number of reasons that provoke the development of pathology with obstruction of the urinary tract.
These include:
- System anomalies;
- Chronic urolithiasis;
- Exacerbation of diseases during pregnancy;
- Prostate adenoma or cancer in men;
- Diabetes mellitus type 1 or 2;
- Gout;
- Severe hypothermia of the kidneys;
- Long-term use of antibiotics;
- Protracted infectious diseases of other organ systems.
The exact causes of the obstructive process are determined by a nephrologist.
Stages
Stages of development of non-obstructive pyelonephritis:
- An acute infectious inflammatory process characterized by fever and pain.
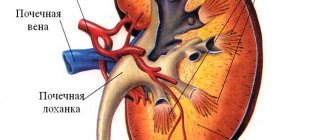
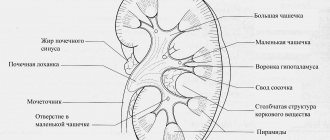
- A chronic process that can be asymptomatic. At this stage, changes occur in the pyelocaliceal system of the kidneys, scarring and sclerosis of tissues is possible, after which we will talk about obstructive pyelonephritis.
The stages of obstructive pyelonephritis are distinguished according to the degree of kidney damage:
- The inflammatory process occurs evenly throughout the kidney, and swelling is observed.
- Stagnant inflammatory foci aggravate the obstruction process, abscesses and carbuncles are formed, pathological changes occur in the collecting system, kidney shrinkage, and necrotic processes.
General signs of the disease
In the clinic of the classic course of acute pyelonephritis or exacerbation of its chronic form, three main symptomatic groups are distinguished: intoxication symptoms, pain and impaired renal functionality. In each case of acute pyelonephritis, all these groups of symptoms will be pronounced.
The intoxication process in pyelonephritis occurs due to poisoning of the body with various poisons released when the kidney tissue is infected. Symptoms of intoxication are expressed in headache, severe weakness, pain in joints and muscle tissue, lack of appetite, nausea and vomiting, thirst, dry mouth. A striking manifestation of intoxication is the occurrence of chills, followed by a sharp jump in body temperature to 39-40 degrees and profuse sweating. Intoxication manifestations belong to the category of general characteristics of the disease, in addition to which local manifestations also occur - pain and impaired renal function.
Content:
- General signs of the disease
- Manifestations of acute pyelonephritis
- Manifestations of chronic pyelonephritis
- Symptoms of the disease in pregnant women and newborns
- When to ask for help
Pain in acute pyelonephritis is usually localized in the lumbar region on the side of the affected kidney. Also, pain can radiate to the left or right hypochondrium, to the groin area and genitals. Soreness can be characterized by both constant presence and paroxysmal symptoms. Pain in the acute form of the disease is often sharp, but dull pain is also quite common. Increased pain is observed when coughing, at night, in case of movement of the leg on the side of which the kidney is damaged.
Pain in pyelonephritis can occur simultaneously with hyperthermia or a couple of days after the temperature has stabilized. In rare cases, the pain is replaced by a feeling of heaviness in the lower back. Mild pain syndrome is usually observed in patients with diabetes, patients with mental disorders or multiple sclerosis.
Cloudy urine is the main sign that kidney function is impaired. Secondary pyelonephritis is usually accompanied by concomitant pathology of a urological nature.
Due to the fact that in most cases of occurrence or exacerbation of pyelonephritis, the patient also experiences acute cystitis, the clinical picture of pyelonephritis can be supplemented by some nonspecific symptoms:
- pain and pain during urination;
- pollakiuria (frequent urination);
- hematuria (blood in the urine);
- nocturia (excessive and frequent urination at night).
In this case, the daily urine rate may become lower due to profuse sweating and fluid loss in the process.
Diagnostic methods
To make a correct diagnosis in both cases, the patient must undergo a clinical blood test and a general urine test, and undergo an ultrasound examination of the kidneys. If ultrasound and laboratory tests show the presence of an obstructive-congestive process, the patient may be prescribed a CT scan or contrast urography and cystography to determine the location of the disturbance in the outflow of urine and its cause.
Symptoms of the disease in pregnant women and newborns
More than 10% of all patients diagnosed with pyelonephritis are pregnant women. Primary pyelonephritis in this condition occurs for the first time precisely during an interesting situation, and secondary pyelonephritis worsens against the background of a growing uterus and its pressure on surrounding organs. As the uterus enlarges, it compresses the ureters and kidneys, and the movement of urine becomes difficult. Also, the symptoms of pyelonephritis in a pregnant woman are often caused by hormonal changes in the woman’s body.
An exacerbation of the disease in a pregnant woman’s body is usually manifested by high body temperature, increased heart rate, signs of intoxication, and pain when urinating. Painful sensations mainly occur at night. However, pyelonephritis in pregnant women is often asymptomatic and patients learn about it only from the results of tests.
Pyelonephritis in an infant is an inflammatory process in the kidneys of a child who feeds on mother's milk. The disease is provoked by pathogenic microbes. More often than boys, girls get sick; the disease usually manifests itself at the age of 4-5 months and is associated with the child’s transition to artificial feeding. Newborns suffer from pyelonephritis in only 1-3% of cases of all childhood diseases, and most often premature infants are susceptible to this pathology.
The symptoms of the disease in newborns and infants differ both among themselves and in comparison with a similar course of the disease in adults.
In infants, when pathology occurs, symptoms such as:
- heat;
- breast refusal (lack of appetite);
- frequent regurgitation, vomiting;
- unpleasant odor of urine, painful urination, expressed by crying, small volumes of urine;
- loose stools;
- high drowsiness;
- high weight loss.
Regarding newborns, it is worth noting that the symptoms of pyelonephritis in them are nonspecific.
Symptoms of neonatal illness include:
- critically low or critically high body temperature;
- severe jaundice;
- breast refusal;
- vomiting and repeated regurgitation;
- developmental delay.
A characteristic symptom for newborn boys is also hyponatremia and hyperkalemia, but sometimes these conditions are characteristic of pyelonephritis and for girls.
Blood tests demonstrate changes in pyelonephritis in a child, such as neutrophilia, anemia with protein deficiency and iron deficiency, accelerated ESR.
A characteristic sign of exacerbation of chronic or the occurrence of acute pyelonephritis in a child will be leukocyturia, detected in urine tests with active leukocytes in the sediment. In parallel, bacteriuria occurs. To clarify the etiology of the disease, children undergo urine culture, after which the flora and antibiotics to which it will be sensitive are determined. The first days of the disease are characterized by the occurrence of microhematuria and macrohematuria, moderate proteinuria.
The Zimnitsky test performed in a child often does not demonstrate pathology. It changes only with large-scale quantitative damage to the tubules. Clearance tests are carried out to understand the level of reduction in reabsorption and filtration. Tests are required to examine urea and creatinine levels in the blood.
Therapy
Treatment of non-obstructive pyelonephritis is carried out exclusively with medication. The patient is prescribed an antibiotic to which the pathogens that caused the inflammation are sensitive. To alleviate the condition during treatment and further prevention, the patient must follow a diet and drinking regime.
If an obstructive process is detected, antibiotic therapy is first prescribed to eliminate acute inflammation. Then the patient is prescribed uroseptics or bacteriostatic drugs to prevent relapse. The doctor determines the location and nature of the obstruction and then decides on the need for surgical intervention. For example, obstructive pyelonephritis that occurs during pregnancy simply requires medicinal support until delivery; kidney stones can be removed with hardware, but congenital anomalies require surgery to eliminate them.
Treatment of pathology
For obstructive pyelonephritis, medical care solves two problems:
- They remove the bacterial infection, which will help achieve remission of the pathology.
- Restore the normal flow of urine and eliminate those factors that interfered with the flow.
To solve the first problem, the patient takes antibacterial drugs. Doctors prescribe it for patients who have acute non-obstructive pyelonephritis, but it is also relevant for patients with obstruction.
During attacks, the patient is hospitalized, and drugs are prescribed intravenously or intramuscularly to quickly stop the infection.
Antibacterial drugs for obstructive pyelonephritis are second and third generation cephalosporins, the penicillin group, and fluoroquinolones.
The principle when choosing a drug to treat a patient is the sensitivity of the isolated pathogenic microflora to it as a result of urine analysis.
In addition to antibacterial drugs, painkillers, anti-inflammatory drugs, uroseptics, and medications are prescribed to normalize body temperature.
Lithotripsy
When eliminating the cause of obstruction, surgical intervention is often used. This is due to the fact that congenital or acquired pathologies of the urinary tract cannot be eliminated using conservative methods.
Therefore, the only correct decision for the patient is to eliminate the cause promptly. If stones are present, lithotripsy is performed, and if the ureter is narrowed, wall plasty is performed to remove the area with adhesions.
In case of a serious condition of the patient, a nephrostomy is applied for emergency removal of urine from the body, and catheterization of the bladder is performed. This will help eliminate swelling and relieve intrarenal pressure.
The prognosis is favorable if you go to the clinic early. If the pathology is eliminated as early as possible, then patients will not know what it is - renal colic, from which some patients even lose consciousness.
Prevention of obstructive pyelonephritis consists of timely treatment of urological pathologies and elimination of foci of infection in the body. If the first signs of pathology are detected, a doctor’s consultation is required.
Possible complications
The main danger with non-obstructive pyelonephritis is its transition to a chronic asymptomatic process with scarring of renal tissue or obstructive pyelonephritis.
Serious complications in the obstructive course of the disease are:
- Development of reflux nephropathy and secondary shrinkage of the kidney.
- The occurrence of focal purulent processes (abscess, carbuncle, tissue necrosis).
- Sepsis and bacteriotoxic shock.
- Development of acute renal failure and organ loss.
Kinds
Inflammatory kidney diseases are divided into several types. There are types of non-obstructive pyelonephritis. It can be acute or chronic, and may also be associated with a reflex. Non-obstructive chronic pyelonephritis associated with reflux affects the structures surrounding the organ.
There are two main forms of obstructive pyelonephritis: acute and chronic.
In the development of acute or chronic obstructive pyelonephritis, the degree of obstruction plays an important role:
- Relative obstruction. The outflow of urine is partially impaired;
- Absolute obstruction. The outflow has completely stopped;
- Increasing obstruction. Gradual, progressive development of the obstacle.
Common types of obstructions are related to the causes of their occurrence. These include:
- Stones;
- Tumors;
- Structural anomalies;
- BPH;
- Foreign bodies.
Forecast
The earlier the disease can be diagnosed, the better the prognosis. With non-obstructive pyelonephritis, complete cure can be achieved a maximum of two weeks after the start of therapy. Obstructive pyelonephritis requires more serious diagnosis and careful treatment of the main cause of the difficulty encountered in the functioning of the kidney. Thanks to modern minimally invasive technologies for operations on the kidneys and ureters, the patient will also soon make a full recovery.
By following doctors' recommendations, most patients manage to achieve complete remission.
Treatment of non-obstructive chronic pyelonephritis associated with reflux
It consists in eliminating or reducing the activity of the inflammatory process, which is possible only by restoring the outflow of urine and sanitizing the urinary tract.
Indications for hospitalization
In case of exacerbation of secondary pyelonephritis, emergency hospitalization to the urology department is indicated due to the potential need for surgical treatment. With exacerbation of primary non-obstructive pyelonephritis, antibacterial therapy can be started on an outpatient basis; Only patients with complications or when therapy is ineffective are hospitalized.
Planned hospitalization is indicated in unclear cases for inpatient examination and in cases of severe hypertension to conduct additional studies and select antihypertensive therapy.
In chronic pyelonephritis, it is necessary to maintain sufficient diuresis. The volume of liquid drunk should be 2000-2500 ml/day. It is recommended to use diuretics, fortified decoctions (fruit drinks) with antiseptic properties (cranberries, lingonberries, rose hips).
Outside of an exacerbation, sanatorium-resort treatment is possible in Essentuki, Zheleznovodsk, Pyatigorsk, Truskavets and at local resorts focused on the treatment of kidney diseases.
Patients with chronic pyelonephritis, complicated by arterial hypertension in the absence of polyuria and loss of electrolytes, are advised to limit the consumption of table salt (5-6 g/day) and liquid (up to 1000 ml/day).
Antibacterial therapy is of leading importance in the treatment of chronic pyelonephritis. This disease can be caused by many types of microorganisms, against which any of the currently available antibacterial drugs can be used. If possible, you should avoid prescribing:
- expensive medicines;
Treatment with antibacterial drugs for chronic pyelonephritis should be carried out after performing a bacteriological analysis of urine with identification of the pathogen and determination of its sensitivity to antibiotics. Difficulties arise in the empirical selection of drugs. However, this type of therapy for this disease is rarely used, mainly during exacerbation of the disease.
Antihypertensive therapy for chronic pyelonephritis is carried out according to the usual regimens. However, it should be noted that arterial hypertension in most cases is associated with an increase in blood renin levels, and therefore ACE inhibitors are considered basic drugs. In case of intolerance (mainly due to cough), angiotensin II receptor antagonists will be the drugs of choice. Due to frequent nephrosclerosis (possibly bilateral), drug doses for such patients must be selected taking into account the Rehberg test.
In chronic pyelonephritis, surgical treatment is aimed mainly at restoring urine passage. With an exacerbation of this disease, which has passed into the purulent phase, kidney decapsulation and nephrostomy are indicated.
ICD-10 category: N11.0
Treatment at home
How to treat the disease at home? To do this, you can use traditional medicine recipes that are based on natural ingredients. Most often, medicinal herbs are used to prepare medicines.
Oats
You will need 2 tbsp. l. dried oat grass and 0.5 liters of water. Place the ingredients on low heat and simmer for 30 minutes. Then strain the prepared broth and take 1 glass 2 times a day.
Corn silk
You should take 1 tbsp. l. corn silk, pour 1 cup of boiling water, put on fire to boil for about 5 minutes. After the time has passed, leave for 30 minutes, then strain the broth and consume 2 tbsp. l. 5 times a day.
Yarrow
For cooking you need 2 tbsp. l. yarrow herb, which should be crushed. Pour 1 cup of boiling water and leave for 1 hour. Take 50 ml of the resulting decoction 3 times a day.
Linen
To prepare the medicine you will need 1 tsp of flax seeds. Pour 1 glass of hot water. Place on the fire and boil for 5 minutes. Then leave for 1 hour. After time, strain the broth and take 50 ml 4 times a day.
Important to remember! Before using a certain alternative medicine, you should consult a specialist!
Content
Definition and general information [edit]
Pyelonephritis is a nonspecific infectious and inflammatory process that occurs predominantly in the tubulointerstitial zone of the kidney.
Chronic pyelonephritis is the most common kidney disease. The incidence is 18 cases per 1000 people. Women get sick 2-5 times more often than men. Prevalence, based on cause of death data, ranges from 8 to 20%.
— primary chronic pyelonephritis developing in an intact kidney (without developmental anomalies and diagnosed disorders of the urodynamics of the UMP);
- secondary chronic pyelonephritis, which occurs against the background of diseases that impair the passage of urine.
According to localization, the process can be one-sided or two-sided.
There are phases of chronic pyelonephritis:
- remission or clinical recovery
Etiology and pathogenesis[edit]
Clinical manifestations[edit]
During the active phase of chronic pyelonephritis, the patient complains of dull pain in the lumbar region. Dysuria is uncharacteristic, although it may be present in the form of frequent painful urination of varying severity. Upon detailed questioning, the patient may bring up a lot of nonspecific complaints:
- for episodes of chilling and low-grade fever;
- discomfort in the lumbar region;
- decreased performance, etc.
With the development of chronic renal failure (chronic renal failure) or tubular dysfunction, complaints are often determined by these symptoms. During the latent phase of the disease, there may be no complaints at all; the diagnosis is confirmed by laboratory tests. The remission stage is based on anamnestic data (for at least 5 years); complaints and laboratory changes are not detected.
Non-obstructive chronic pyelonephritis associated with reflux: Diagnosis[edit]
When interviewing, it is necessary to pay attention to characteristic episodes of pain in the lumbar region, accompanied by fever, the effectiveness of antibacterial therapy, as well as symptoms of chronic renal failure in the anamnesis.
It is important to find out whether the patient has:
— foci of chronic infection;
- anomalies of the kidneys and urinary tract;
- diseases that can cause disruption of urine passage;
— carbohydrate metabolism disorders and the degree of their correction;
— immunodeficiency resulting from any disease or induced by drugs.
Information about previous inflammatory diseases of infectious etiology, the use of antibacterial drugs and their effectiveness is important.
For pregnant women, it is necessary to find out the duration of pregnancy and the characteristics of its course.
When examining a patient with chronic pyelonephritis, pay attention to:
- pain on palpation in the kidney area;
- positive Pasternatsky sign on the affected side;
It is necessary to measure blood pressure and body temperature. A particular tendency to arterial hypertension is detected in patients with secondary chronic pyelonephritis against the background of kidney abnormalities.
Laboratory and instrumental research methods
— Laboratory tests reveal leukocyturia (in most cases neutrophilic) and bacteriuria. Slight proteinuria (up to 1 g/day), microhematuria, hyposthenuria, and alkaline urine reaction are possible.
— Ultrasound allows you to diagnose:
a) swelling of the parenchyma during exacerbation;
b) reduction in the size of the kidney, its deformation, increased echogenicity of the parenchyma (signs of nephrosclerosis) with long-term pyelonephritis without exacerbation.
The expansion of the pyelocaliceal system indicates a violation of the passage of urine. In addition, a Doppler study allows you to clarify the degree of blood flow disturbance.
Further examination to clarify the diagnosis of chronic pyelonephritis in the active stage is individual for each patient.
— Bacteriological urine analysis is indicated for all patients to identify the causative agent of the disease and prescribe adequate antibacterial therapy. When quantitatively assessing the degree of bacteriuria, a level of 10 5 CFU/ml is considered significant. In unusual cases (with polyuria or immunosuppression), a lower degree of bacteriuria may be clinically significant.
— In a general blood test, attention is paid to hematological signs of inflammation:
a) neutrophilic leukocytosis with a shift of the formula to the left;
b) increased ESR.
— A biochemical blood test allows you to clarify the functional state of the liver and kidneys.
— The Rehberg test is performed with minimal suspicion of chronic renal failure (CKD).
— Analysis for daily proteinuria and qualitative studies of excreted proteins are performed in controversial cases for differential diagnosis with primary glomerular kidney lesions.
— According to excretory urography, specific radiological signs of pyelonephritis are revealed. However, the main purpose of its implementation is to clarify the condition of the urinary tract and diagnose urinary passage disorders.
— Radioisotope research methods are carried out to resolve the issue of the symmetry of nephropathy and assess the functional state of the kidney.
— Angiography, CT and MRI are indicated for diagnosing diseases that provoke the development of pyelonephritis:
a) urolithiasis;
b) tumors and developmental anomalies of the kidneys and urinary tract.
— Kidney biopsy is used for differential diagnosis with other diffuse lesions of renal tissue, especially when deciding on the need for immunosuppressive therapy.
— In case of severe arterial hypertension and problems in selecting antihypertensive therapy, it is important to perform a blood test for the content of renin, angiotensin and aldosterone.
Differential diagnosis[edit]
Chronic tubulointerstitial nephritis sometimes develops as part of systemic diseases - sarcoidosis, gout, less commonly others.
The diagnosis of chronic glomerulonephritis is beyond doubt if the patient has nephrotic syndrome or severe glomerular erythrocyturia. However, differential diagnosis becomes more difficult when persistent arterial hypertension (especially at a young age) is combined with changes in urine tests characteristic of chronic urinary tract or genital infections.
During exacerbation of chronic pyelonephritis, differential diagnosis must be carried out with a number of acute diseases of the abdominal cavity and retroperitoneal space.
Non-obstructive chronic pyelonephritis associated with reflux: Treatment[edit]
It consists in eliminating or reducing the activity of the inflammatory process, which is possible only by restoring the outflow of urine and sanitizing the urinary tract.
Indications for hospitalization
In case of exacerbation of secondary pyelonephritis, emergency hospitalization to the urology department is indicated due to the potential need for surgical treatment. With exacerbation of primary non-obstructive pyelonephritis, antibacterial therapy can be started on an outpatient basis; Only patients with complications or when therapy is ineffective are hospitalized.
Planned hospitalization is indicated in unclear cases for inpatient examination and in cases of severe hypertension to conduct additional studies and select antihypertensive therapy.
In chronic pyelonephritis, it is necessary to maintain sufficient diuresis. The volume of liquid drunk should be 2000-2500 ml/day. It is recommended to use diuretics, fortified decoctions (fruit drinks) with antiseptic properties (cranberries, lingonberries, rose hips).
Outside of an exacerbation, sanatorium-resort treatment is possible in Essentuki, Zheleznovodsk, Pyatigorsk, Truskavets and at local resorts focused on the treatment of kidney diseases.
Patients with chronic pyelonephritis, complicated by arterial hypertension in the absence of polyuria and loss of electrolytes, are advised to limit the consumption of table salt (5-6 g/day) and liquid (up to 1000 ml/day).
Antibacterial therapy is of leading importance in the treatment of chronic pyelonephritis. This disease can be caused by many types of microorganisms, against which any of the currently available antibacterial drugs can be used. If possible, you should avoid prescribing:
- expensive medicines;
Treatment with antibacterial drugs for chronic pyelonephritis should be carried out after performing a bacteriological analysis of urine with identification of the pathogen and determination of its sensitivity to antibiotics. Difficulties arise in the empirical selection of drugs. However, this type of therapy for this disease is rarely used, mainly during exacerbation of the disease (see acute pyelonephritis).
Antihypertensive therapy for chronic pyelonephritis is carried out according to the usual regimens. However, it should be noted that arterial hypertension in most cases is associated with an increase in blood renin levels, and therefore ACE inhibitors are considered basic drugs. In case of intolerance (mainly due to cough), angiotensin II receptor antagonists will be the drugs of choice. Due to frequent nephrosclerosis (possibly bilateral), drug doses for such patients must be selected taking into account the Rehberg test.
In chronic pyelonephritis, surgical treatment is aimed mainly at restoring urine passage. With an exacerbation of this disease, which has passed into the purulent phase, kidney decapsulation and nephrostomy are indicated.
Prevention[edit]
General prevention of this disease is:
- to exclude hypothermia;
— treatment of focal infectious processes;
— correction of carbohydrate metabolism disorders.
Prevention of secondary pyelonephritis consists of timely restoration of urinary passage disorders.
Other [edit]
The prognosis for life with chronic pyelonephritis is favorable. Adequate antibacterial therapy and timely surgical interventions make it possible to maintain kidney function for a long time.
Depending on the severity of the pathology, pyelonephritis can be obstructive and non-obstructive. Each of them has its own ways of manifestation in the body, treatment methods and classification. The disease can be chronic, acute, as well as bilateral and unilateral.
Obstructive or non-obstructive pyelonephritis gets its name due to the presence or absence of obstruction. They can be different, for example, urolithiasis, tumor, prostate adenoma or abnormal structures of the genitourinary system.
Disease during pregnancy
How to cure pyelonephritis during pregnancy? Most often, chronic pyelonephritis develops in a woman long before pregnancy. This condition is not the cause of its appearance, but contributes to its active development. What to do if exacerbations occur during pregnancy? Expectant mothers are more susceptible to pyelonephritis than others due to a weakened immune system.
Since many medications are contraindicated during pregnancy, the doctor should prescribe the safest possible medications. The most suitable in this situation are Monural and Amoxiclav.
Symptoms in pregnant women can be treated with medication. That is, if you have an elevated body temperature, you should take an antipyretic drug, after consulting with a specialist.