!!! The “Plow” and “Birch” exercises are fabulously useful for sick and healthy kidneys, but they cannot be done if you have arterial hypertension.
This is an immunoallergic kidney disease, characterized by bilateral non-purulent inflammatory damage to the capillaries (small vessels) of the glomeruli or the cavity of the glomerular capsule. It usually appears 1 to 3 weeks after suffering tonsillitis, tonsillitis, scarlet fever and other streptococcal infections.
, as well as
viral
infectious diseases.
The body's immune system produces antibodies that destroy streptococcus, and after healing, these same antibodies begin to destroy the cells of their own connective tissue, as they identify them with bacterial cells because streptococcal cells and connective tissue cells are similar in structure.
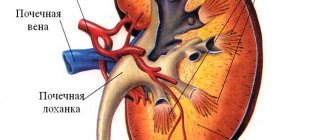
The accumulated immune complexes, which include antibodies, are deposited on the membranes (walls) of the capillaries of the glomeruli of the kidneys, where these immune complexes are enveloped by the substance of the basement membrane. In other words, they grow into the walls of the small vessels of the kidneys; the walls of the capillaries thicken and collapse, the kidney cells atrophy, which leads to functional disorders of the kidneys. There is oliguria (little urine), hematuria (blood in the urine), proteinuria (protein in the urine) and cylindruria (casts found in the urine during laboratory testing are casts of the kidney tubules, consisting of red blood cells, blood proteins and tubular epithelial cells, their appearance indicates the severity of glomerulonephritis).
Pre-existing kidney diseases, such as pyelonephritis, nephrolithiasis, kidney tumors, inflammation of the bladder, prostate adenoma, nephroptosis and abnormalities of the kidneys and urinary tract, play an important role in the pathology of this disease.
One of the most important functions of the kidneys is to remove excess fluid from the body. Therefore, when kidney function is impaired, the body suffers from excess water: renal hypertension develops, since the arteries are filled with high levels; cardiac hypertrophy, as the heart has to work harder to pump a large volume of blood; swelling appears due to a decrease in proteins in the blood (low oncotic pressure of the blood (low protein), increased osmotic pressure (lots of salts)). Anemia develops.
There is a complex classification of types of glomerulonephritis. The clinical picture and severity of this disease depends on many factors. Your attending physician will tell you detailed information about your disease.
Read the book by Nikolai Albertovich Onuchin “Rehabilitation exercises for kidney diseases.”
Therapeutic exercise for glomerulonephritis.
prescribed by the doctor individually, taking into account all the characteristics of the patient at different stages of the disease, determining the activity mode (bed, ward, general).
We will talk about physical therapy for acute glomerulonephritis during the recovery stage and for chronic glomerulonephritis during remission.
Therapeutic exercises for glomerulonephritis are carried out with the aim of
- increase the body's defenses,
- adapt the body to physical activity,
- increase performance,
- help lower blood pressure and
- normalization of metabolism,
- improve blood circulation in the kidney tissue and urination,
- eliminate congestion in the lungs and other organs,
- promote normal bowel function,
- increase sweating and gas exchange,
- create a positive emotional mood for the patient.
We take into account the presence of arterial hypertension and the risk of myocardial infarction. Blood pressure control!
In a set of exercises for glomerulonephritis
- includes exercises in starting positions lying down, sitting on a chair and knee-wrist;
- exercises for glomerulonephritis are performed at a slow pace, movements are smooth with full amplitude,
- attention is focused on inhalation and exhalation,
- the load alternates between different muscle groups in order to redistribute blood and is performed on all muscle groups, especially the muscles of the back, abdominals, buttocks, and thighs.
- Lesson duration 25 - 30 minutes.
Note!
1). If glomerulonephritis is combined with nephroptosis, then you should perform the “Set of exercises for nephroptosis,” but not on a board installed at an angle of 300, but lying in a horizontal plane. 2). For arterial hypertension, place a pillow under your head when performing exercises while lying on your back to reduce the load on the blood vessels of the brain.
Exercises with glomerulonephritis can be performed only with the permission of a doctor, in satisfactory condition and with blood pressure within normal limits. Measure your blood pressure.
Do not start exercises if you feel unwell and tired, if your blood pressure has increased, swelling, pain, etc. Rotational movements of the hands and feet while lying on the bed and diaphragmatic breathing will be enough.
Keep a diary of how you feel, measure your pulse and blood pressure. Divide the sheet into two columns: “Before class” and “After class.” Measure your heart rate and blood pressure before class and write it down in the first column, noting how you feel (it should always be satisfactory before class!). Do the same after class.
If your health has worsened or you feel tired, then you need to reduce the load:
reduce the number of repetitions of exercises,
reduce the amount of exercise
select exercises in ref. lying on your back and stomach positions,
be sure to alternate between “hard” and “easy” exercises,
focus on breathing,
divide the set of exercises into two parts: one part in the morning, the other in the evening,
control the slow pace of exercise.
Development of the disease
Depending on which option, the form of glomerulonephritis predominates, different mechanisms of disease development are activated. But they all lead to kidney failure.
In patients, humoral immunity, which is provided by proteins dissolved in body fluids, is reduced. Allergens, or toxins, bind to these proteins rather than being eliminated through the kidneys. Large molecules are formed that settle on the walls of the glomeruli. Microcirculation suffers, ischemia is observed against the background of a perverted immune response - this is the main trigger for the development of glomerulonephritis. Further along the chain, phenomena such as:
- Renal ischemia is regarded by the body as a threat, since it is a vital organ. The main carrier of oxygen, hemoglobin is found in red blood cells. With hypoxia of the renal tissue, an increase in the number of red blood cells is observed. An excess of blood cells leads to a decrease in fluidity and an increase in blood viscosity. The blood supply to organs throughout the body begins to suffer. Secondary hypoxic changes develop.
- The body is trying to make the blood more fluid, to dilute it with liquid. This leads to sodium and water retention, and peripheral edema appears. The body's retention of sodium leads to loss of potassium and disruption of the heart. Excess sodium causes potassium deficiency. Without this microelement, the heart cannot work, which leads to catastrophically progressive heart failure.
- An increase in water in the body against the background of increased blood pressure causes tachycardia. In order to pump an excess amount of blood, the volume of the heart muscle increases - myocardial hypertrophy develops.
- The kidneys produce a substance that helps maintain normal blood pressure. Hypoxia leads to disruption of the production of this hormone. Patients have persistent arterial hypertension that cannot be treated with conventional antihypertensive drugs.
- Large molecules, which are a combination of blood proteins with allergens, settled in the glomerular apparatus of the kidneys, are regarded by the body as a threat that must be eliminated. A large number of leukocytes rush to the kidneys. The vascular endothelium is damaged. An inflammatory response is observed, manifested by a violation of the permeability of the capillary wall. The liquid part of the blood leaves the vascular bed, the body retains the liquid even more to make the blood fluid, and a vicious circle closes. Swelling, symptoms of respiratory failure, heart failure, and disruption of the endocrine system appear and increase.
- The formed elements of blood that clogged the glomerular apparatus gradually became sclerotic, the glomerulus was replaced by connective tissue. When this process affects more than 50% of the glomerular apparatus, glomerulonephritis is called diffuse.
Situational task about glomerulonephritis, Abstracts from Nephrology
You are a general practitioner at the State Public Hospital at the RV "City Clinic No. 4", Alina came to see you
Mikhailovna (33 years old) with complaints of weakness, fatigue and severe headache. The words
The patient had pharyngitis a week ago and thought it was because of the ice cream she had eaten.
I was actively treated for three days, then gave up due to problems at work. And now it seems to her that
She has a sore throat again and asks you to prescribe her pills. You in turn suggested it
inspect. During the physical examination, you noted: the condition is satisfactory, skin
the integument is pale, there is no edema. Vesicular breathing. Heart sounds are muffled and rhythmic. Heart rate
– 75 per minute, blood pressure – 125/100 mm Hg. Art. The abdomen is soft, painless in all parts. Liver and
the spleen is not enlarged. On palpation, regional lymph nodes are not enlarged, but
moderately painful. When examining the oral cavity, there is hyperemia and swelling of the mucous membrane
membranes of the pharynx. The symptom of effleurage is negative.
Your actions:
1. Prescribe treatment. Repeated appointment in a week.
If you chose step 1:
You prescribe her to drink plenty of fluids, rinse with chamomile 8 times a day, amoxiclav 625 mg, 1
tablet 2 times a day, and absorbable plates “Angal-S” 3 times a day.
A week later, Alina Mikhailovna comes to you complaining of severe headaches,
fatigue, weakness and pain in the lumbar region. She also notes that
a day after her visit to you, her urine color changed “like the color of meat slop”!!!!!
She was treated as you wrote to her. Now Alina Mikhailovna believes that you assigned her
the wrong pills aggravated her condition and that she will not come to you anymore. You'll see me in an hour
You are summoned to the chief doctor because a complaint has been received against you.
Unfortunately, you were fired.
2. Prescribe OAC, OAM and treatment. And a second appointment after the results come out
UAC and OAM.
If you chose step 2.
You prescribe her to drink plenty of fluids, rinse with chamomile 8 times a day, amoxiclav 625 mg, 1
tablet 2 times a day, and absorbable plates “Angal-S” 3 times a day. UAC and OAM.
A day later, Alina Mikhailovna comes to you with test results and complains about
headache, fatigue, weakness, pain in the lumbar region and change in urine color
“Like the color of meat slop.” You perform a physical examination: condition
satisfactory, pale skin, slight swelling. Vesicular breathing.
Heart sounds are muffled and rhythmic. Heart rate – 75 per minute, blood pressure – 142/100 mm Hg. Art. Belly is soft
painless in all departments. The liver and spleen are not enlarged. On palpation, regional
the lymph nodes are not enlarged, but moderately painful. When examining the oral cavity
there is hyperemia and swelling of the pharyngeal mucosa. Symptom of effleurage
positive. Then you look at the analysis data and conduct additional interviews.
CBC: erythrocytes – 3.5×1012/l, hemoglobin – 110g/l, leukocytes – 8.2×109/l, leukocyte
the formula has not been changed; platelets - 180×109 /l, ESR - 26 mm/hour.
OAM: relative density - 1014, yellow color, acidic reaction, protein - 0.88 g/l,
erythrocytes - 10-15 per field of view, acanthocytes 5%, leukocytes - 3-4 per field of view, epithelium
flat – single cells in the field of view, no bacteria.
Due to additional survey, you learned that Alina Mikhailovna had 2 more headaches
years ago. The appearance of headaches was associated with pharyngitis. At the same time,
Symptoms of glomerulonephritis.
Symptoms of glomerulonephritis will depend on the form of the disease, as well as the cause of the inflammation.
The first warning sign is abnormalities in urine tests (hematuria and increased protein content). So, symptoms include:
1. Hematuria – the appearance of red blood cells in the urine. There may be few of them, which is detected only by urine analysis. But with severe hematuria, the urine may turn pink or cola-colored (brown).
2. Proteinuria – increased content of proteins (proteins) in the urine. At low levels, protein is determined in the laboratory. If there is a significant protein content, the urine can be very foamy.
3. High blood pressure.
4. Fluid retention (edema).
5. Weakness and anemia.
Kidney development abnormalities
Pregnant women suffering from kidney disease require clinical observation by a antenatal clinic physician. This contributes to their systematic examination, early detection of complications and timely hospitalization. In addition to women diagnosed with kidney disease before pregnancy, the therapist registers pregnant women with suspected kidney disease.
These are women who during pregnancy were found to have proteinuria, hematuria, pyuria, increased blood pressure, edema (in the first half of pregnancy), as well as women who had gestosis, especially severe. After the examination, they are either removed from the register, or they continue to be monitored if kidney disease is established.
Every pregnant woman who has not previously had kidney disease should be under the strict supervision of an obstetrician during the so-called critical periods of pregnancy, especially at 22-28 weeks. During this period, pyelonephritis in pregnant women most often first appears. During the indicated periods of pregnancy, despite the absence of complaints, it is necessary to conduct a weekly urine test, culture it, and if the indicators deviate from the norm, carry out preventive measures aimed at preventing the development of pyelonephritis.
Thus, if there is an increased number of leukocytes in repeated urine tests (more than 6-8 in the field of view), especially if it has a neutral reaction, in which some of the leukocytes are destroyed, it is necessary to conduct a course of anti-inflammatory or antibacterial therapy with mandatory consideration of the gestational age and the characteristics of the urine microflora .
The same is done when bacteriuria is detected above 105 microbial bodies in 1 ml of urine (“asymptomatic bacteriuria”). The results of treatment are monitored by laboratory parameters. If there is no effect during outpatient treatment, such patients are subject to hospitalization in the second obstetric observation department of the maternity hospital.
The existing disease is judged on the basis of anamnesis, an extract from the outpatient card of the district clinic and the results of an examination carried out at the antenatal clinic. In table Table 5 shows the necessary studies that can be done at the antenatal clinic or district clinic.
Table 12
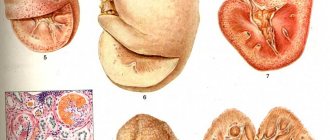
1. Anomalies of quantity: a) aplasia (agenesis) of the kidney - absence of a kidney; b) doubling of the kidney - complete doubling of the kidney (each half of the kidney has its own vessels, its own pelvis and ureter along its entire length; incomplete doubling (doubling of the parenchyma and vessels without doubling the pelvis); c) accessory kidney - this kidney is located below the normal one, has a separate blood supply and a separate ureter, no tissue connection with the normal kidney (Fig. 8-1).
2. Anomalies in size: a) renal hypoplasia - a decrease in the size of the kidney, but there are no structural changes in the kidney.
3. Anomalies of location (dystopia): a) thoracic dystopia of the kidney - location of the kidney in the chest; b) lumbar dystopia - the renal artery arises from the aorta at the level of the II-III lumbar vertebrae, the pelvis faces anteriorly; c) iliac dystopia - the kidney is located in the iliac fossa, the arteries are multiple, departing from the common iliac
Rice. 8-1. Option for localizing the accessory (third) kidney on the right
arteries; d) pelvic dystopia - the kidney is located deep in the pelvis, usually between the rectum and the bladder.
4. Anomalies of relationship (fusion): a) biscuit-shaped kidney - fusion of the kidneys along their medial surface; b) S – shaped or L-shaped kidney – fusion of the upper pole of one kidney with the lower pole of another kidney; c) horseshoe kidney - fusion of the kidneys with the same poles in 90% of cases, the lower ones (Fig. 8-2).
5. Structural anomalies: a) multicystic kidney – unilateral complete replacement of renal tissue with cysts and obliteration of the ureter in the pelvic region or the absence of its distal part; b) polycystic kidney disease - bilateral replacement of the kidney parenchyma with multiple cysts; c) simple (solitary) cyst - a single cystic formation that has a rounded shape on the surface of the kidney and can be localized in its various parts (Fig. 8-3); d) dermoid cyst - the cyst contains fat, hair, and sometimes teeth.
Rice. 8-2. Horseshoe kidney
1111 5
1 – intraparenchymal; 2 – cortical; 3 – peripelvic;
4 – multilocular; 5 – subcapsular; 6 – cortical infected.
Diagnosis of kidney development anomalies is carried out using ultrasound, X-ray CT, MRI and routine x-ray urological studies. The need for treatment arises in cases of development of diseases in the abnormal kidney or the occurrence of renal arterial hypertension.
1111 5
Acute cystitis.
Diagnosis of glomerulonephritis.
Specific signs allow the doctor to suspect glomerulonephritis, but the following methods can be used to confirm:
1. Urinalysis.
The analysis will show red blood cells and their fragments in the urine, white blood cells (an indicator of inflammation), and protein. These indicators indicate damage to the nephrons and deterioration of kidney function.
2. Blood test.
Blood tests will help reveal levels of waste products such as creatinine. When kidney function is impaired, the level of these substances in the blood is increased.
3. Kidney X-ray, ultrasound or computed tomography. If your doctor suspects kidney damage, he may order these tests to image the organ.
4. Kidney biopsy.
During this procedure, the doctor takes a sample of kidney tissue using a special needle. The biopsy is studied in the laboratory to determine the cause of the inflammation.
Complications of glomerulonephritis.
1. Acute renal failure.
Loss of the filtering ability of the kidneys leads to the accumulation of toxic metabolic products in the blood. This condition requires urgent dialysis.
2. Chronic renal failure.
This is a very serious complication - the kidneys gradually, irreversibly lose their filtering ability. A decrease in kidney function to 10% of normal is considered end-stage chronic renal failure, and requires dialysis or a transplant so that the patient can lead a normal life.
3. Hypertension.
Kidney damage leads to fluid accumulation and increased blood pressure. High blood pressure, in turn, damages the kidneys.
4. Nephrotic syndrome.
It is characterized by increased levels of protein in the urine, low levels of proteins in the blood plasma, swelling and other disorders.
Sample answers to problems
Task No. 1.
1. Acute glomerulonephritis occurs after bacterial, viral, fungal, and parasitic infections. The most common acute post-streptococcal glomerulonephritis is caused by nephritogenic strains of group A beta-hemolytic streptococcus.
2. Acute post-streptococcal glomerulonephritis is an immunologically caused disease, which is based on immune complex damage to the glomeruli of the kidneys. During the latent period, which takes from 1 to 4 weeks, antibodies against streptococcal antigens accumulate. Deposits of immune complexes are deposited subepithelially in the form of characteristic “humps” and in the mesangium. In the pathogenesis of glomerulonephritis, cross-reactivity between the antigens of glomeruli and streptococci, as well as damage to the structure of immunoglobulins by pathogen toxins, is important.
3. Oliguria (a decrease in the normal level of diuresis by 20-50%) occurs with glomerulonephritis due to a decrease in the number of functioning nephrons. In addition, intracapillary thrombi, swelling and proliferation of endothelium and mesangial cells lead to decreased filtration in functioning glomeruli. The influence of aldosterone, an antidiuretic hormone that has salt-retaining and antidiuretic effects, is also significant.
4. Hypersthenuria is explained by increased water reabsorption and proteinuria.
5. Hematuria in glomerulonephritis is explained by the following changes: increased permeability of the glomerular capillaries, up to perforation of the basement membranes; damage to the mesangium; involvement of the interstitium in the process.
6. Proteinuria is explained by an increase in the permeability of the basement membrane of the glomerular capillaries due to the loss of the negative charge of the glomerular filter.
7. The pathogenesis of edema consists of several pathophysiological mechanisms, which are activated in different sequences and have unequal degrees of significance. These include: 1) Generalized increase in the permeability of capillary walls; 2) secondary hyperaldosteronism; 3) increased secretion of antidiuretic hormone; 4) hypernatremia, hyperosmia, hypervolemia; 5) hypoproteinemia.
8. Microscopically, a diffuse increase in the size of the glomeruli, proliferation of endothelial and mesangial cells, infiltration of the glomeruli by neutrophils and monocytes, a sharp narrowing of the lumens of the capillaries, focal atrophy of the tubular epithelium, edema and lymphoid infiltration of the interstitium are detected.
9. Intracapillary proliferative glomerulonephritis.
10. The prognosis of acute post-streptococcal glomerulonephritis is generally favorable. More than 95% of children recover in childhood. The prognosis is more serious in adults than in children and adolescents. In adults, in 50% of cases, glomerulosclerosis progresses with the development of chronic renal failure.
Task No. 2.
1. Rapidly progressive glomerulonephritis, which is characterized by the rapid development of renal dysfunction and malignant arterial hypertension.
2. Rapidly progressive glomerulonephritis is divided into three groups: post-infectious (post-streptococcal); for systemic diseases; idiopathic.
3. The pathogenetic mechanisms of rapidly progressive glomerulonephritis are characterized by diversity. At 50 %
In cases of glomerulonephritis, immune complexes are detected, in approximately 30% - antibodies to the basement membrane of glomerular capillaries. In some patients, we can talk about a combination of immune complex and autoimmune glomerulonephritis.
4. A decrease in the glomerular filtration surface and an increase in water reabsorption due to secondary hyperaldosteronism, hypernatremia and increased ADH secretion.
5. The kidneys are enlarged in size, flabby consistency, the cortex is wide, grayish-yellowish in color with small red speckles, the medulla is dark red - “a large mottled kidney.”
6. In the extracapillary space, characteristic “crescents” are formed, initially formed mainly from cellular elements - monocytes, polynuclear leukocytes, podocytes, nephrothelium, fibrin, then transformed into fibrous-cellular and, finally, fibrous. The crescents compress the capillary glomerulus, in which necrotic changes progress. Phenomena of proliferation of endothelial and mesanial cells are observed. In the interstitium there is an inflammatory reaction.
7. Rapidly progressive glomerulonephritis is characterized by the development of extracapillary proliferative glomerulonephritis (glomerulonephritis with crescents).
8. The leading mechanism of hematuria in extracapillary glomerulonephritis should be considered perforation of the basement membranes of the glomerular capillaries.
9. The genesis of proteinuria is caused by an increase in the permeability of the basement membrane of the glomerular capillaries for protein molecules due to the deposition of immune complexes or autoantibodies in the glomerular filter. Of lesser importance is a decrease in protein reabsorption in the tubular part of the nephron.
10. In this observation, rapidly progressive glomerulonephritis is characterized by the development of the nephrotic variant of edematous syndrome. In this case, massive proteinuria occurs - more than 3 g of protein per day, peripheral edema is widespread, and ascites appears. Proteinuria leads to hypoproteinemia and hypoalbuminemia, which causes a decrease in oncotic, then osmotic pressure in the vascular bed with a subsequent decrease in circulating blood volume (CBV). In this disease, in parallel with these processes, various inflammatory mediators are activated, which increase the permeability of the vascular wall, which also helps to reduce the volume of blood volume. The decrease in BCC includes the system for maintaining intravascular volume, i.e., the secretion of aldosterone, activation of antidiuretic hormone, and suppression of atrial natriuretic factor.
11. Renovascular (ischemia of the glomeruli of the kidney), secondary hyperaldosteronism.
Task No. 3.
1. Secondary nephrotic syndrome. A patient with rheumatoid arthritis developed AA amyloidosis with kidney damage, which is clinically manifested by proteinuria, hypo- and dysproteinemia, hyperlipidemia, hypercholesterolemia, and edema.
2. The kidneys are almost always affected by systemic amyloidosis. Increased levels of serum SAA protein promote the deposition of amyloid masses in nephron structures, with the glomeruli being primarily affected. As a result, the permeability of the glomerular filter increases and proteinuria occurs.
3. During the development of amyloid nephropathy, several successive stages are distinguished: latent, proteinuric, nephrotic, azotemic. The increase in proteinuria corresponds to the volume of amyloid deposits in the kidney structures. In the nephrotic stage of amyloid nephropathy, proteinuria is explained, on the one hand, by damage to the glomerular filter, and on the other, by depletion of the reabsorption resource of the tubular epithelium.
4. There are two mechanisms leading to hyperlipidemia and hypercholesterolemia. The first mechanism is associated with increased synthesis of lipoprotein apoprotein precursors in the liver, as a result of which accumulation of lipoproteins is observed, the second is with impaired metabolism of already synthesized lipoproteins due to a decrease in the activity of lipoprotein lipase and lecithin choline acyltransferase.
5. Oncotic, endocrine-renal, osmotic.
6. The kidneys are large, dense, gray-pink in color, waxy, the border between the cortex and medulla is erased (large white kidney).
7. Amyloid is deposited in the capillary loops of most glomeruli, mesangium, in the wall of extraglomerular arteries and arterioles, in the tubular membrane, and in the interstitium.
8. Congo red staining with further examination of the stained preparations in polarized light. In this case, amyloid gives a greenish glow. In addition, to clarify the type of amyloid, it is necessary to use IHC research.
9. In general, the prognosis is favorable. After the development of chronic renal failure, patients die within a year.
Clinical picture
At first, patients only experience increased fatigue, dry hair, and brittle nails. Associating this condition more often with hypovitaminosis, they begin to take medications, vitamin supplements, and even greater impairment of kidney function is observed.
The developed clinical picture is characterized by the appearance of:
- decreased appetite;
- weakness, malaise;
- changes in laboratory data - protein, blood, leukocytes, casts in urine tests. The density of urine increases due to the large amount of protein. Reduced protein amount and dysproteinemia, lipidemia, hypercholesterolemia;
- a tendency to increase blood clotting more often leads to the formation of blood clots of any location;
- swelling;
- disruption of the heart leads to heart failure;
- the functions of the pancreas, thyroid gland, and adrenal glands are affected.
Complications of symptoms included in nephrotic syndrome:
- As fluid retention progresses, edema increases, water accumulates in the abdominal cavity - ascites, in the pleural cavity - hydrothorax, and in the pericardial cavity - hydropericardium.
- Edema of the lungs, brain, retina.
- Thrombosis, thromboembolism.
- Ischemic heart disease, myocardial infarction.
- Stroke.
- As a result of a decrease in the volume of circulating blood, its accumulation in peripheral tissues, and protein deficiency, hypovolemic edema develops - a life-threatening condition.
- The addition of infection causes peritonitis, pleurisy, pneumonia, and pleural empyema.
Clinical picture of nephritic syndrome
With a rapidly progressing process, in response to inflammatory changes of a non-bacterial nature, various combinations of specific, nonspecific symptoms of nephritic syndrome develop. Specific symptoms include:
- the appearance of blood in urine tests;
- increased blood pressure;
- decrease in the amount of urine excreted per day;
- swelling;
- changes in immunological blood parameters.
Non-specific symptoms are often characterized by nausea, vomiting, and malaise.
Treatment of glomerulonephritis.
The main goal of treatment is to prevent further kidney damage.
Treatment of glomerulonephritis and its outcome depend on the following factors:
1. Form of the disease (acute or chronic). 2. The disease that caused glomerulonephritis. 3. The severity of the disease.
Some cases of glomerulonephritis may resolve on their own without any treatment. This is especially true for post-streptococcal glomerulonephritis.
Treatment of arterial hypertension.
Pressure control is the most important measure to protect the patient's kidneys.
To do this, the doctor may prescribe drugs from different pharmacological groups. Most often these are the following groups:
1. Diuretics, in particular thiazide diuretics (hydrochlorothiazide). 2. ACE inhibitors (enalapril, ramipril, perindopril, fosinopril, etc.) 3. AT-II receptor antagonists (losartan, valsartan, etc.)
It is strictly forbidden to arbitrarily choose antihypertensive drugs. The choice of a specific pharmacological group depends on many factors - this is described in special manuals for doctors, and only a doctor can choose the drug correctly.
Treatment of the primary disease.
If glomerulonephritis was caused by any disease, the doctor will need to prescribe appropriate treatment:
1. Bacterial infection: treatment with antibiotics.
2. Lupus or vasculitis: Corticosteroid hormones are usually used to suppress the immune response and inflammation.
3. Berger's disease: immunosuppressants and drugs with omega-3 fatty acids.
4. Goodpasture syndrome: Plasmapheresis, a mechanical process by which antibodies are removed from the blood plasma and the patient is given donor plasma or other replacement fluid, is sometimes prescribed.
Treatment of kidney failure.
In acute renal failure, dialysis is used - artificial blood purification using a special device.
For end-stage renal failure, the only treatment options are dialysis and kidney transplantation. If a transplant is not possible due to health reasons, then permanent dialysis remains the only option.
Advice for patients.
In addition to traditional treatment, your doctor may recommend making some changes to your daily life and diet:
1. Limit salt intake in food. This will minimize fluid retention, swelling and hypertension. 2. Reduce potassium and protein intake to slow down the accumulation of toxic waste products in the blood. 3. Monitor blood sugar levels. 4. Maintain a healthy body weight.