Nephrosclerosis must be understood as a disease associated with the replacement of renal parenchyma with connective tissue. This process contributes to the wrinkling of the organ and its compaction.
As a result of the disease, the functioning of the kidneys is impaired. In medicine, this condition is called a shriveled kidney.
Renal sclerosis can be of two types, depending on the mechanism of development:
- primary (begins due to impaired blood supply to the kidneys, hypertension, atherosclerosis, and other vascular pathologies);
- secondary (accompanies some kidney diseases, congenital anomalies, nephritis).
Nephrosclerosis is often diagnosed not only in humans, but also in some animals. To identify the disease, it is enough to take a urine test and do an ultrasound.
Characteristics of the disease
What is nephrosclerosis? The term hypertensive nephrosclerosis has traditionally been used to describe a clinical syndrome characterized by long-term hypertension, hypertensive retinopathy, left ventricular hypertrophy, minimal proteinuria, and progressive renal failure. So, what is kidney nephrosclerosis, a health condition associated with kidney damage due to chronic high blood pressure, in which tissue is replaced by connective tissue and the kidney itself shrinks in size (“shrinks”). This leads to malfunctions up to the complete cessation of the functioning of the organ. The disease can be divided into two types: benign and malignant. Benign nephrosclerosis is common in people over 60 years of age. The malignant form is rare and affects 1-5% of people with high blood pressure (diastolic blood pressure above 130 mm/Hg). Hypertensive disease must be distinguished from renovascular hypertension, which is a form of secondary hypertension. It is customary to distinguish two forms of this disease:
- primary wrinkled kidney—develops as a result of damage to the kidney vessels;
- Secondary wrinkled kidney - damage to the kidney tissue (parenchyma) in various diseases.
ICD code -10 –I12.
Use of medications
This disease is treated in specialized nephrology centers. It comes down to eliminating the main provoking factor. Attempts to restore lost kidney function without the first step are usually unsuccessful.
Treatment is always comprehensive and long-term. Depending on the clinical picture and general condition of the patient, the following medications may be required:
- Anticoagulants (Heparin) to prevent blood clots.
- Medicines to lower blood pressure.
- ACE inhibitors (Diroton, Berlipril) to dilate the blood vessels of the kidneys.
- Diuretics, which remove excess fluid from the body.
- Calcium antagonists that promote dilation of arteries (Falipamil).
- Multivitamin complexes.
For other disorders caused by kidney dysfunction, medications are selected individually.
Nephrosclerosis symptoms and risk group
It cannot be said that the disease is asymptomatic; it’s just that not everyone seeks medical help on time, attributing all the symptoms to fatigue, a cold, overeating, etc. Classic symptoms of chronic kidney disease:
- loss of appetite;
- urinary disorders;
- decrease in urine volume;
- the presence of constant pulling pain in the lower back;
- nausea;
- vomit;
- high blood pressure;
- itching;
- drowsiness or confusion;
- change in the appearance of urine (bloody, dark, strong-smelling, foamy);
- weight loss and bad taste in the mouth.
Symptoms may appear mild, but develop over time and become a chronic condition of the body. The risk group includes people with:
- poorly controlled moderate to high blood pressure;
- elderly age;
- other kidney diseases.
Clinical picture
Nephrosclerosis, also known as “shrunken kidney,” is quite difficult to identify in the initial stages, since there are no characteristic symptoms. The patient does not experience any discomfort. Only when you consult a doctor with other complaints and after a diagnostic examination does it become possible to identify abnormal processes.
When the disease becomes stable, the following signs appear:
- swelling of the face and limbs;
- the number of urges to urinate increases, but the volume of urine produced decreases;
- pain in the lumbar area;
- strong thirst;
- high blood pressure;
- fatigue, weakness;
- itching of the skin.
The listed symptoms of kidney nephrosclerosis should be a reason to undergo a more in-depth medical examination. Only after receiving its results can you begin therapy.
Cause of nephrosclerosis
Nephrosclerosis is not an independent disease. The term "hypertension" is used to refer to high blood pressure, and "nephropathy" refers to kidney damage. It follows that the disease is caused by chronic high blood pressure, which causes damage to kidney tissue, including small blood vessels, glomeruli, renal tubules and interstitial tissues. The tissue hardens and thickens. Constriction of blood vessels means that less blood flows into the tissue, which reduces the supply of oxygen, leading to tissue death (ischemia).
Mechanism of occurrence
As a result of benign arterial hypertension in the kidneys, hyaline (pink, amorphous, homogeneous material) accumulates in the walls of small arteries and arterioles, causing thickening of their walls and narrowing of the arterial openings, that is, a process known as atherosclerosis occurs. The resulting impaired blood flow causes tubular atrophy, interstitial fibrosis, glomerular changes, and scarring around the glomeruli. Additional complications often associated with hypertensive nephropathy include damage to the glomeruli, leading to protein and blood in the urine. Hypertensive nephropathy refers to kidney failure that can be attributed to a history of hypertension. However, despite the known association between hypertension and chronic kidney disease, the underlying mechanism remains unclear.
Diagnostics
The basis of nephrological diagnostics are laboratory tests (urine and blood tests), as well as X-ray diagnostics and ultrasound of the kidneys. These studies must be carried out for each person once a year. In the presence of diseases such as diabetes mellitus, arterial hypertension, vascular atherosclerosis, obesity (risk group for chronic nephrosclerosis), it is necessary to conduct a more in-depth study, for example, a test for microalbuminuria, determine the level of creatinine in the blood, perform a Zimnitsky test (determining the relative density of urine ) and conduct other specific studies.
One of the effective diagnostic methods for kidney diseases is ultrasound.
Glomerular ischemia, hypertension and hyperfiltration
High blood pressure can damage the endothelium, commonly known as the lining of a blood vessel, in the long term. This leads to the accumulation of plaques that settle in the renal arteries, causing stenosis and coronary kidney disease. In this situation, the organ supplied by the narrowed artery suffers from inadequate blood flow, which in turn reduces its size. An alternative mechanism for hypertensive nephropathy is prolonged glomerular hypertension and hence glomerular hyperfiltration. They can occur simultaneously, but do not have to. The idea is that hypertension leads to glomerular sclerosis, which ultimately means decreased kidney function. As a compensatory mechanism, unaffected nephrons relax to increase blood flow to the kidney perfusion and increase glomerular filtration through the intact glomeruli.
Methods for detecting renal pathology
For effective treatment, kidney nephrosclerosis in a child requires timely diagnosis. However, it is complicated due to the appearance of pronounced symptoms only in the later stages. Therefore, the patient’s treatment occurs late. The outcome in such cases is negative. Kidney nephrosclerosis is diagnosed using laboratory and instrumental methods. The first include:
- Blood chemistry. Renal dysfunction is determined by elevated levels of urea, creatinine and uric acid. In addition, total protein decreases. In the last stages of the disease, the levels of magnesium, phosphorus and sodium increase.
- General urine analysis. The disease is determined by increased protein content and the appearance of red blood cells in the urine. At the same time, the relative density of urine decreases.
- General blood analysis. With nephrosclerosis, the level of hemoglobin and platelets decreases.
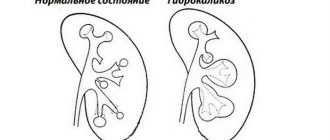
Using instrumental methods, not only the kidneys, but also its vessels are examined. One of the common diagnostic procedures is ultrasound examination. On ultrasound, doctors identify such signs of nephrosclerosis as atrophy of the renal cortex, calcium deposition in the renal tissue and lack of separation between the renal cortex and medulla.
To detect nephrosclerosis, X-ray examination methods are performed, such as excretory urography of the kidney and angiography of the kidney vessels. In both cases, the administration of a contrast agent is necessary.
Using excretory urography, the volume of the kidney is determined and based on the obtained indicators, doctors can judge whether it is reduced or not. Vascular angiography is necessary to assess the state of the blood supply to the kidneys.
In the images, specialists can detect narrowing and kinking of the renal artery. This indicates that the kidney does not receive the necessary nutrition and its tissue gradually dies. In addition, doctors can determine the disturbance of blood supply in the renal vessels using Doppler - it will show its slowdown.
Treatment of kidney nephrosclerosis and prognosis
The goal of therapy is to slow the progression of chronic disease by lowering blood pressure and albumin levels. Ideal blood pressure <130/80 mm Hg. for patients with hypertensive nephropathy, because research shows that anything above or below this can increase the risk of cardiovascular disease. It is recommended to change your lifestyle: weight loss, exercise, reducing salt intake, giving up bad habits. A patient's prognosis depends on many factors, including age, ethnicity, blood pressure, and glomerular filtration rate. Lifestyle changes (reducing salt intake, increasing physical activity, etc.) have been shown to improve outcomes, but are not sufficient without pharmacological treatment. The malignant form of kidney nephrosclerosis requires surgical treatment, which usually involves removal of the affected organ (nephrectomy). This operation can be performed in several ways. In particular, it is possible to perform abdominal or laparoscopic surgery, as well as endoscopic percutaneous retroperitoneal nephrectomy. In particularly severe cases, the patient is transferred to hemodialysis or undergoes a donor kidney transplant. Video: Nephropathy
Nutritional Features
An excellent addition to the course of treatment is to follow a fairly strict diet. Nutrition for kidney nephrosclerosis is selected by the doctor individually for each patient. Typically, the following principles are followed:
- Limit protein intake. However, you cannot completely abandon it. When choosing protein foods, preference should be given to poultry, fish and dairy products. It is important to completely exclude potatoes, cereals and bread from the diet.
- The diet must necessarily include seafood, but you should not abuse them due to their high phosphorus content.
- Limiting table salt consumption. At any consultation, the nephrologist will say that at stages 1-2, up to 15 g of salt per day is allowed, and at stages 3-4 this amount is halved. You cannot completely abandon this spice, as the likelihood of dehydration increases.
- Be sure to include potassium-rich foods in your diet. For example, bananas, dried apricots, raisins.
- Nutrition should be as balanced as possible, containing the required amount of calories and vitamins.
Most patients are forced to adhere to this diet for the rest of their lives.