A discomforting state after intimacy and an increased urge to urinate are precisely these complaints that doctors often hear from young women who have had sexual intercourse for the first time. Moreover, approximately a third of young and middle-aged women suffer from it.
The description of this phenomenon is very similar to cystitis, and in its essence it is. The disease is provoked by E. coli, which, even judging by the name, is an inhabitant of our intestines. Painful phenomena begin to be observed if, for some reason, it manages to get into the vagina and then penetrate the urethra. Most often, this can happen during sexual intercourse, especially if partners do not pay enough attention to their personal intimate hygiene.
Cystitis after sex
Moreover, doctors say that the greatest risk factor for the development of inflammatory diseases of the urinary tract in women is their sexual activity.
The likelihood of developing the disease is determined by the frequency, duration, and regularity of sexual intercourse. Since the disease in question is directly related to the onset of sexual activity, its name sounds accordingly - honeymoon cystitis or cystitis after sex. The correct medical name is postcoital cystitis; this is the name used in domestic and foreign medical literature.
Symptoms of the disease
The first symptoms of honeymoon cystitis are:
- constant feeling of a full bladder,
- discomfort and pain when urinating,
- painful sensations in the pelvic area.
These phenomena disappear on their own already on the third or fourth day; their complete disappearance is observed after a week. But practice shows that only the manifestations of cystitis of the first wave disappear.
Without proper timely treatment, the symptoms of honeymoon cystitis may reappear over time, this can happen in a month or a year.
Symptoms
This cystitis is characterized by an acute onset.
Soon after intercourse, symptoms such as
:
- frequent but scanty painful urination;
- pain in the lower abdomen;
- hyperthermia;
- episodic enuresis (urinary incontinence);
- Possible hematuria (presence of red blood cells in the urine).
Often, manifestations of cystitis disappear on their own within a few days. However, this does not mean that the disease has been cured. In most cases, the lack of adequate treatment leads to the development of a chronic form of cystitis, which is characterized by a long course with periodic exacerbations and can lead to serious diseases of the kidneys and bladder.
Risk factors
The most important factor influencing the occurrence of the disease is sexual activity. Doctors consider the ascending route to be the main route of penetration of microflora into the bladder. The anatomical features of the female body are to blame for the frequent development of cystitis and urethritis:
- proximity of the urethra to the vagina,
- its short length
- its relatively large diameter.
But with the same anatomical structure, only a third of women suffer from honeymoon cystitis. Let's try to find out what the reason is.
Doctors believe that the occurrence of chronic cystitis and urethritis occurs due to vaginal ectopia of the external opening of the urethra and its hypermobility. These words mean pronounced mobility of the external opening of the urethra, caused by the presence of adhesions, which are the remnants of the deflowered hymen. vaginal ectopia leads to the location of the opening of the urethra at a place lower than usual, namely, at the very border of the entrance to the vagina. In this case, the adhesions are weakly expressed or completely absent.
Causes of the disease
In both cases, during swimming, the external opening of the urethra moves towards the vagina, and at the same time it opens. As we can see, the conditions for the penetration of pathogenic microorganisms, including E. coli, are simply ideal. The reason becomes obvious, increasing the likelihood of an inflammatory process in the bladder. The situation is aggravated by sexual intercourse itself, which promotes the injection of vaginal contents into the opened lumen of the urethra.
Anatomical variations in the location of the urethral opening most often determine the possibility of developing a chronic disease due to primary postcoital disease.
But the cause of such unpleasant phenomena as:
- hurts,
- exacerbation of honeymoon cystitis,
- painful, frequent urination,
- A burning sensation in the urethra can be observed even after a routine examination by a gynecologist.
Honeymoon cystitis occurs during the first sexual intercourse, which is accompanied by a frequent urge to urinate and pain in the lower abdomen. Inflammation of the bladder mucosa is a common disease among women.
Features of treatment
Typically, treatment in the initial stages of the disease is quick and easy. Antibacterial drugs are effective in combating the spread of infection in the bladder and urinary canals. Perhaps the most potent drug is Monural. Treatment is limited to a single dose for recovery to occur. But you can take the drug only as prescribed by a specialist.
In addition to the use of antibacterial and anti-inflammatory drugs, without which it is impossible to carry out treatment, patients with honeymoon cystitis should take into account the following points during therapy:
- strict bed rest;
- therapeutic nutrition;
- drinking plenty of fluids.
If treatment is carried out correctly, improvements can already occur within a week from the start of therapy. To avoid re-infection, it is important to adhere to good personal hygiene.
It is much more difficult to carry out treatment in situations where cystitis has become chronic. Then, instead of conventional antibiotic therapy, immunostimulation and local treatment of honeymoon cystitis will be needed, in which the antibiotic should be injected into the affected bladder. Treatment with physiotherapeutic procedures, in which medications are also administered into the bladder cavity, is also possible.
There are also cases when conservative treatment is powerless, then surgical intervention becomes inevitable. To protect yourself from complications, when you notice the first symptoms of cystitis, you should consult a specialist.
CYSTITIS honeymoon
Honeymoon cystitis occurs during the first sexual intercourse, which is accompanied by a frequent urge to urinate and pain in the lower abdomen. Inflammation of the bladder mucosa is a common disease among women.
Why is cystitis called the honeymoon disease?
Many people associate the honeymoon with an active sex life. The physiological characteristics of a person determine the consequences of such sexual behavior. Additionally, honeymoon syndrome means that on the first wedding night the young wife loses her virginity, and this can lead to diseases of the genitourinary system, accompanied by painful sensations of varying intensity.
There are a number of such features:
- When deflowering, the microflora of the girl’s vagina is activated, and the addition of bacteria from the sexual partner is also observed. This phenomenon can provoke an inflammatory process that spreads to the organs of the urinary tract.
- If a woman has not entered into intimate relationships for a long time, then harsh sexual intercourse can lead to the development of the disease.
- Prolonged sexual intercourse also causes honeymoon cystitis.
CYSTITIS honeymoon
Cystitis. When not to go to the doctor
Principles of treatment
Therapy for this disease is almost always conservative. It is prescribed by a urologist taking into account the clinical picture and general condition of the patient.
How to treat honeymoon cystitis? The basis of therapy is taking medications. They will be discussed in more detail below. A woman is also required to follow a special diet. The latter implies the exclusion of overly spicy and salty foods. All foods that can irritate the bladder mucosa (sour, fried, smoked) are also prohibited. The diet should be dominated by porridges and soups, fermented milk products, and various drinks (fruit drinks, jelly).
Reasons for appearance
There are a number of factors that provoke the inflammatory process:
- Damage to the urinary organs by pathogenic microorganisms. We are talking about E. coli getting into the vagina during anal sex.
- Pathology of the development of the urethra, which contributes to the unhindered penetration of microbes.
- Insufficient moisture in the vagina in an excited state, which leads to damage to the urethra with subsequent infection.
- Bacteria contained on the mucous membrane of the penis become the causative agents of honeymoon cystitis in conditions of weakened immunity of a woman. There is a violation of the vaginal microflora (low levels of lactobacilli).
- Honeymoon cystitis is typical not only for girls after defloration (rupture of the hymen). The postcoital form of the disease also occurs in women who have been married for several years. The reason for this phenomenon may be the use of spermicides to protect against unwanted pregnancy.
- A prolapsed kidney is also one of the factors that provokes the pathological process. The ureter is blocked, which interferes with the normal movement of urine.
- The development of inflammation in the bladder is due to the presence of vaginitis. Sexual contact only aggravates the course of the disease, which leads to complications.
- During oral-genital contact, there is a high risk of infection if the partner develops dental caries. Bacteria, along with saliva, penetrate the urethra and then into the bladder cavity, causing irritation of the mucous membrane.
- Failure to comply with personal hygiene rules. It is necessary to wash yourself after sexual intercourse, especially if we are talking about defloration.
- If a woman does not urinate after sex, there is also a risk of developing honeymoon cystitis.
- The psychosomatic nature of honey period syndrome in the lives of lovers should not be ruled out.
Among women
Women are most susceptible to this disease, which is due to the structure of the urethra (wide and short).
Much depends on the state of the vaginal microflora: if opportunistic agents predominate, then the risk of cystitis is high. Even if all hygiene standards are observed and latex contraceptives are used, a woman may experience symptomatic signs of bladder inflammation.
In men
In most cases, men do not suffer from honeymoon cystitis.
If they exhibit characteristic symptomatic manifestations, then we are talking about possible infection with a sexually transmitted infection.
How to treat honeymoon cystitis
Honeymoon cystitis can be cured with the help of medications and traditional medicine.
The exact dosage, frequency and duration of treatment for the disease is determined by the doctor.
First aid
The principle of therapeutic action is as follows:
- To relieve pain, you need to hold a bottle of warm water between your legs in the crotch area.
- If the pain is unbearable, you can take Uropirin. This analgesic is used to eliminate pain due to pathologies of the urinary tract.
- You should not take antibiotics without a doctor’s recommendation, since it is necessary to first identify the etiology of the inflammatory process. Cystitis can act either as an independent disease or as a symptom of a secondary disorder.
Drug treatment
For honeymoon cystitis, the following medications are prescribed:
- Uroseptic Furadonin. Does not cause addiction syndrome. The product should not be used by people with severe renal failure.
- Antibiotic Monural in powder form. A single dose is sufficient to achieve positive dynamics in the clinical symptoms of honeymoon pathology.
Traditional medicine recipes
The most effective folk remedies for honeymoon cystitis are:
- Sitz baths based on chamomile infusion.
- Treatment of the vulvar mucosa with a saturated saline solution (1 tablespoon of sea salt per 250 ml of warm water).
- Ingestion of a decoction based on corn silk.
First aid measures
If the first signs of pathology are detected, you should visit a gynecologist as soon as possible, who will tell you how long the therapy will last and what medications should be used.
Your partner should be warned about the presence of cystitis, since women are advised to abstain from sexual intercourse during the period of treatment.
Warm baths, to which herbal decoctions of chamomile or calendula are added, will help relieve primary symptoms for a while.
This procedure helps eliminate pain and has a general calming effect.
Prevention of honeymoon cystitis
The development of the disease after intimacy can be prevented if you follow a number of these rules:
- Do not neglect genital hygiene. Avoid using soap. Give preference to intimate hygiene gels that contain lactic acid.
- Contact a urologist promptly for advice if you observe symptoms of honeymoon cystitis.
- Do not hold back the urge to urinate (stagnation of urine provides a favorable environment for the proliferation of pathogens, which increases the risk of developing the disease).
- Drink at least 2 liters of water per day (when the acidity in the bladder changes, conditions arise in which bacteria actively multiply).
- Empty your bladder before sexual intercourse.
- Avoid hypothermia.
- Be sure to treat the acute form of the disease.
Cystitis is a common disease in which the mucous membrane of the bladder becomes inflamed. Sometimes it occurs after the start of sexual activity. This is the reason why it is called honeymoon cystitis.
The disease negatively affects not only the psychological state of a woman, but also her intimate life. The condition requires qualified help, because an infection has been introduced into the genitourinary organs. Today, honey cystitis is called not only inflammation that occurs after the first sexual intercourse, but also cystitis associated with intimacy in general.
E. coli entering the bladder is especially dangerous. If the intestines are its usual habitat, then in the genitourinary system it begins to actively multiply, inevitably leading to inflammatory reactions. In addition, cystitis can be caused by viruses, bacteria, and fungi.
How to recognize the disease?
Certain symptoms will help you recognize the development of honeymoon cystitis. Most often, patients turn to urologists with complaints such as painful and frequent urination, as well as pain and burning after intimacy. Moreover, very often all symptoms disappear a few days after their onset. In this case, the disease is hidden, which is very dangerous for the sick person.
For some, symptoms of the disease may reoccur after 1-2 months, while for others, cystitis may not manifest itself in any way for several years.
It is much more difficult to get rid of a disease that has become chronic. Latent chronic cystitis is dangerous because it inevitably leads to wrinkling of the walls of the bladder, as a result of which the organ is deformed and its functioning is disrupted.
Diagnosis of the disease
Unfortunately, not all women who notice symptoms of honeymoon cystitis seek medical help. At the same time, you should not hope that the disease can disappear on its own, because with an infectious lesion, the bladder will shrink until its functionality is impaired.
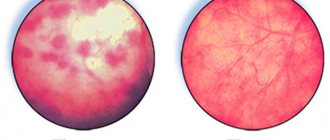
There are often cases when honeymoon cystitis does not manifest itself for a long time, and no changes are observed in the urine. Cystoscopy comes to the aid of specialists - a method of examining the bladder that uses a special optical device. If a woman complains of certain symptoms indicating the development of honeymoon cystitis, then laboratory tests and ultrasound of the pelvic organs are performed to confirm the diagnosis.
Honeymoon syndrome
Postcoital cystitis is often called “honeymoon syndrome.” The disease received this name back in the days when girls kept their virginity until marriage.
The pathological process is a consequence of infection from the intestines or genitals. The urethra in women is shorter and wider, this creates favorable conditions for the rapid penetration of pathogens.
Causes of honey cystitis
A number of reasons can lead to the appearance of the disease:
- colpitis;
- vaginal dysbiosis;
- bacterial vaginosis of the vagina;
- lack of proper adherence to intimate hygiene rules;
- promiscuous sex life;
- alternating vaginal and anal sex;
- hard sexual intercourse;
- prolonged sexual intercourse;
- lack of lubrication;
- dryness of the genital canals;
- using a diaphragm or spermicides as contraception;
- presence of sexually transmitted diseases;
- diabetes;
- obesity;
- overly spicy food;
- change of sexual partner;
- frequent hypothermia;
- endocrine disorders;
- smoking;
- heavy physical activity;
- genitourinary anomalies.
When the urethra is displaced downward and inside the vagina or its excessive mobility, injury occurs.
Symptoms of honey cystitis
Honey cystitis is characterized by a sudden onset. Soon after intimacy, a woman may begin to experience the following symptoms:
- pain in the lower abdomen, which may not stop throughout the whole day, and at times intensify;
- frequent and painful urge to urinate with scanty urine output;
- urinary incontinence;
- hyperthermia;
- the appearance of pus in the urine;
- general malaise;
- feeling of bladder fullness.
If the appearance of cystitis after sexual intercourse has become commonplace, this will inevitably have a negative impact on family relationships. Many women who suffer from this disease are diagnosed with neuroses.
If clinical symptoms occur after the first sexual intercourse, they usually disappear after a few days. But this does not mean that the disease has receded. It may reappear in a few months, or even years. If the disease acquires a latent form, it can lead to damage to the deeper layers of the bladder, and this threatens further shrinkage of the organ.
The danger of this pathological process is associated with the spread of the infectious process along the ascending pathways, reaching the kidneys. As a result, serious problems that pose a threat to a woman’s health may develop.
How to recognize the disease?
Certain symptoms will help you recognize the development of honeymoon cystitis. Most often, patients turn to urologists with complaints such as painful and frequent urination, as well as pain and burning after intimacy. Moreover, very often all symptoms disappear a few days after their onset. In this case, the disease is hidden, which is very dangerous for the sick person.
For some, symptoms of the disease may reoccur after 1-2 months, while for others, cystitis may not manifest itself in any way for several years.
It is much more difficult to get rid of a disease that has become chronic. Latent chronic cystitis is dangerous because it inevitably leads to wrinkling of the walls of the bladder, as a result of which the organ is deformed and its functioning is disrupted.
Diagnosis of the disease
Unfortunately, not all women who notice symptoms of honeymoon cystitis seek medical help. At the same time, you should not hope that the disease can disappear on its own, because with an infectious lesion, the bladder will shrink until its functionality is impaired.
There are often cases when honeymoon cystitis does not manifest itself for a long time, and no changes are observed in the urine. Cystoscopy comes to the aid of specialists - a method of examining the bladder that uses a special optical device. If a woman complains of certain symptoms indicating the development of honeymoon cystitis, then laboratory tests and ultrasound of the pelvic organs are performed to confirm the diagnosis.
Diagnosis of postcoital cystitis
In the early stages, honeymoon cystitis is not difficult to identify; this will require the following studies:
- general blood analysis. With cystitis, an inflammatory reaction will be visible: increased levels of ESR and leukocytes;
- general urine analysis. Proteinuria, hematuria, pyuria, bacteriuria are detected;
- . Usually given after a microscopic urine test. It determines the number of red blood cells and white blood cells in one milliliter of urine;
- urine culture for sterility. Using the analysis, you can identify the causative agent of the disease and decide on the choice of antibacterial agent;
- Ultrasound of the bladder and kidneys;
- examination by a gynecologist to determine the position of the urethra in relation to the vagina;
- gynecological smear for flora. It is taken from three places: the urethra, vagina and cervical canal. Necessary to rule out STDs.
Diagnostic methods
During their honeymoon, not all women seek medical help. Some try to cure the disease at home, others ignore it completely. Both approaches to solving the problem are wrong. At the initial stage of the pathological process, a visit to the urologist should be made.
Diagnosis of the disease begins with studying the patient's history and complaints. Then they move on to instrumental and laboratory examination methods, which involve the appointment of:
- general urinalysis;
- urine analysis for microflora;
- ultrasound examination;
- cystoscopy.
The studies carried out make it possible to identify the inflammatory process and determine the type of bacteria that caused its development. To exclude sexually transmitted diseases, you may additionally need to consult a gynecologist.
How to treat honeymoon cystitis
General principles in the treatment of postcoital cystitis:
- compliance with bed rest;
- drinking plenty of fluids to remove pathogenic microflora and their breakdown products from the bladder;
- phytotherapy. This implies the use of medicinal preparations that have a diuretic and anti-inflammatory effect;
- dietary food. A dairy-vegetable diet is recommended. You should exclude from your diet foods that can irritate the bladder: spicy, salty, smoked, fried, pickled, alcoholic drinks;
- strengthening the immune system;
- antibacterial therapy;
- symptomatic treatment, which involves the use of analgesics, antispasmodics, and anti-inflammatory drugs;
- normalization of the natural balance of microflora of the genital organs;
- treatment of concomitant diseases.
If you consult a doctor in a timely manner and strictly follow his instructions, then in about a week you will be able to return to a full life. At the same time, we should not forget about constant hygiene of sexual life.
If the disease is advanced, it will be much more difficult to get rid of it. The treatment regimen includes a whole range of measures:
- systemic antibiotic therapy;
- introduction of antibacterial solutions into the bladder cavity;
- therapeutic exercises to strengthen the pelvic muscles;
- physiotherapeutic procedures.
The most popular drugs in the treatment of honey cystitis are Furadonin and. Heating, herbal baths, infusions and teas are used as folk remedies. Using unconventional recipes on your own can cause serious harm.
In cases where the disease does not respond to conservative treatment and sexual activity becomes impossible, specialists resort to surgical intervention. The essence of the operation is that the urethral opening is raised several centimeters.
Is it possible to have sex during treatment?
Antibiotic therapy disrupts the normal microflora, promoting the development of bacteria. For this reason, experts recommend abstaining from intimacy during treatment.
It is also worth considering the fact that during sexual intercourse the mucous membrane is subject to additional irritation, which is why the clinical picture may intensify and the healing process may be delayed.
Postcoital cystitis itself is not a contagious disease, so you cannot pass it on to your partner. Therefore, theoretically, having sex during treatment is possible, unless the disease was caused by sexually transmitted infections.
Sex during cystitis is not prohibited. It is simply advisable to postpone it for the period of exacerbation. After the antibiotic therapy has come to an end and the exacerbation has passed, you can return to sexual activity, while strictly observing intimate hygiene.
Prevention
If cystitis occurs due to an abnormal location of the urethra, antibiotic therapy or surgery is required. But how can you reduce the risk of postcoital cystitis so that it does not manifest itself as unpleasant symptoms?
- It is necessary to be tested for sexually transmitted infections to prevent bladder inflammation. If you have such diseases, you should get rid of them. Both partners undergo treatment.
- Intimate hygiene should be carefully observed. Before and after sex, you should thoroughly wash your hands and external genitalia. It is forbidden to alternate vaginal and anal sex, since most cases end in cystitis.
- It is not recommended to practice positions that cause urethral irritation.
- Avoid irritation of the mucous membrane. The use of some contraceptives causes dryness of the vaginal mucosa. As a result, microtraumas of the epithelium are formed.
Prevention of honey cystitis
Prevention of honey cystitis largely depends on etiological factors. In case of abnormalities in the location of the urethra, surgery may even be required, although in many cases antibiotic therapy is sufficient.
Let's highlight general preventive measures:
- avoid casual sex, use condoms;
- undergo regular preventive examinations and get tested for STDs;
- strictly observe sexual hygiene;
- wash yourself in a timely manner;
- change your underwear and sanitary pads regularly;
- empty your bladder before sexual intercourse;
- strengthen your immune system.
They say that you have to pay for pleasure. One of the proofs of this statement is cystitis after sexual intercourse. The disease cannot be ignored, as it is fraught with serious complications. Correct and timely treatment will help you quickly get rid of the problem, and preventive measures will help you avoid its occurrence altogether.
Experts refer to honeymoon cystitis as cystitis that occurs in a woman after sexual intercourse. The disease is characterized by inflammation of the inner mucous membrane that covers the bladder. Inflammation is caused by pathogenic microbes from the vagina or intestines that have entered the urethra.
This painful condition has the most negative impact on the general condition of a woman. Sexual contacts become painful, which causes physical and psychological discomfort. What causes honeymoon cystitis, treatment, symptoms, what are the causes of this disease? Let's figure it out together:
What causes honeymoon cystitis? Causes of the disease
Very often, cystitis occurs in those women who suffer from colpitis or bacterial vaginosis. As is known, due to the anatomical features of the urethra, which in women is short and wide, infection that affects the bladder easily penetrates into it.
It is very dangerous when the bladder mucosa is affected by E. coli, which always lives in the human intestines. Once in the bladder, the rod actively multiplies, causing a strong, intense inflammatory process. In addition, inflammation is caused by staphylococci, streptococci, as well as chlamydia and trichomonas that penetrate the mucous membrane of the bladder.
There may be other causes of the disease. For example, some diseases that reduce immunity: diabetes, obesity or thyroid dysfunction. The appearance of cystitis can be triggered by hypothermia, metabolic disorders, as well as physical and psycho-emotional fatigue.
How does honeymoon cystitis manifest itself? Symptoms of the disease
The main symptoms of honeymoon cystitis include: - Painful sensations when urinating; - The appearance of blood in the urine; - Pain in the lower abdomen, which becomes more severe as the bladder fills. — With an exacerbation of cystitis, the state of health sharply worsens. General weakness and malaise appear, and body temperature may rise. — Signs of cystitis are observed immediately after sexual intercourse, or 2-3 days after sex.
What to do if you have honeymoon cystitis? Treatment of the condition
Therapy for this disease is carried out by a doctor after an examination and an accurately established diagnosis. Drug treatment is prescribed individually. Antibacterial drugs are usually prescribed, in particular the drug Monural. This remedy is taken once, after which recovery quickly occurs.
In addition, when treating honeymoon cystitis, bed rest should be observed, therapeutic nutrition and plenty of fluids are recommended.
It is much more difficult to treat this disease if it has become chronic. In addition to taking antibiotic medications orally, you will also need immunostimulation, as well as direct injection of an antibiotic or other drugs into the area of the affected bladder.
How does traditional medicine treat honeymoon cystitis? Folk remedies
Mix equal amounts of flax seeds, dried lingonberry leaves, and dried calendula flowers in a bowl. Also add the same amount of tricolor violet herb and lovage. Mix the collection thoroughly. Pour 2 tbsp into the cavity of the thermos. l. healing herbal mixture, add 400 ml. boiling water Keep the thermos closed for 3-4 hours. Then drain the infusion through a strainer and squeeze out the raw materials. Drink a third of a glass three times a day, before meals.
Mix equal amounts of dried cornflower flowers, leaves of the wintergreen plant, and crushed angelica root. Add the same amount of cinquefoil herb and nettle. Pour 2 tbsp into a thermos. l. mixture, add half a liter of boiling water. Leave for 4 hours. Strain. Drink half a glass before meals (half an hour).
Finely chop the parsley roots. Add the same amount of chopped herbs to this garden spice. Stir. Now pour 1 tsp into an empty thermos. mixtures. Add 200 ml. boiling water Leave for 3 hours. Strain the infusion. Drink the entire amount in three doses - 1 hour before meals.
Regular dill will help relieve symptoms and treat cystitis. Cut the greens into smaller pieces, add 3 tbsp. l. into a small saucepan. Now pour 2 glasses of hot water there. Place in a boiling water bath, keep for 15 minutes. Then remove from the stove, wrap in a towel. Wait until it cools down and strain. Drink a third of a glass before meals (half an hour before).
When treating honeymoon cystitis, it is very useful to take warm baths (35 degrees) with the addition of decoctions and infusions of medicinal plants. Such baths take no more than 15 minutes.
If you suspect you have this disease, be sure to consult a doctor. Before taking treatment measures, you need to make an accurate diagnosis, which cannot be done without the participation of a specialist. So keep that in mind. Be healthy!
Cystitis is an inflammatory process of the mucous membrane of the bladder. It is often also called honeymoon cystitis due to the fact that it occurs after the first intimate night (another name for the disease is newlywed cystitis). Why can this disease progress so rapidly? - you ask.
The close proximity of the urethra and vagina causes the development of cystitis after sex
The main reason for the appearance of the disease is sexual intercourse, during which the vaginal microflora moves into the urinary canal, and since in women it is quite short and wide, all kinds of infections and bacteria penetrate there without difficulty.
The reason for this phenomenon may be hidden in a violation of the vaginal microflora itself, or simply the basic rules of hygiene are not observed (constant cleanliness of the intimate areas, and so on).
Unfortunately, today many suffer from cystitis, which appears precisely after sexual intercourse. This disease leaves an unpleasant mark not only on a woman’s daily pastime, but also on her intimate life. At the first signs of cystitis, you should immediately seek help from a doctor. But, before you go to a specialist for help, you need to know the symptoms of cystitis.
Cystitis of newlyweds: symptoms and treatment Cystitis of newlyweds: symptoms and treatment
Urologists often encounter such pathology in their patients as honeymoon cystitis. This is an inflammation of the bladder that occurs in newlyweds after unprotected sex. This pathology occurs in both women and men. If you do not consult a doctor in a timely manner or self-medicate, the infection spreads and reaches the kidneys.
Development of postcoital cystitis in spouses
Honeymoon cystitis is a predominantly female disease in which there is acute inflammation of the bladder mucosa. The risk group includes women who have not previously had sexual intercourse.
This pathology of newlyweds is called postcoital cystitis.
The causative agents of the disease are opportunistic microorganisms (Escherichia coli, Klebsiella, cocci) that penetrate the urethra and bladder from the vagina or intestines.
Men are at risk of developing cystitis during anal sex without using barrier contraception (condom). In many newlyweds, the mucous membrane of the urethra and bladder is sensitive to changes in microbial composition. Any unfavorable factors or decreased immunity can contribute to the activation of infection. Very often the inflammation becomes chronic.
Etiological factors
The following reasons for the development of cystitis during the honeymoon are identified:
- neglect of condoms;
- the presence of intestinal or vaginal dysbiosis;
- alternating traditional sex with non-traditional sex;
- decreased immunity;
- hypothermia;
- presence of diabetes mellitus;
- presence of chronic intestinal diseases;
- failure to comply with intimate hygiene rules.
Risk factors include poor nutrition, obesity, thyroid disease, and the presence of an STI in a partner. The most common causative agent of infection is opportunistic flora. It is present in a woman's intestines and vagina, but is not normally found on the lining of the bladder and urethra. Ideally, the urinary tract and urine are sterile.
Clinical manifestations of cystitis
Symptoms of postcoital cystitis do not have specific features. Acute inflammation occurs with frequent and painful urination, pain in the pubic area, increased body temperature, changes in the nature of urine (it becomes cloudy). Fever is accompanied by chills, malaise, and headache. The main symptom is pollakiuria.
During the separation of urine, patients are bothered by pain. The frequency of migrations can reach 30-40 per day. Some people urinate every 30 minutes. Symptoms include bladder pain. It intensifies with the accumulation of urine in the organ. Some patients have to strain to empty their bladder.
Sometimes involuntary urination occurs. Signs of postcoital cystitis include nocturia. At the same time, mictions become more frequent at night. With the naked eye you can see that the appearance of urine changes. It often contains sediment, flakes, blood or pus. Symptoms of the disease appear within 2-3 days after sexual intercourse.
They often subside and appear again after a while. In the case of a chronic course of the disease, complaints persist, but the symptoms are less pronounced. During the acute phase, the signs of the disease differ little from acute cystitis.
Examination and treatment tactics
Patients should be treated after examination. The following studies are required:
- palpation of the abdomen;
- general urine analysis;
- blood analysis;
- Ultrasound of the kidneys and bladder;
- urethral smear analysis;
- uroflowmetry (assessment of urine flow rate);
- cystoscopy (inspection of the bladder).
With cystitis, the following changes in the general urine test are possible:
- presence of bacteria;
- increase in specific density (more than 1030 g/l);
- increase in the number of leukocytes;
- cloudiness;
- the appearance of fungi (with specific cystitis).
Treatment of honeymoon cystitis is conservative. It is prescribed by a urologist taking into account drug tolerance.
Treatment involves bed rest, drinking plenty of fluids, taking antibiotics and uroantiseptics, sitz baths or dry heat (in the remission phase), and using diuretic herbs (lingonberry leaves).
For pain, NSAIDs or antispasmodics are prescribed. Antibiotics include fluoroquinolones (Tsiprolet, Abaktal, Nolitsin), as well as uroantiseptics (Furadonin, Monural). All drugs have indications and contraindications. They need to be taken into account. If specific microbes (viruses, fungi, chlamydia) are detected as a result of urine culture, other medications are used.
Additionally, herbal-based drugs (Canephron) may be prescribed. Patients are recommended to drink cranberry or lingonberry fruit drinks. They have a diuretic effect. For a speedy recovery, you need to eat right. The diet should be dominated by fermented milk products, cereals, soups and various drinks (fruit drinks, jelly, compotes).
After acute symptoms subside, physical therapy is performed. It is important to prevent the disease from becoming chronic. If this happens, then etiotropic therapy is carried out. Chronic cystitis can lead to complications such as organ shrinkage, pyelonephritis, and urethritis. After the course of treatment, repeat tests are performed.
Postcoital cystitis is common. In the absence of complications, the prognosis is favorable. To prevent the disease, you need to use condoms, increase your immunity, change your underwear more often, use intimate hygiene products and antiseptics after sexual contact.
Source: https://nepropal.ru/medovogo-mesyacza.html
Causes of cystitis
As mentioned above, during sexual intercourse the urethra moves slightly towards the vagina and opens, thereby allowing infections to enter the intimate area. As a result, the conditions for the development of cystitis can be called ideal, and further active sexual life only aggravates the current situation.
The onset of the disease will coincide with the date of the first sexual intercourse. That is why doctors often use the term defloration cystitis (it is associated with trauma, disruption of the virgin structure of the vagina), and further sexual intercourse can aggravate it. But there are other reasons that contribute to its aggravation and further development:
- Hypothermia of the body (in the intimate area).
- Overly spicy food.
- Smoking.
When the hymen ruptures, there is a risk of developing cystitis
It is important to know: you may be surprised, but honey cystitis can develop even after changing sexual partners.
The dangers of honeymoon cystitis are as follows:
- First of all, if you do not treat the disease, then over time it will develop into a chronic form, and it is much more difficult to cure.
- In addition, honeymoon cystitis has an extremely negative effect on your intimacy with your partner, since the unpleasant sensations do not give you peace.