Cystitis is an inflammatory process of the mucous membrane of the bladder, which is accompanied by pain and discomfort when urinating. Postcoital means the appearance of the disease after sexual intercourse: it manifests itself either immediately or after 1-2 days. This is the necessary period of time for bacteria to gain a foothold in the bladder cavity. In some sources you can find the name “honeymoon syndrome”.
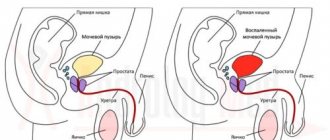
The anatomical structure of the genitourinary system puts women at greater risk of infection.
The length of their urethra is only 4 cm, which is 5 times shorter than that of a man. This facilitates the penetration of various microorganisms after intimate intercourse. Even among representatives of the stronger sex, this distance is not insurmountable; cystitis occurs in them too.
Etiology of the disease
Representatives of all age groups are susceptible to inflammation. The statistics are frightening: approximately a quarter of women of reproductive age have been treated for postcoital cystitis at least once.
Numerous forums on this topic indicate the widespread nature of the problem.
The reason for the development of pathology is microorganisms:
- bacteria (staphylococci, streptococci, enterococci, E. coli);
- virus (for example, herpes simplex);
- fungal pathogens (mainly Candida genus).
The disease does not necessarily develop through the entry of harmful organisms from the outside. It may also be the result of activation of one’s own opportunistic microflora. There are many factors that contribute to the development of the disease:
- Anatomical predisposition: displacement of the urethra or external urethral opening. There is constant trauma to the mucous membrane, as a result of which bacteria easily enter and multiply inside.
- Sexually transmitted diseases can contribute to the development of postcoital cystitis.
- Insufficient lubrication and prolonged sexual intercourse lead to damage to tissue integrity.
- Opportunistic microflora of the partner’s penis, which causes inflammation, can also affect a woman’s urinary system.
- "Missionary position.
- Anal penetration precedes vaginal penetration. A common pathogen is Escherichia coli.
- Neglect of the rules of personal intimate hygiene, especially after visiting public places: baths, saunas, swimming pools and after sexual intercourse.
- Frequent change of sexual partners.
- The presence of untreated or chronic diseases of the genitourinary system.
- Incorrect and illiterate use of contraceptives, especially spermicide-containing ones, which destroy the vaginal mucosa.
- Hormonal imbalance.
- A girl’s first sexual contact, or intimate intimacy after long-term abstinence.
- Adhesions and residual fragments of the hymen formed as a result of mobility of the ureter.
If you treat your health carefully and minimize the conditions for the successful progression of the disease, then the likelihood of developing an inflammatory process is noticeably reduced.
Therapeutic measures for postcoital cystitis
Treatment of postcoital cystitis is complex and includes taking medications, using auxiliary folk remedies, and surgical intervention if necessary. In the early stages, treatment is aimed at preventing new exacerbations. However, if cystitis occurs again after sexual intercourse, specific treatment methods are prescribed.
During treatment, sexual activity is not recommended. This can provoke an exacerbation of the disease and cause infection of the partner. Also, during therapy you need to carefully monitor your intimate hygiene and stop using tampons.
Symptoms
The manifestations of pathology are individual for each person, but there are common characteristic signs. The first symptom in all patients was pain: both at rest and when visiting the toilet.
Symptoms of postcoital cystitis:
- sudden and frequent urge to urinate;
- pain, pain and burning during bowel movements;
- feeling of bladder fullness;
- redness in the perineal area;
- pain in the lower abdomen and lumbar spine;
- urinating in small portions;
- change in the color and odor of urine;
- the presence of impurities in urea (blood, pus, mucus);
- deterioration in general health;
- headache;
- temperature.
It becomes difficult to live with such manifestations: it is constantly necessary to have the restroom in sight, and it is inconvenient to leave suddenly in front of others.
Sexual life requires adjustment and abstinence for the period of treatment. In addition to physical discomfort, psycho-emotional stress arises.
When the first signs appear, consult a doctor immediately; time will only intensify the symptoms and increase the duration of treatment.
Symptoms
The disease has no specific symptoms. 1-2 days after sex, the first signs of the inflammatory process appear:
- pain in the bladder;
- increased urge to urinate;
- false urges;
- itching and burning when urinating;
- hyperemia of the external genitalia;
- temperature rise to low-grade levels and higher;
- possible change in urine color, hematuria.
Signs also include weakness, dizziness, pain in the lower abdomen.
In some cases, signs may appear already in the first hours after intimacy and disappear 24-48 hours after the development of symptoms.
Forms of pathology
There is an acute and chronic form of this disease. If it is diagnosed for the first time, it is an acute form; recurrent cases indicate a chronic form.
It is often inconvenient to talk about such delicate problems, so many try to cope with the disease on their own. This should not be done, since postcoital cystitis most often takes a chronic form.
The girl should immediately consult a doctor and tell her partner about this. Joint examination and treatment will be more productive.
Diagnosis
When the first signs of the disease appear, you should immediately seek qualified medical help. Making an accurate diagnosis consists of several stages:
- Studying the history of the disease: dynamics, symptoms, period of development, personal feelings and manifestations of a particular patient.
- A urologist conducts an external examination of a woman.
- To exclude various anatomical pathologies, a gynecological examination is performed
- Based on the examination and clinical history, laboratory tests and instrumental examination methods are prescribed:
- A general urine test, which allows you to determine the degree of damage to the entire genitourinary system by the number of leukocytes. The presence of impurities makes it possible to draw conclusions about the development of complications.
- A blood test allows you to judge your general health and the presence of inflammatory processes.
- A biochemical blood test allows you to evaluate the functioning of internal organs and obtain information about metabolism.
- It is advisable to conduct a bacterial culture of urine to determine the causative agent of the disease. This analysis may take some time. Therefore, it is often necessary to treat the disease with a broad-spectrum antibiotic.
- Taking a smear from the vagina reveals sexually transmitted infections that often accompany cystitis.
In some difficult cases or with frequent relapses, it is possible to use cystoscopy (a method for examining the inner surface of the bladder, in which a small catheter with optical and lighting systems is inserted into the urethra) and ultrasound diagnostics.
High-quality diagnostics guarantees the correct choice of medications and the effectiveness of treatment.
Diagnosis of the disease
To identify postcoital cystitis, the following methods are used:
- General urine and blood tests.
- Cytoscopy.
- Ultrasound of the pelvis.
- Urine culture.
- Laboratory examination of a vaginal smear for the presence of gynecological disorders.
- Study of the anatomical structure of the genitourinary system.
Based on the results of analyzes and hardware techniques, an individual program is developed.
Treatment
Treatment of postcoital cystitis in women involves conservative therapy and surgical intervention. Timely management will ensure the effectiveness and short duration of the fight against the disease.
Since the cause of the disease is harmful microorganisms, a course of antibiotics is prescribed, to which specific pathogens are sensitive.
Table 1. Drugs for the treatment of postcoital cystitis
| Pathogen | A drug |
| Bacteria | “Monural”, “Furamag”, “Nolitsin”, “Palin”, “Furadonin”, “Furagin”, “Nitroxoline” |
| Virus | "Cycloferon", "Viferon", "Acyclovir", "Ganciclovir" |
| Fungi | "Fluconazole", "Nystatin", "Ampholip" |
Specific medications, dosage and course duration are determined only by the attending physician.
At the same time, probiotics are prescribed to maintain normal intestinal microflora. Medications may be prescribed to relieve symptoms. For example, various analgesics are used to relieve pain. Immunomodulators and vitamin complexes are also selected.
Non-drug methods:
- the use of antiseptics by drip through the urethra;
- sitz baths;
- warming up with heating pads;
- a set of gymnastic exercises.
The use of complex measures gives the fastest results.
It is recommended to follow a certain diet, which should exclude foods that cause irritation to the mucous membrane. Too fatty, salty, sweet, and sour foods should be minimized. Drinking plenty of fluids and eating foods with a diuretic effect help speed up recovery. It is recommended to drink alkaline mineral waters.
If the disease is a consequence of another pathology, then treatment is carried out simultaneously. Cystitis can give some complications and become the root cause of other pathologies: thrush, endometritis, vaginosis, inflammatory processes of the uterus, appendages, pyelonephritis. You shouldn’t delay their treatment either.
Under no circumstances should you stop taking antibiotics, even if all symptoms have completely disappeared.
Lack of treatment or an undertreated condition threatens the disease to become chronic, which is much more difficult and time-consuming to treat. Measures taken at the wrong time can affect the quality of the patient’s intimate life: avoidance of sexual relations, psychological disorders.
A good addition to drug treatment is the use of traditional medicine. Various herbal remedies, herbal teas, decoctions and mixtures help soothe irritated mucous membranes, reduce swelling, and strengthen the immune system. Coltsfoot, chamomile, bearberry, blueberry, horsetail - this is not a complete list of medicinal plants that are used in the treatment of cystitis. Home remedies will relieve symptoms and reduce inflammation.
There are also ready-made herbal preparations: “Cyston”, “Canephron”, “Fitolysin”.
Congenital malformations are treated surgically. The operation is called “urethral transposition”. A small incision is made between the external opening of the urethra and the clitoris. Then suturing occurs, as a result of which the distance between the vagina and the external urethral canal increases. a special catheter is inserted.
Some modern technologies for carrying out this intervention allow it to be carried out on an outpatient basis. However, in most cases hospitalization is still required. 2-3 days after surgery, the urethral catheter is removed. Since suturing is performed using catgut (self-absorbable thread), the sutures are not removed. The rehabilitation period usually lasts 2-3 weeks. Feedback from patients after surgery allows us to conclude that the outcome is 85-95% successful.
The prognosis for treatment of postcoital cystitis is positive. But since immunity is not developed during recovery, the likelihood of inflammation reoccurring is high.
An important condition for successful therapy: it is necessary to abstain from sexual intercourse.
The disease itself is not sexually transmitted, but taking antibiotics disrupts the normal microflora of the vagina, reducing its protective functions. Trauma and the risk of parallel infection may delay treatment.
Cystitis can have the following complications:
- Infection of the genital organs, which leads to reproductive dysfunction.
- Development of other inflammations of other organs.
- The risk of developing cancer of the genitourinary system increases.
Preventive measures
Postcoital cystitis in women is one of those diseases that first needs to be prevented and only then treated. If preventive measures are not effective, only then does the doctor decide on drug treatment.
Prevention involves the following methods.
- Washing before and after sexual intercourse. Washing is done from front to back so as not to introduce E. coli from the rectum. For this, only running water is used.
- You can insert the penis into the vagina only with a sufficient amount of lubrication. If lubrication in the vagina is not enough, you need to use special intimate gels.
- You should avoid sexual positions that have a strong impact on the urethra.
- It is advisable to urinate after sex.
- Daily change of linen.
- Avoiding tampons.
- Avoid tight, synthetic or constricting underwear.
- Timely emptying of the bladder.
- Drink at least 2 liters of fluid per day.
- Timely treatment of gynecological diseases.
- Avoiding hypothermia.
- Do not use NSAIDs.
- Do not use catheters to drain urine.
- It is forbidden to alternate anal, vaginal and oral contact in one sexual act.
- It is prohibited to use spermicides for contraception.
- It is forbidden to wash your face with soap or use deodorants and sprays on your genitals.
In addition to such prevention, which is useful even for completely healthy people, in the presence of symptoms of cystitis, it is recommended to prescribe antibiotics. There are no precise medical recommendations on this matter; several types of antibiotics are used at the discretion of the attending physician, but they do not provide 100% effectiveness.
Undesirable complications sometimes occur, including the emergence of strains resistant to bacteria. Some patients develop vaginal and intestinal dysbiosis from antibiotics.
Prevention
Caution and accuracy in the intimate area are important measures to prevent any inflammatory process of the genitourinary system. To avoid infection or exacerbation of the chronic form, the following measures are taken:
- compliance with personal hygiene rules;
- compliance with hygiene standards and rules in intimate relationships;
- use of contraceptives without sperm and lubricants;
- if there is insufficient lubrication, use additional products;
- emptying the bladder before sexual intercourse;
- undergoing regular gynecological examinations and tests for various infections;
- having a permanent reliable sexual partner;
- good quality and naturalness of underwear;
- sufficient fluid intake;
- good balanced nutrition;
- taking vitamin complexes.
A trusting relationship with your partner will help you make a quick and only correct decision - see a doctor. Both are diagnosed with the disease. Paying attention to your own health and following simple hygiene rules and regulations will help you avoid unpleasant consequences.
How to confirm the diagnosis
When diagnosing postcoital inflammation, it is necessary to differentiate it from chronic recurrent inflammation. They begin with a medical history and gynecological examination. From the woman's words, the doctor can establish a connection with coitus. During a gynecological examination, attention is paid to the structure and location of the urethra. With postcoital cystitis, it will be noticeably displaced downward. In some cases, the doctor may palpate the adhesions stretched between the urethra and hymen.
The next stage is laboratory diagnostics. A general urine test is required. It is better to do it immediately after the onset of symptoms and before starting treatment. The analysis will contain signs of inflammation: leukocytes, bacteria, mucus, epithelium, protein and red blood cells may appear.
Additionally, a three-glass test and Nechiporenko analysis are prescribed. This helps differentiate inflammation in the urethra or bladder. To determine the bacterial flora, a sensitivity culture is prescribed. Urine is collected with a catheter into a sterile tube.
Instrumental diagnostic methods are necessary to confirm the diagnosis and exclude gynecological pathologies. Carry out:
- cystoscopy;
- Ultrasound of the pelvic organs and bladder;
- PCR diagnostics for sexually transmitted infections;
- vaginal smear.