To reduce the manifestation of symptoms and correct the clinical picture, a diet for nephropathy is necessary. Any disease of the excretory system disrupts the normal functioning of many organs. The diet should contain low protein and low carbohydrate foods. Thanks to a competent balanced diet, the effects of medications are improved and metabolic processes in the body are normalized.
Useful foods for nephropathy
Since with nephropathy a large amount of protein is released along with the urine, the diet is aimed at saturating the body with protein.
As a result of poor kidney function, fluid accumulates in the body. Therefore, dietary nutrition is focused on reducing and completely eliminating swelling.
Basic characteristics of nutrition in case of illness:
- 1 increase the amount of foods containing protein;
- 2 reduce the consumption of fat-containing foods (about 40% should be vegetable fats);
- 3 enrichment of the body with lipotropic substances that help normalize lipid metabolism in the body and reduce cholesterol;
Recommended products and dishes:
- dietary bread products that do not contain salt;
- vegetable, vegetarian, dairy, cereal, fruit soups;
- lean meat: lean veal, beef, lean pork, boiled or baked in one piece;
- fish – lean varieties, boiled in pieces and chopped, lightly fried after boiling or baked;
- all dairy products, but with reduced fat content;
- cereals – puddings made from oatmeal and buckwheat, porridge, krupeniki;
- The most useful vegetables are potatoes, carrots, zucchini, cauliflower, pumpkin, and beets. Green peas are useful when baked, boiled, or stewed;
- any fruits and berries. Strawberries, raspberries, and lingonberries relieve inflammation well;
- Among drinks, preference should be given to compotes, fruit juices, and herbal infusions.
Folk remedies for the treatment of nephropathy
There are many folk remedies and herbs that relieve inflammation and normalize kidney function.
Collection No. 1
To collect, you need to take St. John's wort (30 g), coltsfoot (25 g), yarrow flowers (25 g) and nettle (20 g). Everything is crushed and mixed thoroughly. Pour 40 grams of the collection into ¼ liter of boiling water and let it brew for a while. The broth is divided in half and drunk in two doses. You need to drink it for 25 days.
Collection No. 2
Flax seeds, comfrey, bearberry leaves, gorse. Each herb should be taken in two parts and mixed with blackberry leaves (1 part) and juniper fruits (1 part). Mix everything thoroughly, pour ¼ liter of hot water, boil for 10-15 minutes over low heat. Take the resulting decoction three times a day.
Collection No. 3
You need to take one part of cornflower and birch buds, mix with two parts of bearberry, add four parts of three-leaf watch. Pour boiling water (250 ml) into a spoonful of the mixture and cook for about 10-12 minutes over low heat. You need to drink the decoction in three doses.
Collection No. 4
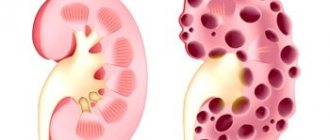
- Classification of diabetic nephropathy by disease stages
Lingonberries are very effective against diseases. Twist the berries and mix with sugar 1:1. We put the resulting mixture into jars, tie it with paper and put it in a cold place. Add berries to taste to the water and drink like compote.
Collection No. 5
Strawberry leaves and berries relieve inflammation well. You need to take berries and strawberry leaves 1:1, pour the mixture with a glass of water and cook for about 10 minutes. You need to drink 20 g three times a day.
Watermelon peel decoction
Not only the pulp of the watermelon, but also its rinds, which need to be brewed, help relieve swelling.
Dangerous and harmful products for nephropathy
With nephropathy, a large number of foods are allowed and the diet is not much different from the diet of a healthy person. But there are still limitations:
- sharp limitation of salt intake;
- reducing foods containing extractives (these are substances that increase the secretion of digestive juice);
- limiting foods containing simple carbohydrates (mainly foods containing glucose);
- the consumption of confectionery products, sweet flour products, and ice cream is limited;
- All types of canned food, spicy and spicy foods are excluded from the diet;
- You should not eat pickles, smoked meats, marinades, or seasonings.
Diet for kidney nephropathy: what is possible and what is not
Grocery list
Recommended for diseases:
- dietary bread products that do not contain salt;
- vegetable, vegetarian, dairy, fruit;
- low fat dairy products;
- lean meat;
- lean varieties of fish.
If you have nephropathy, you should not eat radishes.
In case of nephropathy, the following foods are excluded:
- baked goods;
- fat cottage cheese, sour cream, milk;
- Radishes and legumes are prohibited among vegetables;
- smoked, spicy, marinated dishes.
Drinking regime
The required amount of fluid promotes the elimination of uric acid salts and stabilizes metabolic processes. It is important to follow a drinking regime. Be sure to drink plenty of fluids every day to increase urine output. This liquid is distributed evenly throughout the day. It is useful to drink clean water, tea, herbal infusions, such as chamomile flowers, and rosehip infusions throughout the day. Mineral water, cocoa, and strong tonic drinks are excluded from the diet.
Sample menu for one day
Water with lemon juice after waking up is a good stimulant for the whole body.
After waking up, drink 1 liter of water with a small amount of fresh lemon juice. After 15 minutes, drink a green smoothie made with water, green wheat sprouts and lemon or eat fruit. An hour after fruit, it is beneficial to eat a vegetable salad. Use fresh, seasonal vegetables. Add your choice of pumpkin, sunflower or flax seeds to the salad, season with vegetable oil. From 12:00 to 15:00 digestion is strongest, so it’s good if lunch occurs at this time. Lunch should be complete and light at the same time. Be sure to include dishes made from fresh salad, steamed vegetables and cooked grains or legumes. You can eat whole grain, yeast-free bread. It is prohibited to wash down lunch with any liquid. 2 hours after eating, take a decoction of immunomodulating herbs. For dinner, it is beneficial to eat cooked and fresh vegetables.
Return to contents
Treating diabetes with mineral water baths
Depending on the degree of the disease, treatment is prescribed:
- taking medications;
- kidney diet;
- medicinal blood purification - hemodialysis.
Increased sugar in itself requires adherence to a diet. Failure to follow your doctor’s nutritional recommendations for diabetic nephropathy will cause complications and death.
- normalization of sugar levels in the body;
- blood pressure control;
- restoration of fat metabolism;
- elimination or cessation of the development of pathological changes in the kidneys.
- drug treatment;
- dietary nutrition;
- traditional medicine recipes.
- increase physical activity within reasonable limits;
- give up harmful habits (smoking, alcohol);
- improve psycho-emotional background, avoid stress;
- maintain optimal body weight.
- proteinuria;
- swelling;
- weaknesses;
- drowsiness;
- nausea;
- severe shortness of breath;
- high blood pressure;
- pain in the heart;
- unbearable thirst.
- stimulate the pancreas to secrete insulin;
- reduce the absorption of glucose in the intestines;
- promote the penetration of glucose into tissues;
- slow down the rise in blood sugar levels;
- increase the sensitivity of adipose tissue to insulin and reduce the amount of sugar released from the liver.
In case of severe kidney damage, renal replacement therapy is performed.
And if in the first stages treatment is prescribed in the form of preventive measures, advanced cases require a more serious approach.
For the treatment of diabetic nephropathy, all methods of eliminating pathology are prescribed by a doctor.
loading.
One of the most dangerous and frequently occurring complications of diabetes mellitus is abnormal changes in the structure and function of the kidneys. About 75% of diabetics are susceptible to pathology; in some cases, death cannot be ruled out.
Timely detection of nephropathy in diabetes mellitus and professional treatment of the disease make it possible to avoid irreversible health consequences.
The initial stages of the disease do not manifest themselves in any way, which quite often leads to untimely detection and, as a consequence, treatment of the disease.
Systematic visits to the doctor and timely completion of the necessary tests will help identify nephropathy in the early stages
These symptoms indicate severe stages of nephropathy that require urgent medical attention.
Look
Votes: 210
Patients with type II diabetes, along with the diet, are prescribed tablet medications designed to:
Diet features
What and how much you can eat with diabetic nephropathy, which is nodular-diffuse glomerulosclerosis, depends on the severity of the disease. It is determined by the presence of albumin in the urine and creatinine in the blood.
To do this, tests are done:
- urine for albuminuria;
- urine for blood albumin-creatinine ratio (SACR);
- blood for creatinine and urea with calculation of glomerular filtration rate (GFR).
When prescribing treatment, blood pressure levels are also taken into account. Reducing it and maintaining indicators within the range of no higher than 120–130 by 70–80 is an even more important goal than normalizing glycemia.
This is due to the fact that when the glycated hemoglobin level is 9 or higher, the risks and vascular complications do not increase proportionally, taking the form of a plateau. But the higher the blood pressure, the faster not only cardio, but also all other complications inherent in type 2 diabetes mellitus progress.
Therefore, in diabetic kidney disease, to prolong life and reduce the risk of death, it is necessary to strictly control blood pressure and glycemia. For blood pressure, an ACE inhibitor or a drug from the Sartana group is prescribed.
Sugar is reduced and controlled with a drug from the renoprotective group Gliflozin, which helps improve or reduce GFR. If your cardiovascular risk is high, your doctor recommends taking cardio-aspirin.
Hemoglobin and cholesterol levels are checked. Their results are the basis for prescribing appropriate medications.
And of course, diet and daily physical exercise are required. You need to at least walk for 30 minutes, at a fast pace or at an above-average speed.
Foods and nutritional rules for microalbuminuria
With episodic, and even more so with constant microalbuminuria, when there is a loss of protein in the urine from 30 to 300 mg per day, from the daily diet you need:
- remove fast carbohydrates;
- give up red vegetables and fruits, with the exception of cranberries, cherries and plums;
- limit your daily protein intake to no more than 1 g of protein per 1 kg of body weight (see table below).
We draw attention to the need to abstain from any alcoholic beverages and a categorical ban on smoking tobacco.
Protein content in basic foods allowed for type 2 diabetes
Another important nuance of the diet for diabetic microalbuminuria, which in almost 100% of cases is accompanied by high blood pressure, is limiting the consumption of table salt to 3-5 g per day + a complete ban on pickles. It should be understood that natural products already contain NaCl compounds, so you should get used to preparing all dishes without adding salt.
On a note. Alas, sparkling mineral water is excluded from the menu.
From this point on, the diabetic should get used to regularly taking tests to monitor the levels of potassium, calcium and phosphorus in the blood, and adjust the content of the diet in accordance with the test results (pictured in the tables below). In diabetic microalbuminuria, vitamin D production is usually impaired, so the doctor must select an individual daily dose of alfacalcidol or calcitriol.
Nutrition for proteinuria
At this stage of diabetic nephropathy, the diet takes on all the features of a low-protein diet, and the diabetic is advised to limit daily protein intake to 0.8–0.7 g/kg body weight. It has been proven that such a nutritional system significantly reduces proteinuria, GFR and cholesterol after 130 days.
Diabetic kidney disease requires menu adjustments based on calcium and potassium content
You should also further limit your daily NaCl intake to 2–2.5 g. This means that you must not only stop adding salt to dishes during cooking, but also switch from regular bread to special bread, which is prepared without salt.
As side dishes, it is recommended to use mainly pearl barley and oatmeal, brown rice, broccoli, cauliflower and “regular” cabbage. Buckwheat and potatoes are acceptable.
The best meats are veal and young lean beef, lamb, and rabbit. Fish varieties that contain less salt than others are river perch, pike perch, grass carp, trout, carp, and pike.
Diet in the stage of chronic renal failure
The goal of any dietary treatment for diabetic kidney disease is to delay the timing of dialysis by facilitating the work of the residual nephron.
If diabetic nephropathy has led to the development of chronic renal failure, then according to domestic protocols, the diabetic is recommended to:
- If the creatinine level is <250 µmol/l - diet 7P : protein consumption of no more than 0.7–0.6 g per 1 kg of body weight and calculation of daily caloric intake based on 35–40 calories per 1 kg of body weight. It is advisable to replace some animal proteins with soy proteins. It contains more polyunsaturated fatty acids, vitamins and microelements, less cholesterol and phosphorus, and as a result of its processing in the body, much less purine compounds are formed.
- If the creatinine level is 250–500 µmol/l - diet 7B . This therapeutic nutrition system provides for protein consumption in the range of 0.6–0.5 g per 1 kg of body weight. Phosphorus is limited to 700 mg per day, and potassium to 2.7 g. To limit the consumption of the latter trace element, you should eat less peas, beans, lentils, red cabbage, white bread, rice, mushrooms, peanuts, nuts, and whole milk.
- If creatinine is >500 µmol/l - diet 7A:
- protein restriction of 0.4–0.3 g/kg body weight, but not more than 25 g per day;
- potassium control - no more than 1.6 g per day;
- phosphorus monitoring - up to 400 mg per day;
- inclusion in the daily diet of food supplements containing essential essential amino acids and keto analogues of amino acids, which increases protein utilization and thereby significantly reduces the risk of developing a negative nitrogen balance.
The therapeutic nutrition systems for diabetic nephropathy - 7B and 7A, also have prohibitions. These low-protein diets are contraindicated in nephrotic syndrome and GFR falling below 5 ml/min. They also need to be temporarily abandoned during acute infectious diseases.
Keto analogues of amino acids certified in the Russian Federation
European diabetologists for chronic renal failure prescribe one of two diets calculated by the founder of therapeutic nutrition with protein restriction for patients with progressive nephropathy S. Giovannetti.
Here are their requirements:
- With a plasma creatinine level of 2–5%, a traditional diet that limits consumption per 1 kg of diabetic body weight is:
- protein - up to 0.6–0.5 g;
- phosphates - up to 12–8 mg;
- calories - up to 35 kcal.
- When the level of creatinine in the blood plasma is above 5% - an artificial diet in which it is necessary:
- limit protein to 0.3 g/kg, phosphates to 7–6 mg/kg, calorie content to 20–18 kcal/kg;
- avoid foods and dishes with a lot of potassium;
- Be sure to include in your daily diet food supplements with essential essential amino acids and keto analogues in the range of 16–14 g per day.
By the way, the artificial diet is also called the Swedish diet. It has become widespread since food supplements of EA acids and keto analogues help to avoid the development of malnutrition syndrome and do not reduce the quality of life as perceived by a diabetic.
It should be recalled once again that in case of diabetic nephropathy, especially if a person has switched to a low-protein diet, it is necessary to regularly monitor albumin, K, Ca, Ph, lymphocytes and erythrocytes, and daily urea excretion. It is necessary to weigh yourself regularly to correctly calculate your daily protein dosage.
The final video in this article presents a set of exercises that can be performed by diabetics with diabetic nephropathy who have not yet managed to control their blood pressure. This gymnastics will help avoid the formation of another, no less life-threatening complication of type 2 diabetes, such as diabetic foot.
The effect of nutrition on kidney function
Malfunctions of the kidneys lead to disruption of the process of potassium excretion in the body, which is responsible for the performance of paired organs, the heart muscle and muscle tissue. Therefore, its excess or deficiency can lead to irreversible consequences in the body. Doctors recommend increasing daily potassium intake in the initial stages of nephropathy, and reducing it in later stages.
Excessive phosphorus content in human blood leads to the gradual leaching of calcium from the body, to the development of aching joints and the gradual thinning of bone and cartilage tissue. Phosphorus also causes tissue hardening, resulting in rapid growth of connective tissue in the kidneys, heart muscle, joints and lungs. Therefore, renal pathology is manifested by itchy dermatoses, heart rhythm disturbances and a feeling of heaviness in the lungs. In the acute period, it is necessary to strictly limit the intake of this element, which will help speed up the recovery process.
Sufficient intake of clean drinking water into the body is an important condition for a proper diet. Water helps cleanse the body of harmful compounds, which has a positive effect on the dynamics of recovery. To ensure good urine passage, during treatment it is necessary to avoid spicy, fatty, salty and canned foods, which retain fluid in the body and lead to contamination and increased swelling.
Symptoms of nephropathy
The presence of nephropathy in the initial stages will be indicated by an increased protein content. There are no external manifestations. At stage 3, symptoms of the disease appear:
- weight loss,
- increased blood pressure,
- darkening of the color of urine and the presence of blood in it (in later stages),
- nausea and vomiting,
- headaches and dizziness,
- poor appetite
- thirst,
- shortness of breath, heart pain,
- swelling and fluid accumulation in the abdominal cavity,
- cycle disruption in women.
Dietary table No. 7
Diet for diabetic nephropathy No. 7 is recommended for restoring metabolic processes, reducing swelling, intrarenal and blood pressure. Used for diabetic and dismetabolic nephropathy, glomerulonephritis, chronic renal failure and other renal pathologies.
- What's good for your kidneys - 9 foods to improve kidney function, backed by science
According to the table's recommendations, restrictions include foods high in carbohydrates and fats. Dishes are prepared without salt. The daily volume of fluid consumed is no more than 1 liter. The daily calorie content of foods is no more than 2900 kcal, including carbohydrates - up to 450 g, proteins - up to 80 g, fats - up to 100 g, sugar - up to 90 g.
During diet No. 7 you are allowed to consume:
- vegetable broth soups;
- lean meats and tongue;
- lean fish;
- dairy products, except cheese;
- porridge;
- vegetables;
- fruits;
- eggs no more than 2 pcs.;
- honey, jam, jelly;
- bread and pancakes without salt.
It is prohibited to use:
- salted flour products;
- fatty meat and fish products and broths based on them;
- mushrooms;
- hard and soft cheese;
- legumes;
- products with a high proportion of oxalic and ascorbic acids;
- chocolate.
Authorized Products
During the diet, dishes are prepared without adding salt or with a minimum amount of it. Allowed products:
- vegetable soups,
- fruits and vegetables,
- lean meat and fish,
- low-fat dairy products, except hard cheeses,
- rice and buckwheat porridge,
- whole wheat bread,
- eggs up to 2 times a week,
- vegetable oils,
- compotes, infusions and herbal teas.
What products are prohibited?
There is a fairly wide range of food products, the consumption of which, if you are following a diet for renal failure with diabetes, is not only not recommended - it is directly prohibited.
First of all, you should not consume sugar and products containing it, or large amounts of fructose, including honey, fruit molasses, etc. Such products should be completely excluded.
In addition, you should not eat any baked goods made from white flour. These products contain a lot of fast carbohydrates. Limit the consumption of fruits with too much fructose content - bananas, dates, grapes, melon. You should also not eat sweet varieties of pears, apples, and watermelon.
You should not eat fried foods or fatty meats. Pork, lamb, and fatty fish are prohibited. It is also not recommended to eat dairy products with high fat content - fatty cottage cheese, sour cream, etc.
In addition, you should not eat pickles and smoked meats - they also always contain a lot of salt, which increases blood pressure.
- Diet for kidney hemodialysis list of products table for high potassium
Butter and margarine, which contain huge amounts of animal fat, are excluded. It is also undesirable to use mayonnaise.
It is forbidden to drink carbonated drinks, especially sweetened ones, as well as fruit juices, even natural freshly squeezed ones - taking them can cause an increase in glucose levels.
Of course, any doses of alcoholic beverages, as well as hot seasonings and spices, are prohibited. You should drink tea with caution, and it is better to avoid coffee altogether.
Diet can cause problems with stool, which can be resolved by taking gentle natural remedies.
Read more about nutrition components
During the period of illness of paired organs, their performance is impaired, which manifests itself in a decrease in the removal of waste and toxins from the body. The most difficult for the kidneys are nitrogenous compounds, which are formed from protein products of animal origin. Therefore, all diets for renal pathologies are aimed at gradually reducing the daily amount of animal protein consumed and replacing it with protein of plant origin.
It is important to remember that a sudden refusal of protein foods traumatizes a weakened body and can lead to a worsening of the condition. Therefore, this process must be gradual. It is recommended to first replace fatty foods with dietary ones (chicken, low-fat fish, veal).
A large amount of salt in the daily diet leads to the formation of swelling and an increase in intrarenal and blood pressure. Therefore, to reduce the severity of these symptoms, gradual salt restriction is necessary.
It is recommended to cook food without salt or, if necessary, add a little salt before eating. To improve the taste characteristics of food, salt can be replaced with tomato juice without salt, lemon juice, garlic, onions, and herbs.
Menu for diabetic nephropathy
It is recommended to make at least one day a week completely vegetarian:
- at 8 o’clock for breakfast oatmeal porridge with flax seeds and blueberries, rooibos tea or currant berries;
- at 10 o'clock second breakfast of pumpkin casserole with rice, chicory;
- at 14:00 for lunch vegetable soup with herbs and sago, tofu and tomato salad with basil;
- at 16:00 for an afternoon snack: 50 g of cottage cheese with apricot jam without sugar, rosehip decoction;
- at 19 o'clock for dinner bell peppers stuffed with vegetables, bread without salt with hummus or bean paste;
- Before going to bed, drink 100 ml of kefir with a teaspoon of bran.
We recommend reading the article on the prevention of diabetes. In it you will learn about risk factors for developing diabetes, types of preventive measures and diet to prevent diabetes. Find out more about urine testing for diabetes here.
The diet for diabetic nephropathy is based on the exclusion of simple carbohydrates, limiting cholesterol, protein and table salt. All spicy, fatty and salty foods are prohibited. Vegetables, cereals, vegetarian first courses, fruits and berries are recommended.
Dairy products are included in small quantities. Meat or fish are allowed no more than once a day, alternately. If there is a violation of the blood electrolyte levels, it is necessary to make additional adjustments to the menu.
Products for the diet
The patient's food should be varied. The daily diet consists of cereals, meat or fish, vegetables, fruits, dairy and fermented milk products. The norm of liquid consumption is two liters.
It is worth knowing that fruit and berry juices are prohibited for dietary nutrition, even those made from low GI fruits. With this treatment, they lose fiber, which serves as a uniform supply of glucose to the blood.
It is better to eat fruits and berries in the morning, no more than 150 - 200 grams. They should not be pureed, so as not to increase the GI. If a fruit salad is prepared from these products, this should be done immediately before consumption in order to preserve as many useful vitamins and microelements as possible.
Low GI fruits and berries:
- black and red currants;
- gooseberry;
- apples of any variety, their sweetness does not affect the index;
- pear;
- apricot;
- blueberry;
- raspberries;
- strawberry;
- strawberries
- any types of citrus fruits - lemon, orange, tangerine, pomelo, lime.
Vegetables are the basis of diabetic nutrition and make up up to half of the entire diet. They can be served for breakfast, both, and for afternoon tea and dinner. It is better to choose seasonal vegetables, they contain more nutrients.
Vegetables for diabetic nephropathy with low GI:
- squash;
- onion;
- garlic;
- eggplant;
- tomato;
- green beans;
- lentils;
- fresh and dried split peas;
- all types of cabbage - cauliflower, broccoli, white and red cabbage;
- Bell pepper.
Cereals can be used as side dishes or added to first courses. You should be extremely careful when choosing them, as some have medium and high GI. For diabetes that is not burdened by other diseases, doctors allow you to occasionally eat corn porridge - the GI is within high limits, since it is rich in nutrients. But in diabetic nephropathy, its consumption is contraindicated. Since even a minimal jump in blood sugar puts a strain on the kidneys.
Allowed cereals:
- pearl barley;
- barley grits;
- Brown rice;
- buckwheat.
Almost all of their dairy and fermented milk products have a low GI; only the following should be excluded:
- sour cream;
- cream 20% fat;
- sweet and fruity yogurt;
- butter;
- margarine;
- hard cheeses (low index, but high calorie content);
- condensed milk;
- glazed curd;
- curd mass (not to be confused with cottage cheese).
Eggs are allowed for diabetics no more than one per day, since the yolk contains harmful cholesterol. With this nephropathy, it is better to reduce the consumption of such a product to a minimum.
This does not apply to proteins; their GI is 0 units, and the yolk index is 50 units.
Meat and fish should be chosen from low-fat varieties, removing any remaining skin and fat from them. Caviar and milk are prohibited. Meat and fish dishes are included in the daily diet, preferably once a day.
The following meats and offal are allowed:
- chicken;
- quail;
- turkey;
- rabbit meat;
- veal;
- beef;
- beef liver;
- chicken liver;
- beef tongue.
From fish you can choose from:
- hake;
- pollock;
- pike;
- cod;
- perch.
By forming a diabetic diet for a patient from products of all the above categories, a person receives proper and healthy food.
It aims to maintain blood sugar levels within a normal range.
diabetes.guru
Diet 7 b
KBZHU is calculated for each individual person, taking into account his characteristics.
For nephropathy, nutrition should be high in calories and should be 3500 kcal per day. Foods high in vegetable fats and slow carbohydrates should be eaten. A decrease in caloric content leads to the fact that the body begins to consume its own proteins, resulting in poisoning with harmful substances formed during these reactions. In this regard, the load on the kidneys increases.
To correctly calculate calories, fats, carbohydrates, proteins that enter the body with food, there is a KBJU index. For each patient, the index is calculated individually, taking into account age and goals. Using the numerical values of the product composition, you can calculate the calorie content. For example, a 10 g piece of hard cheese contains 2.4 g of protein, 3 g of fat and 0.2 g of carbohydrates. Calorie content is calculated using the following formula: 2.4×4+30×9+0.2×4=37 kcal.
Diet depending on the stage of the disease
- At the initial stage, you can stick to your normal diet, but with minor restrictions for preventive purposes. You can follow diet number 7.
- At the stage of proteinuria, you need to switch to a moderately low-protein diet (diet 7a). Daily protein intake is 0.75-08 g per kilogram of the patient’s weight. That is, for men this is approximately 55 g, and for women – 40-45 g. Half of the daily protein should be of animal origin.
- At the third stage, you need to adhere to the following principles of therapeutic nutrition:
- Daily protein limits depend on the severity of chronic renal failure. This will reduce azotemia and increased filtration of protein metabolites through the kidneys.
- The energy value of the diet must be coordinated according to the body’s energy consumption and its deficiency must be increased at the expense of fats and carbohydrates. This will improve the absorption of protein from food and reduce the breakdown of protein from the body's reserves.
- It is important to regulate the amount of fluid and salt, taking into account the excretory activity of the kidneys. When edema and arterial hypertension appear, you need to sharply reduce the amount of salt and liquid.
The formation of diabetic nephropathy is accompanied by impaired renal function. The disease develops gradually. In this case, several stages of the disease are distinguished, each of which is characterized by certain symptoms and the degree of damage to the organ. To treat and prevent the disease at each stage, in addition to treatment with medications, you need to adhere to proper nutrition. The diet for diabetic nephropathy directly depends on the stage of the disease. As a rule, one of three types of low-protein diet is used - 7, 7 a, 7 b. Each of the diets is used in the complex treatment of diabetic nephropathy.
What should you consume?
The main part of the diet should be vegetables. They should be consumed raw, steamed, stewed, boiled - just not fried.
There are no restrictions on vegetables, with the exception of potatoes. It is recommended to consume it in baked form, no more than 200 grams per day.
Buckwheat should be recognized as the most useful cereal, which must be included in the diet for diabetic nephropathy. It contains virtually no simple carbohydrates, which are contraindicated for diabetics. Other cereals, especially semolina, should be consumed with caution.
Eating greens in general and green vegetables in particular is very beneficial. It is better to obtain animal fats from dairy products, controlling their quantity.
Among the juices, it is recommended to use tomato and mixtures of tomato with other vegetable juices.
From fruit juices, it is permissible to take small amounts of fresh plum juice.
In general, nutrition for kidney failure and diabetes, in addition to limiting certain foods, should also be moderate in portions. In no case should you overeat - this negatively affects both the balance of enzymes in the body and the condition of the kidneys.
You should not eat pearl barley - it contains too many carbohydrates.
What is nephropathy
Diabetes mellitus causes pathological deterioration of the kidney vessels. This condition is called nephropathy and causes kidney failure. High risk of death. Nephropathy requires medication and diet. In more advanced cases, hemodialysis or a kidney transplant is required. There are 5 stages of nephropathy:
- At stage 1, there is a slight increase in the renal vessels. There is no clinical picture. A medical examination will not show any abnormalities in the tests.
- At stage 2, the structure of the vessels changes, the walls thicken. The clinical picture is also absent.
- At stage 3, initial nephropathy is present. The patient's condition does not worsen, but tests will show increased protein in the urine.
- At stage 4, symptoms become severe. A medical examination will show a strong deviation of the protein content in the urine from the norm.
- At stage 5, kidney failure occurs. Only drastic methods will save the patient’s life: hemodialysis or a kidney transplant.
In the early stages of kidney disease, there are no significant symptoms. Diabetics need to be screened regularly. This will help diagnose complications at earlier stages.
General recommendations
The choice of diet for nephropathy is made by the attending physician, based on the data obtained during the examination. The way of eating during the acute period of the disease helps to cope with severe swelling of the body and normalize the water-salt balance. Thanks to this, the severity of signs of intoxication in the body is reduced and the diuretic function is normalized. The choice of dietary table is made with the aim of reducing the amount of harmful compounds that can come from food.
Depending on the severity of symptoms, the cause of the pathological process, as well as the general condition of the patient, dietary table 7, 7a, 7b is prescribed.
All areas of nutrition are based on general principles:
- reducing the amount of fatty foods and animal protein, which are gradually replaced by vegetable fats;
- reducing the amount of salt consumed per kilogram of weight;
- refusal of canned, fried, smoked, salted, spicy and pickled foods;
- plenty of drinking regime;
- fractional meals with frequent meals in small portions;
- exclusion of light carbohydrates and sugar;
- with an increased concentration of potassium in the blood - a decrease in its intake from food;
- if potassium levels are low, ensure sufficient intake from food;
- reducing the amount of food high in phosphorus;
- eating foods that contain large amounts of iron;
- all products are consumed boiled or cooked on a steam grill;
- Dietary nutrition for children is similar to that for adults.
Diet effectiveness
The treatment menu is compiled separately for each patient. The goal of the diet is to reduce the impact on the kidneys, normalize the body’s water balance, and reduce or completely eliminate the consumption of harmful foods.
- less animal proteins, more plant proteins,
- reducing salt intake,
- reducing food portions, the interval between meals is no more than 2-3 hours,
- normalization of potassium intake up or down,
- exclusion of fast carbohydrates from the diet,
- normalization of water consumption, increasing consumption of iron-containing products,
- control of consumption of phosphorus-containing products,
- exclusion of fried, salted, smoked, fast food and semi-finished products,
- bake, boil or cook food in a double boiler.
Nitrogen compounds formed when consuming animal proteins put a strain on the kidneys.
To reduce the negative impact during illness, animal proteins are replaced with plant proteins.
A sharp refusal of protein foods provokes a stressful state for the body. You need to gradually reduce the amount of protein foods, replacing fatty meat with diabetic meat. Then switch to plant proteins.
Diabetics are recommended to have a daily fluid intake of at least 2 liters. With diabetic nephropathy, water is an additional burden on the affected organs. The daily dose of fluid is reduced by 2 times. The main sign of excess fluid intake is swelling.
Causes of nephropathy
Diabetes is the root cause of kidney disease. But there are factors that increase the risk of nephropathy:
- hypertension;
- sudden surges in blood sugar;
- obesity;
- lipid metabolism disorder;
- diseases of the genitourinary organs;
- non-compliance with the prescribed diet;
- taking toxic medications;
- bad habits and alcohol.
Sources used:
- https://edaplus.info/feeding-in-sickness/nephropathy.html
- https://etopochki.ru/kidney/drugoe/dieta-pri-nefropatii-pochek.html
- https://motiv-tarif.ru/dieta-diabeticheskoy-nefropatii-pochek-spisok-produktov/
- https://tvoyapochka.ru/lechenie/dieta-pri-diabeticheskoj-nefropatii
- https://hearth-health.ru/menyu-pri-nefropatii-diabeticheskoy/
- https://endokrinolog.online/dieta-pri-diabeticheskoj-nefropatii/
- https://stopzaraza.com/diety/dieta-pri-diabeticheskoj-nefropatii-pochek-spisok-produktov-dlya-diabetikov-2.html
- https://diabeto.ru/dieta/dieta-pri-nefropatii-pochek-i-saharnom-diabete/
Diet - direct impact on the prognosis of IgA nephropathy
The disease is not uncommon and affects about 1% of the world's population. Because the clinical manifestations are often insidious, assessing the incidence as well as the prognosis becomes more difficult. It usually affects young people and is three times more common in men than women. The cause is unknown, only that the infection is a direct sign of kidney disease. Regarding the mechanisms responsible, it has been shown that in patients with IgA nephropathy, a small portion of IgA has an abnormal structure and is deposited in the kidneys. The rest of the IgA works fine, especially against infections.
Berger's disease is characterized by:
- the presence of blood in the urine;
- detected only in the kidneys;
- diagnosed using immunofluorescence, which reveals IgA deposits on a kidney fragment taken during a biopsy;
- is final (incurable);
- clinically difficult to predict and may progress to renal failure;
- There is currently no specific treatment, but there is symptomatic therapy that requires early intervention to protect the kidneys;
- often recurs on a transplanted kidney;
- the reasons are unknown.
The complex mechanisms responsible for mesangial cell damage are not yet fully understood. The causes are likely related to environmental factors and genetic predisposition. Therefore, adjusting the diet of patients with IgA nephropathy is so far the only way to prevent the development of the disease and help preserve negative processes. The prognosis and quality of life of the patient directly depends on the menu. What should patients with IgA nephropathy eat? Diet plays a very important role in prevention and treatment. Basic knowledge about diet will help you correctly adjust the menu of a sick person.