Symptoms
Symptoms of the disease often appear:
- painful sensations above the pubis and in the pubic area;
- frequent urge to go to the toilet (every 5-15 minute period);
- painful urination with burning and stinging;
- impurities of blood cells in the urine;
- an increase in temperature in the human body, exceeding 37.5, etc.
The last two symptoms often indicate the spread of the infectious process beyond the boundaries of the mucosal layer, which can lead to serious consequences.
What do doctors advise?
At the first signs of infection, it is difficult to immediately go to the doctor. This is hampered by frequent urges to go to the toilet, the interval between which can be several minutes.
During the first 24 hours it is recommended:
- to be at home;
- drink a lot of plain water;
- Avoid spicy, fried and salty foods in your diet.
Spicy foods can irritate the mucous membrane of the urinary organ and contribute to exacerbation of inflammation. You need to drink a lot of fluid so that the amount of urine is large, and it washes away the infectious agents. Ideally, you should drink 1-2 more glasses of cranberry juice. It contains substances that prevent microorganisms from attaching to the mucous membrane of the bladder and corroding it.
If you drink a lot of water, the body can cope with the infection on its own. The mucous membrane of the bladder produces substances that envelop bacteria in a film and prevent them from attaching to the surface. However, the production of these substances is directly dependent on the woman’s hormonal background. Therefore, whether cystitis will go away depends on whether or not there are hormonal disorders associated with metabolism and menopause.
In adults
Men are more resistant to infection due to anatomical features. In most cases, pathogens die when passing through the long, narrow urethra. However, even with a mild form of cystitis, the immune system is weakened, which increases the risk of infection.
Men are more resistant to infection due to anatomical features. In most cases, pathogens die when passing through the long, narrow urethra.
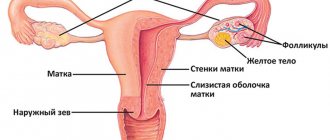
Women have a higher chance of developing a bacterial infection. They have a wide and short urethra through which pathogens pass relatively easily. In addition, another source of infection is located close to the vagina - the anus. Often, with a mild course, infection occurs and complications develop.
Causes
The main reason for the onset of the inflammatory process in the bladder area is infectious effects of various natures, including bacteria, viruses and fungi. Bacteria can enter and develop in the bladder due to various predisposing factors leading to cystitis. For example due to:
- hypothermia;
- due to the peculiarities of the structure of the urinary system of the female body;
- ignoring sanitary and hygienic rules;
- emerging venereal diseases;
- frequency of changing partners for sexual relations and unprotected sex;
- due to hormonal changes;
- traumatic situations;
- surgical intervention;
- due to a gynecological and urological disease;
- problems with stagnation of urine due to diseases in the urinary system or the rarity of the urination process, etc.
First you need to decide what caused cystitis and identify its main cause. Prescribing antibacterial and anti-inflammatory therapeutic methods is possible only after this, which will lead to improved well-being and complete recovery in the future.
In children
Due to an immature immune system, diseases in children progress much faster. If cystitis is of bacterial origin, complications will rapidly develop if left untreated. In case of poisoning with toxins, poor diet, allergies and similar factors, there is also a risk of worsening the condition. At the first signs of illness, the child should be seen by a doctor.
Inflammation in the bladder can sometimes go away on its own without outside intervention. The likelihood depends on the form and cause of the disease. However, in most cases, chronicity occurs and complications develop.
Inflammation in the bladder can sometimes go away on its own without outside intervention. The likelihood depends on the form and cause of the disease.
Most often, cystitis is of non-infectious origin. The body sometimes on its own, without treatment, suppresses the following types of inflammation:
- Allergic. If inflammation of the mucous membranes is caused by any product, wash, contraceptives, etc., it is enough to eliminate the irritant for the symptoms to disappear.
- Chemical. To prevent the development of the disease, you should stop taking irritating substances (medicines, spoiled foods, etc.) and help the body remove toxins.
- Hormone. The occurrence of inflammation is associated with an imbalance in the body and physiological changes. When hormonal levels fluctuate, bladder tissue loses its tone and becomes flabby, and problems with emptying may occur.
- During pregnancy. Irritation of the mucous walls most often appears in the first trimester. This is due to a rush of blood to the pelvic organs and an enlargement of the uterus. Later, the body rebuilds itself and the symptoms disappear.
- Postpartum. If cystitis is not accompanied by a bacterial infection and is caused by a minor injury or high blood pressure, there is a possibility that the symptoms will disappear on their own.
Acute infectious cystitis does not go away on its own. The immune system can prevent bacteria from entering before they reach the bladder. If the introduction has already occurred, you will have to use antibiotics (Monural, Amoxiclav), since the concentration of pathogens has increased.
Chronic cystitis also does not disappear without therapy. The occurrence of remissions is not associated with cure, but with the transition of pathogens to an inactive form. With any weakening of the immune system, the concentration of microbes increases again, and specific symptoms arise.
Why
Cystitis will go away on its own if the patient eliminates the factor causing inflammation of the mucous membranes. If the cause of irritation is dangerous injuries, tumors or infection, you will not be able to cope on your own.
Such conditions require surgical intervention or conservative treatment. With relatively safe factors (hypothermia, taking medications, lack of lubrication during sex, etc.
https://www.youtube.com/watch?v=Eo1_vZ46Lcc
) the patient is able to reduce inflammation without outside help. However, it is strongly recommended to consult a doctor.
Can cystitis go away on its own?
Can cystitis go away on its own? This issue worries a large number of people, because people have minimal desire to see doctors. Before answering this question, it is worth understanding what cystitis is?
Description
Cystitis is an inflammation of the urinary mucosa, which is accompanied by painful urination and increased body temperature.
Inflammation of the urinary tract is a polyetiological disease. That is, it can develop under the influence of various negative factors. These include:
- Bacteria
- Viruses
- Fungi
- Protozoa
- Injuries
- Malignant tumors of the bladder and nearby organs
- Inflammatory diseases of organs that are located in close proximity
- Autoimmune processes.
There are primary cystitis, which develops when exposed directly to the mucous membrane of the bladder, as well as secondary, which is a complication of other pathologies. Primary is most often of an infectious and traumatic nature. But secondary, it can arise not only due to damage to nearby organs, but can also have a distant focus.
Symptoms
My grandmother treated cystitis only this way...
This cheap remedy is in every home! How I cured real cystitis...
Treatment
> Question answer
Inflammatory processes in the bladder are diagnosed in patients of any age and gender, although the greatest susceptibility is observed in girls and women of reproductive age. Regardless of status, be it a “business woman” or a simple worker, everyone is interested in the question of how long the disease will take them out of commission and whether cystitis can go away on its own.
Genesis of development
Contrary to theoretical judgments that in any pathology the body's reserve forces are capable of turning on the self-healing mechanism, in practice, unfortunately, self-healing of cystitis has not been observed. The doctors’ verdict is that untreated forms of cystitis do not go away on their own.
With an attentive attitude towards yourself and correct behavior at the beginning of the disease, the painful clinic can smooth out and take a latent course, but one cannot count on its complete elimination.
Even if patients manage to improve their condition with self-treatment, this only indicates that they “succeeded” in transferring it from an acute form of the disease to a chronic course. At the same time, the slightest provocation of the disease can result in a relapse.
The great microbiologist Ilya Mechnikov said that inflammation is a protective reaction of the body aimed at eliminating foreign damaging agents and their metabolic products.
In our case, these are bacterial, viral or fungal representatives.
Their effect disrupts the natural phagocytosis of epithelial cells of the mucous lining of the reservoir cavity of the bladder, causing manifestations of pathological symptoms.
Penetrating inside and attaching to the walls of the organ (in 90% of cases, it is Escherichia coli), the pathogen begins to multiply intensively. A critical increase in pathogen colonies leads to the manifestation of acute signs of cystitis (pain, itching, cramping, frequent toileting). Many factors contribute to the penetration of pathogens into the bladder organ, due to:
- prolonged exposure to cold;
- features of the anatomical structure of the urethral system of women;
- errors in intimate hygiene;
- promiscuous and unprotected sexual relationships;
- hormonal imbalances;
- the influence of concomitant diseases of a urological or gynecological nature;
- surgical manipulations and injuries;
- disorders in the urinary system (stagnation of urine, rare urination).
It is ridiculous to hope for the voluntary “departure” of a pathogenic pathogen. Without appropriate medical therapy, he will never leave the nutrient medium of the urinary bladder reservoir “of his own free will.” Inflammatory reactions are not able to go away on their own, without specially selected therapy and stopping the provocative factors that contributed to its development.
Indeed, sometimes inflammatory reactions in the bladder organ stop without the use of targeted therapy. This mainly concerns manifestations of cystitis of the secondary form, when tissue inflammation in the bladder develops due to the influence of the root cause:
- Urolithiasis (formation of stones in the bladder).
- Strictures of the urethra (narrowing of its internal lumen).
- Gynecological pathologies.
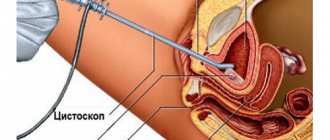
- Catheterization.
Can cystitis go away on its own, albeit figuratively? Let’s look at some striking examples.
Successful treatment of the original source of the disease - removal of stones from the bladder cavity, transurethral resection (elimination of narrowing of the urethra), installation of a cystostomy or relief of gynecological pathologies, leads to self-healing of cystitis. Although we can only talk about this figuratively, since the cure occurred only thanks to the elimination of the background cause.
Relief of all similar pathologies with signs characteristic of cystitis is also regarded by patients as self-healing.
- Signs of the disease that appear after intimacy may be similar (discomfort and pain) to the classic form of infectious cystitis, although in fact they are not it.
- An increase in the resistance of the mucous lining of the bladder provokes the deposition in the tissue structure of the bladder reservoir of immune circulating complexes that cause inflammatory processes, which in no way relates to cystitis, but often becomes the cause of the development of interstitial cystitis. Although a tank culture test does not reveal an infectious pathogen, because it essentially cannot be there. Symptoms often go away soon, but even if they are present, the therapy is similar to the treatment for an infectious form of cystitis. But treatment is longer in nature, with the possible manifestation of frequent recurrent conditions.
- With signs of a neurogenic bladder disorder, the reasons are completely different, but the clinical picture is very similar to inflammatory damage to the bladder tissue. Therapy in this case is aimed at treating neurological pathology, and not at stopping inflammatory reactions (which, in principle, should not exist).
Relief of the causative factor does not require additional therapy for cystitis. But it is not correct to assume that the disease went away on its own.
Cystitis must be treated and delay is unacceptable. The processes of inflammation in the bladder will not stop on their own. A decrease in severe symptoms, and sometimes their complete lull, does not indicate a cure. The clinical picture of the disease can take on a hidden, latent character, or enter the chronic stage, which will certainly result in relapses.
In addition, a long-term absence of comprehensive therapeutic treatment can result in dangerous consequences:
- The development of pyelonephritis, due to bacterial damage to the kidney tissue, which can in the shortest possible time lead to complete failure of renal function - acute renal failure, which is a serious threat to the patient’s life.
- Infertility. The proximity of the female organs to the bladder exposes them to a high risk of an inflammatory reaction spreading to them, which can cause the development of salpingoophoritis, endometritis or vaginitis, which negatively affects the reproductive system of women.
- Hemorrhoids and a high risk of developing malignant tumors in the cavity of the final segment of the large intestine (rectum), when inflammatory reactions spread to it.
- Septic foci in various parts of the body. The presence of purulent processes during inflammation causes melting of the vascular walls. The entry of infection and purulent inclusions into the blood leads to the development of various local foci of purulent infection, including the peritoneal cavity, liver and brain.
- The development of multiple diverticulum cavities (protrusions) in the bladder, which becomes the main cause of persistent urinary retention and constant pain.
You should not self-medicate. Not a single attempt has yet been crowned with success, and no one has been able to completely overcome the inflammatory process in the bladder without medication. It is impossible to decide on your own that the disease has passed.
It is possible to understand that cystitis has passed only by how urine tests have changed after treatment:
- there should be no trace of bacteria in it;
- undetectable mucus;
- the presence of blood cells (erythrocytes and leukocytes) and epithelium should not exceed the norm;
- An important indicator is the acidity of urine; it should not have an alkaline structure.
Only after proper therapy and repeated monitoring of urine, which will meet all indicators, can we say with confidence that the disease has passed.
Can cystitis go away without treatment Link to main publication
Cystitis is an extremely unpleasant disease. But many people hate problems with making appointments with specialists and tedious waiting in line more than all their ailments.
In addition, among the arguments in favor of ignoring clinics are doubts about the competence of doctors and the high cost of drugs.
Most are accustomed to enduring mild colds on their legs, resorting to course treatment only in the most serious cases.
Causes of cystitis
To find the answer to this question, you need to understand how cystitis occurs and occurs. Often this is not the name given to a specific disease, but to symptomatic inflammation of the bladder, leading to disruption of its functioning. There are dozens of possible causes for cystitis. First of all, a distinction is made between primary and secondary cystitis.
Secondary accompanies diseases of the urinary system such as various tumors, kidney stones, and also often accompanies the development of sexually transmitted infections.
Primary occurs due to various reasons, but if left untreated, it can develop into a chronic form and even lead to other, more serious ailments. Most often, discomfort appears after:
- Hypothermia.
- Injuries to the mucous membrane, for example, caused by the use of a urinary catheter.
- Contact with harsh hygiene products.
All these factors are often just catalysts. In 80% of cases, the main culprit of the disease is an infection, which can be the most common E. coli.
In a healthy state, the body suppresses the proliferation of harmful bacteria, but as soon as it weakens, the pests get out of control.
Some people have a high tolerance to external factors, while others only need to be in a draft and then suffer for a long time from frequent painful urges to go to the toilet.
Why is cystitis dangerous?
If we continue the analogy with respiratory tract infections, then similarities can be found in the consequences of acute cystitis.
Just as a simple acute respiratory infection, if left untreated, can “go downhill” and develop into bronchitis, and in severe cases, pneumonia, so inflammation in cystitis can spread beyond the bladder mucosa.
In this case, the infection makes its way up to the kidneys. If you completely ignore the body’s alarm signals and endure pain, you can successfully develop pyelonephritis.
On one's own
How the disease develops
However, for the disease to begin to develop, penetration of the pathogen is not enough. This must be a large number of microorganisms that first adhere to the inner lining of the bladder, then penetrate into its upper layer. If microorganisms have managed to stick to the mucous membrane, then a normal stream of urine can no longer wash them away. The colony of pathogenic microflora grows, and when a critical mass is reached, the inflammatory process begins. The infection manifests itself with characteristic signs:
- pain and stinging when urinating;
- unbearable desire to urinate;
- frequent visits to the toilet several minutes apart.
Thus, the answer to the question: can cystitis go away on its own without treatment is negative.
Lack of treatment for a bacterial infection leads to the fact that the inflammatory process affects the deep layers of the wall of the bladder. This in turn contributes to a change in the structure of tissues and a decrease in the volume of the organ.
Chronic cystitis occurs in every second woman who has had an acute form of the disease. Relapses occur 3 or more times a year. Chronication of the process is facilitated by:
- incorrectly selected medications and uncontrolled course of treatment;
- overly active sex life;
- presence of genital infections;
- stress on the lower back (for example, wearing high-heeled shoes);
- using the wrong underwear (thongs).
During the period of chronicity, structural changes in the walls of the bladder outstrip the manifestations of this process, and the disease can be triggered.
The danger of self-medication
Uncontrolled use of antibiotics is dangerous. Drugs in this series are used only in the presence of infection.
Uncontrolled use of antibiotics is dangerous. Drugs in this series are used only in the presence of infection. Incorrect selection and illiterate use can lead to disruption of the microflora. As a result, other pathogens may enter the bladder. Failure to comply with dosages and course duration leads to the development of resistance in bacteria. In such cases, it is necessary to use outdated remedies or medications with powerful side effects.
In the absence of adequate therapy, pathogens spread throughout the body. They can be transported in urine, lymph or blood. When microbes penetrate the kidneys, pyelonephritis develops. In men, inflammation of the prostate gland or testicles often occurs. In women, the pathogen can enter the uterus and ovaries. As a result, complications such as infertility and impotence develop.
In the inflamed organ, the mucous membranes are destroyed. Microbes penetrate deeper into the walls. This leads to the development of hemorrhagic cystitis. Ulcers and erosions appear in the bladder. Blood clots are found in the urine, the color of the liquid becomes saturated. Depending on the time the red blood cells remain in the cavity, the color of the urine changes to brown or scarlet. Severe bleeding requires hospitalization.
Treatment of cystitis in children
Symptoms and treatment of cystitis
all about cystitis
Subsequently, functional tissues are replaced by connective tissues. The bladder partially or completely loses its capacity. The patient has problems with bowel movements: incontinence, frequent urges, etc. Obstruction may develop due to the formation of adhesions. The mucous membranes begin to die. Necrosis is accompanied by the release of purulent exudate. When ruptured, peritonitis develops. Lack of help is fraught with death.
Symptoms of sand in the bladder and kidneys
The initial manifestations of urolithiasis may not have any obvious signs. Just cloudiness and a little suspension in the urine. You may not even realize that there is sand in your kidneys. Especially if you don’t look closely at what the fluid removed from the kidneys looks like. However, it is at this initial stage of nephrolithiasis that it is optimal and most effective to treat sand in the kidneys, preventing the formation of large stones.
Causes of sand in the urinary tract
It is extremely rare that kidney stones form without any cause or external symptoms. This may include trouble urinating or changes in urine color. If there are small grains of sand in the urinary sediment, then we can safely assume that the sand in the bladder appears from the kidneys, because small pebbles up to 1 mm in size easily exit through the ureters. The reasons for this condition are:
- disturbances in mineral metabolism that occur due to improper monotonous nutrition or an overdose of complex vitamin preparations;
- chronic inflammation of the urinary tract (pyelonephritis, nephritis, cystitis), contributing to nephrolithiasis;
- hormonal problems, which is more typical for women;
- general diseases (endocrine and intestinal), which is more common in men.
Approaches to the treatment of kidney stones in men and women are the same, but some features should be taken into account:
- For men, infectious pathologies, metabolic disorders and poor nutrition are more common.
- In women, local inflammation (cystitis), pregnancy complications (gestational pyelonephritis, congestion during pregnancy) and gynecological diseases are of greater importance.
Do not think that sand in the kidneys is an accident that will disappear without consequences. The problem always arises against the background of certain reasons and is manifested by typical signs of the onset of nephrolithiasis. Even if you try to remove the sand in the bladder on your own, this does not at all guarantee getting rid of kidney stones.
Characteristic symptoms
When sand and kidney stones appear, the following symptoms will occur:
- pain in the side caused by the irritating effect of small stones on the inner surface of the ureters;
- slight temperature reaction with an increase in the evening, which is explained by inflammation in the urinary tract;
- an unpleasant and painful process of emptying the bladder, when sand flows through the urethra;
- external changes in urine in the form of cloudiness and sediment.
Sometimes stones and sand in the kidneys manifest themselves as typical symptoms of exacerbation of chronic pyelonephritis, or blood can be detected in the urine if small stones injure the walls of the ureters.
Sand in the bladder, which often has no symptoms, always indicates an increased risk of urolithiasis. It is advisable to do something before serious problems arise in the urinary tract. The best option is to see a doctor and try to remove the sand from the kidneys. This will be the optimal method for preventing complicated forms of nephrolithiasis.
Diagnosis of the initial stages of urolithiasis
Before treating sand in the kidneys yourself, you should confirm the presence of pathology. It is necessary to make sure that there is no tumor, coral stone in the kidney or hydronephrosis. It is optimal to undergo a full diagnosis, for which you need to see a doctor. General clinical tests and ultrasound scanning are usually sufficient to detect nephrolithiasis. The specialist will see the reasons for the formation of sand and will notice problems in the ureter if microlith flows through it. And pay attention to the release of small stones from the bladder.
Therapeutic measures
If the question arises of how to treat sand in the kidneys, then the answer should be sought from a specialist.
The doctor will be able to explain why medications are used and tell you what to do to reduce pain in the side. This is especially important in cases where the microlith in the kidney is slightly larger than 8 mm and goes along the ureter: painkillers will help to survive the advancement of the stone. Diet for sand in the kidneys will be of great importance for treatment. Often it is enough to follow the diet recommended by the doctor to stop the sand from coming off. Why you just need to exclude foods that provoke metabolic disorders. It is advisable to increase the volume of fluid you drink, giving preference to mineral water recommended by your doctor.
The following medications will be effective for men and women:
- uroseptics with anti-inflammatory effects;
- diuretics;
- special medications for litholysis.
A good option for preventing kidney stones is a diet for sand in the kidneys and increasing water load. If everything is done in accordance with your doctor's recommendations, you may not need to use medications. However, the very fact of identifying small grains of sand in the urinary sediment indicates a high risk of nephrolithiasis.
Consequences
Negligence in the treatment of cystitis is unacceptable. The main manifestations will not go away on their own!
If cystitis is not treated with the presence of imaginary features of complete health, inflammation can develop and then manifest itself in a more severe form.
Due to the appearance of purulent elements in the genitourinary system, pain and resistive sensations will be unbearably and painfully disturbing. In such conditions, it will be very difficult to alleviate the inflammatory exacerbation and will lead to generalization processes with damage affecting neighboring organs (renal, prostate, gynecological systems). All this can contribute to the emergence of threats to the health and life of the patient.
Disease prevention
In order to reduce the risk of cystitis, you must follow simple rules:
- do not overcool;
- observe the rules of genital hygiene;
- feet should always be warm;
- refuse synthetic underwear;
- do not wear thongs;
- follow a diet, do not abuse salty and smoked foods;
- promptly treat infectious diseases;
- regularly visit a gynecologist (male urologist) to treat diseases;
- to live an active lifestyle;
- when working sedentarily, take a break every 2-3 hours;
- drink 1.5-2 liters of water daily;
- strengthen the immune system.
With the right approach to treating cystitis, the symptoms of the disease disappear within 2-3 days. The course of prescribed medications must be completed to the end. Lack of treatment will lead to complications that are difficult to get rid of.