Pyelonephritis is an inflammatory pathology of infectious etiology with a predominant lesion of the renal collecting system. The chronic form of pyelonephritis is characterized by alternating remissions and exacerbations. In the first case, during the period of calm, the patient feels quite well. Exacerbation of pyelonephritis is manifested by symptoms of an infectious-inflammatory process. The danger of a long-term chronic course of the disease is gradual tissue necrosis and impaired renal function, resulting in severe consequences, so timely therapy and supervision by a specialist is necessary.
Causes
Like most chronic illnesses, pyelonephritis is unpleasant and dangerous because periods of calm alternate with moments of exacerbation. And at first glance it seems that the exacerbation of pyelonephritis appeared out of nowhere. What can provoke an exacerbation of kidney disease? Here are the main reasons:
- allergies with intoxication of the body;
- pregnancy;
- recent onset diabetes mellitus;
- disturbance of urine outflow;
- weakened immunity;
- sexual infections;
- vesicoureteral reflux;
- stress;
- seasonal colds and infections.
Also, do not discount the usual hypothermia, intoxication with drugs and alcohol. The movement of stones and insufficiently frequent urination, as well as all kinds of urological manipulations, may also be to blame.
Don't take off your clothes right away in the spring. Warming in the spring is temporary, which is why so many colds develop during this period.
Stages of exacerbation of chronic pyelonephritis
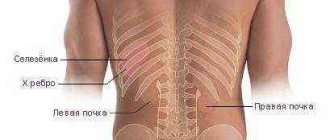
The disease is characterized by the manifestation of 2 stages: primary and secondary. In the first stage, which is also called uncomplicated, the disease begins due to an infection spread through the bloodstream. The secondary stage is characterized by urinary tract disorders. As a result, the pathways narrow, stones and tumors appear, making it difficult to remove urine from the body, causing it to stagnate. Moreover, the disease is more common among women in young years, and among men in old age.
Symptoms
Most often, exacerbation of pyelonephritis makes itself felt by weakness and lethargy, plus too high a temperature. There is also lower back pain and discomfort. If the exacerbation is too active, the following symptoms may occur:
- increased urination;
- swelling of the hands and face;
- changes in the composition of urine (determined only in the laboratory);
- swelling of the whole body (with severe inflammation);
- increase in pressure;
- heartache;
- abdominal pain (especially in the lower part);
- symptoms of renal colic;
- chills;
- headache;
- thirst and dry mouth;
- pale skin;
- dyspnea;
- accumulation of fluid in the abdomen (with severe exacerbation);
- lack of coordination;
- vision problems.
Chronic pyelonephritis can cause kidney failure or cystitis.
Sources of pyelonephritis
The main routes for the passage of pathogenic bacteria into the kidneys are:
- Urethra – bladder – kidneys. According to numerous studies, this spread of bacteria is most common in women. This can be explained by a shorter urethra than in men, as well as by the peculiarities of the anatomy of the genital organs, which creates excellent conditions for the rapid spread of bacteria throughout the groin and vagina, subsequently moving to the area of the bladder and kidneys. If we talk about the types of pathogens of this disease, it is worth highlighting kidney damage by E. coli, staphylococcus, Klebsiella, enterococcus, and pathogenic fungi.
- Instrumental manipulation is a less common route of infection. This may include the use of catheters. The most common pathogenic microorganisms in such cases are Pseudomonas aeruginosa or Klebsiella.
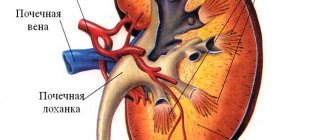
- Another reason for the development of pyelonephritis is the impaired outflow of urine in the ureters and bladder, which will be followed by its partial reflux back into the renal pelvis. If therapy is not started in a timely manner, stagnation of inseparable fluid occurs, as well as the growth of pathogenic bacteria that enter the kidneys, thereby causing an inflammatory process.
- Another cause of pyelonephritis can be called the entry of pathogenic microorganisms into the kidneys from another internal organ through the general blood flow through blood vessels. The risk of bacteria entering increases significantly if the ureters are blocked by stones or if the prostate is enlarged (in men).
It is worth highlighting factors predisposing to the development of the disease:
- the presence of congenital anomalies in the structure of organs such as the kidneys and bladder;
- acquired immunodeficiency syndrome occurring in the body;
- development of diabetes mellitus in the body;
- age factor (the older the person, the higher the percentage of risk of developing pathology);
- existing pathologies of the prostate gland, during the development of which it increases in size;
- development of kidney stones;
- spinal cord injury.
Diagnostics
If the exacerbation is not too serious, then hospitalization is not too necessary. But you definitely need to call a doctor. You will also need tests that will tell you how to cope with an exacerbation. The following tests and examinations are most needed:
- laboratory urine analysis;
- sterility analysis;
- for sensitivity to antibiotics;
- Ultrasound of the kidneys;
- radioisotope scintigraphy;
- CT.
Relapse of pyelonephritis - treatment and first aid
In case of severe symptoms, it is recommended to call a medical team
, followed by hospitalization and treatment in a hospital. If the symptoms described above begin to appear at home, the patient must be put to bed and drink should be limited. You can independently check the likelihood of an exacerbation of pyelonephritis using a special test. The patient is placed on his back and asked to bring the leg bent at the knee as far as possible to the chest. If the pain intensifies significantly when you inhale, there is every reason to believe that there is an inflammatory process in the kidneys. If chronic pyelonephritis was diagnosed earlier, there is a very high probability that a relapse of the disease has begun.
For severe symptoms (high blood pressure, intense pain, significant problems with urination, fever), it is recommended to call a medical team, followed by hospitalization and treatment in a hospital. Therapy for exacerbation of inflammation of the mucous membrane of the pelvis involves, first of all, an etiological drug effect in combination with the removal of concomitant symptoms and restorative herbal medicine.
Along with diagnostic measures, urine sediment is taken for bacteriological culture, based on the results of which antibacterial treatment is prescribed. Antimicrobial drugs are used: antibiotics (penicillins, macrolides, cephalosporins), sulfonamides (Biseptol, Trimetaprim), uroseptics (derivatives of nitrofuran, hydroxyquinoline and nalixidic acid). Antibacterial therapy is prescribed for a course of at least 10 days and is not interrupted even if the general condition is normalized and symptoms disappear.
Antispasmodic drugs (No-Shpa, Papaverine, Platyfillin) are used as symptomatic treatment to relieve smooth muscle spasms in combination with non-narcotic analgesics (NSAIDs). To reduce blood pressure, angiotensin-converting enzyme inhibitors (Capoten, Captopril) are used.
For herbal medicine, natural pharmaceutical preparations and decoctions of medicinal herbs are used. The first include such pharmacological agents as Canephron-N and Fitonephrol. Medicinal plants used for relapses of pyelonephritis include chamomile, marshmallow, nettle, bearberry, lingonberry, which have a pronounced anti-inflammatory effect. Also used are decoctions of birch leaves, corn silk, cornflower flowers, and juniper, which have a mild diuretic effect.
Traditional treatment
The basis of treatment is antibacterial therapy. It is also necessary to remove obstacles to the outflow of urine. This means that you need to remove the stones and eliminate the ureteral stricture.
If you have chronic pyelonephritis, you need to learn on your own to determine whether an antibiotic is helping you. To do this, we monitor whether the temperature dropped after a couple of days and whether the tests improved on the third or fourth day. Antibiotics for any ailment are a very individual matter, but for pyelonephritis they are most often prescribed:
- aminopenicillins (including amoxicillin and amosin);
- protected penicillins (for example, ampicillin/sulbactam or clavulanate/amoxicillin);
- cephalosporins (ceftibuten, cefixime);
- aminoglycosides, such as amikacin or gentamicin;
- fluoroquinolones (moxifloxacin, sparfloxacin);
- sulfonamides (actually sulfanilamide, sulfadizine);
- nitrofurans (macmiror);
- non-fluorinated quinolones (ofloxacin, norfloxacin);
- 8-hydroxyquinoline derivatives (quinosol and nitroxoline);
- uroantiseptics of plant origin;
- You will also need immunomodulators, IVs to get rid of toxins in the kidneys, diuretics and vitamins. Instead of IVs, today plasmaphoresis is more often prescribed, as well as drugs to improve renal circulation and thin the blood.
The main requirements for antibiotics for pyelonephritis are their low nephrotoxicity, a wide range of activities, good bactericidal properties and the ability to be excreted in high concentrations in the urine.
Features of pyelonephritis in pregnant women
Approximately one in 20 pregnant women (4%) experiences signs of the disease.
The problem can develop in the middle of the second to early third trimester, which is caused by increasing pressure of the uterus on the ureters and kidneys. For this reason, urine flows more slowly, stagnating in the kidneys. The number of pathogenic bacteria increases, and if you add sluggish or acute cystitis to this, the likelihood of the onset of pyelonephritis increases significantly. When the first alarming symptoms appear, you need to see your doctor as soon as possible, since complications in the form of anemia, renal failure, sepsis, premature birth, gestosis and eclampsia (the latter conditions are dangerous for the life of a woman and child) cannot be excluded. But with adequate therapy started on time, troubles can be avoided (self-medication is not allowed).
Traditional treatment
In case of exacerbation of pyelonephritis, the following plants will be needed: horsetail, birch leaves, juniper (fruits), lingonberry leaves, bearberry, cranberry, dandelion, kidney tea, St. John's wort. The ideal option is to combine traditional medicine with herbal therapy:
- Calamus, bearberry and flax are mixed in equal parts, poured with boiling water (for 50 grams of collection you need 0.5 - 0.6 liters of water). Boil for 5 - 7 minutes, cool, drink 0.5 - 1 glass 2 - 3 times a day.
- Rose hips and nettle leaves are effective in combating stones. They are brewed in a tablespoon per 1/4 liter of boiling water and drunk as teas.
- Melt the butter, add propolis, stir. Eat the gruel every day three times, 2 tsp.
Exacerbation of the disease
Patients with indolent pyelonephritis undergo complex therapy, which has several goals:
- destruction of infection in the kidneys;
- increasing general immunity;
- normalization of urine outflow from the urinary ducts.
During drug therapy, patients adhere to a diet, and when the condition improves, they undergo hardware treatment - electrophoresis, SMT therapy.
Regime and diet
To reduce the load on the urinary system, they resort to diet therapy. Nephrologists recommend sticking to a diet with a predominance of kefir, low-fat cottage cheese, and homemade yogurt. In case of relapses of chronic inflammation, exclude:
- spices;
- canned fish;
- any spices;
- alcohol;
- meat and mushroom broths;
- strong coffee;
- Black tea;
- spicy dishes;
- carbonated drinks.
The basis of the diet should be boiled vegetables, dietary meat, dairy products, and fresh fruits. To speed up the removal of bacteria from the kidneys, drink up to 2 liters of free liquid per day. Good for drinking:
- bearberry decoction;
- kidney tea;
- fruit drinks;
- vegetable juices.
People with hypertension limit their daily salt intake to 3 g. For chronic inflammation of the kidney parenchyma, melons - watermelons, melons - are useful.
To avoid recurrences of pyelonephritis, you need:
- take daily walks in the fresh air;
- avoid overheating and hypothermia;
- treat foci of chronic infection.
If you have pyelonephritis in young children, you should temporarily skip kindergarten.
First of all, treatment for chronic pyelonephritis is aimed at destroying the bacterial flora. The doctor takes into account the sensitivity of microorganisms to antibiotics and prescribes:
- protected penicillins – Augmentin, Abiclave, Amoxil-K;
- cephalosporins – Cefepime, Kefpim, Maxicef;
- aminoglycosides – Amikacin, Flexelit, Amicil;
- fluoroquinolones – Ofloxacin, Zoflox, Floxal;
- nitrofurans - Furazolidone, Solafur, Nitrofurantoin.
After a course of antibiotics, uroseptics are prescribed - Urodixin, Nevigramon, Negram. They destroy bacteria in the urinary tract and prevent the formation of microbial flora in the ureter, bladder and urethral canal.
To relieve symptoms of chronic inflammation in the kidney, the following are used:
- non-narcotic analgesics (Amidopyrine, Ibuklin) - reduce lower back pain, lower body temperature;
- antioxidants (Lipin, Epadol) – reduce the severity of signs of intoxication with nitrogenous substances;
- antihistamines (Zyrtec, Chloropyramine) – remove swelling of the eyelids and limbs, eliminate other allergic manifestations;
- antiplatelet agents (Ticlopidine, Dibazol) - thin the blood, improving its microcirculation in the affected organs.
For chronic inflammation in the organs of the genitourinary system, immunostimulating drugs are prescribed - Echinacea Hexal, Ruzam, Imunofan, Bifidumbacterin.
Anti-relapse therapy for pyelonephritis takes at least 3 months. During antibiotic treatment, patients should be under the supervision of a nephrologist.
Surgery is a radical method of treating pyelonephritis, which is used only when indicated:
- low effectiveness of drug therapy;
- frequent relapses of chronic disease;
- purulent complications;
- hydronephrosis;
- blockage of the urinary tract with stones.
For stones, open or laparoscopic surgery is performed to remove stones. Depending on the location of the stones, the surgeon dissects the pelvis (pyelolithotomy) or the kidney tissue (nephrolithotomy).
In case of complete damage to the parenchyma and its replacement with scar tissue, nephrectomy (kidney removal) is resorted to. During the operation, the doctor removes the affected organ only if the person has a healthy second kidney.
Traditional recipes for the treatment of pyelonephritis are used only with the permission of the attending physician. Decoctions with:
- bearberry;
- lingonberries;
- juniper;
- parsley;
- cornflower;
- celery;
- calendula;
- currants;
- sage.
For chronic inflammation of the kidney tissue, the following are used:
- Bearberry infusion. 10 g of dry herb is poured into 200 ml of boiling water and left overnight. The filtered infusion is drunk throughout the day.
- Herbal collection. Mix lingonberries, cornflower, calendula and sage in equal quantities. 2 tbsp. l. the collection is boiled in ½ liter of water for 4-5 minutes. Drink 100 ml of decoction three times a day.
Taking diuretic decoctions is contraindicated in patients with severe renal failure.
For chronic diseases of the genitourinary system, treatment in regions with a warm climate is recommended. To restore kidney function they resort to:
- mud therapy;
- mineral baths;
- reflexology.
Physiotherapeutic procedures stimulate the outflow of urine from the kidneys and prevent stone formation. Sanatorium-resort treatment should be completed twice a year only during periods of remission.
Acute pyelonephritis occurs due to an ascending urinary tract infection: if pathogens enter the bladder through the urethra, they are able to migrate from there to the ureter and renal pelvis, and then cause inflammation. Patients experience urinary problems: if urine cannot flow normally (due to a urinary stone or foreign body), pathogens rise faster into the organs. Most of them are bacteria: most often E. coli.
An attack of pyelonephritis can cause a variety of symptoms: from delirium due to fever to mild pain.
It is important to know! Chronic pyelonephritis can be asymptomatic for a long time. However, over time, kidney function becomes impaired, causing kidney failure in extreme cases.
Possible symptoms indicating exacerbation of chronic pyelonephritis:
- fatigue;
- back pain;
- gastrointestinal complaints;
- weight loss;
- anemia (anemia);
- high blood pressure.
A physical examination, blood and urine tests are required to confirm the diagnosis. Imaging methods are also used - ultrasound (sonography) and X-ray examinations. To identify the causative agent of the disease and determine appropriate therapy, the doctor conducts a bacteriological analysis.
Pyelonephritis must be treated with antibiotics for approximately 7 days. If the fever does not go away, you need to extend the treatment. During the acute stage, it is recommended to maintain bed rest and drink as much as possible to remove pathogens. Antipyretic and anti-inflammatory drugs help avoid common symptoms.
Causes of exacerbation
In many cases, pyelonephritis is the result of an ascending infection: if pathogens enter the bladder through the urethra, they can migrate from there to the renal pelvis. Bacteria are common causative agents of inflammatory diseases of the upper urinary tract.
Unlike glomerulonephritis, pyelonephritis affects only the connective tissue of the kidneys. Chronic forms also have adverse effects on other organ systems.
Pyelonephritis is one of the most common kidney disorders. Women are approximately twice as likely to develop the disease. A shorter urethra encourages bacteria to enter the bladder and from there rise through the ureters into the renal pelvis. However, the incidence increases with age in men.
Urinary problems are a concomitant symptom of pyelonephritis. A common cause of urinary obstruction is urinary stone. If urine cannot be disposed of properly, the result can be what are called ascending infections.
Acute nephritis and pyelitis occur in phases in which the body's immune system is weakened. Possible causes of this include treatment with certain drugs—immunosuppressants—and tumors. Beneficial for chronic pyelonephritis is kidney damage caused by the abuse of nephrotoxic analgesics. People with diabetes have an increased risk of developing pathology.
It is important to know! Most often, pyelonephritis is caused by invasion of Escherichia Coli, staphylococci, enterococci, Proteus or Kliebsilla. If the infection occurs during a hospital stay (for example, through a catheter), many other and sometimes very different pathogens are usually involved.
A typical sign of acute pyelonephritis is sudden severe malaise. Sometimes fever appears and the heart rate increases.
Other symptoms of exacerbation of pyelonephritis:
- loss of appetite;
- unexplained weakness;
- hyperkinesis;
- local spasm.
However, in some cases, exacerbation of chronic pyelonephritis may also begin slowly and be accompanied by atypical symptoms - cephalalgia, weakness and sudden weight loss. In acute pyelonephritis, gastrointestinal signs are possible - dyspepsia, abdominalgia or gastrointestinal obstruction. Renal function is not limited in the acute form of the disease. The latent form can be asymptomatic for years.
Dangerous complications
Kidney infection can lead to various complications: from initially simple purulent pyelonephritis, multiple renal abscesses are formed. In this case, pathogens are able to penetrate the bloodstream and cause urosepsis - blood poisoning. Kidney inflammation can lead to blood in the urine (hematuria).
Acute pyelonephritis often causes serious complications, especially if the infection appeared in the hospital. With diabetes, narrowing of the urinary tract and during pregnancy, the risk of developing acute chronic pyelonephritis increases. In women, pelvic inflammation often goes unnoticed (50% of cases are not diagnosed). Infection can lead to miscarriage and premature birth.
It is important to know! If pyelonephritis affects kidney function, it can lead to complications such as high blood pressure and electrolyte imbalances. Progressive kidney failure caused by pyelonephritis occurs in only about 1 in 1000 people.
Prevention
Important:
- Maintain a drinking regime and regularly include some of the herbs mentioned below in your daily fluid intake.
- While on vacation, it would be good to undergo treatment at a sanatorium that specializes in kidney problems.
- Among herbal preventive remedies, for example, Canephron N is popular.
- To fight bacteria, you should eat garlic and drink chamomile. Other plants needed for prevention are parsley and lingonberries. Any herbal mixtures or individual herbs can be drunk as infusions or decoctions in a water bath three times a day.
You can also watch a video about the treatment of exacerbation of chronic pyelonephritis.
Classification by stages
Unilateral (left- or right-sided) pyelonephritis occurs mainly with acute inflammation of the renal structures. When inflammation becomes chronic, both kidneys are affected in 93% of cases. But the severity of inflammatory reactions in them can be different.
Slow inflammation is accompanied by gradual replacement of parenchymal tissue with scar tissue. This leads to an irreversible decline in kidney function.
In its course, pyelonephritis goes through 3 stages:
- First. The mucous membrane of the renal tubules is depleted, losing vitality. In the loose connective (interstitial) tissue that forms the basis of the organ, compactions with admixtures of blood and lymph appear.
- Second. Sclerotic changes begin in the parenchyma and tubules, that is, they are replaced by dense scar tissue. As a result, the nephrons in which fluid is filtered become depleted and die. At the same time, desolation and fusion of the glomeruli and a narrowing of the diameter of blood vessels occur.
- Third. The affected organ shrinks and its surface becomes lumpy. The parenchyma is replaced by connective tissue. Therefore, the kidney stops functioning.
According to the activity of inflammatory reactions, three phases of chronic pyelonephritis are distinguished:
- active;
- hidden (latent);
- remission.
With timely antibiotic therapy, active inflammation is replaced by a phase of clinical recovery.
Chronic pyelonephritis is characterized by three stages of inflammation in the kidney tissue. At stage I, leukocyte infiltration of the interstitial tissue of the medulla and atrophy of the collecting ducts are detected; the renal glomeruli are intact. At stage II of the inflammatory process, cicatricial sclerotic damage to the interstitium and tubules is noted, which is accompanied by the death of the terminal sections of nephrons and compression of the tubules. At the same time, hyalinization and desolation of the glomeruli, narrowing or obliteration of blood vessels develop. In the final stage III, the kidney tissue is replaced by scar tissue, the kidney is reduced in size and looks wrinkled with a bumpy surface.
Based on the activity of inflammatory processes in the renal tissue in the development of chronic pyelonephritis, the phases of active inflammation, latent inflammation, and remission (clinical recovery) are distinguished. Under the influence of treatment or in its absence, the active phase is replaced by a latent phase, which, in turn, can go into remission or again into active inflammation. The remission phase is characterized by the absence of clinical signs of the disease and changes in urine tests. According to clinical development, erased (latent), recurrent, hypertensive, anemic, azotemic forms of pathology are distinguished.
Chronic pyelonephritis in the acute stage is characterized by certain symptoms. However, it is worth considering this disease as a whole. So, there are 4 stages of chronic pyelonephritis. They are characterized by the following changes in the body:
- At the first stage, the glomeruli of the kidneys are not affected by the infection, they are not involved in the pathological process. But atrophy of the collecting ducts is actively occurring. This process occurs evenly.
- At the second stage, the still insignificant desolation and hyalinization of some glomeruli of the organ begins. The vessels narrow significantly, which leads to an increase in pressure in them. Scar-sclerotic changes are steadily increasing in the tubules.
- Further, in the stage of exacerbation of chronic pyelonephritis, the death of most glomeruli occurs. During the third stage of the disease, tubular atrophy is observed, and the connective tissue grows.
- At the last stage, most of the glomeruli die. Because of this, the organ loses a lot in size. Healthy functional tissues are replaced by scars. The kidney becomes unable to perform its assigned functions. This process becomes irreversible.
For this reason, the sooner proper, comprehensive treatment is started, the greater the patient’s chances of recovery. Self-medication can be extremely dangerous. Therefore, if characteristic symptoms appear, you should consult a doctor as soon as possible.