Possible reasons
The color of urine changes as soon as the inflammatory process starts in the body. The type of urine largely depends on the concentration of substances excreted by the body, such as salts or pigments. Normally, various factors can cause changes in the color of the excreted fluid.
It depends on the:
- the amount of substances dissolved in urine;
- physical activity of the baby;
- his current state;
- drinking regime.
Cloudy urine in a child 2 years of age, younger or older, occurs immediately after sleep. Usually doctors advise not to pay attention to this or to observe the child during the day. If, in addition to the change in color, your child has a stomach ache or other symptoms, he may be sick.
Adults should pay attention to the color of the baby’s urine in order to promptly notice and eliminate problems that have arisen. To do this, it is enough to collect urine once a day and pour it into a special container for color assessment.
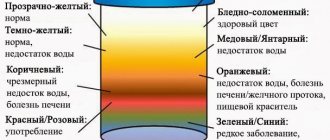
Cloudy urine in a child may have different shades of color
Cloudy and discolored urine in children 2 years of age or older may indicate:
- a disease developing in internal organs;
- reactions to medications taken;
- influence of the external environment.
Among the factors influencing the color of the discharged liquid are:
- foods that the child eats;
- the medications he is taking;
- amount of drinking water consumed.
Urine fluid may change color due to factors such as:
- metabolic disorders in the body;
- an indicator that the child is growing: the older he is, the darker the urine will be;
- parts of the day. The color of urine in the morning is more saturated.
Causes of changes in urine color include:
- dark color of urine during morning toilet. However, if the color of the liquid returns to normal during the day, there is no need to worry;
- consumption of products with a high coloring effect. These include beets, pumpkin, carrots;
- lack of fluid entering the body. This can cause dehydration and intoxication of the body, because harmful substances are not eliminated in full;
- external air temperature is too high;
- taking certain types of medications that can color urine when excreted from the body;
- consumption of vitamin complexes, which include vitamins B and C.
The color of urine is also affected by some diseases that are present in the child’s body:
- infections of the genitourinary system. In this case, blood particles may appear in the secreted fluid. This indicates that inflammation of the bladder and kidneys has begun.
Dietary changes
The ideal indicator for a newborn is colorless urine that has no odor. In the first 2-7 days of life, urine may be cloudy. In breast-fed children, colorlessness persists for up to 6 months, that is, until complementary foods are introduced. During this period, the tone of urine may change from a wheatish hue to an amber color (as in adults). This indicator is affected by nutrition.
Fact! On the first day of life, a baby's urine may be brick-colored. This phenomenon is a consequence of the release of urates due to the consumption of colostrum.
The baby’s body is extremely vulnerable, and all its organs can react sharply to the medicinal compounds consumed by the mother. Many active ingredients pass into breast milk - the mother should remember this and discuss the possibility of taking any medication with the doctor.
A baby’s urine may change color when consuming natural drinks (juice, fruit drink, compote, decoction) from the following plants:
- beet;
- blackberry;
- black currant;
- rhubarb;
- carrot.
The listed products act as dyes, but do not worry, they do not cause any harm to the child’s body.
Urine may take on a darker hue due to dehydration - a condition that is extremely dangerous. A lack of fluid in the body is more often diagnosed in the summer, so parents should monitor the child’s water regime. Dehydration occurs when the temperature rises.
If cloudy urine appears one time in a child and the condition is not accompanied by other manifestations, most likely this is a natural physiological reaction of the body. If this symptom recurs, you should contact a medical facility.
Diagnostics
To determine the causes of abnormal urine color in children, the doctor prescribes a range of tests and studies:
Urine according to Nechiporenko. Norm and features of carrying out
| Study | Description |
| General analysis | It is performed to determine the chemical composition of urine. This will allow you to quickly identify diseases of the kidneys, endocrine system and the presence of tumors. Cost – about 200 rubles. |
| Urine examination using the Nechiporenko method | Detects hidden infections of the urinary system and kidneys. The price is approximately 290 rubles. |
| Carrying out samples according to Zimnitsky | It is used for suspected diseases such as diabetes, pyelonephritis, and renal failure. Cost – 300 rub. and more |
| Sulkowicz method | The method allows you to recognize diseases of the endocrine system. The price starts from 150 rubles. |
| Diagnosis of urine according to Kakovsky-Addis and Amburge | The method is used to determine the likelihood of inflammatory processes. Its price is from 700 rubles. |
| Bacterial culture | It detects the presence of harmful bacteria and microbes in a person. The price starts from 800 rubles. |
During the examination it is worth knowing that:
- in infants who are fed breast milk or formula, urine is most often light and clear;
- when the child grows up and begins to feed on his own, the urinary fluid becomes more yellow;
- if the child needs to go to the toilet at night, the color will be even more concentrated.
Each diagnostic method differs in its method of collecting urine. This is often done using small urine bags. This is convenient for both boys and girls.
The most important thing is the general analysis, which provides complete information about the following:
- texture and color;
- density and weight;
- acidity and hemoglobin level;
- the presence of ketone bodies and urolobilinogen;
- content of glucose, nitrates, bilirubin and protein.
In addition, urine sediment is examined for the presence of:
- tumor cells;
- fungi and parasites;
- harmful bacteria;
- white and red blood cells;
- cylinders
Depending on the ratio of inorganic substances contained, other tests are additionally prescribed, as well as ultrasound of the genitourinary system and biochemical blood tests.
Urine collection rules
The basic rules for collecting urine in young children are as follows:
- Informing the attending physician what medications the patient was taking to prescribe the necessary tests.
- Purchasing a special container from a pharmacy.
- Collecting material after the child wakes up in the morning.
- Wipe your genitals with a tissue before urinating to keep them clean. You need to take average urine.
For a good analysis, you will need about 30 ml of liquid, which is sent to the laboratory no later than 2 hours from the moment of collection.
The appearance of sediment in the urine
As soon as a child has urine with sediment or flakes, it can be assumed that protein compounds have appeared.
According to the standard, only a small amount of this substance is permissible. Its excessive concentration indicates that there is a dysfunction of the kidneys and the genitourinary system as a whole.
It happens that the presence of protein indicates an excessive load on the body, for example, such a load can be hypothermia, stressful situations, depression and excessive physical activity.
If there is sediment in your child's urine, the first thing you need to do is remember what new foods have been introduced into the diet. If in general the child behaves normally and his appetite is not impaired, then there is a possibility that the tests will soon return to normal.
In other cases, when the child’s behavior changes significantly, you should contact an appropriate specialist.
When to see a doctor
However, some manifestations are considered deviations from the norm:
- the presence of flakes and cloudiness of urine, which does not go away for some time. This may be a sign of inflammation within the urinary system or kidneys. If urine sits in the test container for too long, it becomes cloudy due to the precipitation of mineral salts. This reaction indicates the baby’s good health;
- the presence of a large number of red and white blood cells in the fluid. This happens when the liver is poisoned. She does not have time to process these substances due to the high load;
- when the temperature remains normal, but the color of the urine changes and pain is felt in the abdominal area, there may be problems with the excretory systems;
- at elevated temperatures and turbidity of the urine, dehydration can be suspected. To normalize the baby’s condition, he is given a lot of plain water to drink;
- turbidity of the excreted fluid, accompanied by a strong odor, may occur with some diseases, such as diabetes or a urinary tract infection;
- Dark colored urine occurs with hepatitis.
Pediatric doctors advise parents to carry out a similar procedure every six months, even if there are no symptoms of the disease.
Color standards for children's urine
Like any liquid, urine has many characteristics. Color and transparency depend on metabolism, mobility, climatic conditions and the amount of fluid drunk. The norm of incoming fluid for a child weighing 3-10 kg is 100 ml per 1 kg of body weight, and for a child weighing 11-20 kg it is 50 ml per 1 kg of body weight per day. Conclusion: the less the baby drinks and moves, the richer the color of his urine will be.
It is also very important to know what he ate the day before. If beets were present in the diet, then the urine will take on a reddish tint, carrots will turn orange, and rhubarb will give a greenish color. Eating artificial colors (sweets, candies, marmalade, carbonated drinks, etc.) will give your urine a bright yellow tint. That is why the pediatrician always checks what your child has eaten in the near future.
Ideally, the liquid should be transparent, light wheat in color, without odor, flakes or sediment. And even if a child’s urine becomes cloudy, this does not mean that he is not healthy. It becomes like this when in contact with air for a certain time.
Treatment methods
If the cause of the pathology is the development of an inflammatory process, antibacterial and anti-inflammatory drugs are prescribed. In case of poisoning and intoxication, you should drink a lot and take vitamin complexes to replenish the lack of nutrients in the body.
Cloudy urine in a child 2 years of age or older requires the following actions:
- it is necessary to give the child more fluids;
- you need to stop feeding foods with coloring elements;
- Excessively fatty and salty foods should be avoided;
- you need to cancel or replace medications after consultation with your pediatrician.
Medications
Diseases of the urinary system are treated by a pediatric nephrologist. For therapy, not only drug therapy is used, but also physical therapy, and in some cases, surgery.
For treatment, drugs that have proven themselves in medical practice are used. They are effective for destroying pathogenic microbes, inflammatory processes and normalizing metabolic processes in the body. The doctor decides what medications are needed in a particular situation. He also chooses the dosage of medications and the schedule for taking them.
If pathological changes are detected in a child, the treatment regimen includes:
- diuretics and blood pressure-lowering drugs – for kidney disease;
- hepatoprotectors – for injuries or infections of the liver area;
Hepatoprotectors - Medicines for the liver - antibiotics, antispasmodics and analgesics - for urolithiasis.
The dosage depends on the complexity of the symptoms and the age of the child. The cost of treatment depends on the duration of the course and the type of medications prescribed.
Traditional methods
Cloudy urine in a child 2 years of age and older can sometimes be cured with folk remedies.
For example:
| Recipe | Description |
| Anti-inflammatory infusion | Helps with diseases such as cystitis and pyelonephritis. Includes:
Prepare as follows: 1. Plants are taken in equal parts. 2. 1 tbsp. l. dry raw materials are poured with 400 ml of boiling water. 3. After 2 hours, the infusion is filtered and can be taken. Take 4 times a day, half an hour before meals. The course of admission is at least 7 days |
| Diuretic composition | For this decoction: 1. Take 1 tbsp. l. bearberry. The raw materials are poured with 200 g of water and boiled for 20 minutes over low heat. 2. Leave the container for half an hour to infuse. 3. The strained drink is diluted with 1 tbsp. water (pre-boiled). The composition is taken 50 ml 3 times a day, 30-40 minutes after meals. Course duration – week |
| General strengthening composition | For this infusion you need: 1. Take 2 tbsp. l. corn silks and pour boiling water (300 ml). 2. Leave to infuse for 2 hours. The strained medicine is taken 3 times a day before meals, 1 tbsp. l. Reception course – 2 weeks |
You can also take cranberry or lingonberry juice to treat mild inflammatory infections of the genitourinary system. To normalize, it is enough to drink 1 tbsp. l. several times a day for 3 days.
Diet
Sometimes a special diet is recommended to restore normal functioning of the genitourinary tract and the normal color of urine. With it, the number of products with increased diuretic ability increases. At the same time, it is forbidden to eat fried and fatty foods: they retain fluid in the body.
The daily menu should contain a lot of:
- fresh fruits and vegetables;
- croup;
- quality fermented milk products;
- fish;
- homemade juices and fruit drinks;
- eggs;
- green tea.
You need to eat little by little at least 5 times. You should also drink as much clean water as possible.
Other methods
In addition to drug treatment and the use of traditional methods, surgical intervention is sometimes used. This happens when other methods are ineffective. Physiotherapy is also used to normalize the color and eliminate the symptoms of cloudy urine.
The most effective in this case will be the following methods:
- electrophoresis. It is performed for inflammatory infections accompanied by painful attacks. The current pushes the medicine to the diseased area, reducing its manifestation;
- laser therapy. A beam of light easily penetrates the problem area and reduces pain, restoring damaged tissue;
- magnetic therapy. Mobilizes the body's protective properties, providing a general strengthening effect;
- mud therapy. Effective for cystitis and chronic pyelonephritis. Before use, the composition is warmed to a comfortable warm temperature. Heat stimulates blood flow and thereby normalizes the functioning of the diseased area.
It is prohibited to use any methods of physiotherapy for any tumors and diagnosed polycystic disease. They provoke the growth of diseased cells and can cause the rapid development of the disease.
Clinical (general) urine analysis
Urine is a biological fluid produced by the kidneys and excreted from the body through the urinary tract.
Approximate norms for the volume and frequency of urination depending on age
| Age | Volume of one portion of urine, ml | Number of urinations | Daily urine volume, ml |
| 1 day | — | 4–5 | up to 60 |
| Up to 6 months | 10–30 | 20–25 | 300–500 |
| 6 months - 1 year | 15–60 | 15–16 | 350–750 |
| 3–5 years | 90 | 10 | 1000 |
| 7–8 years | 150 | 7–6 | 1200 |
| 10–12 years | 250 | 5–6 | 1500 |
Clinical urine analysis is a standard mandatory test not only for diseases (suspected diseases) of the kidneys and urinary tract, but also for any clinical examination in general.
Rules for collecting urine for research
- The dishes must be clean, dry, flat-bottomed, free of detergent residues, glass or plastic, and specifically designed for collecting urine.
- Thorough hygienic treatment of the external genitalia.
- The first morning urine is taken, the entire portion.
- Urine must be delivered to the laboratory within 1.5 hours after collection.
Physical properties of urine
Color
Urine contains pigments that color it yellow in varying degrees of saturation. The less urine, the richer it is, the more intense the yellow color. In diseases accompanied by excessive urination (for example, diabetes), the urine becomes almost colorless (pale pale yellow).
Three circumstances can change the color of urine:
1) illness; 2) some food products; 3) some medications.
With jaundice, urine becomes a rich dark yellow color. Blood entering the urine (injuries, stones in the urinary tract, glomerulonephritis, etc.) gives it a red tint, the saturation of which is determined by the volume of blood that has entered. Eating large quantities of carrots turns urine orange, beets red, rhubarb greenish. Methylene blue (blue), ingested by a child when cleaning the oral cavity, gives the urine a blue color, the antibiotic rifampicin gives it a red color.
Transparency
Normally, urine is clear, but when standing (settled), it becomes cloudy due to the precipitation of salts. The turbidity of freshly excreted urine may be due to the presence of protein, leukocytes, red blood cells, mucus, fat, and an increased amount of salts. The more of the above, the more intense the turbidity.
Smell
The characteristic odor of urine intensifies when it comes into contact with air. There are very few diseases that specifically change the smell of urine. A classic such disease is diabetes mellitus, in which the smell of urine takes on a fruity hue. The smell of urine can be affected by certain foods (garlic, horseradish, etc.) and certain medications.
Density
Speaking about the density of urine, as a rule, we mean its relative density. The density of urine is not constant and fluctuates all the time during the day. Density is determined by the amount of various substances dissolved in urine. The kidneys, in the process of filtering blood, form the so-called primary urine. A significant portion of the primary urine is reabsorbed and returned to the bloodstream. The kidneys thus produce more concentrated secondary urine. This is the concentration function of the kidneys, the violation of which (for example, in diabetes insipidus, some types of chronic nephritis, etc.) leads to a decrease in the relative density of urine. The appearance of protein, sugar, leukocytes, red blood cells, etc. in the urine increases the density of urine. The concentration function of the kidneys, and therefore the average relative density of urine, depends on age.
| Age | 1 day | Up to 6 months | 6 months - 1 year | 3–5 years | 7–8 years | 10–12 years |
| Relative density of urine | 1,008–1,018 | 1,002–1,004 | 1,006–1,010 | 1,010–1,020 | 1,008–1,022 | 1,011–1,025 |
The relative density of urine is determined using a special device - a urometer. The urometer is lowered into a special narrow cylinder, into which 50 ml of urine is first poured. Thus, to determine the density of urine, it is necessary that at least 50 ml be delivered to the laboratory. In pediatric practice, this does not always work out, so in the form of a clinical blood test you can often see the following entry: Density - m/m (variants of small m., m. m. m/urine, etc.), which translates as "little urine" However, it is possible to determine the density in a small amount of urine. To do this, the available amount is diluted a certain number of times with distilled water to make 50 ml, the measurement is carried out in a urometer and the last two digits of the resulting indicator are multiplied by the degree of dilution.
Normal range: 1.002–1.040.
Chemical examination of urine
Reaction
Let us first remind you what pH is. pH is the ratio of hydrogen ions (H+) and hydroxide ions (OH-). If the amount of H+ is equal to the amount of OH-, the solution is called neutral. If H+ > OH-, the solution is called acidic, if H+ < OH- - alkaline.
Normally, urine is slightly acidic. Any long-term pH shift is an undesirable factor that can lead to the formation of kidney stones in the urinary tract. Stones are different. Urate and uric acid stones are formed when the urine reaction shifts to the acidic side, phosphate stones - when the reaction shifts to the alkaline side.
A shift in the urine reaction to the acidic side is possible when:
- excessive protein intake;
- fever;
- prolonged physical activity;
- fasting;
- diabetes
A shift in the urine reaction to the alkaline side is possible when:
- vegetarian diet;
- loss of hydrochloric acid by the body (through vomiting);
- chronic urinary tract infection.
Normal range:
pH = 5.0–7.0.
The average value is 6.25.
Protein
Normally, there is no protein in the urine. That is, theoretically it is there, but its quantity is so small that detection requires special techniques that have no practical feasibility. The research begins with qualitative samples, i.e. That is, they are trying to answer a simple question: is there protein in the urine or not? To do this, urine is mixed with a certain reagent: if a reaction occurs, there is protein, if there is no reaction, then there is no protein. If there is no protein, the study ends here; if there is, then they answer the following question: how much protein is in the urine? To do this, quantitative tests are carried out - the amount of protein in the urine is determined in grams per liter. Most quantitative samples used detect protein when its concentration exceeds 0.03 g/L. If the amount of protein is less than 0.033 g/l, the expression “traces of protein detected” or “barely noticeable traces of protein” is often used. Proteinuria , which is the name given to the condition in which protein is detected in the urine, can be pathological (associated with kidney disease) and functional (not associated with kidney disease).
Functional proteinuria can occur with:
- physical activity;
- emotional stress;
- excess protein foods;
- increase in body temperature.
The most common causes of pathological proteinuria include:
- glomerulonephritis and pyelonephritis;
- nephropathy of pregnancy;
- hypertension and circulatory failure;
- kidney tuberculosis, etc.
Glucose
There is no glucose in the urine, but it may appear briefly with active absorption of sugar or when treatment with glucose is carried out (intravenous administration). Normal blood glucose levels are 3.3–5.5 mmol/L. There is such a thing as the “sugar threshold” - a critical level of increased glucose in the blood, after which it appears in the urine. For most healthy people, regardless of age, the sugar threshold is 8.8–9.9 mmol/l. Hence the important conclusion that glucosuria (detection of glucose in the urine), as a rule, occurs when its level in the blood is above 10 mmol/l. Most often this occurs with diabetes mellitus. Inflammatory processes in the kidney tissue (nephritis) can lead to a decrease in the sugar threshold. In this case, glucose can be found in the urine even when its level in the blood is normal. In the vast majority of cases (both in medical institutions and at home), test systems in the form of strips are used to detect glycosuria, onto which a few drops of urine are applied. The color change is compared with a rating scale, and on this basis a conclusion is given not only about the presence of glucose in the urine, but also about its quantity.
Ketone bodies (acetone)
Ketone bodies include three components of urine - acetone, acetoacetic acid and betahydroxybutyric acid. Normally, ketone bodies are not detected in urine. Their appearance indicates disturbances in the metabolism of fats and carbohydrates. Such disorders occur many times more often in children than in adults. The fact is that the human body receives energy mainly from glucose. Glucose accumulates in the body, primarily in the liver, in the form of a special substance - glycogen. In adults, glycogen reserves are huge, in children they are insignificant. With physical exertion, emotional stress, high body temperature, i.e., with any phenomenon that requires significant energy expenditure from the child’s body, a situation may arise when glycogen reserves run out. As a result, the body begins to receive energy from fat reserves. Intensive breakdown of fat is accompanied by the formation of ketone bodies, which are excreted in the urine ( ketonuria ).
In addition to the listed conditions, ketonuria can occur with:
- diabetes mellitus;
- low-carbohydrate diet;
- prolonged fasting;
- repeated vomiting.
The most common method for determining ketonuria is similar to that used to detect glycosuria - test strips + urine, color change, comparison with a rating scale, conclusion about the presence or absence of ketone bodies.
Bile pigments
Bile pigments (bilirubin, urobilin, bile acids, etc.) are absent in the urine. Their appearance indicates an increase in the level of bilirubin in the blood, and what is primarily important is the increase in conjugated bilirubin, which occurs with hepatitis and obstructive jaundice. An increase in the level of free bilirubin in the blood does not lead to the appearance of bile pigments in the urine, since free bilirubin is combined with albumin and therefore does not pass through the kidney filter.
Microscopy of urinary sediment
After urine has stood for at least 1-2 hours, sediment will form. The sediment is collected with a special pipette (which is why the container for collecting urine must have a flat bottom). The resulting liquid is centrifuged, and then the sediment from the centrifuge tube is examined under a microscope. In the urinary sediment you can see blood cells, salt crystals, epithelial cells, mucus and much more. The image that a laboratory doctor sees in a microscope is a circle within which the objects in question are present. The round picture available for inspection is called the field of view - this is, in fact, what is visible at a given moment in time in a given preparation. So, the doctor looked into the microscope and saw 5 leukocytes. In the analysis form it will look like this: leukocytes - 5 in the field of view (more often: 5 p/zr or p/z, p. zr., pz, pzr). As a rule, you have to look into the microscope several times. The doctor looked, saw 5 leukocytes, slightly moved the preparation - 3 leukocytes, moved it again - 2. Thus, in the final analysis there will be not one number, but a range. For example, leukocytes: 2–5 per field of view. The number of elements visible in the field of view can be very large, so large that they simply cannot be counted. Now that we understand the meaning of the expression “field of view,” the phrase “red blood cells in the entire field of view” or “leukocytes in ½ field of view” becomes clear. Sometimes the expressions “leukocytes in groups of 20–30”, “clusters of red blood cells 10–15” are found. Let us explain: when the shaped elements are concentrated in several layers, it is called a group, and when they are located nearby and can be counted, it is a cluster. The opposite situation is also possible: there are not many objects under consideration, but very few. In this field of vision there is, but in the other there is not. Or even two pieces were found for the entire drug. Hence the entries: “occasionally”, “in places”, “single red blood cells in the preparation” or “1-2 red blood cells not in every field of view”.
Red blood cells
The appearance of red blood cells in the urine largely depends on the pH of the urine. In a slightly acidic and slightly alkaline environment, red blood cells retain their appearance for quite a long time, except that they swell slightly, but in an acidic environment they lose hemoglobin. This process is called leaching. Red blood cells that have lost hemoglobin are called leached. Leached red blood cells look like colorless rings. Normally, there are very few red blood cells in the urine. Single unchanged red blood cells can be detected when the mucous membranes of the urinary tract are damaged by salt crystals or when there is scratching due to itching in the genital area. Detection of red blood cells in the urine - hematuria - a sign of bleeding in the urinary system; most often this occurs with urethritis, cystitis, nephritis, urolithiasis, injuries and kidney tumors. If there are so many red blood cells that it causes the urine to change color, the condition is called gross hematuria. If the urine color is normal, and red blood cells are detected only by microscopy, this condition is called microhematuria.
Normal range:
single in the preparation - 0–2 not in every field of view.
Leukocytes
Leukocytes are always present in urine, but their numbers are small. Inflammatory processes in the urinary system sharply increase the number of leukocytes. Therefore, counting leukocytes in urinary sediment is one of the most effective ways to diagnose urinary infections. The dynamics of the number of leukocytes allows us to evaluate the effectiveness of the treatment. An increase in the level of white blood cells in the urine is called pyuria .
Normal range:
boys - 5–7 in the field of view; girls - 7–10 in sight.
Cylinders
In some kidney diseases, protein, leukocytes, red blood cells, fat droplets, and epithelial cells may accumulate in the renal tubules. Such clusters form a kind of cast of the tubule - a cylindrical formation. These formations are called cylinders. Accordingly, an increased number of casts in the urine is called cylindruria. The appearance (shape, color, size) of the cylinder depends on the material from which it was predominantly formed, therefore the analysis not only indicates the number of detected cylinders, but also their type. Hyaline casts are formed mainly from protein, leukocyte casts - from leukocytes, granular casts - from kidney epithelial cells, blood casts - from erythrocytes. Cylindruria can be a reflection of a significant load on the kidneys in any general disease, and also indicate an inflammatory process in the renal tissue.
Normal range:
single in the preparation.
Epithelial cells
The inner surface of the urethra, bladder, ureters, and kidneys is lined with special epithelial cells. Inflammatory processes in the urinary tract lead to the fact that epithelial cells are found in significant quantities in the urinary sediment. A laboratory doctor has the ability to distinguish, for example, kidney epithelium from bladder epithelium, therefore the type of epithelial cells detected is indicated in the analysis results. This provides information about in which part of the urinary system the inflammatory process is taking place. In addition to the epithelial cells of the urinary system, the urine sediment may also contain cells of the so-called squamous epithelium. Squamous epithelium is the epithelium of the mucous membrane of the vagina and external genitalia.
Normal range:
single in the preparation.
Salts
Salt crystals may be found in urine sediment. The types of salts are determined by the reaction of the urine and have no special diagnostic value. Crystals of uric acid and urate are found in acidic urine. Urates are salts of potassium urate, sodium, calcium and magnesium. Phosphates are formed in alkaline urine. Oxalate salts appear in both acidic and alkaline urine. Their occurrence is often associated with eating food containing oxalic acid (apples, grapes, citrus fruits, tomatoes, sorrel, beets, etc.).
(This publication is a fragment from the book by E. O. Komarovsky “Handbook of Sensible Parents. Part One” adapted to the format of the article)
author Komarovsky E.O. published 12/23/2014 15:51 updated 11/24/2016 — Diseases and treatment
Possible complications
If the disease is neglected, the following may occur:
- renal failure;
- poisoning. Its signs, in addition to changes in the color of urine, are severe vomiting and sharp pain in the abdomen;
- cirrhosis or hepatitis;
- urolithiasis;
- tumor in the pancreas area;
- very dark urine color may be the first sign of kidney stones, gallstones and bladder stones, liver damage from toxins and hemolytic anemia.
Cloudy urine is often a sign of illness in a baby. If you do not pay attention to the color of urine, you can waste time and then the disease will enter the chronic stage.
If a child is 2 years old, or older or younger, the urine has become cloudy and dark in color, such symptoms should not be ignored. Sometimes such a sign indicates the onset of a serious illness. Parents should consult a doctor for an examination and, if necessary, begin treatment.
Tips for parents
If you find sediment in your child’s urine or a change in its color, this is not always a cause for concern. First of all, evaluate:
- How long ago did the child empty his bladder?
- Did he have any dietary problems?
- How was the urine stored and at what temperature?
- Did the baby have any stress or heavy physical activity?
- How much liquid does a baby drink per day?
- Does he have any other manifestations of diseases, and has his general condition become impaired?
Only after analyzing all this can you make a decision about your further behavior.
What does sediment consist of?
Turbidity of urine can be explained by the presence in it of such cellular elements as leukocytes, erythrocytes, bacteria, epithelial cells, urate, phosphate or oxalate salts, protein. These tiny particles can settle or float in the urine in the form of threads, small grains and suspensions. Sometimes they can be seen as white flakes in an infant's urine.
Urates appear in the body during the processing of meat, phosphates - during the absorption of breast milk and dairy products, and oxalates are formed after the child has consumed fruits and vegetables rich in vitamin C. Urates, phosphates and oxalates, as a rule, form honey fungus or a dense cloud on the surface of urine. Crystals of these salts can accumulate in the kidneys in the form of sand grains, and in particularly difficult cases, form urinary stones of various sizes. Their number can increase not only due to an unbalanced diet.
Oxalaturia manifests itself in disorders such as hypovitaminosis (insufficient amount of vitamin B6), magnesium deficiency, Crohn's disease, diabetes mellitus, chronic pyelonephritis, and metabolic disorders. With phosphaturia, a lot of phosphate salts, as well as calcium and magnesium, are released in urine. This often occurs when the acidity of the gastric juice increases, which, in turn, leads to disturbances in mineral metabolism. With uraturia (excessive secretion of uric acid), the sediment in the urine becomes brick-red in color.
Additional Information. If parents see that sediment or plaque has appeared in the child’s pot after a certain time, but the urine is clear and nothing bothers the baby, there is nothing very bad in this situation. Salts can be excreted in the urine, which begin to be deposited at the very bottom of the pot if it is not washed well. The baby’s toilet should be washed daily with soap and disinfected with special products.
Sediment under a microscope
Cases when cloudy urine is normal
If you suddenly see cloudiness in your urine and the appearance of a white sediment or flakes in it, or it turns white, do not panic ahead of time. It is quite possible that this is not a symptom of any disease at all. Normally, the urine of any healthy person can form sediment when stored for a long time. Mineral substances that are in the urine crystallize and precipitate over time and from a decrease in temperature. This makes the urine cloudy, white, and mixed with flakes. That is why for analysis you should take only the morning portion of urine, collected no later than two hours before delivery.
Cloudiness, flakes, and white urine are also possible as a result of dehydration. This often happens in the summer, after intense physical activity, visits to saunas and baths. These changes do not require special treatment - you just need to drink enough fluid (at least 2 liters per day). Various herbal teas, non-carbonated mineral water, fruit drinks and the like are perfect for this.
We should not forget about proper, balanced nutrition. Very often, cloudy, white urine with white flakes appears after eating salty, spicy foods, or a predominance of meat dishes in the diet. All this puts a lot of pressure on the kidneys, which causes their failure and changes in urine.
Here it would not be amiss to mention excessive consumption of alcohol, toxic substances and drugs. These substances destroy the structural unit of the kidney - the neuron, as a result of which it functions worse.
White urine in a child: understanding the causes of the pathology
A change in the color of urine can tell parents a lot of things. However, we should not forget that food, drinks, and medications also affect its shade.
Before you turn to a specialist for help, remember if your child has taken anything unusual for his diet.
It should also be noted that children from birth to three years old need to take it at least once every three months.
If you are going to vaccinate your baby, then you need to know that blood and urine tests are a mandatory procedure before vaccination.
The appearance of so-called “white” urine can signal the onset of quite serious diseases. If the urine does not change color over the course of 3 days, you should urgently undergo additional tests.
The appearance of white urine can be caused by:
- Diabetes mellitus
- Kidney failure
- Using large amounts of water
- Eating diuretic foods, for example, watermelon, grapes.
- Use of medicinal diuretics
If you still haven’t decided whether to go to the doctor or not, then remember, if over the course of a week the volume of urine has decreased and it has become almost transparent, immediately go to see a specialist.
Do not self-medicate. This is especially true for very young children. Self-administration of medications is strictly prohibited.
It should be noted that the exception is newborn babies. In the first months of life, their urine is pale in color. This can easily be explained by the fact that the newborn consumes breast milk or. Only when complementary foods are introduced will the baby’s urine change shades.
So, white urine, in rare cases, can be considered normal. However, if the color remains transparent for one week, you should immediately seek help from a pediatrician, who will definitely prescribe a clinical urine and blood test.
How to recognize
After collecting urine, a change in color or the presence of sediment is alarming.
Normally, children have light-colored urine, while newborns have transparent urine. It is odorless and has a uniform consistency. The color of this liquid is affected by food, medications, diseases and other factors. Changes in color and consistency may be temporary and do not require treatment. Sometimes this is a symptom of pathology. Pathology can be noticed during urination or in the form of sediment formation. After collecting the analysis, when the container is standing, inclusions can be found at the bottom. It is white, yellow or another color.
White flakes indicate the presence of kidney and urinary system diseases. Most often, they indicate an inflammatory process, as a result of which mucus and epithelial cells become deposited. The urine may be dark in color.
Preliminary diagnosis of the disease by the color of urine
Without waiting for a diagnosis in the laboratory, you can visually determine the ongoing disease in the body. Laboratory tests will only confirm the current situation:
- Dark red tone - glomerulonephritis develops, damage to the internal walls of the bladder occurs.
- Sandy sediment – the formation of urolithiasis.
- Yellow-green tone – hepatitis.
- Dark yellow urine – burns, dehydration, hydronephrosis.
- A whitish sediment, bloody discharge or the presence of pus – pyelonephritis.
The detection of an abnormal shade, both in a newborn and in an older baby, does not indicate pathology. It is necessary to pay attention to the general condition of the baby. If fever and other symptoms of inflammation appear, then consultation with a pediatrician is essential. But if the child does not show signs of illness, then there is no reason to worry.
Preventive measures
If the reasons for the loss of color in your baby’s urine are physiological and associated with excess hydration, then he just needs to drink a little less water or eat juicy fruits. Everything will return to normal within a couple of days.
Preventive measures to prevent urine discoloration, if associated with pathologies, correspond to measures to prevent these diseases:
- To reduce the risk of developing diabetes in infants, nursing mothers are advised to eat as little sugar as possible, and formula-fed infants are advised to choose unsweetened infant formula;
- In order to prevent the occurrence of infectious diseases of the urinary tract and kidneys, it is necessary to monitor the temperature, not allowing children to become hypothermic;
- Encourage the child's mobility, do physical exercises with him, including taking baths on time. Massage has a beneficial effect on the baby's health;
Physical exercises with babies
- It is necessary to keep the baby clean and dry at all times;
- It is better to wash the baby’s intimate parts with water, blotting with a clean cotton cloth. In girls, washing should be done from front to back to prevent microorganisms from entering the anal area into the genital area.
Important! The use of wet wipes should be avoided. This increases the likelihood of developing a urinary infection.
Changes in the color of urine in most cases are a harmless consequence of the use of certain foods or medications, and its discoloration is caused by drinking large amounts of liquid. However, sometimes this can indicate the development of diseases, so it is important to consult a doctor promptly if you have alarming symptoms.
Additional Research
The pediatrician will prescribe the necessary tests to accurately determine the disease and send you for additional advice to a nephrologist, urologist or other specialist.
Tests that may be prescribed:
- general urine analysis;
- general urine analysis;
- analysis according to Nichiporenko;
- Zimnitsky's technique;
- Ultrasound of the kidneys, bladder, liver.
Dr. Komarovsky notes that diseases are often sluggish. In this case, the child may not be bothered by fever, pain and cramps, but cloudy urine or other symptoms may be observed. They should alert parents who cannot look for the cause on their own when it comes to a child. Timely contacting a doctor will help identify the problem at the initial stage, which means treatment will be more effective.