Etiology.
There are about 40 known causes of arterial hypertension, which are divided into congenital and acquired. Among congenital ones the most common are:
• fibromuscular dysplasia of the renal arteries; • hypoplasia of the renal artery and kidney; • extravasal compression of the renal artery; • aneurysms of the renal arteries; • arteriovenous fistulas.
Acquired factors for the development of ARH:
• atherosclerosis; • nonspecific aortoarteritis; • nephroptosis; • kidney infarction; • trauma; • dissecting aortic aneurysm.
Atherosclerosis
- the main cause of renovascular hypertension in people over 40 years of age, accounting for 60-85% of cases. Atherosclerotic plaques are localized mainly at the mouth or in the proximal third of the renal artery.
In the vast majority of cases, unilateral lesions are observed, while bilateral lesions occur in approximately 1/3 of cases and lead to a more severe course of ARH. The right and left renal arteries are affected equally often. In 10% of cases, atherosclerosis of the renal arteries can be complicated by thrombosis. The disease is more common (2-3 times) in men.
Fibromuscular dysplasia (FMD)
As a cause of renovascular hypertension, it ranks second after atherosclerosis. It occurs mainly in young and even children (from 12 to 44 years), the average age is 28-29 years. FMD is found 4-5 times more often in women than in men.
Morphologically, this pathological condition manifests itself in the form of dystrophic and sclerosing changes, affecting mainly the inner and middle lining of the renal arteries and their branches. In this case, hyperplasia of the muscular elements of the wall can be combined with the formation of microaneurysms.
As a result, there is an alternation of areas of narrowing and expansion (aneurysms), which gives the arteries a unique shape - in the form of strings of pearls or beads. The pathological process, although widespread, is unilateral in 2/3 of cases.
Nonspecific aortoarteritis
ranks third in frequency among the causes of ARH (up to 10%). It is characterized by a primary lesion of the medial tunic of the vessel. Inflammatory infiltration of the media with transition to the adventitia and intima ends with sclerosis and destruction of the elastic frame of the renal artery, which leads to stenosis of its lumen.
The pathological process is mainly limited to the proximal segment of the vessel and almost never spreads to its intraorgan branches. In contrast to fibromuscular dysplasia, nonspecific aortoarteritis always has varying degrees of severity of aortic damage.
Vasorenal hypertension can develop as a result of extravasal compression of the renal artery, as a result of thrombosis or embolism of the renal artery, aneurysm formation, hypoplasia of the main renal arteries, nephroptosis, tumors, cysts, anomalies of the kidneys, etc.
Trigeminal neuralgia: symptoms and treatment
After the first painful attack, you can grimace as much as you like, feel every millimeter of facial skin and even pat yourself on the cheeks approvingly.
Everything is fine! But the fear of the next attack has settled in my soul forever...
This is how most of my patients describe the onset of a painful and difficult-to-treat disease called trigeminal neuralgia (trigeminal neuralgia, Fothergill's disease).
Waiting for the pain
Unlike tension headaches, trigeminal neuralgia is characterized by sudden, short-term, intense, recurring pain in the area of innervation of one or more branches of the trigeminal nerve, usually on one side of the face, but can affect both sides, and can (in an atypical form) manifest as a burning sensation , pressing, aching, bursting, constant or wave-like pain or a feeling of goosebumps running across the face.
Attacks of these pains in the face (lip, eye, nose, upper and lower jaw, teeth, gums, tongue) can occur spontaneously or be provoked by talking, chewing, brushing teeth, touching certain areas of the face (trigger points that trigger an attack; usually located in area of the nasolabial triangle). Their frequency varies from single to tens and hundreds per day! During the period of exacerbation, more often in the cold season, attacks become more frequent.
The pain is so severe that patients cannot concentrate on anything else and are in constant tension, all the time waiting for the next attack (they do not touch the painful side of the face, do not brush their teeth, do not chew on the affected side). There have been cases where patients, unable to bear the pain any longer, committed suicide.
What really hurts
The main cause of true trigeminal neuralgia is compression (squeezing) of the trigeminal nerve root by an arterial and, less commonly, venous vessel directly at the brain stem, from where this nerve actually exits.
The trigeminal nerve, on the one hand, is the main sensory nerve of the face and oral cavity, on the other, it also contains motor fibers that innervate the masticatory muscles.
Therefore, in addition to transmitting information to the brain about what our face is doing at any given time, the trigeminal nerve carries impulses to some of its own facial muscles, which is why pain is often accompanied by a tonic, long-term (trismus), or short-term (tic) contraction of these muscles.
There are several hypotheses to explain why nerve compression leads to the development of trigeminal pain, but none of them is yet generally accepted.
In all cases, confirmation of a neurovascular conflict is carried out only with the help of MRI, so the doctor will definitely refer you to this study. Unfortunately, in 15% of patients, even MRI is not able to accurately establish the diagnosis.
Then electromyography (EMG) or electroneurography (ENG) can help doctors.
Diagnostic problems
But alas, most often after the first attacks a person is sent not to a neurologist’s office, but to a dental clinic. This is due to the fact that the area of pain is located not only on the face, but also in the oral cavity.
Very often, healthy teeth are removed by mistake on the affected side, sometimes this “attraction” lasts for months and years, and only after losing half of the “emergency reserve” of teeth does the patient begin to suspect something...
The standard for diagnosing classical trigeminal neuralgia, according to the diagnostic criteria of the International Headache Society (IHS, ICHD-II), is the presence of at least 4 points out of the 5 below:
- The pain occurs in the form of attacks lasting from several seconds to 2 minutes in areas of the face corresponding to the zones of innervation of the trigeminal nerve.
- The pain is sudden, intense, sharp, similar to an “electric discharge”, caused by irritation of various areas of the face and oral cavity when eating, talking, washing the face, brushing teeth.
- Attacks of pain are stereotypical for each patient.
- There are no neurological symptoms during the interictal period.
- Taking carbamazepine causes pain relief at the onset of the disease.
Conservative therapy
Treatment always begins with conservative therapy, the basis of which is anticonvulsants (in particular carbamazepine). Their use at the onset of true trigeminal neuralgia leads to regression of the pain syndrome in 90% of patients.
That’s why it’s so important not to delay seeing a doctor! However, with long-term use, the effectiveness of the drugs sooner or later decreases, toxic damage to the liver, kidneys, and changes in the cellular composition of the blood may develop, so conservative therapy can only be considered temporary.
In turn, patients prefer vascular drugs, antispasmodics, sedatives, ointments with anesthetics, physiotherapeutic procedures, acupuncture, laser therapy, and are happy to use traditional medicine methods and efferent methods of therapy (plasmapheresis, hemosorption).
In my experience, all this does not bring any particular relief, but it significantly distracts from the anxious anticipation of an attack. And... the time before examination and surgical treatment is delayed, which sometimes leads to tragic consequences. Meanwhile, the operation cannot be delayed.
Neurosurgical treatment
As for surgical treatment, today neurosurgeons have two main methods at their disposal:
Vascular decompression.
The essence of the method, as the name suggests, is to eliminate compression, i.e. compression of the nerve by the adjacent vessel. The method is indicated for all types of vascular compression of cranial nerves.
To use it, an established diagnosis of classical trigeminal neuralgia is sufficient. A contraindication is the presence of severe concomitant pathology that makes it impossible to perform a neurosurgical operation.
Stereotactic radiosurgery, or “gamma knife”.
To achieve the effect, the trigeminal nerve root is irradiated with a dose of ~ 90 Gy and the affected cells are “burned out”.
Indications for the use of this method are aggravated somatic status (presence of chronic diseases, mainly cardiovascular and endocrine) and the patient’s categorical refusal of surgical intervention.
The use of the method is justified by the non-invasive nature of the technique, which significantly reduces the likelihood of complications, however, radiosurgery is less effective and has a higher number of relapses.
In general, the success of treatment for trigeminal neuralgia, just like the treatment of other diseases, depends on a clear diagnosis, strict adherence to surgical technologies and... your timely visit to the doctor!
Valentina Saratovskaya
Photo thinkstockphotos.com
Products by topic: carbamazepine
Source: https://apteka.ru/info/articles/bolezni-i-lechenie/nevralgiya-troynichnogo-nerva-simptomy-i-lechenie/
Pathogenesis.
Narrowing or occlusion of the renal artery results in decreased renal blood flow and decreased perfusion pressure. This in turn causes insufficient stretching of the adductor arterioles of the Malpighian glomerulus.
The granular cells of the juxtatomerular apparatus (JMA), located in the medial layer, which are a kind of volume-receptor apparatus, very subtly react to any changes in renal hemodynamics and release renal incretrenin into the blood. The development of ischemia of the renal tissue leads to hyperplasia of JGA cells, resulting in hypersecretion of renin.
Renin itself is an enzyme that converts angiotensinogen coming from the liver into angiotensin I, which, under the influence of angiotensin-converting enzyme, becomes angiotensin II. The latter is one of the strongest vasoconstrictors, which, directly acting on systemic arterioles, causes their spasm, which sharply increases peripheral resistance.
In addition, angiotensin II stimulates the production of aldosterone by the adrenal cortex, which leads to the development of secondary hyleraldosteronism with sodium and water retention in the body (increasing blood volume) and in the wall of arterioles, causing their swelling and an even greater increase in peripheral resistance.
Peripheral vasospasm, hypernatremia and hypervolemia lead to worsening arterial hypertension. This is the essence of the generally accepted “renopressor” theory of the pathogenesis of ARH, the founder of which is Goldblatt.
In contrast, Grollman’s “renoprivilegic” theory suggests that the body’s hypertensive reaction to disruption of the normal blood circulation of the kidney is not caused by increased production of pressor substances, but, on the contrary, by insufficient production of depressor substances by the kidney.
According to this theory, “any decrease in the amount of renal tissue in the body, disrupting to one degree or another the metabolic function of the kidneys, will create the prerequisites for the development of arterial hypertension.”
The experiment actually proved that complete removal of both kidneys, as a rule, leads to the development of malignant hypertension. A.A. Spiridonov believed that this theory was imperfect for the following reasons: firstly, renal artery stenosis does not always lead to a decrease in the size of the kidneys and the amount of renal parenchyma; secondly, one of the effective methods of radical treatment of ARH - nephrectomy, according to Grolman's theory, should have led not to a hypotensive, but to a hypertensive effect.
At the same time, the existence of depressor substances secreted by the kidney is generally recognized. The main one is prostaglandin F2, which has a pronounced hypotensive effect due to the direct expansion of the lumen of small arterioles.
The natural course of atherosclerotic RH is characterized by a progressive decrease in renal blood flow, which ultimately leads to complete loss of renal function (“ischemic nephropathy”).
This disease manifests itself in middle or old age. In contrast, fibromuscular dysplasia usually appears at a young age, is more common in women, does not have a progressive course, and rarely leads to ischemic nephropathy.
Vazoneural conflict on MRI
The nervous system allows a person to navigate the world of sensations: thanks to it, he perceives smells, taste characteristics of food, makes visual portraits of what he sees, hears and distinguishes sounds.
The functionality of sensory and motor reactions, as well as the body’s response to irritation coming both externally and internally, depends on it. Isolated nerve cells from different parts of the brain are united into clusters. They are called cranial nerve nuclei. Each cell has processes. Part of them, going to the sides of the nucleus, uniting, becomes the nuclei of the cranial nerves.
Those, in turn, are divided into parts: one of them goes to the cells that make up the cerebral cortex, the other part extends to the cells of other organs and tissues of the body.
In this way, the relationship between the brain and every cell of the human body is established.
Several intracranial nerve roots are located on the surface of the face. These are the so-called ordinary nerves. Nerve fibers are also laid along the vessels (along venous and arterial).
Vazoneural conflict is the result of a connection between a nerve and a vessel, in which the walls of the latter create compression on the nearby nerve.
Reasons why the vessel puts pressure on the nerve fiber:
- it surrounds the nerve process like a loop (this is considered an anomaly in the location of the vein or artery);
- inflammation progresses in the bone canal, which is why it gradually narrows; when the space decreases, the nerve and vessel passing through the canal begin to put pressure on each other (during otitis media or another ENT disease);
- the vessel running next to the nerve fiber has an enlarged wall (a sign of an aneurysm);
- a large vessel compresses a part of the trigeminal nerve, which does not have fibers with a myelin sheath (this happens when a person has manifestations of sclerosis).
How does vasoneural conflict occur?
There are frequent cases when a vasoneural conflict occurs when the cerebellar artery pulsates, which passes to the trigeminal nerve. When the heart contracts, blood begins to move through the vessels. Blood flow creates a pulsation in their walls. As a result, there is compression of the nearby nerve.
The result of constant compression of pulse oscillations on the nerve area next to which the vessel passes is its demyelination. The nerve loses its myelin sheath (which is normally present).
Due to the sheath, information is transmitted along the nerve processes (also a pain signal), when it is destroyed, the person suffers from trigeminal neuralgia.
It is for this reason that with vasoneural conflict the appearance of this syndrome is observed.
What are the symptoms?
- pain appears in the innervation area (the place where the processes of the trigeminal nerve pass through the tissues and receive signals from the branches of the trigeminal nerve). Usually this is one of the two halves of the face,
- the pain syndrome comes on suddenly,
- in 80 out of 100 cases, the pain disappears in unexpected attacks and does not bother you for some period of time, in 20 cases it becomes constant;
- an attack of pain can last a few seconds or last for minutes;
- the part of the face affected by the pathology may involuntarily twitch during pain symptoms due to muscle contractions, the skin is sometimes redder, tears flow from the eyes, and salivation increases;
- the patient places his hand on the painful area and tries to breathe less slowly;
- as soon as the attack passes, painful points are felt in the place where the nerve enters the facial surface.
Factors contributing to the occurrence of pain attacks:
- Prolonged exposure to the cold, leading to hypothermia;
- Migraine attacks;
- Nervous tension;
- Chewing;
- Some foods can cause an attack (alcoholic drinks);
- Talk;
- Sanitation of the oral cavity with a brush.
Other causes of neuralgia:
- The nerve is destroyed (occurs with multiple sclerosis);
- Compression of the nerve process by a neoplasm from the outside;
- Neuroma (type of tumor);
- Bruises and fractures of the skull bones;
- Diseases of an infectious nature.
How are inflammation of the trigeminal nerve and trigeminal neuralgia related?
Neuritis (the process of inflammation) is a pathology that results from the spread of an inflammatory reaction from nearby organs (during caries, sinusitis) or the penetration of infection through the blood. Infectious damage to the nerve process ends with the myelin sheath becoming thinner, and symptoms of trigeminal neuralgia appear.
The exit site of the trigeminal nerve is circled; the MRI image shows a large vessel causing compression of the nerve.
Trigeminal nerve inflammation on MRI
MRI images will show both demyelination of the fibers and inflammatory diseases that led to the development of neuritis: the presence of exudate in the sinuses, an edematous process in the middle and inner part of the ear.
MRI of the brain and vasoneural conflict
Symptoms indicating trigeminal neuralgia are a direct reason to suspect the presence of a vasoneural conflict.
MRI of the brain has become the main method for determining this pathology. The medical specialist looks at the location of the nerve relative to nearby tissues, veins and arteries.
MRI is based on the influence of a magnetic field, and not on X-ray radiation, as is the influence of CT or X-ray examinations.
Therefore, if there are no contraindications to it, then the examination is safe for the patient.
You will find contraindications for the MRI procedure here.
What does MRI of the brain show in case of vasoneural conflict?
Using MRI for suspected vasoneural conflict, the doctor will immediately pay attention to the trigeminal nerve.
Using MRI, its structure, bone canals, and location in relation to nearby vessels are assessed; the doctor will look for the presence of vascular loops and inflammatory foci in nearby organs. MRI is the only possible diagnostic method that can help identify areas of nerve demyelination that occur as a result of trauma, compression, and multiple sclerosis.
The method determines the presence of a vasoneural conflict and the source of its development.
To maximize the information content of the examination, an MRI with contrast is prescribed. The contrast agent, entering a vein, accumulates in the bloodstream, penetrating the vessels in the brain. One of these vessels will be the cause of the vasoneural conflict. With the help of contrast, the vessels will be visible more clearly on MRI images, which means that abnormal changes in them will become more noticeable.
In tumor formations, the vascular network is denser, and the blood circulation in it is stronger than in healthy tissues. Due to this, its cells receive nutrition and grow. Under the influence of contrast, the formation that creates compression of the trigeminal nerve glows brighter. This helps to detect it in a timely manner and find out what caused the neuralgia.
Source: https://mrt-v-spb.ru/vazonevralnyy-konflikt-na-mrt/
Clinical manifestations.
There are no pathognomonic symptoms of vasorenal hypertension characteristic of some forms of hypertension (Conn's syndrome, Itsenko-Cushing syndrome, pheochromocytoma). Patients' complaints can be divided as follows:
• characteristic of cerebral hypertension - headaches, a feeling of heaviness in the head, tinnitus, pain in the eyeballs, memory loss, poor sleep; • associated with overload of the left side of the heart and coronary insufficiency - pain in the heart, palpitations, a feeling of heaviness in the chest; • a feeling of heaviness in the lumbar region, mild pain, hematuria in case of renal infarction; • caused by ischemia of other organs, the main arteries of which are affected simultaneously with the renal vessels; • characteristic of systemic inflammatory response syndrome (with nonspecific aortoarteritis); • characteristic of secondary hyperaldosteronism - muscle weakness, paresthesia, attacks of tetany, isohyposthenuria, polyuria, polydipsia, nocturia.
However, it should be noted that in approximately 25% of patients, renovascular hypertension is asymptomatic.
Diagnostics.
The following anamnestic data are important for making a diagnosis:
• development of stable hypertension in children and adolescents; • refractoriness to treatment of hypertension in people over 40 years of age, in whom the disease had previously been benign and antihypertensive therapy was effective; identification of intermittent claudication and/or symptoms of chronic cerebrovascular insufficiency in these patients; • connection of the onset of hypertension with pregnancy and childbirth (without nephropathy); • connection of the onset of hypertension with instrumental studies or manipulations in the area • of the kidneys, with operations on the kidneys and abdominal aorta; • development of hypertension after an attack of pain in the lumbar region and hematuria in patients with heart disease, arrhythmias or in patients with post-infarction cardiosclerosis and episodes of embolism in other arterial territories.
During the examination, the pressure in the upper and lower extremities should be measured, which will exclude coarctation syndrome and identify lesions of the arteries of the upper and lower extremities.
It is important to take measurements in the horizontal and vertical positions of the patient. If the blood pressure is higher in the orthostatic position, then one can think of nephroptosis.
Auscultation of the abdominal aorta and renal arteries is necessary - in approximately 40-50% of patients, a systolic murmur is heard in the projection of the renal arteries or abdominal aorta.
Diagnostics can be helped by listening to systolic murmur over superficial arteries: carotid, subclavian and femoral - as a sign of systemic damage in atherosclerosis and aortitis.
Based on anamnesis, examination and a number of studies, the following signs can be identified that allow one to suspect renovascular hypertension:
• arterial hypertension resistant to two or more antihypertensive drugs and diuretics; • the appearance of arterial hypertension before the age of 20 years in women or after 55 years in men; • rapidly progressing or malignant hypertension;
• 1 presence of different manifestations of atherosclerotic disease; • normal urine test; • azotemia, especially developing during the use of ACE inhibitors or angiotensin II receptor blockers; • systolic murmur over the abdominal aorta and renal arteries; • differences in kidney size exceeding 1.5 cm (based on ultrasound).
The above signs only allow us to suspect and make an assumption about renovascular hypertension, which is often quite justified, but they do not make it possible to fully confirm this diagnosis.
Additional research is needed to confirm or exclude it. The most reliable and reliable method for detecting IH is renal angiography, which can be performed in specialized vascular centers. It allows you to determine the cause of the stenotic process, assess the degree of stenosis and its localization, which is crucial for deciding on surgical treatment.
Along with this, there are a number of minimally invasive screening methods that can detect damage to the renal arteries and determine indications for angiography and avoid it in patients with a different genesis of hypertension.
In particular, renal scintigraphy with ACE inhibitors, duplex scanning, magnetic resonance angiography, and CT angiography have high sensitivity and can be used in combination or alone to achieve adequate screening of patients before conventional radiocontrast angiography.
Renoscintitraphy with angiotensin-converting enzyme (ACE) inhibitors
. The use of ACE inhibitors for functionally significant renal artery stenosis leads to a decrease in glomerular filtration rate due to the elimination or significant weakening of the constriction of efferent arterioles.
The consequence of this is characteristic changes in the renogram. In this case, on the side of the lesion of the renal artery, the effect of “medical nephrectomy” is revealed, which highly accurately indicates a violation of the main renal blood flow.
Scintigrams using ACE inhibitors should be interpreted sequentially with low, medium and high probability of IH. A normal scintigram using ACE inhibitors shows a low probability of IH (less than 10%).
A reduced, poorly functioning kidney and bilateral symmetrical abnormalities, such as cortical tubular retention, indicate an intermediate likelihood of IH.
Criteria associated with a high probability of IH include deterioration of the scintigraphic curve, decrease in relative uptake, prolongation of renal and parenchymal transit time, and prolongation of T-max.
Duplex scanning.
This study has the advantages of being non-invasive and inexpensive. Two techniques are used to detect RH: direct visualization of the renal arteries and analysis of Doppler waveforms.
Direct visualization of the renal arteries includes ultrasound examination of the main renal arteries with color or power Doppler studies, analysis of blood flow velocity in the renal arteries. Signal enhancement can be achieved by administering a contrast agent, which facilitates visualization of the renal arteries.
Three-dimensional ultrasound angiography allows detailed visualization of the renal arteries; the accuracy of the image is comparable to three-dimensional magnetic resonance angiography.
Four criteria are used for ultrasound diagnosis of significant proximal renal artery stenosis or occlusion:
1) an increase in the maximum systolic velocity in the renal artery (in the literature, the threshold for significant stenosis of the renal artery is 100-200 cm/s); 2) the renal-aortic coefficient of maximum systolic velocity is greater than 3.5; 3) turbulent flow in the poststenotic region; 4) visual observation of the renal artery without a detectable Doppler signal, indicating occlusion.
In addition, with the help of ultrasound it is possible to identify indirect signs of ARH, in particular, a decrease in the size of the kidneys due to its ischemic atrophy. Kidneys less than 7-8 cm in length are usually severely damaged by ischemia. In these circumstances, revascularization usually does not restore function or eliminate hypertension, and nephrectomy is indicated in these patients.
Magnetic resonance angiography
with contrast Gadolinium is now available as a high-resolution imaging system with high quality three-dimensional images. Blood appears bright, while immobile tissue remains dark. Subtraction of unenhanced images removes all background signals and improves vascular signals.
Spiral computed tomography angiography (CTA)
is a non-invasive method, however, requiring the administration of 50-100 ml of contrast agent intravenously. It can be adapted to measure renal blood flow in patients with renal renal hypertension and can also provide three-dimensional images of blood vessels.
How does it manifest?
There are no specific symptoms characteristic only of renovascular arterial hypertension, except for high blood pressure numbers. Damage to the glomerular system leads to persistent vascular hypertension, which is manifested by a small difference between high numbers of systolic and diastolic pressure. Patient complaints are individual in each case and depend on the presence of kidney disease. An experienced physician will suspect renovascular hypertension if antihypertensive drugs do not have the desired effect or if there is a history of inflammation, trauma, or vascular pathological processes. Heredity does not play a significant role in the occurrence of renal hypertension. Laboratory studies show signs of renal failure.
Diagnostic tactics.
The first step in diagnosing renovascular hypertension is clinical diagnosis and selection of patients with an average and high probability of this pathology according to clinical criteria. Non-invasive screening tests provide targeted selection of patients with a high likelihood of renal artery stenosis who should undergo X-ray examination.
Spiral CT can provide excellent visualization of the renal vessels (Fig. 1), but requires large amounts of contrast. Currently, magnetic resonance angiography provides a good image of the renal vessels without risk to the patient.
But, with its higher cost and lower availability, it should be reserved for patients with indeterminate functional imaging findings but a high clinical suspicion of ICH, and patients who have a contraindication to standard angiography: renal failure or allergy to iodine drugs.
Rice. 1.
CT angiography. Stenosis of the right renal artery (indicated by an arrow)
Treatment.
In the natural course of the disease and the absence of appropriate treatment, about 70% of patients die over the next 5 years from complications of systemic arterial hypertension (cerebral stroke, myocardial infarction, renal failure).
Conservative treatment in most patients with renovascular hypertension is ineffective or gives an inconsistent and short-lived effect. Even if it was possible to achieve a decrease in blood pressure, with persistent stenosis of the renal artery, an even greater disruption of the blood supply to the kidney occurs and secondary shrinkage of the kidney will soon develop with a complete loss of its function.
Long-term drug therapy is justified only if surgical intervention is impossible and as an addition to surgery if it does not lead to a decrease in blood pressure.
The main methods of treatment for patients with renovascular hypertension are x-ray endovascular dilatation (RED) of the renal arteries and surgery.
Indications for performing RED of the renal arteries are monofocal stenosis of the renal artery in fibromuscular dysplasia and atherosclerotic stenosis of the proximal segment of the renal artery, as well as stenosis of the segmental branches of the renal artery.
The diameter of the dilatation catheter balloon is selected depending on the diameter of the unaffected part of the renal artery and should exceed it by 10%. The main principle of balloon dilatation is its repeated implementation with a gradual increase in pressure in the balloon. In recent years, to prevent restenosis, the procedure has been supplemented with renal artery stenting.
Indications for surgical treatment.
An accurately established diagnosis of renovascular hypertension, if it is impossible to perform RED and stenting or their ineffectiveness, is an indication for surgical treatment.
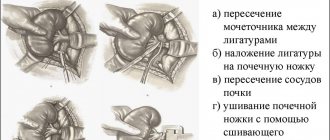
There are 3 types of open operations for VRG.
1) reconstructive operations on the renal arteries, 2) conditionally reconstructive operations, 3) nephrectomy.
In the presence of hemodynamically significant narrowing (more than 50%) or occlusion of the renal artery, it is necessary to perform an intervention aimed at restoring the main renal blood flow. Contraindications to surgery are severe heart failure, acute disorders of cerebral and coronary circulation less than 3 months ago, as well as shrinkage of both kidneys.
Approximately 30-35% of patients with ARH have bilateral stenoses of the renal arteries. For hemodynamically equivalent lesions, a tactic of staged operations (with an interval of 3-6 months) is advisable, and to facilitate the implementation of the future, second stage, one must begin with reconstruction of the right renal artery with extensive mobilization of the aorta and ligation of 2-3 lumbar arteries.
Simultaneous reconstruction of the renal arteries is used in case of multiple stenoses of the renal arteries or in patients with aortitis, when reconstruction of the renal and visceral arteries is planned. In cases of renal artery lesions of unequal degree, blood flow should initially be restored on the side of the larger lesion.
In patients with hemodynamically significant stenosis on one side and a shriveled kidney on the other, first of all, it is necessary to restore blood flow on the side of the stenosis and, subsequently (after 3-6 months), if hypertension persists, perform nephrectomy on the other side.
In case of frequent combined lesions of the renal and brachiocephalic arteries, the question of the priority of revascularization of each of these areas is decided depending on the results of the test with artificial hypotension. Lack of cerebral tolerance to a decrease in blood pressure indicates the need for an initial restoration of cerebral blood flow. Operational access.
Access to the renal artery can be achieved using thoracophrenolumbotomy, median or superior transverse laparotomy. We give preference to thoracophrenolumbotomy, which provides optimal conditions for any type of reconstruction of all parts of the renal arteries and abdominal aorta.
It gives the smallest depth of the surgical wound and the largest angle of the surgical action. This most important circumstance allows us to consider thoracophrenolumbotomy as the access of choice for renovascular hypertension.
Symptomatic arterial hypertension (AH), which occurs against the background of a violation of the main blood flow of the kidneys without visible damage to the parenchyma, is called renovascular. Occurs in 1-15% of people suffering from high blood pressure. The main cause of the disease is vasorenal conflict.
Why does vasorenal conflict occur?
Vasorenal conflict refers to the presence of an additional renal artery or an abnormal passage of its branch. This leads to compression of the ureter and difficulty in the outflow of urine, which provokes expansion of the pelvis. Vasorenal conflict can be congenital or acquired. In the first case, the causes of pathology are:
- fibromuscular dysplasia;
- aneurysm of arteries in the kidneys;
- renal artery hypoplasia;
- vascular fistulas;
- extravasal compression of the renal arteries.
Vasorenal conflict can occur against the background of thrombosis and embolism of the renal artery, neoplasms in the kidneys, and vascular sclerosis. Of the acquired diseases, the causes of pathology are:
- dissecting aortic aneurysm;
- nephroptosis;
- glomerulonephritis;
- pyelonephritis;
- systemic vasculitis;
- Takayasu's disease;
- malignant neoplasms;
- atherosclerosis;
- urolithiasis disease;
- traumatic aneurysm of the renal artery;
- kidney infarction.
Symptoms of the disease
Please note that 25% of patients with renovascular hypertension are asymptomatic. Due to the nonspecificity of symptoms, doctors face a number of difficulties when making a diagnosis. The main symptoms of renovascular hypertension:
- pain in the eyeballs;
- heaviness in the head;
- headache;
- noise in ears;
- muscle weakness;
- memory impairment;
- heartbeat disturbance;
- pain in the heart area;
- pain and heaviness in the lumbar region;
- heaviness in the chest.
Symptoms of vasorenal arterial hypertension
The disease does not have any specific symptoms; they may vary depending on the stage of development of the pathology. However, there are some manifestations that occur in the vast majority of cases. These include:
- Regular headaches;
- Ringing in the ears, flickering of “flies” before the eyes;
- Sleep disturbance (insomnia);
- Feeling of chest tightness;
- Heart rhythm disturbances;
- Pain in the lumbar region;
- Frequent urination;
- Increased thirst.
The disease in all cases is accompanied by high blood pressure, sometimes not amenable to drug therapy. Most often, it is possible to lower the levels only after the main cause of renovascular hypertension has been eliminated.
Note. Although there are no specific symptoms, with this pathology both diastolic and systolic indices are most often elevated, but the difference between them will be very small.