Latent - meaning of the word
The word latent from Latin latens(-entis) is translated as “implicit”, “hidden”. This term is used in medicine to define the implicit smoothed type of course of a viral or bacterial infection. Or when the infection manifests itself, but the virion cannot be found using a laboratory test for some reason.
Many diseases can occur hidden and unnoticed, for example, viral infections such as herpes, pyelonephritis, TORCH infections, hepatitis virus and others.
Latent flow - what does it mean?
Once an infection enters the body, it does not always manifest itself openly. Sometimes the virus behaves hidden, it lives quietly in a cell. After division, it passes into daughter plants, but leaves no toxins and does not cause any signs of disease at all. In medicine, this phenomenon is called the latent course of the disease.
The virus can manifest itself under certain conditions, for example, during reinfection. Then a person suddenly discovers that he is sick, although there were no prerequisites for this before.
This is not good for the patient, but not entirely bad either. You just need to be aware that this infection is present in the body, and be on guard. Because when the immune system is weakened, the disease will immediately make itself known.
Sometimes, if a virus has been in a cell for a long time and has not been able to manifest itself, its shell closes tightly, and the RNA of the virus cannot escape and create problems for its carrier. Such a virus remains sealed in the cell forever.
What determines the type of viral infection?
What is the reason that in some people the virus manifests itself immediately, while in others only the latent type of the disease is diagnosed?
Immunologists believe that the type of disease may be associated with two factors:
- The body's sensitivity to the pathogen. Some types of virions cause disease only in children. And the immune system of an adult is quite strong and is not susceptible to the weak effects of the virus.
- A small amount of viruses enters the body, which cannot counteract leukocytes. Therefore, the virus behaves non-aggressively. He is just trying to survive in new conditions.
The disease can be present in the body for many years and not appear until the person catches a cold. During an acute respiratory infection, the immune system weakens, there are no barriers to contain the infection, and then the first symptoms appear.
Cytomegalovirus in adults and children
One of the so-called TORCH infections is cytomegalovirus (CMV). It affects pregnant women and causes complex pathologies in newborns. CMV also very often occurs latently. In adults, the infection proceeds almost unnoticed. Young children may experience the following symptoms:
- jaundice;
- pneumonia;
- mild or moderate damage to the central nervous system;
- diseases of the gastrointestinal tract and genitourinary system, which periodically recur.
Adults usually do not even need to be tested for this infection. There are still exceptions. Those who plan to undergo radiation treatment, those who have AIDS, as well as young women planning pregnancy need to know about the presence of infection.
Is there a threat if the infection has been in the body for a long time, but does not provoke any complications? If it is indeed CMV infection, the latent course is usually harmless.
Etiology of glomerulonephritis
Typically, the onset of the disease in the 1st-3rd week is preceded by a streptococcal infection in the form of pharyngitis, tonsillitis, scarlet fever, and skin lesions (impetigo-ciderma). It has been established that acute glomerulonephritis is caused, as a rule, only by nephritogenic strains of b-hemolytic streptococcus of group A, having M12, 18, 25, 49, 55, 57, 60 antigens (others are much less common).
Among pyogenic skin strains of streptococcus A, nephritogenic one usually has T14 antigen. It is believed that if an outbreak of streptococcal A infection in a children's group is caused by nephritogenic strains, then 3-15% of infected children will develop nephritis, although among adults and children around the sick child, approximately 50% show changes in the urine, i.e. they are likely , suffer torpid (low-symptomatic, asymptomatic) nephritis.
Among children who have had scarlet fever , 1% develop acute glomerulonephritis during hospital treatment and 3-5% of children treated at home.
A respiratory viral infection in a child with chronic tonsillitis or carriage of cutaneous nephritogenic streptococcus can lead to activation of the infection and cause the occurrence of acute glomerulonephritis.
The etiological factors include cooling the body in a humid environment (“trench” nephritis). Cooling causes reflex disorders of the blood supply to the kidneys and affects the course of immunological reactions.
Chronic renal failure
Renal failure can be acute or chronic; There is also a subclinical course with a very long latent period.
A patient with a subclinical course has dry mouth, general weakness, and nausea. But classic symptoms and pain in the kidney area usually do not occur. Therefore, the patient does not at all suspect that he needs to go to the doctor and have his kidneys checked. The main symptom indicating the need for testing is polyuria, which gradually turns into oliguria.
It often happens that a long latent course of CRF (chronic renal failure) leads to the need for hemodialysis. This type of therapy is used quite often. Treatment of chronic renal failure with subclinical or latent course is carried out standard. If necessary, adsorbents and anti-inflammatory drugs are prescribed. Antibiotics are prescribed only when the causative agent of the infection is found.
With a latent course of pyelonephritis, which leads to renal failure, an increased erythrocyte sedimentation rate may be found in the analysis - above 12 mm/h. Leukocyturia is observed - up to 25 thousand in 1 ml of urine.
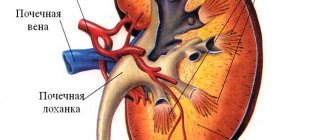
To investigate the causes of inflammation, if any, an ultrasound of the kidneys, angiography of the organ's vessels and also a sonogram are performed. On the sonogram you can see a cyst, an enlargement of the renal pelvis or stones in them. Only sometimes is an excretory urogram used.
Clinical picture of glomerulonephritis
Acute diffuse glomerulonephritis develops 6-12 days after infection, usually streptococcal (tonsillitis, tonsillitis, pyoderma); The most nephritogenic is group A 3-hemolytic streptococcus, especially strains 12 and 49. Hematuria (often gross hematuria), edema, oliguria, and hypertension are characteristic. In children, acute glomerulonephritis usually has a cyclic course with a rapid onset, and in most cases ends with recovery. In adults, the erased version with changes in urine without general symptoms is more common, gradually taking a chronic course.
The first signs of acute glomerulonephritis appear 1-3 weeks after an infectious disease or exposure to other factors. The disease begins with general weakness, headache, nausea, lower back pain, chills, and loss of appetite. There may be rises in body temperature to very high numbers. There is pallor of the face, swelling of the eyelids, and a sharp decrease in the amount of urine produced. The decrease in urine volume can last 3-5 days, after which diuresis increases, but the relative density of urine according to tests decreases. Another characteristic sign is the presence of blood in the urine - hematuria. Urine takes on the color of “meat slop” or becomes dark brown or black. In cases of microhematuria, the color of urine may not change. At the beginning of the disease, fresh red blood cells predominate; later, predominantly leached ones are released.
Proteinuria (albuminuria) is usually moderate (up to 3-6%), lasting 2-3 weeks.
Microscopy of urinary sediment reveals hyaline and granular casts, and with macrohematuria - erythrocyte casts. A study of endogenous creatinine clearance reveals a decrease in the filtration capacity of the kidneys. The Zimnitsky test detects decreased diuresis and nocturia. A high relative density of urine indicates preserved concentrating ability of the kidneys.
The content of residual nitrogen (acute) and urea in the blood increases. The content of creatinine and cholesterol is increased. When studying the balance of acids and bases in the blood - acidosis; a decrease in albumin and an increase in a- and b-globulins are detected. Leukocytosis and accelerated ESR are observed in the blood.
Edema is one of the most characteristic symptoms of glomerulonephritis. They are usually located on the face, appear in the morning, and decrease in the evening. Before visible edema develops, about 2-3 liters of fluid can be retained in the muscles and subcutaneous tissue. In obese children of preschool age, edema is more difficult to determine; sometimes they are determined only by some compaction of the subcutaneous tissue.
Hypertension is observed in approximately 60% of cases. In severe cases of glomerulonephritis, the increase in blood pressure may last for several weeks. Damage to the cardiovascular system in acute glomerulonephritis is observed in 80-85% of children. There may be an enlargement of the liver, changes in the function of the central nervous system.
With a favorable course of the disease, timely diagnosis and treatment, swelling disappears after 2-3 weeks and blood pressure normalizes. Typically, recovery from acute glomerulonephritis occurs after 2-2.5 months.
Antibodies LgG and Lg M
Antibodies are protein molecules that the body produces in response to the action of a pathological agent that has penetrated inside.
When the body gradually adapts and seeks means to fight a bacterium or virus, Lg M antibodies are formed in the blood. This class of antibodies makes up only 10% of all immunoglobulin fractions. But it is very active and at the same time activates other protective mechanisms.
The main immune response is provided by class G antibodies, or they are also called LgG. If a blood test finds predominantly these antibodies, it means that the disease is in an acute stage. They become active after 5 days during the normal course of the disease. But with latent LgG, the pathogenic microorganism is not noticed.
To determine some diseases, such as hepatitis of different strains, there are special tests to detect antibodies that can be performed at home.
LgG can cross the placenta to the fetus. And therefore, often at birth the child has some kind of protection, although still weak.
The healing process is indicated by Lg A antibodies usually circulating in the circulatory system. Sometimes it happens that no signs of infection were observed, but there are antibodies in the blood. This means that the disease passed in a latent form.
conclusions
So, how does latent differ from the usual acute or chronic course of the disease? The latent course of the disease is a hidden process. Pathogenic organisms in this course can be either passive, or their influence is so weak that the immune response to them is hardly noticeable.
It is usually not possible to detect antibodies using a biochemical blood test in this course of the disease. Inflammatory processes in the body sometimes go away on their own without traces, and sometimes are completely absent.
Latency
(from Latin latentis “hidden, invisible”):
- the property of objects or processes to be in a hidden state, without manifesting themselves explicitly [1];
- delay between stimulus and response:
- in computer and network technologies, latency is a delay or wait that increases the actual response time compared to the expected one;
- in computer networks, shows how long it takes a data packet to travel from one intended point on the network to another;
- in relation to network switches, the time it takes for a packet to pass through the switch;
- latency (characteristic of RAM) - time (in clock cycles) for executing a processor command or waiting for data to be delivered from memory; can be reduced by using read-ahead and multithreading technologies.
Is it possible to diagnose a disease with a hidden course?
Finding a latent disease using conventional diagnostic methods is a rather difficult task. If the virus does not manifest itself in any way, then antibodies will not be detected in the blood. A person may mistake mild weakness, which sometimes occurs, for overwork.
Doctors are unable to detect the virus using conventional diagnostic tests because the pathogen is often mutated. And the tests are designed only for standard strains. Another reason is that the virus is still too weak. Every disease has a latent period when viruses actively multiply and gain strength to resist antibodies.
The virus can be found when it enters the active phase and begins to multiply and cause harm to the body. Or when, at the end of the latent period, it is still possible to “detect” a pathogenic organism using diagnostic tests and give it a definition.
Latent tuberculosis infection can be determined by two parameters. Firstly, if there is a marker of predisposition to the disease. Secondly, a reduced cytokine index is detected. Then a person can safely be diagnosed with “latent tuberculosis.” This means that it is necessary to plan treatment measures and register the person with a tuberculosis dispensary.
Differential diagnosis
When the first nonspecific signs of latent tuberculosis appear, differential diagnosis is carried out with the exclusion or confirmation of the following diseases:
- lymphogranulomatosis (Hodgkin's disease);
- mycobacteriosis (MAS infection);
- chronic airway obstruction;
- oncological pathology of various localizations, including lung cancer.
To conduct a qualitative differential diagnosis, various research techniques are used, including CT (computed tomography) or MRI (magnetic resonance imaging).
Treatment
In each specific case of a latent disease, treatment will be different. Some bacteria respond to certain antibiotics, while others are difficult to treat with drugs. For example, the same cytomegalovirus is “embedded” in the cell’s DNA and it is generally impossible to “get it out” from there or to influence it with drugs. The host's body simply adapts to the pathogen.
If anicteric hepatitis B is suspected, the patient may be prescribed a special diet to support the liver. But while there are no official test results confirming the presence of hepatitis, no treatment is being carried out.