Renal pressure, or diastolic, indicates the condition of the vessel walls.
Its excessive increase or decrease indicates the development of pathologies in the kidneys and renal vessels. The cause of high blood pressure is traditionally associated with cardiovascular disease. However, not everything is so simple. In approximately every 7 patients, high blood pressure is caused by narrowing of the renal blood vessels.
This phenomenon is called increased renal pressure or renal hypertension.
What it is?
Renal pressure is a diastolic blood pressure indicator, the value of which deviates from the norm as a result of malfunctions in the renal system. The disease is diagnosed in 20-30% of hypertensive patients.
The kidneys filter the blood, remove excess fluid, breakdown products and harmful substances that accidentally enter the bloodstream. When the water-electrolyte balance is disturbed and the depressor system is suppressed, the organ begins to function incorrectly: the influx of plasma decreases, water and sodium are retained, causing swelling. Due to excess sodium ions, the walls of the arteries swell. Vessels become more sensitive. Kidney receptors begin to synthesize an excess amount of the enzyme renin, which is transformed into angiotenis, and then into aldosterone. These elements are responsible for vascular tone, reduce the lumen of the arteries and lead to an increase in pressure.
Normally, lower (renal) pressure is in the range of 60-90 mmHg. Art. The upper reading of the tonometer should not exceed 140 mmHg. Art. With hypertension of renal origin, blood pressure can increase to 250/150-170 mm Hg. Art. The difference between systolic and diastolic readings ranges from 100 to 120 units.
Some disorders of the filtering organ can provoke a decrease in the tonometer numbers. But such a symptom is extremely rare.
The connection between kidneys and blood pressure
Nephrogenic arterial hypertension (renal pressure) is a disease that most often affects people in the older age category. You can cope with it only by following all the recommendations of a specialist. Kidneys and blood pressure have a close relationship. That is why people with disorders of the excretory system often have increased blood pressure.
The kidneys are a paired organ of the excretory system that is responsible for:
- blood filtration to cleanse it of harmful chemical components;
- removing excess fluid from the body.
With poor functioning of the organ and the presence of an excessive amount of fluid in the blood, blood pressure increases. Hypotension may also occur. This may be due, on the contrary, to an insufficient amount of fluid in the blood.
People with certain cardiovascular diseases are often prescribed diuretics (water pills). Taking them is essential for normalizing kidney function. Thanks to such drugs, blood vessels are cleansed of excess fluid.
Blood pressure levels may be elevated due to the presence of various diseases. This is also possible due to congenital abnormalities of the kidney tissue. The occurrence of hypertension may be due to the inability of the kidneys to fully remove salt deposits. The close connection between the paired organ of the excretory system and blood pressure is obvious. Increased blood pressure levels contribute to damage to kidney tissue, and this only aggravates the situation. Arterial hypertension occurs in almost all people with disorders in the functioning of the excretory internal organ.
Therapeutic strategy
Treatment of renal hypertension, the symptoms of which are similar to hypertension, aims to normalize blood pressure and slow the progression of renal failure, thereby improving the patient’s well-being and increasing life expectancy. Newly diagnosed nephrogenic disease or suspicion of it is a direct indication for hospitalization to clarify the etiological factor of high blood pressure.
Drug treatment
Pharmacotherapy should be selected exclusively by a doctor. Medicines are needed to bring blood pressure back to normal and improve the functional state of the kidneys. Even taking into account the fact that traditional antihypertensive drugs are used to treat pathology, without consulting a nephrologist, taking them with a high degree of probability will not have the desired therapeutic effect. The standard treatment regimen for hypertension of renal origin includes the following groups of drugs:
- beta blockers (Atenolol, Metoprolol, Nebivolol);
- ACE inhibitors (Captopril, Enalapril, Fozinopril);
- diuretics (Furosemide, Indapamide, Spironolactone);
- calcium channel antagonists (Verapomil, Diltiazem, Lacidipine).
Beta blockers neutralize the effects of epinephrine and norepinephrine on special receptors in the heart, resulting in a decrease in heart rate and stabilization of blood pressure. Angiotensin-converting enzyme inhibitors reduce the production of the main mineralocorticosteroid hormone of the adrenal cortex (aldosterone), which prevents an increase in vascular tone.
Hypertensive patients are recommended to take a course of these drugs. The daily dosage is selected individually, taking into account the form of the disease, age and weight of the patient. Thanks to their prolonged action, such tablets allow you to keep your blood pressure under control throughout the day, even with a single dose.
Diuretics utilize excess fluid from the body, preventing the formation of edema, improve kidney function and normalize blood pressure. Calcium antagonists protect the heart muscle from dystrophic changes. For the treatment of nephrogenic hypertension, patients are often prescribed drugs based on Amlodipine. In addition, products of chemical and herbal origin, which are designed to improve the functioning of the organs of the urinary system, provide tangible benefits in the fight against the disease.
Surgical intervention
If a salt-free diet and medication do not bring any results, then it is advisable to think about surgery. Surgical intervention allows you to completely restore vascular patency. Modern clinics are equipped with equipment that allows them to perform high-tech operations with minimal risk to health. The following surgical techniques demonstrate excellent results in the treatment of renal hypertension:
- Percutaneous balloon angioplasty. Using a catheter equipped with a balloon, the specialist straightens the stenotic areas of the arteries. The obvious advantage of this manipulation is the fact that the patient is not under general anesthesia during the operation, and the intervention itself takes very little time. In rare cases, complications occur in the form of rupture of a vessel or exacerbation of bleeding.
- Open angioplasty. The essence of the operation is to remove atherosclerotic plaques and reconstruct the affected area of the renal artery, for which one’s own vessels or prostheses are used. The advantage of the technique is that the patient’s blood flow is completely restored and deposits that provoke an inflammatory reaction are removed. Old age should be considered a contraindication to surgery, since the likelihood of cardiovascular complications is high.
Causes of development and possible diseases
Diastolic pressure is considered low when its level is up to 60 mmHg. Art. This phenomenon occurs both as a result of normal processes in the body (young or old age, pregnancy) and in pathologies. The following diseases cause its decrease:
- kidney disease (glomerulonephritis, pyelonephritis);
- cardiovascular;
- gastrointestinal ulcer;
- intoxication due to inflammation;
- allergic reaction;
- exacerbation of autoimmune pathologies;
- oncology;
- severe dehydration;
- hormonal imbalances.
These factors provoke a deterioration in the patency of blood vessels, their filling with blood and, as a consequence, a drop in renal pressure. However, this indicator can also increase in various pathological conditions. So, it is called high at a level above 90 mm Hg. Art. An increase in pressure occurs due to:
- renal failure;
- hyperfunction of the thyroid gland;
- cardiovascular diseases;
- diabetes;
- long-term use of nervous system stimulants (medicines and caffeine);
- stress.
These reasons affect not only the diastolic pressure, but also the condition of the body as a whole. This explains changes in a person’s well-being with lower blood pressure disorders.
Symptoms of the disease
The complex is formed from the symptoms of hypertension and underlying kidney disease. The manifestation of symptoms depends on the form of the disease: benign develops gradually, malignant develops rapidly.
The first option is characterized by stable blood pressure with a predominant increase in diastolic pressure. Complaints of shortness of breath, loss of strength, discomfort in the heart.
The second option is characterized by increased blood pressure and a sharp weakening of vision (up to its complete loss). This is due to poor blood circulation in the retina. Complaints of acute headache accompanied by vomiting and dizziness.
Typical signs of the pathology are similar to the symptoms of arterial hypertension: dizziness and headaches, panic attacks, decreased brain activity ( memory problems, decreased concentration ).
Renal hypertension usually manifests itself against the background of kidney damage in certain diseases (pyelonephritis, diabetes mellitus, glomerulonephritis), so its symptoms are always associated with the underlying disease.
Common complaints include:
- pain in the lumbosacral spine;
- frequent urge to urinate;
- double increase in daily urine output;
- periodic increase in temperature;
- fatigue, general malaise.
The disease begins suddenly, the increase in pressure is accompanied by pain in the lumbar region. The tendency to hypertension can be inherited from hypertensive parents. Conventional medications designed to lower blood pressure do not work in such situations.
The clinical picture of PG depends on the degree of change in blood pressure, the initial condition of the kidneys, complications (heart failure, heart attack, damage to the retina and cerebral vessels).
Classification
The mechanisms described above are implemented due to a variety of diseases and pathologies. The disease is classified depending on its form. Vascular ischemia of the kidney is caused by congenital or acquired pathologies.
- Congenital diseases - vasorenal form, include the following: fibromuscular dysplasia of the artery - stenosis of the vessel wall;
- renal artery aneurysm;
- hypoplasia of the artery - congenital underdevelopment;
- aortic anomaly;
- Kidney fistula – arteriovenous.
- Renal artery stenosis – blockage by an atherosclerotic plaque or thrombus;
- cyst;
Etiology and pathogenesis
The main causes of renal hypertension:
- congenital kidney defects: abnormal structure, insufficient volume, double structure;
- inflammatory processes: pyelonephritis, other inflammatory nephrodiseases.
Factors that increase blood pressure can be congenital or acquired. Congenital causes:
- renal artery stenosis;
- aortic stenosis;
- coarctation of the aorta;
- proliferation of vascular tissue.
Acquired causes of high blood pressure include:
- nephropathy due to diabetes mellitus;
- atrophic disorders of kidney tissue due to age-related changes;
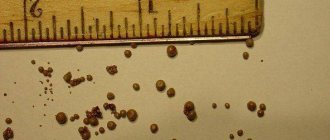
- urolithiasis;
- fibrous capsular contracture.
Arterial hypertension often develops with renal failure. In the absence of timely diagnosis and treatment, the pathology can lead to death. At the first signs of renal hypertension, you should consult a doctor; delaying the examination can cost your life.
Urolithiasis is one of the factors in the development of renal hypertension
Hypertension of the renal arteries can develop against the background of other diseases:
- Libman-Sachs disease;
- complications of diabetes;
- scleroderma;
- liver diseases;
- classic hypertension.
Symptoms and first signs
In adults, pathology manifests itself in two groups of signs: symptoms of high blood pressure and manifestations of kidney disease.
The slow-onset form of renal pressure can be recognized by the following symptoms:
- persistent high blood pressure (both upper and lower);
- headache;
- dizziness;
- reduced performance;
- muscle weakness;
- dyspnea;
- feeling of palpitations and discomfort in the chest.
In the fast-flowing form, the following symptoms appear:
- strongly increased lower pressure (120 mm Hg and above);
- decreased visual acuity;
- constant headache, especially in the back of the head;
- dizziness;
- nausea and vomiting.
With any form of nephrogenic arterial hypertension, in addition to the listed symptoms, the patient also complains of pain in the lumbar region (dull, pulling or sharp).
How to diagnose
Diagnostics consists of several stages. First of all, you need to collect anamnestic data (time of onset of the disease, whether there is an effect from medications, whether there is heredity, connection with kidney disease, malignancy of the course). Based on a detailed survey, the origin of hypertension can be assumed.
Correct measurement of blood pressure is important. As a rule, with renal hypertension, a significant increase in numbers is detected, much more than with the usual form of the disease. There is an increase in diastolic pressure and a decrease in pulse pressure. When measuring, it is necessary to take into account the numbers from both the right and left hands. If there is a significant difference between them, then nonspecific aortoarteritis occurs.
Diagnostics
Diagnosis is carried out comprehensively, since there are no characteristic complaints from the patient. To make a correct diagnosis, the doctor must carefully evaluate the clinical picture, how long ago symptoms appeared, and the results of laboratory and instrumental studies.
The patient is prescribed:
- Analysis of urine. Makes it possible to evaluate kidney function and identify functional disorders.
- Ultrasound of the kidneys. Necessary to identify structural abnormalities of the organ.
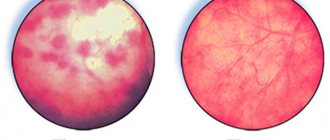
- Contrast radiography. Clearly shows the structure of the kidney and the presence of pathological inclusions.
- Angiography. Provides broad information about the condition of the vessels, the width of their lumen, the presence of blood clots, atherosclerotic plaques and other inclusions, allowing one to assess the size and functionality of the arteries.
- MRI. Appointed for a detailed examination of the structure and functioning of the organ.
In parallel, the doctor can give a referral to a cardiologist to rule out cardiac causes of increased blood pressure. It is impossible to cure hypertension without detailed diagnostics. Only drugs whose mechanism of action is aimed at eliminating the main problem will help lower blood pressure.
Diagnostic procedures
The first stage of diagnosis involves a thorough general medical examination, as well as targeted familiarization with the patient’s complaints and collection of anamnestic data. In making a diagnosis, an important role is played by measuring blood pressure in the upper and lower extremities, auscultation of the heart muscle and large arteries.
General and biochemical blood tests are mandatory. The latter is necessary to determine the quantitative content of electrolytes, urea and creatinine in the blood mass. They also perform a general urine test, samples (according to Zimnitsky and Kakovsky-Addis), and bacteriological examination of urine.
Instrumental diagnostic methods such as ultrasound examination of parenchymal organs and dynamic renal scintigraphy make it possible to identify the root cause of high blood pressure. Detection of damaged renal vessels is carried out using traditional aorthrography, selective or digital subtraction angiography.
At the final stage, in order to clarify the nature of hypertension, determine the functional significance of the affected arteries, and also develop optimal intraoperative tactics, the patient is required to undergo a radioimmunological study of the level of renin in blood taken from the renal vein. Recently, a pharmacoradiological test with Captopril has been increasingly used to diagnose renovascular hypertension.
How to treat kidney pressure?
Treatment is aimed at treating the underlying renal pathology and relieving symptoms. The only way to reduce renal pressure is with medications:
- ACE inhibitors – enalapril, lisinopril, captopril. They inhibit the action of the enzyme that converts angiotensin I to angiotensin II. This eliminates the constant support of blood vessels in tone;
- α-blockers – prazosin, butyroxane. The tablets interfere with the action of adrenaline and norepinephrine, which stimulate an increase in blood pressure; calcium antagonists – normodipine, amlodipine. They reduce the level of calcium absorption and thereby relieve muscle fibers, in particular the heart muscles, from excess tension;
- Angiotensin II receptor antagonists - losartan, candesartan. The drugs reduce the sensitivity of receptors that, when angiotensin appears, signal the synthesis of aldosterone;
- Diuretics – spironolactone, furosemide. Facilitate the removal of fluid and excess sodium ions.
The therapeutic course is selected individually and in accordance with the nature of the underlying disease. The answer to the question of how to treat increased renal pressure necessarily includes a diet that limits the amount of salt.
It is important to restore normal hemodynamics, water balance in the body, remove excess fluid, normalize cardiac activity, and the nature of glomerular filtration. Among the ways to radically eliminate renal manifestations, conservative and surgical techniques can be distinguished. The selection of a specific regimen is made by the doctor. The list of drugs is wide: non-steroidal anti-inflammatory drugs, glucocorticoids in different dosages, antibacterial agents and antiseptics for internal use, etc.
- Pyelonephritis is treated with anti-inflammatory drugs and antibiotics.
- For glomerulonephritis, immunosuppressants are used, but with caution.
- Nephritis is eliminated in the same way as pyelonephritis, but surgical intervention is possible.
Surgical treatment is indicated in a strictly limited number of cases, if there is no other option.
The following basic methods are used:
- angioplasty - a catheter is inserted through an artery into a narrowed vessel, compressed air is passed through the latter so that it expands the walls of the vessels, returning them to their original state;
- stenting - instead of air flow, the vessel expands with a stent;
- bypass surgery - in this case, severely damaged areas of veins and arteries are excised, and the blood is redirected through healthy vessels.
Treatment of renal hypertension
We have looked at how the kidneys affect blood pressure, now we need to evaluate the treatment offered by medicine and decide what actions should be taken if problems arise. If your blood pressure has increased, you should first visit a cardiologist to identify the exact cause of this phenomenon. If the reading decreases, the need for consultation becomes urgent as immediate medical attention may be required.
It is important to remember that you cannot reduce blood pressure at your own risk; medications must be prescribed by a doctor. In this case, the causes become the “stumbling block” - not knowing what factors caused the disease, the victim can completely destroy the kidneys in attempts to regulate blood pressure levels. Treatment of the disease begins only after a comprehensive examination, and the following methods can be used:
- Surgical intervention if cysts, neoplasms and other pathologies form, which cannot be removed by other means.
- Drug therapy with the prescription of tablets - this method is in demand if the cause of the pathology is excessive or insufficient production of renin.
- With the development of arterial hypertension, treatment should be carried out against the background of diet therapy.
- Traditional recipes can be used as an additional and preventive method. Herbal mixtures from which tinctures and decoctions are prepared can demonstrate good results, but it is advisable to first consult with specialists.
As for drugs that are usually prescribed for therapeutic purposes, it is mandatory to take diuretics, which include Furosemide, Hydrochlorothiazide, Amiloride, Triamterene and others. Lisinopril and Enalapril are prescribed, which are ACE inhibitors. Among β-adrenergic receptor blockers, the most popular are Atenolol, Labetalol, and Carvedilol. Vitamin complexes, potassium preparations, calcium antagonists are also prescribed - the latter include Nifedipine and Verapamil.
The drugs serve to normalize blood pressure, and after achieving the goal, they begin to eliminate the underlying pathology. If there are problems with the renal vessels, arterial bypass or balloon dilatation is performed.
If there are no signs of organ functioning, the phenomenon is regarded as a direct need for removal and nephrectomy is performed. In cases where there is chronic renal failure, hemodialysis is prescribed.
Even if measures to normalize the condition were carried out successfully, sudden changes in pressure should not be allowed in the future. The most effective is complex treatment, when drugs are taken against the background of a diet, accompanied by a correct diet and lifestyle, and the drinking regime is not ignored.
Folk remedies
Folk remedies in combination with other treatment methods help to quickly get rid of blood pressure problems. To normalize blood pressure, the following means are used:
- The most popular collection includes thyme, bear's ears, elecampane, birch leaves, marigold, dill seed and immortelle. A mixture of 3 tablespoons of each herb is poured into 2 liters of boiling water and left for 5-6 hours. The infusion is intended for use within 1 day.
- Kefir. Doctors advise people with hypertension to drink this fermented milk product, as it can reduce blood pressure. Moreover, it can not only be taken orally, but also used to create medicinal masks. To do this, kefir is rubbed daily into the skin of the face and scalp.
- Medicinal herbs. Herbal remedies are considered the most effective and safe. To create medicinal mixtures, oats, chamomile, St. John's wort and strawberries are used.
- Delicious and healthy tea is obtained from lingonberry leaves: pour 3 tablespoons of leaves with a glass of boiling water and leave for 2 hours. You should drink half a glass before meals.
To get rid of renal hypertension quickly at home, it is recommended to use home remedies. To do this, you will have to take a napkin or terry towel and moisten it with cooled water. Then a damp towel is placed on the forehead for 35-40 minutes. Such a cooling compress will lead to a temporary decrease in lower and upper blood pressure.
Nutrition and diet
When treating renal pressure, patients are prescribed a special diet. They are advised to exclude certain foods. These include:
- salt;
- fried and fatty foods;
- spicy foods;
- products with a high content of various seasonings.
All of these foods contribute to the worsening of nephrogenic hypertension. After their consumption, the level of blood pressure increases, which in turn destroys kidney tissue. The performance of the excretory paired organ is significantly deteriorated. Experts also recommend avoiding drinking tea, coffee and other drinks that contain caffeine. Drinking alcohol is also prohibited.
The patient is advised to give preference to only moderate physical activity. The sick person should include the following foods in their diet:
- Sea kale. This food component saturates the body with useful microelements. Sea kale contains a huge amount of vitamins.
- Onion and garlic. Such food products not only have a positive effect on kidney function, but also relieve a person of germs. They normalize blood pressure and restore the body's protective functions.
- Fresh juices from vegetables. They prevent the formation of kidney stones and include a large amount of vitamins. They can be prepared from celery, parsley and coriander.
- Cranberries and lingonberries. Such berries have a positive effect not only on the kidneys, but also on the entire body as a whole.
- Fish and fish oil. Such products contain phosphorus necessary for the body. There are also many useful microelements.
It is no coincidence that you need to stop eating salt. This food supplement retains excess fluid in the body. This negatively affects the health of not only people with kidney pressure, but also those who do not have any pathologies. You can consume no more than 4-5 grams of salt, and it is better to avoid it altogether.
The patient should avoid eating canned foods and various deli meats. As a rule, they contain a huge variety of seasonings. You should not eat salted fish. It contains an excessive amount of salt.
Prevention
All preventive measures are based on the general maintenance of the health of the blood vessels of the heart and kidneys. These organs are closely interconnected, and therefore influence each other. To avoid the development of the disease, it is necessary to adhere to proper nutrition: reduce the consumption of salt and animal fats. It is also recommended to follow a daily routine. Do morning exercises regularly, treat yourself to walks in the fresh air, go to bed and get up at the same time every day. Rid your body of the negative effects of bad habits.
Forecast
With timely and properly selected treatment, the prognosis is favorable.
It worsens in the case of rapid progression of the renovascular form of the disease and in the absence of adequate treatment of any form, since irreversible changes occur in the renal tissue.
With an advanced parenchymal form and bilateral kidney damage, the prognosis is unfavorable, which becomes conditionally favorable after a kidney transplant.
Hydronephrosis Kidney cancer Increased intraocular pressure: symptoms, causes and treatment Hypertension Polycystic kidney disease Pyelonephritis
Possible complications
Neglect of doctor's recommendations or inadequate therapeutic strategy often become the culprits in the development of difficult-to-treat diseases, not to mention possible death. High blood pressure with kidney damage greatly increases the risk of the following disorders:
- violation of the biochemical composition of the blood;
- deterioration of cerebral circulation;
- hemorrhagic stroke of the brain;
- swelling of the lung tissue;
- progression of renal or heart failure;
- blindness resulting from damage to the optic nerve and retinal hemorrhage;
- cardiac ischemia;
- necrosis of parenchymal tissue.