A timely and correct diagnosis is half of successful treatment. If the classic course of glomerulonephritis - glomerular inflammation of the kidneys - has its own striking characteristic features, then latent forms of the disease can imitate a variety of pathologies. In order for the doctor to make the correct diagnosis, the patient must undergo a comprehensive clinical, laboratory and instrumental examination.
What is glomerulonephritis
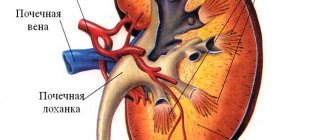
Glomerulonephritis is a collection of various kidney diseases, which are united by the fact that the glomerular apparatus is damaged.
Regardless of the cause of the pathology, the immune system actively participates in the process. Specific forms of antibodies, proteins of the complement system and cytotoxic cells appear that affect the epithelial wall of the glomerular apparatus. This leads to a disruption of the filtration function, due to which protein molecules and even blood cells (mainly red blood cells) enter the primary urine. Usually this disease is a bilateral process - both organs are affected. That is why, without proper diagnosis and treatment, the symptoms of renal failure quickly develop.
International recommendations now include glomerulonephritis in chronic kidney disease. This allows you to more clearly determine the degree of renal failure and select the most effective strategy for managing the patient.
Diagnostics
Reasons for examination for glomerulonephritis: the appearance of edema, blood in the urine, pressure that cannot be reduced.
The urologist prescribes:
- Ultrasound of the kidneys
. In an acute condition, ultrasound shows thickening of the epithelial cells of the kidneys, an unclear outline, increased echogenicity, and a change in the vascular pattern. To determine the chronic form of glomerulonephritis, ultrasound diagnostics are not always informative, although a characteristic symptom is often observed - a change in kidney volume. In any case, an ultrasound is necessarily performed to exclude other diseases. - Blood test for antistreptococcal antibodies
. The latent form of the disease is determined by the high concentration of complement and IgA in the blood serum. - Blood chemistry.
Total protein in the blood serum is reduced. The proteinogram indicates an increase in the amount of a1 and a2 globulins. Azotemia, the presence of urea, cholesterol, and creatine in large quantities is detected in the blood. - General urine analysis, urine samples according to Zimnitsky, Reberg, determination of daily protein loss.
Analyzes show low urine volume, increased frequency of night urination, against the background of a decrease in daytime urination. Blood and protein are found in the urine (depending on the form of the pathology). In chronic GN, a general urine test reveals leukocytes, red blood cells, and casts. - Excretory urography
. This is an x-ray using contrast fluids to show the vessels, canals and cavities in the kidneys. - Kidney biopsy
. The most accurate diagnostic measure in which the kidney tissue is examined directly.
To make a diagnosis and successfully treat glomerulonephritis, the urologist needs data from the entire range of studies.
Cost of urologist services at the University Clinic
| Service | price, rub. |
| Appointment (examination, consultation) with a urologist with the highest qualification category. | 1700 |
| Obtaining a urological smear | 350 |
| Laser removal of single papillomas and condylomas, up to 3 pcs. | 4000 |
Second stage: laboratory tests
If glomerulonephritis is suspected, the following laboratory methods are prescribed:
- general blood analysis;
- blood chemistry;
- clinical urine analysis;
- tests according to Nechiporenko, Zimnitsky, Reberg - according to indications;
- allergy tests;
- immunological blood test.
The results of the CBC of patients with glomerulonephritis show signs of acute inflammation - leukocytosis and accelerated ESR. Also noteworthy are the manifestations of anemia - a decrease in the level of red blood cells (erythrocytes) and hemoglobin.
Biochemistry is accompanied by hypoproteinemia (a decrease in the level of total protein and albumin against the background of an increase in globulins). With the development of renal failure, the level of urea and creatinine progressively increases.
A general urine test is the most important laboratory method in diagnosing exacerbations of glomerulonephritis. The following pathological changes are observed in it:
- increase in relative density of urine;
- color change;
- proteinuria – from microalbuminuria to massive protein excretion in the urine (3 g/day or more);
- hematuria, erythrocyturia.
Immunological examination and allergy tests can identify various disorders in the functioning of the body's defense system and confirm the autoimmune nature of the disease.
Causes of development of glomerulonephritis
Among the reasons for the development of this pathology, it is necessary to highlight the following:
- genetic predisposition of patients (carriage of the genes NPHS, ACTN4, INF2 and others);
- previous bacterial infections where the causative agents were staphylococcus or streptococcus (tonsillitis, pharyngitis, furunculosis, infective endocarditis);
- long-term use of nephrotoxic medications (penicillamine, interferon, gold preparations, anabolic steroids);
- viral infectious processes that lead to disruption of the functioning of the immune system (hepatitis, herpes viruses, parvoviruses);
- systemic autoimmune processes that are accompanied by damage to the glomerular system of the kidneys (lupus, vasculitis, Wegener's granulomatosis);
- ingestion of toxic substances from a polluted environment into the body;
- injection drug use;
- development of oncological or hematological pathologies.
Risk group
Acute glomerulonephritis affects people of any age, but the disease is more common in young patients under 40 years of age. The disease ranks 2nd among complications of urinary tract infections in children.
According to statistics, glomerulonephritis is the most common cause of early disability due to the development of renal failure.
The disease is especially severe in pregnant women. Since during pregnancy the urinary system bears an increased load, women planning to have a child are recommended to undergo an ultrasound of the kidneys to exclude hidden nephritis.
Forms of glomerulonephritis
The modern classification of glomerulonephritis is based not on the clinical picture, but on data from a kidney biopsy followed by cytological examination. This is what made it possible to identify the following forms of the disease:
- Berger's disease (IgA nephropathy). Specific antibodies Gd-IgA1 appear in the blood, which affect the glomerular membranes of the kidneys.
- Glomerulonephritis with minimal morphological changes. The biopsy shows virtually no abnormalities. It is considered the most benign form of the disease. Occurs in children.
- Thin basement membrane syndrome . The key clinical symptom is the development of mass hematuria (a large number of red blood cells in the urine)
- Alport syndrome is a congenital form of the disease. In addition to kidney damage, problems with vision and hearing can also be found.
- Postinfectious glomerular nephritis. Occurs several weeks after a staphylococcal or streptococcal infection.
- Rapidly progressive type . Prognostically unfavorable form of pathology. The biopsy specimen reveals “crescent” cells. Kidney failure develops quickly.
- Focal segmental glomerulonephritis . Characteristic of this form is the development of processes of replacement of the glomeruli with connective tissue (nephrosclerosis).
- Membranous glomerulonephritis. Serious changes in the structure of glomerular membranes with functional changes occur.
- Membranoproliferative GN. Active proliferation of the epithelium is observed, which gradually reduces its permeability.
- C3 glomeropathy . A special form of pathology in which the C3 protein of the complement system affects the glomerular apparatus of the kidneys.
Third stage: instrumental examination methods
Instrumental tests allow you to confirm the doctor’s assumptions, determine the morphological form, features of the course of glomerular inflammation and make a clinical diagnosis.
Kidney ultrasound is an effective, safe and non-invasive method for diagnosing diseases of internal organs. Acute or chronic glomerulonephritis has the following signs on ultrasound:
- the kidneys acquire blurry, indistinct contours;
- bilateral thickening of the parenchyma (functional layer);
- increased echogenicity, heterogeneity of the structure of the renal tissues: both hypo- and hyperechoic foci (“pyramids”) appear.
Ultrasound examination of blood flow (Dopplerography) shows a decrease in vascular resistance in the arcuate (arc) arteries. At the same time, blood flow in segmental and interlobar vessels can remain normal.
Confirming the diagnosis and determining the nature of changes in tissues can only be done with the help of a morphological study. The role of kidney biopsy is especially important in chronic glomerulonephritis.
The diagnostic procedure is a minimally invasive surgical procedure and is performed only in a hospital setting. Under local anesthesia, the surgeon inserts a thin, hollow needle through the skin of the lower back, capturing a small piece of kidney tissue. Then microslides are prepared from the resulting biomaterial, which a cytologist carefully examines under a microscope. The obtained histological examination data reflect the morphological features of inflammation, make it possible to determine the type of glomerulonephritis (for example, membranous, mesangioproliferative, mesangial, etc.) and even make a prognosis of the disease.
If complications develop, the diagnostic plan may include additional laboratory and instrumental tests.
With the help of a timely comprehensive examination, it is possible to diagnose glomerulonephritis at an early stage, and begin treatment of the disease before irreversible changes occur in the kidney tissues. This will allow you to quickly get rid of unpleasant symptoms, avoid the development of complications and achieve a full recovery.
Three classic symptoms will appear: swelling, reddish urine and increased blood pressure, which may be accompanied by a headache or not bother the patient, determined only by measurement. The first appearance of these symptoms in young people is likely to lead to a diagnosis of acute glomerulonephritis. In old age, these changes in most cases will be attributed to primary chronic glomerulonephritis. Chronic glomerulonephritis is also diagnosed when acute glomerulonephritis exists within 12 months from the onset of the disease.
The diagnosis of rapidly progressive glomerulonephritis is usually made if, just a month and a half after the onset of the acute process, the density of urine decreases, nephrotic syndrome develops and blood pressure rises. This is accompanied by an increase in urea and creatinine in the blood.
Urine and blood tests and, if necessary, a kidney biopsy help confirm the diagnosis of glomerulonephritis. A general urine test reveals protein, a large number of red blood cells, and casts (casts of the renal tubules). A biochemical blood test for glomerulonephritis shows a decrease in total protein and an increase in its individual types.
Dr. Lerner offers personalized. In St. Petersburg, it is possible to call a doctor at home. We send herbal medicines to other cities by mail.
Ask your question to the doctor.
Kidney failure and other kidney problems are often detected through a standard urine test. A blood test may also be added to laboratory diagnostics. More complex instrumental diagnostic methods are used only to track the dynamics of changes in the structure of the kidneys. So, for example, glomerulonephritis on ultrasound, depending on the form of the pathology, may not give visible changes at all. Below you can find out how the pathology is formed and what is visible during ultrasound examination.
Urine tests
The main methods for diagnosing glomerulonephritis are urine tests. To confirm the diagnosis and assess the performance of the kidneys, the following types of tests are prescribed:
- Types and classification of glomerulonephritis: causes and prevention
- General urine analysis - allows you to identify deviations in chemical parameters.
- Zimnitsky's test - reveals the concentration, excretory and functional properties of the kidneys.
- Research using the Nechiporenko method - determines quantitative indicators of leukocytes, erythrocytes and cylindrical bodies.
- Reberg's test - evaluates the glomerular filtration rate and excretory capacity of the kidneys. Used for differential diagnosis of renal tissue damage.
- Micro-examination of sediment - determines the presence of cellular components of blood, epithelium, salts and casts.
- Bakposev - reveals the presence of staphylococci and other bacteria and their sensitivity to antibiotics.
In 50% of patients with acute glomerulonephritis, increased levels of protein, leukocytes and cylindrical bodies are detected in the urine. Less commonly, the epithelium of renal tissue. With glomerulonephritis, deformed red blood cells are also detected in the urine, which indicates a decrease in glomerular filtration. With a normal form of red blood cells, the diagnosis of glomerulonephritis may be erroneous.
Let's consider what changes in urine are detected during the acute course of the disease:
- Oliguria – increased density and decreased total volume of urine excreted.
- Proteinuria is an increase in the amount of protein; indicators can range from 3 to 30 g/liter.
- Presence of blood in the urine: microhematuria - more than 3 red blood cells are observed in the field of view, macrohematuria - a large number of red blood cells, sometimes in the form of clots, and the color of the urine becomes bright red.
- Reduced amylase may indicate the development of renal failure and the presence of diabetes mellitus.
- Bacteriuria is the presence of pathogenic microorganisms. In diffuse glomerulonephritis, bacteria are absent.
With this diagnosis, urine results may remain unchanged for a long period.
The chronic form of glomerulonephritis is characterized by the following features:
- The urine becomes a little cloudier and begins to foam when excreted. The density of urine decreases.
- The volume of daily diuresis increases to more than 3 liters per day, with a predominance at night.
- The amount of protein increases to 20 g/liter; as the disease progresses, proteinuria increases.
- In rare cases, red blood cells are found in the urine.
- Analyzes show the presence of casts and fibrin threads in urine.
Urinalysis for glomerulonephritis is of great importance. It is recommended to conduct longitudinal studies to assess the development of the disease, determine the effectiveness of treatment and prevent renal failure.
Basic Research
The first visual examination of the patient is aimed at determining external symptoms. Next, the doctor determines the presence of recent infectious diseases and measures blood pressure.
The symptoms of glomerulonephritis have many similarities with acute pyelonephritis, so the doctor always refers the patient to diagnostic procedures.
The patient is examined in the clinic, after which he is admitted to the hospital. The attending physician places him on bed rest and prescribes a strict diet. When conducting medical examinations, doctors often, after patients undergo laboratory tests, discover that they have glomerulonephritis, which occurs without characteristic symptoms.
Urine tests
To formulate a correct diagnosis, laboratory tests are required. Examinations for glomerulonephritis include a dynamic study of the composition of urine. Such examinations give a correct picture of the changes and course of the inflammatory process. A general urine test is prescribed, according to Nechiporenko and the Kakovsky-Addis method. Characteristic signs of the disease are:
- oliguria – decrease in urine volume;
- hematuria - an increase in blood cells in the urine;
- proteinuria – increased content of protein compounds in urine.
Glomerulonephritis always occurs with proteinuria, which is typical when filtration in the kidneys is impaired. Diagnosing hematuria is important. It occurs as a result of inflammation of the glomeruli and, along with proteinuria, most qualitatively reflects the course of the disease and the dynamics of recovery. These symptoms indicate the persistence of the inflammatory process. On the 3rd day, oliguria can be observed, which is subsequently replaced by polyuria. If this symptom persists for more than 6 days, the patient’s life may be in danger.
Clinical picture of glomerulonephritis
Severe clinical symptoms depend on the form of the disease. However, it is customary to distinguish several groups of leading syndromes that occur most frequently:
- Kidney failure. Accompanied by a decrease in the volume of daily urine, the development of peripheral edema (as well as ascites, hydrothorax or anasarca), severe intoxication and secondary damage to other organs and systems.
- Arterial hypertension. Due to disruption of the functioning of the renin-aldosterone system, an increase in blood pressure occurs, which is difficult to respond to drug therapy.
- Dysuric phenomena. This includes changes in urine color, consistency, and frequency of urination.
- Inflammatory phenomena. Possible increase in body temperature (especially against the background of bacterial infections).
- Severe aplastic anemia.
- Symptoms of electrolyte disturbances (cardiac arrhythmias, muscle weakness, cramps).
What is important to know about the disease can be learned from this video.
First stage: conversation and clinical examination
The first thing a patient’s examination begins with is the collection of complaints and anamnesis. Most often the patient is concerned about:
- unstable increase in blood pressure (mainly due to the diastolic component);
- headaches, attacks of dizziness;
- flickering of flies before the eyes;
- noise, ringing in the ears;
- decrease in the number and volume of urination (oliguria, anuria);
- change in urine color: it becomes dirty brown, rusty in color (the color of “meat slop”);
- constant feeling of thirst;
- the appearance of edema, first on the face and upper body, then spreading to the chest and abdominal cavity (hydrothorax, anasarca);
- dull aching pain, discomfort in the lumbar region;
- increase in body temperature to 38.5-39°C;
- signs of intoxication - fatigue, weakness, loss of appetite.
Possible glomerulonephritis is also indicated by a recent bacterial (angina, acute rheumatic fever) or viral infection, vaccination, or interaction with toxic substances.
Then the doctor conducts a clinical examination, including an assessment of the patient’s habitus (the patient’s appearance), palpation and percussion of the kidneys, auscultation of the heart, lungs and blood pressure measurement. Objective signs of glomerulonephritis can be considered swelling (the favorite localization is the eyelids), pain on palpation of the kidneys, a weakly positive Pasternatsky sign, and hypertension.
Based on the data obtained, the specialist makes a preliminary diagnosis and draws up a plan for further examination. Differential diagnosis of glomerular inflammation is carried out with pyelonephritis, amyloidosis, urolithiasis, tuberculous changes and tumors in the kidneys.
Glomerulonephritis: general picture of the disease and causes of its occurrence
Glomerulonephritis is a disorder of the glomerular filtration glomeruli in the kidneys.
Glomerulonephritis is a disorder of the glomerular filtration glomeruli in the kidneys. In this case, as a rule, both kidneys are affected at once. As a result of decreased glomerular performance, urine volume and quality decrease. That is, kidney failure develops.
Most often, the onset of the disease is caused by infectious diseases such as tonsillitis, scarlet fever, tonsillitis or purulent skin infection. In all these cases, the causative agent is streptococcal bacteria. The process of onset of glomerulonephritis in this case looks like this:
- The patient suffers from the above infections. After 10-14 days, visible complete recovery occurs.
- However, during the period of illness, the human body begins an internal struggle, which is expressed in an allergic reaction. As a result, antibodies are produced, which subsequently bind pathogenic microbial cells and carry them throughout the body along with the bloodstream.
- Next, the associated bacterial cells settle in the glomerular apparatus of the kidneys, which are responsible for filtering the blood. Thus, glomerulonephritis begins.
In addition, the causes of the onset of the disease can be:
- Acute glomerulonephritis with nephrotic syndrome
Recommended reading:
Symptoms of drug-induced kidney damage and treatment
- Banal and prolonged hypothermia in water;
- Past illnesses such as malaria or tuberculosis;
- Also, vaccination can be a provocateur of glomerulonephritis (if the body is weakened);
- An allergic reaction to certain groups of medications or toxins that have entered the body.
Recommendations for patients with glomerulonephritis
In order to completely recover from the disease, you must strictly adhere to all the recommendations of the attending physician.
To completely recover from the disease, you must strictly adhere to all the recommendations of the attending physician. Because often it is diet therapy and bed rest for 2-5 weeks that are the key to successful treatment. Drug therapy in this case relieves only the symptoms of the disease (normalizes blood pressure, reduces swelling, increases urine volume).
After successful treatment, patients who have suffered glomerulonephritis are contraindicated for at least two years from active sports, heavy physical labor, hypothermia and overheating, swimming in ponds and working with chemicals. If possible, sanatorium-resort treatment is indicated.
Source: LecheniePochki.ru
Treatment of glomerulonephritis in adults
The symptoms and treatment of glomerulonephritis in women and men are no different. Therapy involves a large range of measures:
- Elimination of foci of infection.
Treatment of teeth affected by caries and chronic sinusitis, excision of enlarged tonsils and adenoids. - Antibiotics
. The selection of medications is carried out after analyzing the data from the tests performed. Antibiotics treat only bacterial forms of pathology. Treatment of acute glomerulonephritis is often carried out with Amoxiclav and other penicillin drugs.
- Nonsteroidal anti-inflammatory drugs
. To improve the condition of the kidneys, a course of indomethacin or ibuprofen is prescribed with a gradual increase in dosage. - Immunosuppressants
. All forms of the disease require a decrease in the activity of the immune response. Steroid and cytostatic drugs are prescribed to suppress the degradation process in the glomeruli. The drugs have side effects, so the dosage of the drugs is carefully selected. Modern immunosuppressants: tacrolimus, mycophenolate mofetil, cyclosporine, rituximab. - Reduced pressure.
Kidney failure is a symptom of chronic glomerulonephritis. Hypertension becomes a consequence of impaired diuresis, edema, and hormonal disorders. Treatment of adult patients is carried out with the following drugs: Captopril, Enalapril, Ramipril. - Diuretic therapy
. To remove sodium, reduce blood pressure, and restore urine excretion functions, diuretics are used: Furosemide, Verapamil, Eufillin, Hypothiazide. - Anticoagulants, antiplatelet agents
. It is important to improve hematopoiesis, fluidity, and prevent the formation of blood clots. Based on these tests, the doctor chooses Heparin, Dipyridamole. - Diet
. Glomerulonephritis must be treated by following diet No. 7. Salt is excluded from the diet, and liquid drinking is limited. It is important to eat foods high in calcium and vegetable fats. - Mode.
You need to stay in bed and don't get nervous. Patients are strongly recommended to undergo sanatorium-resort treatment in a warm, dry climate and sunbathing. - Physiotherapy
. Physiotherapeutic treatment is included in the general range of prescriptions, but is not an independent method. The therapeutic complex includes treatment with electromagnetic fields, dry heat, and herbal medicine. Such measures for glomerulonephritis restore the ability of glomeruli to filter, normalize blood pressure, and relieve swelling. - Alternative medicine
. You can’t even try to fight such a dangerous disease using traditional methods. But recipes aimed at strengthening the immune system are acceptable. A urologist should select acceptable herbal preparations.
What is glomerulonephritis
Glomerulonephritis (GN) is an inflammation of the kidneys that affects the glomeruli (glomeruli), tubules and interstitial (connective) tissue of the kidneys. This is an immune disease, so it is very difficult to treat.
glomerulonephritis
» data-medium-file=»//i2.wp.com/medcentr-diana-spb.ru/wp-content/uploads/2017/09/glomerulonefrit.png?fit=450%2C300&ssl=1?v=1572898626″ data-large-file=”//i2.wp.com/medcentr-diana-spb.ru/wp-content/uploads/2017/09/glomerulonefrit.png?fit=827%2C550&ssl=1?v=1572898626″ class =»alignnone wp-image-7210 size-full» src=»https://i2.wp.com/medcentr-diana-spb.ru/wp-content/uploads/2017/09/glomerulonefrit.png?resize=898 %2C597″ alt=”glomerulonephritis” srcset=”//i2.wp.com/medcentr-diana-spb.ru/wp-content/uploads/2017/09/glomerulonefrit.png?w=898&ssl=1 898w, // i2.wp.com/medcentr-diana-spb.ru/wp-content/uploads/2017/09/glomerulonefrit.png?w=450&ssl=1 450w, //i2.wp.com/medcentr-diana-spb.ru /wp-content/uploads/2017/09/glomerulonefrit.png?w=768&ssl=1 768w, //i2.wp.com/medcentr-diana-spb.ru/wp-content/uploads/2017/09/glomerulonefrit. png?w=827&ssl=1 827w" sizes="(max-width: 898px) 100vw, 898px" data-recalc-dims="1″ />
Glomerulonephritis can be an independent disease or associated with systemic diseases - infective endocarditis, hemorrhagic vasculitis, lupus erythematosus, etc.
The disease remains asymptomatic for a long time. When the patient realizes that something is wrong with the kidneys and consults a doctor, it turns out that the affected organs cannot cope with their function. The situation leads to disability, condemning a person to lifelong attachment to an artificial kidney machine or to waiting for a donor for an organ transplant. This can be avoided if, after an infection, you visit a urologist, get tested and have an ultrasound of your kidneys.
Symptoms
The danger of glomerulonephritis lies in disorders of the renal glomeruli - glomeruli. This entails: weak glomerular filtration due to a decrease in its rate, the appearance of blood and protein in the urine, and a decrease in the volume of urination.
In adults, the disease occurs latently (hidden), changes in the quality and quantity of urine are possible. A blurred clinical picture, unnoticed by the patient, leads to a chronic form. If the disease has been diagnosed and drug therapy has been administered, the acute form can be cured in 2-3 months.
In children, the symptoms are striking, in 85% of cases there are disturbances in the vascular system and in the functioning of the heart.
Ultrasound diagnosis of glomerulonephritis
An ultrasound examination, as a rule, is not a particularly informative diagnostic method.
An ultrasound examination, as a rule, is not a particularly informative diagnostic method. In this case, it is only possible to identify structural changes in the kidneys and their location. It is worth knowing that if glomerulonephritis is in a chronic form, then the specialist will not see any special changes on ultrasound. The structure of the kidneys and their shape will remain unchanged.
Recommended reading:
Causes of prolapsed kidney: symptoms and treatment
If glomerulonephritis is in an acute form, then the following changes can be noted on an ultrasound of the kidneys:
- Rapidly progressive glomerulonephritis and its classification
- Thickening of the parenchyma of both kidneys;
- Change in the contours of the kidneys to unclear;
- It is also possible to detect increased echogenicity, and against its background the presence of hypoechoic pyramids may be noted;
- Also, if ultrasound angiography is performed, the vascular pattern will be combined;
- If Doppler sonography is performed, then a reduced peripheral resistance index will be noted in the arcuate arteries. At the same time, in the segmental and interlobar arteries the resistance index values will be normal.
Important: the nephrologist uses all the data obtained to prescribe the most effective treatment for glomerulonephritis.
Other research methods
It is permissible to carry out special instrumental diagnostics. Inspection with the help of technical devices greatly simplifies the placement, especially in young children. For a more detailed study of the course of the disease, its treatment and determination of the onset of consequences dangerous to the patient’s health, various technical tools are used: endoscopy, X-rays, computed tomography and ultrasound radiation.
Blood analysis
Using a blood test, you can determine the level of nitrogen in protein compounds. The composition begins to change if the amount of water increases. To exclude the diagnosis of acute pyelonephritis, a special immunological test is used to determine the true cause of the disease. It is two-level - the first helps to identify disorders in the body’s immune system, and the second helps to identify changes.
Differential diagnosis
Diagnosis of differential is based on study using the exclusion method. The presence of symptoms and laboratory tests allows you to compare data using logical analysis algorithms and separate diseases with similar characteristics. Glomerulonephritis is similar in its symptoms to many kidney diseases. This is the difficulty of determining by differential diagnosis. By exclusion, tuberculosis, pyelonephritis, kidney tumor and nephropathy must be excluded.
Ultrasound
The diagnosis of glomerulonephritis using ultrasound is quite easy to distinguish from other diseases by some specific signs: changes in the tubules and connective tissues, tissue thickening, diffuse transformations of the glomeruli, increased volume. A characteristic sign is also the accumulation of excess fluid in the internal organs, which confirms the diagnosis.
It is possible to overcome severe kidney diseases!
If the following symptoms are familiar to you firsthand:
- constant lower back pain;
- difficulty urinating;
- blood pressure disorder.
The only way is surgery? Wait, and do not act with radical methods. It is POSSIBLE to cure the disease! Follow the link and find out how the Specialist recommends treating...
A timely and correct diagnosis is half of successful treatment. If the classic course of glomerulonephritis - glomerular inflammation of the kidneys - has its own striking characteristic features, then latent forms of the disease can imitate a variety of pathologies. In order for the doctor to make the correct diagnosis, the patient must undergo a comprehensive clinical, laboratory and instrumental examination.
Why does glomerulonephritis occur: there are many reasons
The cause of glomerulonephritis is acute or chronic streptococcal and other infections: ARVI, pneumonia, measles, tonsillitis, scarlet fever, tonsillitis, streptoderma (skin infection), chicken pox. If the primary infection is supplemented by hypothermia or exposure to a damp climate (trench nephritis), then the likelihood of a severe complication increases several times. This is due to a failure of immunological reactions, leading to impaired blood supply to the kidneys.
Urologists note a connection between glomerulonephritis and toxoplasmosis (Toxoplasma gondii), meningitis (Neisseria meningitidis), and staphylococcus (Staphylococcus aureus). After an outbreak of streptococcal infection, glomerulonephritis occurs within 1-3 weeks in 10-15% of patients. It is especially often caused by nephritogenic strains of b-hemolytic streptococcus A.
In response to the introduction of foreign microorganisms into the body, the body produces substances to destroy them. But sometimes, for unknown reasons, the immune system malfunctions, attacking kidney cells with foreign substances. An inflammatory process occurs, accompanied by tissue damage and impaired urine filtration. Microscopic blood clots form inside the renal vessels.
Blood appears in the urine (hematuria). Sometimes there is so much of it that the urine looks like meat slop. But more often, little blood is released, and it can only be detected using laboratory methods.
Glomerulonephritis: you have had an infection - check your kidneys urgently
Doctors have a saying that “jade doesn’t hurt.” Unfortunately, kidney diseases, which are often complications of acute respiratory viral infections, tonsillitis, scarlet fever, and other infections, are mild or asymptomatic. Glomerulonephritis is especially dangerous - glomerular nephritis, leading to disability.
CLICK TO MAKE AN APPOINTMENT or ultrasound tests
Risk group
Acute glomerulonephritis affects people of any age, but the disease is more common in young patients under 40 years of age. The disease ranks 2nd among complications of urinary tract infections in children.
According to statistics, glomerulonephritis is the most common cause of early disability due to the development of renal failure.
The disease is especially severe in pregnant women. Since during pregnancy the urinary system bears an increased load, women planning to have a child are recommended to undergo an ultrasound of the kidneys to exclude hidden nephritis.
Why does glomerulonephritis occur: there are many reasons
The cause of glomerulonephritis is acute or chronic streptococcal and other infections: ARVI, pneumonia, measles, tonsillitis, scarlet fever, tonsillitis, streptoderma (skin infection), chicken pox.
If the primary infection is supplemented by hypothermia or exposure to a damp climate (trench nephritis), then the likelihood of a severe complication increases several times.
This is due to a failure of immunological reactions, leading to impaired blood supply to the kidneys.
Urologists note a connection between glomerulonephritis and toxoplasmosis (Toxoplasma gondii), meningitis (Neisseria meningitidis), and staphylococcus (Staphylococcus aureus). After an outbreak of streptococcal infection, glomerulonephritis occurs within 1-3 weeks in 10-15% of patients. It is especially often caused by nephritogenic strains of b-hemolytic streptococcus A.
In response to the introduction of foreign microorganisms into the body, the body produces substances to destroy them. But sometimes, for unknown reasons, the immune system malfunctions, attacking kidney cells with foreign substances. An inflammatory process occurs, accompanied by tissue damage and impaired urine filtration. Microscopic blood clots form inside the renal vessels.
Blood appears in the urine (hematuria). Sometimes there is so much of it that the urine looks like meat slop. But more often, little blood is released, and it can only be detected using laboratory methods.
Symptoms of glomerulonephritis
There are two forms of the disease: acute and chronic. Acute glomerulonephritis gives more vivid symptoms, while chronic glomerulonephritis is practically unnoticeable for a long time. Urologists note that the disease manifests itself more clearly in children than in adults.
Acute glomerulonephritis
The acute form gives at least three groups of symptoms:
Two variants of the course are possible: typical (cyclic) with vivid symptoms and latent (acyclic) glomerulonephritis is expressed by a gradual onset and erased symptoms. Acyclic is dangerous due to late diagnosis. It is this that often develops into chronic glomerulonephritis.
In the acute form of the disease, the patient's temperature rises, weakness, nausea and lower back pain appear. A characteristic symptom of the disease is swelling, especially in the face and neck. Swelling appears in the morning and gradually goes away during the day. The amount of urine produced decreases and becomes reddish in color.
But, more often than not, the symptoms of the disease remain vague. People attribute a slight increase in temperature and weakness to a recent illness. Swelling is also not always pronounced. An adult, especially one who is overweight, often does not notice an increase of 3-4 kg, and the faint reddish tint of urine also does not cause suspicion.
Jade does not cause intense pain, only a slight heaviness in the lower back. Therefore, people often do not consult a doctor, and the disease becomes chronic.
In 60% of patients, blood pressure begins to periodically increase, which is not reduced by conventional antihypotensive drugs. And 85% have problems with the functioning of the heart and blood vessels. Therefore, patients often come not to a urologist, but to a cardiologist or therapist. Nephritis is detected only after tests and ultrasound of the kidneys are prescribed.
Chronic glomerulonephritis
Chronic glomerulonephritis gives 2 groups of symptoms:
- nephrotic signs (urinary problems);
- hypertensive symptoms.
It is not uncommon to have a mixed type of syndrome—hypertensive plus nephrotic.
Also, as with the acute form, a latent course and hematuric type of the disease are possible, when the urine contains red blood cells, and other symptoms are practically invisible.
All forms of glomerulonephritis recur, especially often in the spring and autumn after a streptococcal infection.
Complications and prognosis for cure
In severe cases, nephritis progresses rapidly, causing kidney failure, accompanied by severe swelling. Impaired kidney function leads to poisoning of the body with unresolved toxins. Problems arise with the functioning of other organs - the heart, liver, brain.
Undiagnosed and untreated glomerulonephritis becomes chronic and leads to renal failure. The kidneys shrink, decrease in size, and cannot fully perform their function.
If the disease is not treated, you can get:
- acute renal failure (in 1% of cases);
- acute heart failure (2-3%);
- intracerebral hemorrhage and visual impairment;
- preeclampsia, eclampsia (acute renal encephalopathy);
- chronic glomerulonephritis.
With timely contact with an experienced urologist, the symptoms of acute glomerulonephritis - edema and arterial hypertension - disappear within 2-3 weeks. For a complete recovery, you will have to undergo treatment for at least 2 months.
How is glomerulonephritis diagnosed?
The diagnosis of “acute glomerulonephritis” is made based on several factors:
- History of infectious disease;
- Clinical manifestations - high blood pressure, swelling, urinary disorders;
- Laboratory data.
The urologist evaluates urinary, edematous and hypertensive syndromes.
Patients submit:
- Urine tests
(Zimnitsky and Reberg tests), which detect protein and traces of blood. The analysis reveals clotted cylinders consisting of coagulated protein and other components. These are a kind of “casts” of the kidney tubules, washed with urine. An important symptom is micro- or macrohematuria, when the urine changes color to almost black. At the first stage of the disease, fresh red blood cells are found in the urine, followed by leaching. The Zimnitsky test shows nocturia, decreased diuresis and high relative density of urine. - Blood from a finger
, in which an increase in the level of leukocytes and an acceleration of ESR are diagnosed. These changes indicate an inflammatory process. - Blood biochemistry
. With glomerulonephritis, a sharp increase in residual nitrogen is detected, indicating weak kidney function. An increase in the concentration of cholesterol, creatinine, ALT and AST is diagnosed.
The urologist prescribes an ultrasound of the kidneys and an ultrasound scan of the renal vessels. A kidney biopsy may be ordered to confirm the diagnosis.
What does a kidney ultrasound show for glomerulonephritis?
Ultrasound shows the beginning picture of renal sclerosis - the contours of the kidneys lose clarity, and their tissue becomes dense due to inflammation. The pyramids through which excreted urine enters the collecting system look too dark (hypoechoic).
As the disease progresses, the kidneys shrink. Normally their size is:
- length – 10.5-11 mm;
- width – 4.5-5 mm;
- the thickness of the parenchyma - the substance that makes up the organ - is 1.5-2.5 cm.
With degenerative changes that accompany glomerulonephritis, the kidney tissue shrinks. The kidney becomes uneven with areas of retraction. A layer of calcium salts is deposited around the pyramids that filter urine, which looks like a white rim on ultrasound.
The longer the disease lasts, the smaller the kidneys become. Their contours are completely “blurred” and the organs become difficult to recognize against the background of the surrounding tissue. The internal renal structures become completely indistinguishable.
The blood supply to the organ is also disrupted, visible on ultrasound and Doppler, as a depletion of the vascular pattern and a general decrease in blood flow.
Treatment of glomerulonephritis
The disease, especially when diagnosed late, takes a long time and is difficult to treat. The patient is prescribed anti-inflammatory drugs, antibiotics, and hormones. During treatment, it is important to follow a strict salt-free diet. An indicator of the success of treatment is an improvement in general condition, normalization of laboratory parameters and the disappearance of signs of acute inflammation on ultrasound.
Unfortunately, glomerulonephritis, especially chronic, often recurs after another cold or simply in the off-season. Therefore, people suffering from it need to periodically undergo tests and undergo ultrasound examinations of the kidneys and adrenal glands.
If an ultrasound shows that degenerative changes in the kidneys have stopped, we can assume that the person has overcome an unpleasant disease.
Where to get a kidney ultrasound and be checked for glomerulonephritis in St. Petersburg
In St. Petersburg, such an examination is performed at the specialized urological clinic Diana. The cost of an ultrasound scan of the kidneys and adrenal glands is only 1000 rubles. Ultrasound diagnostics is performed using the latest generation expert equipment. Here you can get advice from an experienced urologist and undergo any tests.
, please select a piece of text and press Ctrl+Enter
link:
Source: https://medcentr-diana-spb.ru/urologiya/glomerulonefrit-proverte-pochki/
Acute and chronic glomerulonephritis on ultrasound
Acute glomerulonephritis is a bilateral inflammation of the glomeruli. Inflammation and sclerosis of the glomeruli impairs kidney function and can ultimately lead to kidney failure. Glomerulonephritis occurs as a late complication of pharyngeal infection. More common in children than in adults.
There may be complaints of recent fever, sore throat and joints, swelling of the face and ankles, cloudy urine, oliguria, and high blood pressure. There is anemia in the blood, high urea and creatinine. There are red blood cells, protein in the urine, and a decrease in glomerular filtration rate.
Acute glomerulonephritis often progresses to chronic glomerulonephritis. Irreversible sequential fibrosis of the glomeruli slowly occurs, the glomerular filtration rate decreases, urea and creatinine accumulate in the blood, and intoxication occurs. After 20-30 years, chronic glomerulonephritis leads to chronic renal failure and ultimately death.
Acute glomerulonephritis does not have any special ultrasound signs. You can notice a slight bilateral enlargement of the kidneys, the renal pyramids are well visualized, the echogenicity of the cortical zone is slightly increased. In chronic glomerulonephritis, ultrasound shows small, smooth, hyperechoic kidneys.
Sources used:
- https://uzi.guru/zhivot/poch/diagnos-pch/glomerulonefrit-pochek-uzi.html
- https://unclinic.ru/urologija/glomerulonefrit-diagnostika-i-lechenie/
- https://medcentr-diana-spb.ru/urologiya/glomerulonefrit-proverte-pochki/
- https://vsepropechen.ru/pochki/bolezni-02/glomerulonefrit/diagnostika-glomerulonefrita.html
- https://lecheniepochki.ru/zabolevaniya/glomerulonefrit/glomerulonefrit-na-uzi.html
- https://store-e.ru/glomerulonefrit-pochek-na-uzi-sovremennaya-klassifikaciya/