The successful functioning of the body is ensured by special substances of internal secretion - hormones, which control and ensure constancy in the internal environment of the body. Disruption of their balance leads to unstable hormonal levels, which negatively affects, first of all, the human psyche and nervous system, subsequently manifesting itself in various dysfunctions in organs and systems. Hormonal cystitis is a clear confirmation of this.
Not everyone understands the mechanism of dependence of inflammatory processes in the bladder walls on the imbalance of hormones in the body. Let’s try to figure out what is unique about the manifestation of this pathology, and whether it is possible to cope with it without any special “losses.”
A little about the main thing
Let us immediately note that the hormonal type of cystitis manifests itself exclusively in females. Unlike women, the hormonal level of the stronger half of humanity remains almost unchanged throughout life. Only closer to old age may there be a decrease in the secretion of androgens or testosterone. This happens so imperceptibly and gradually that men do not even notice that their new life cycle has begun.
Unlike the male sex, a significant decrease in the secretion of female hormones occurs during the premenopausal period (40–45 years), and monthly in young women of childbearing age during the regulative cycle (menstruation). In any case, the dominant role belongs to female steroid hormones, estrogens, the low level of which can significantly affect the functional state of the whole organism.
Prevention
Disease prevention is aimed at timely elimination of infections of the genitourinary system. Compliance with your doctor’s personal hygiene instructions and taking medications that balance hormones and immunity will help avoid the development of complications. For women who are prohibited from taking contraceptives, they should try to avoid stressful situations. Additionally, a diet is followed, the use of natural vitamins is prescribed, and it is mandatory to get rid of alcohol and smoking. Preventive measures are more relevant for women during menstruation.
Main causes and symptoms
The role of estrogens is not limited to ensuring the reproductive ability of women, as many people think. They perform a protective function in the bone, vascular and cardiac systems. Their effect on the genitourinary system is due to the strengthening of cell membranes in the renal tissues, the mucous lining of the urethral tract and the bladder organ.
Under the influence of estrogens, the tissue structure acquires firmness and elasticity, the permeability of the bladder walls decreases, which prevents irritation of the nerve endings and stabilizes the functions of the detrusor.
A severe estrogen imbalance in the body occurs immediately before the onset of menstruation, completely changing the mechanism of natural functions of the female body.
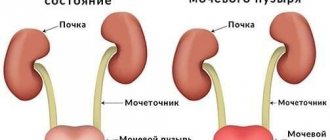
A decrease in estrogen secretion leads to thinning of the mucous lining in the urinary organs with the formation of many cracks on its surface, facilitating the introduction of pathogens and the development of infectious and inflammatory processes with frequent relapses.
Similar “metamorphoses” with hormonal imbalance occur in older women (in the menopause phase) who have passed childbearing age, because the body no longer needs stable secretion of the required level of estrogen.
There is also a special risk group among women, most susceptible to the development of infectious and inflammatory processes with the genesis of hormonal imbalance:
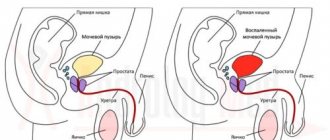
- Patients with gynecological diseases. For example, inflammatory processes in the appendage system, which significantly affects hormonal secretion, causing a significant imbalance in the body. Cystic and tumor neoplasms, uterine fibroids, or endometriosis are all diseases that affect almost a third of the female population. Before menstruation begins, myomatous nodes or the mucous lining of the uterus swell. Since the uterus is anatomically located close to the bladder, it creates pressure on its walls, provoking the symptoms of cystitis.
- Teenage girls. It is too early to judge the current regulative cycle based on the first menstruation. At the age of puberty, it changes until a certain interval (28–30 days) is established between cycles. And it is incorrect to say that an estrogen imbalance at this age will necessarily lead to the development of infectious and inflammatory reactions in the bladder walls. Because violations of this nature cannot be the cause of cystitis, but are only a provocative factor in its development. This means that the young “ladies” already had inflammatory processes in the bladder walls, but the clinical picture may have been of a latent (hidden) nature, without a pronounced manifestation of symptoms, and hormonal changes only led to an exacerbation of the disease.
- Women of menopausal age in whom a decrease in estrogen levels occurs against the background of age-related decline in the natural functions of the ovaries. This fact leads to a decrease in the phagocytic functions of the body, which makes it possible for pathogens to be activated, causing inflammatory reactions in the walls of the cystic cavity.
There are a number of additional factors that provide prerequisites for the development of cystitis of hormonal origin. They are due to:
- violation of vaginal microbiocenosis (decrease in the level of normal microflora),
- lack of hygiene during regular periods (menstruation),
- incorrect selection of hormonal contraceptives,
- decreased immune defense during the menstrual cycle,
- individual intolerance to certain hygiene products.
In principle, any negative changes in health are an excellent background for the introduction of infection, and problems with the balance of hormones during the regulative cycle are generally an entry point for a pathogen. Therefore, women prone to cystitis are advised to take maximum precautions during this period.
Hormonal cystitis from dyshormonal disorder
Diseases of the genitourinary system can be the result of a dishormonal disorder. The state of the protective lining of the bladder depends on the hormonal background of the body. As a result of hormone imbalance, the function of the mucous membrane decreases and there is a risk of developing bacteria and viruses.
The main difference between hormonal cystitis is that its symptoms appear during menopause, before or after menopause, that is, when hormonal changes occur in the body.
- Types of cystitis in women: symptoms and treatment
It should be noted that only women suffer from this form of inflammation. There is almost no change in the hormonal balance in men throughout almost their entire lives. In the age category of 45-50 years, they experience some changes in the form of less androgens and testosterones being produced. This process is so slow and gradual that men’s entry into a new phase of the life cycle occurs unnoticed by them.
With the hormonal background of women, everything is much more complicated. Its changes occur before each menstrual cycle, and it changes especially noticeably with the onset of the premenopausal period. Estrogens play the main role here.
Estrogen is the main female sex hormone that plays a large role in the functioning of the whole organism. Reproductive function and the nervous system are affected by it, it protects the heart, blood vessels, bones, and participates in water-salt metabolism.
In relation to the genitourinary system, estrogens are involved in improving the cellular structure of the bladder membrane. With their help, the fabric becomes more elastic and resilient.
After women reach the age of 45, a woman’s reproductive function decreases; the ovaries produce less steroid sex hormones - estrogens, which can provoke the development of cystitis.
If we talk about changes in hormonal balance during menstruation, the first half of menstruation is accompanied by increased production of estrogen, then their level noticeably decreases, and progesterone is actively produced. Thus, a violation of the amount of hormones can provoke the development of an infiltrated infection.
Lack of estrogen leads to negative changes in the body:
- the mucous membrane of the urinary system becomes thinner;
- cracks appear;
- increased vulnerability develops.
Signs of the disease
The main difference between cystitis caused by an imbalance of hormones and other forms of the disease is the manifestation of signs of the disease before, during, or after regulation. It is at a time when hormonal changes occur in the body, which leads to the activation of pathogenic flora in the bladder walls.
The symptoms of hormonal cystitis are similar to the general symptoms of the disease, manifested by:
- nagging pain and cutting,
- scanty urination,
- constant imperative urges,
- vaginal discomfort in the form of itching and burning,
- changes in the color and structure of urine.
Menopausal women may suffer from involuntary urinary discharge or micturition incontinence.
Symptoms
When cystitis worsens before menstruation, the following signs appear, characteristic of a disease of any etiology:
- problems with urination (frequent urge, painful pain at the end of the process, feeling of incomplete emptying of the bladder);
- a small amount of fluid released;
- cloudiness, change in color and odor of urine;
- pain in the lower abdomen and perineum;
- sleep disturbances associated with nighttime urge to go to the toilet;
- involuntary urination;
- symptoms of general weakness and malaise.
The clinical picture against the background of hormonal disorders in the female body is characterized by additional signs (emotional disorders, decreased memory and concentration, deterioration of skin condition), which requires contacting a doctor for a diagnostic examination.
Diagnostic examination
The diagnostic search includes standard examination methods that are used in diagnosing any type of cystitis:
- laboratory monitoring of urine and blood condition,
- bacteriological test to determine the pathogen (tank culture),
- mandatory identification of the hormonal ratio in the body relative to the norm,
- ultrasound examination at the beginning of the “lunar cycle” and at its end. This method helps to assess changes in the bladder walls and prescribe effective therapy.
Diagnostics
To make an accurate diagnosis, doctors use different methods. First, a woman is interviewed and talks about her condition. Then the patient is examined by a gynecologist to make sure whether the cause of inflammation is related to the improper functioning of the genital organs or not. The suprapubic area is palpated.
The woman is prescribed laboratory tests. A general blood test can reveal an increase in ESR (erythrocyte sedimentation rate) and an increase in the number of leukocytes in this fluid. When examining urine, doctors pay attention to changes in its color and quantity, and detect epithelial particles and bacteria in it.
The woman is prescribed laboratory tests. A general blood test can reveal an increase in ESR (erythrocyte sedimentation rate) and an increase in the number of leukocytes in this fluid.
If cystitis is suspected, a blood test for hormones must be performed. Through this test, specialists determine the levels of progesterone, testosterone and estrogen in the sample. A reduced or increased content of active substances will indicate an imbalance in their balance in the woman’s body.
To determine which microorganisms triggered the inflammatory process, a smear is taken from the vagina and urethra.
To clarify the conclusion, differentiated diagnostics are carried out using instrumental methods that make it possible to distinguish hormonal pathology from other types of cystitis and genitourinary diseases.
Ultrasound examination (ultrasound) of the pelvic organs reveals the disease by deformation of the bladder walls. This method helps determine the cause of the pathology if it is associated with inflammation of the uterus or its appendages.
Cystoscopy evaluates the condition of the mucous membrane of the bladder and determines the type of disease. Using this method, tumors, stones, and ulcers can be detected in the bladder.
Ultrasound examination (ultrasound) of the pelvic organs reveals the disease by deformation of the bladder walls.
Treatment protocol
Therapy for this type of cystitis consists of three areas:
- Relief of pathogenic effects and symptomatic drug therapy - consisting of the prescription of traditional antibiotic therapy in accordance with the resistance of the identified pathogen. Prescriptions of drugs that reduce pathological symptoms - antispasmodic and analgesic medications.
- Eliminate hormonal imbalance. The treatment regimen is drawn up according to an individual treatment protocol.
- Prompt elimination of the causes of hormonal disorders - tumors, cysts, fibroids, etc. For these pathologies, hormonal therapy is not prescribed, since it can provoke the active growth of tumors.
Preventive actions
Acute inflammatory process and relapses of cystitis can be avoided by following preventive measures, including:
- maintaining intimate hygiene, especially during and after sexual intercourse;
- absence of hypothermia and overheating of the body;
- wearing seasonally appropriate clothing and high-quality underwear;
- performing a set of exercises to improve blood flow and tone the muscles of the genitourinary organs (Kegel exercises);
- timely consultation with a doctor in the presence of genitourinary infections;
- taking medications that normalize hormonal levels in accordance with the recommendation of an endocrinologist.
It is important to follow a diet when signs of cystitis occur (refusal to sour, salty, pickled and smoked foods). You should drink more fluids (cranberry, lingonberry juice, rosehip decoction) and eat foods rich in phytoestrogens (legumes, soybeans, nuts, red grapes, sprouted grains).