Urethral stricture is a pathology that is more common in men than in women. The narrowing of the lumen of the urethra causes its partial or complete patency.
In this case, bladder emptying is disrupted, which leads to significant discomfort, and also seriously threatens the patient’s health due to excessive accumulation of urine.
Depending on the causes of urethral stricture in men, treatment for the disease is chosen.
General information
According to statistics, urethral stricture affects 1–2% of the stronger half of humanity and no more than 0.5% of women. This is explained by the structural features of the urinary system. Even the symptoms of patients of different sexes can vary significantly.
Urethral stricture is considered a serious urological problem that requires immediate treatment. If you do not consult a doctor promptly, serious consequences are likely, including blockage of the outflow of urine and kidney failure.
ICD 10 code No. 35.
Anatomical aspects
The prevalence of urethral stricture in men is explained by the extent of the organ, which consists of several sections surrounded by the prostate membrane. Therefore, any infectious or inflammatory process, accompanied by an increase in the size of the prostate gland or injury to the penis, easily leads to compression of the passage and disruption of the outflow of fluid.
In women, the urethra is much shorter, so stricture is rarely detected.
Varieties
Urethral stricture is differentiated depending on etiology, location, and characteristics.
Etiological classification:
- Post-traumatic – the provocateur is damage to the walls of the urethra.
- Congenital - caused by genetic disorders during the intrauterine development of the baby, rarely manifests itself.
- Inflammatory - narrowing occurs due to an infectious-inflammatory process or replacement of connective organ tissue.
- Idiopathic - diagnosed if the cause of the pathology is not clear.
- Iatrogenic – occurs due to improperly performed medical procedures, sometimes the result of medical error.
Pathomorphological changes:
- Primary – not accompanied by complications, first identified in the patient.
- Recurrent - a repeated form, often occurring with the formation of fistulas and abscesses.
By location:
- prostatic;
- membranous;
- bulbous;
- capitate;
- stricture of the external part.
According to the size of the narrowed area of the urethra:
- Short – up to 2 cm.
- Long – from 2 cm.
- Subtotal - 2/3 of the organ is affected.
- Total (panurethral) – along the entire length of the excretory canal.
- Obliteration of the urethra - the passage is completely blocked.
Pathology is also classified depending on the severity of the process.
Stages of development
There are 3 characteristic stages of urethral stricture:
- Initial – accompanied by damage to the epithelial layer.
- Medium – diagnosed in the presence of urine leaks that provoke secondary infection.
- The latter – scar tissue forms and grows, which leads to a sclerotic process.
Important! If you resort to therapy when a stricture is detected at an early stage of development, you can avoid complications that will take longer to treat.
Urethral stricture - symptoms and treatment
Stricture disease of the urethra (stenosis of the urethra) is a fairly common reason for patients to visit a urologist. Stenosis is a complete loss of patency or obstruction. This is a very serious condition that significantly worsens the patient’s quality of life, and sometimes leads to disability.[1][2][13]
The first mention of this disease was found on papyri in the tombs of the pharaohs about 3,000 years ago. Also, references to this problem can be found in the Indian Vedas, the works of Hippocrates and Avicenna.[1][2]
Urethral stricture (after benign prostatic hyperplasia) is the second most common cause of difficulty urinating, affecting 1% of men.[1][3][4][6][11]
Urethral strictures can occur at any age, mainly in males. They are much less common in women.
Unfortunately, at present there is no single definition of urethral stricture that would fully reflect the essence of the ongoing functional changes and would satisfy specialists in urethral surgery. The most commonly used definition is:
A urethral stricture is a cicatricial narrowing of the lumen of the urethra, which is accompanied by obstruction of varying degrees of severity.
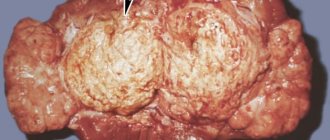
The World Health Organization and the International Association of Urology (SIU) recommend a definition that defines urethral stricture as fibrous narrowing/stenosis of any part of the urethra surrounded by the corpus spongiosum, resulting from the formation of spongiofibrosis.[11] Narrowing of the posterior urethra that is not associated with a pelvic fracture is termed stenosis. Not recommended terms include “posterior urethral stricture” and “bladder neck stricture.”[7]
Most urethral strictures are acquired. There are four main reasons:
- iatrogenic;
- idiopathic;
- traumatic;
- inflammatory.[7][13]
The largest share is occupied by iatrogenic urethral strictures , which, according to various authors, range from 33% to 45%.[1][2][13] Such urethral strictures are a consequence of various urethral (medical) manipulations.
It should be recognized that the increase in injuries (industrial and domestic), as well as the significant development of surgery of the prostate gland, bladder, and the frequent performance of various endourethral manipulations have contributed to a significant increase in the number of patients with cicatricial strictures/stenoses of the urethra.[12]
The leading causes of the formation of iatrogenic urethral strictures:[13]
- Transurethral interventions, including traumatic urethral catheterization.
- Post-catheter strictures:
- ischemic;
- post-inflammatory;
- post-radiation;
- introduction of aggressive chemicals (silver and alcohol-containing substances);
- unsuccessful treatment of hypospadias;
- repeated bougienages.
About 30% of urethral strictures are idiopathic (caused by unknown causes or occurring spontaneously). The most likely cause of such strictures is considered to be a previously undetected minor injury, such as injury to the perineum while riding a bicycle, motorcycle, or horse.[7]
Idiopathic strictures are often localized in the bulbous urethra and occur predominantly in young male patients (48%).[9] Most likely, this is due to an undiagnosed childhood injury or a congenital anomaly of the urethra. In elderly patients, decreased blood supply and tissue ischemia are possible mechanisms.[9]
The next possible cause of the development of pathology is rupture of the urethra as a result of trauma , fracture of the pelvic bones (in 10%) and gunshot wounds. Damage to the posterior urethra due to trauma to the pelvic bones during a car accident occurred in 68-84% of patients, and in 25-60% - due to a fall on the perineum.[1][2][8][13]
Inflammatory diseases , such as bacterial urethritis, balanitis obliterans, lichen sclerosis, can also lead to the formation of urethral stricture. Bacterial (gonococcal) urethritis as a factor in the development of stricture is more common in developing countries. Other reasons make up only a small part.
The main reasons for the development of urethral stricture are presented more clearly in the table below.
| Congenital pathologies | Injuries |
| Idiopathic disorders | Ischemia |
| Infection | Radiotherapy |
| Catheterization | Lichen sclerosis |
| Transurethral manipulation | Failed treatment of hypospadias |
Features in men
The frequency of pathology among men is explained by the length and structure of the organ:
- Prostatic section – the prostate gland is located around it. With her diseases, the canal is easily compressed.
- Membranous – surrounded by the diaphragm.
- Penile – extends to the external opening.
It is worth noting that along its length the male urethra consists of different tissues. Therefore, depending on the location of the damage, the signs of pathology can vary significantly. The most common option is narrowing of the prostatic segment.
Traditional methods of treatment
Procedures of this type at home are a very serious matter that should be discussed with your doctor. The use of traditional methods can eliminate not very pleasant symptoms, but will not completely eliminate the disease.
Leeches, which must be placed on the skin, focusing on the ureteral canal, are considered an effective remedy.
The session is long, lasting up to eight hours. You can also use decoctions made from black currants and lingonberries. To normalize the outflow of urine, decoctions of elderberry, chamomile, juniper and black poplar are used.
Features in women
The urinary tract in women is short and less susceptible to injury. However, the pathology often develops in young women, who are at risk for the growth of scar tissue and narrowing of the passage due to gynecological operations.
The defect develops in any segment of the urethra, and a large area is affected. The danger is that fluid retention leads to bladder overflow, which provokes compression and displacement of other organs, impairing their functionality.
Treatment
In severe cases of the disease, urethral resection is performed.
At the present stage, medical science knows several options for treating urethral strictures. These include:
- observation;
- bougienage;
- internal optical urethrotomy;
- resection of the urethra with the formation of an anastomosis;
- replacement urethroplasty.
Patients with no or few complaints, normal urinary tract conditions and a small amount of residual urine in the bladder can be under medical supervision. In this case, an annual examination is required. Such patients should be aware of the possible risks of disease progression and the need for active treatment in the future.
Urethral dilation is one of the oldest methods of palliative treatment. The purpose of such an intervention is to expand the stricture to a normal diameter (for this section of the urethra). To do this, a bougie of a certain size is inserted into the urethra after local anesthesia and left for 15-20 minutes. This procedure is repeated periodically. The frequency of its implementation is determined by the doctor, focusing on urination parameters.
Internal optical urethrotomy is equivalent in effectiveness to bougienage. It is used for short traumatic strictures of the spongy urethra. Its essence is to dissect the scar in the narrowing zone. It ensures dilation of the urethra if epithelization precedes excessive growth of scar tissue, which does not always happen. After the intervention, a 3-6 month bougienage or autocatheterization is recommended. Most patients have progression of the pathological process after surgery and require open surgery.
Resection of the urethra with terminal anastomosis is an effective radical method of treating traumatic strictures of the membranous and spongy part of the urethra. However, when the urethra is affected by spongiofibrosis, such intervention is accompanied by frequent relapses of the pathological process. This can be avoided by using anastomotic urethroplasty.
Replacement urethroplasty is one of the most complex surgical interventions on the urethra. It is used for urethral strictures longer than 2 cm, as well as in cases where other methods are not effective. The choice of reconstructive surgery technique depends on the location and length of the narrowing, as well as the presence of complications.
When should you be wary?
The clinical picture of the disease largely depends on the intensity of the process and the location of the stricture. Therefore, you should consult a doctor at the slightest change in urination - this will allow you to identify the pathology at an early stage.
Signals for medical help are:
- Pain in the pelvic area.
- Unpleasant sensations during bowel movements.
- Feeling of constant fullness of the bladder.
- Presence of blood in the urine.
- Leakage of a small amount of liquid after visiting the toilet.
Important! One of the characteristic signs of a stricture is a tight abdomen, which is explained by problems with urine output.
Causes
The etiological conditions of narrowing of the urethra come down to three large groups: inflammation of the urethra; traumatic injuries; ulcerations.
• Inflammation of the urethra
Urethritis belongs to the first group, but not all to the same extent. While superficial and short-term aseptic or bacterial non-gonococcal inflammations remain without influence on the caliber of the urethra, gonorrheal inflammation often entails a narrowing, firstly, due to the intensity of the inflammatory process, and secondly, and this is most important, due to its chronic course and its returns. Indeed, urethral strictures with chronic and recurrent gonorrhea occur in those places where old urethritis stubbornly persist. If, as an exception, they are observed in the second year after the onset of urethritis, then in general they are detected only after 3 or 4 years. Therefore, strictures are most often observed in middle age, between 30 and 50 years.
• Traumatic injuries
Large urethral injuries, wounds and ruptures, when left to their own devices, inevitably entail strictures, and the extent of these latter in relation to the circumference of the urethra, as well as the degree of closure of its lumen, depends on the intensity of the injury itself. Damage to the mucous membrane from stones, stone fragments, foreign bodies, false passages, damage due to inept catheterization can also become the starting point for the formation of strictures. In addition, they can be caused by cracks in the mucous membrane due to a strong and rapid erection, due to the sudden straightening of a tense penis, etc. If these microtraumas are formed during gonorrhea, then they have an even stronger effect in the sense of narrowing of the urethra and give rise to mixed strictures of a kind structures (sclerotic-cicatricial strictures). Rupture of the gonorrheal chord may be a type of these strictures. Through slight disruption of the integrity of the mucous membrane of the urethra, those strictures are formed that are caused by excessively frequent sexual intercourse and prolonged erections, masturbation.
Inadvertent cauterization of the urethra can be included in this etiological group of injuries.
• Ulcerations
No matter how rare urethral ulcerations may be, they still exist, and they constitute the third group of exceptional causes of stricture formation.
The main cause is gonorrheal ulceration. Strictures developing after simple or syphilitic chancre are observed very rarely, since this type of venereal infection, very exceptional even in the area of the external opening of the urethra and the navicular fossa, is extremely rare in the deeper parts of the urethra.
Main reasons
Among the factors leading to the development of the defect, congenital make up only 2%, iatrogenic 13%, inflammatory 15%, post-traumatic 70%.
It is possible to trace which provocateurs most often lead to pathology.
| Type of stricture | Causes |
| Post-traumatic | Penetrating wounds, blunt trauma, fracture of the penis or pelvic bones, the presence of a foreign body in the lumen, chemical and thermal burns |
| Iatrogenic | Carelessness when performing procedures in men such as cystoscopy, urethroscopy, catheterization, bougienage, penile replacement, stone removal, brachytherapy In women - cervical amputation, vaginal hysterectemia, birth injuries |
| Inflammatory | Urethritis caused by tuberculosis, gonorrhea, chlamydia, balanitis, diabetes mellitus, decreased blood flow in the urethra, arterial hypertension, metabolic disorders, cardiac ischemia, vascular atherosclerosis, oncology |
| Congenital | Genetically determined anomalies during intrauterine development |
As an independent problem, stricture is rarely diagnosed.
Causes of stricture formation
Any damage to the mucous membrane and spongy body of the urethra leads to the formation of a scar that can change the diameter of the urethra. The most common causes of urethral strictures are:
- traumatic effects (blunt or penetrating trauma to the pelvic ring, perineum and genital organs; damage as a result of intraurethral manipulations and surgical interventions; chemical burns);
- inflammatory process (gonorrheal urethritis; xerotic obliterating balanitis; damage to the urethra due to prolonged stay of the catheter, endoscopic procedures and operations that contribute to microtrauma of the mucous membrane and provide access to the penetration of infectious agents);
- congenital anomalies.
Inflammatory strictures of the spongy urethra are characterized by:
- latent onset of the disease;
- slow progressive course;
- lack of clear boundaries of damage to spongy tissue;
- alternating areas of active inflammation with completed spongiofibrosis;
- periurethral fibrosis involving the membranes of the testicles, muscles and tissue of the perineum in the pathological process.
In some patients, the cause of urethral stricture cannot be determined. In this case, the history does not reveal injuries, urethritis, catheterization, etc. In such cases, a diagnosis of “idiopathic stricture” can be established.
Symptoms of the disease
The main signs of pathology include:
- Delayed urination or complete absence.
- Weak liquid flow, splashing.
- The need to strain the abdomen during the process of emptying.
- Feeling of bladder fullness after going to the toilet.
- Liquid leakage.
- Pain in the pelvic area.
- The presence of blood in urine or semen.
The clinical picture often develops rapidly, the symptoms appear clearly. During sexual intercourse, the secretion of seminal fluid decreases.
Rehabilitation period
After procedures to expand the urethra, a period of rehabilitation is necessary. During this time, you must adhere to the following rules:
- Take antibiotics and painkillers regularly as prescribed by your doctor.
- If you have a catheter, you need to take care of it regularly.
- For 2 weeks after surgery, you should avoid taking a bath, visiting a pool, sauna, steam bath, or swimming in open water.
- It is possible that to prevent scar tissue from blocking the urethra again, the catheter will have to be inserted and removed several times a week.
- For a month after the procedure, you should not lift weights or engage in heavy physical labor.
- It is necessary to drink enough fluid. It is not recommended to drink carbonated drinks and alcohol.
- You need to eat right and avoid eating salty and sour foods.
- You should not have sex for two weeks after surgery.
- If you have problems with urination, the catheter does not drain urine, the volume of urine or frequency of urination has changed, signs of inflammation or a large amount of blood in the urine have appeared, you should immediately consult a doctor.
Possible complications
If urethral stricture is not treated, severe consequences develop over time:
- Atrophy of the bladder as a result of overstrain of muscle tissue.
- Infectious and inflammatory processes due to constant stagnation of urine, which easily become chronic. These include cystitis, orchitis, pyelonephritis.
- Renal dysfunction, renal failure.
- The formation of stones is urolithiasis.
- Hydronephrosis of the kidneys, characterized by dilation of the pelvis of paired organs.
Even after surgical treatment, the following complications are possible:
- Recurrence of stricture.
- Bleeding.
- Blood saturation of the spongy tissue of the penis, which promotes fibrosis.
- Displacement of the stent installed in the lumen of the canal, which causes pain in a sitting position and during sexual contact, injures the mucous membrane of the organ.
To avoid complications, it is necessary to resort to examination at the first signs of a defect.
Why is it important to get rid of urethral stricture?
If urination occurs with difficulty and the outflow of urine is disrupted, then an infection begins to multiply in the urinary system, as a result of which, first of all, the kidneys suffer.
The most serious complication of urethral stricture is renal failure, that is, the inability of the kidneys to work, which can threaten the patient’s life.
Urethral stricture can lead to the formation of urinary stones and contribute to the deterioration of bladder function. In severe cases of stricture disease of the urethra, the latter completely loses its patency and independent urination becomes impossible.
If the patency of the urethra is not restored, urine excretion in such a situation can only be carried out through a catheter installed in the bladder through a puncture in the lower abdomen (epicystostomy). It must be remembered that a person has one urethra. If it narrows, then there is no paired organ that could replace it. A dysfunctional urethra poses a big problem for the functions of the entire urinary system.
Diagnostics
To draw up a quality therapy program, it is necessary to identify the cause of the narrowing of the urethra. To do this, the patient is prescribed the following procedures:
- They take a smear from the urethra for bacteriological culture, direct immunofluorescence, PCR - they help identify the infection or antigens, DNA of the pathogen.
- General urine test for the level of leukocytes, red blood cells, protein, and the presence of pus.
- Uroflowmetry - to determine the speed of urine movement.
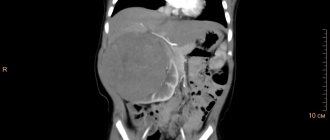
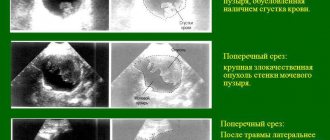
- Ultrasound of the bladder and pelvic area, kidneys - makes it possible to visually assess the volume of residual urine and identify lesions of other organs.
- Urethrography or radiography - if stones are suspected.
- Rectal palpation - to study the size and texture of the prostate gland.
- Multislice computer voiding cystourethrography - CT for layer-by-layer examination of tissues during the process of emptying.
- Cystoscopy is an examination of the bladder with a cystoscope with a built-in camera.
The treatment regimen is based on the results obtained. It is advisable to give the urologist a detailed description of the clinical picture so that a medical error does not occur due to the similarity of symptoms with signs of other problems of the genitourinary system.
Important! Depending on the cause, the diagnostic program can be expanded.
Clinical manifestations
Difficulty urinating and weak urine stream are the main symptoms of urethral stricture.
Patients complain of difficulty urinating , up to the inability to urinate at all. The stream of urine is weak and splashes in all directions, which leads to particular discomfort for patients. Every time they have to clean up urine that does not end up in the toilet and even change clothes after urinating. Almost all patients note leakage of urine into their underwear, which requires pads and frequent changes of underwear.
The act of urination, as a rule, is not complete, does not lead to a feeling of emptying the bladder, and as a result, frequent repeated urges . Many people note pain and pain during the act of urination and immediately after it. There may be blood and purulent inclusions in the urine. Sometimes patients experience pain in the penis during erection, painful ejaculations, blood in semen and pain in the pelvic area.
It should be noted that most of the symptoms described above can occur with other diseases of the genitourinary system. For example, with prostate adenoma, acute and chronic prostatitis, etc. Very often, patients who have not been thoroughly examined are unsuccessfully treated for prostate pathology, which steadily recurs due to regurgitation (backflow) of urine and constant reinfection of the prostate gland with the pathogen contained in it.
That is why a complete and timely examination of patients with suspected urethral stricture is so necessary for the correct selection of treatment.
If at least one of the above complaints appears, you should contact a specialist and under no circumstances engage in self-diagnosis!
After a thorough history taking, the doctor will be able to preliminarily suggest a possible cause of the disease and prescribe the necessary research methods.
Pathology therapy
In the vast majority of cases, the defect is treated surgically. Conservative methods are indicated if the stricture is infectious in nature - as an additional measure, antibacterial and anti-inflammatory drugs are prescribed, with the help of which they destroy pathogens and reduce severe symptoms.
Stricture surgery
Which operation is indicated for the patient depends on the severity of the pathology, the size of the stricture, the number of narrowings, and the presence of complications. There are several common methods that allow you to remove the defect, restore the natural flow of urine, and eliminate the clinic characteristic of the disease.
Bougienage
This operation involves widening and stretching the canal by installing a special metal rod or balloon catheter. The indication is the presence of a lesion no more than 2 cm long or a single stricture with a uniform narrowing of 5–6 cm in length.
Flaws:
- The risk of complications caused by organ injury and the general condition of the patient. Sometimes the urethra has to be not just stretched, but torn.
- Frequent relapses. At the same time, there is an increase in the size of the scars.
- It does not allow you to restore blood circulation, violations of which often become the cause of the defect.
Important! Repeated use of the procedure is not recommended.
Optical urethrotomy and laser treatment
Internal optical urethrotomy is performed for small strictures. Using a urethral cystoscope, the affected section of the organ is dissected and a metal rod is inserted. However, the technique does not completely heal the patient, since after an operation of this type, after 2–3 months, the urinary canal is again subject to narrowing. The exception is if the process proceeds with minimal fibrosis and it is possible to completely excise the connective tissue.
Optical urethrotomy is not repeated.
Laser surgery is considered the least traumatic. Sclerotic areas of the mucosa are burned out with a laser. After the procedure, anti-burn solutions and ointments are used to treat wounds. But even with this technique, relapses are observed in 40–50%. In many ways, the risk of re-development of the pathology depends on the correct selection of medications during restoration.
Stenting
A special spring or stent is inserted into the lumen of the urethra, which allows you to expand the canal in a narrowed area. The operation is rarely practiced, since there is a high probability of side effects, for example, displacement of the stent, which leads to injury to the wall. As a rule, the technique is indicated if the stricture is less than 0.5 cm.
Excision of part of the urethra
A urethroscope is used to resect the urethra or a limited area thereof. After excision of the damaged segment, the ends of the urethra are sutured. If it is necessary to remove a large part of the passage, complex surgery is performed, including excision of tissues, as well as their replacement with a graft made from the mucous membrane of the patient’s lips or cheeks, or foreskin. When it is necessary to completely remove the urethra, a special catheter is inserted, through which urine is removed.
Replacement urethroplasty
This technique is preferable when it comes to both small and extensive defects located in various parts of the urethra. The method allows you to completely cure the patient if the length of the stricture is no more than 1 cm. A positive result is achieved in 80%.
As a rule, damaged tissue is removed with a laser, and a graft is sewn in its place. Relapses occur in only 10%.
Traditional methods of treatment
Therapy at home involves the use of decoctions of medicinal herbs. They are most often prepared from the following plants:
- black poplar;
- juniper;
- elderberries;
- chamomile;
- currants;
- bearberry;
- yarrow;
- St. John's wort.
Such drugs enhance the diuretic effect and have anti-inflammatory properties, therefore the use of folk recipes during the recovery period is indicated.
Examples:
- Currant leaves are poured with boiling water and left in a closed container for several hours.
- Mix birch leaves, bearberry and licorice. Pour 12 g of the collection with water and keep in a steam bath for 15 minutes. Then the broth is infused in a thermos.
Important! Not every stricture can be treated with traditional methods. Often the use of herbs provokes an increase in the defect. Before resorting to home therapy, consult a urologist. In addition, it is necessary to take into account contraindications to medicinal formulations, for example, an allergic reaction to the components.
Another way is to use leeches, which are placed directly on the ureter area. A hirudotherapy session lasts up to 8 hours. The procedure must be performed by a specialist and only with the permission of a doctor.
Features of treatment
This pathology must be treated under the supervision of doctors. Basically, surgery is used to correct the problem. M.I. Kogan in his description identifies several types of procedures:
- Stenting. This method is used extremely rarely, as there is a risk of displacement of the implanted fragment.
- Bougienage. In this case, the narrow section is eliminated using a metal tube. The internal diameter of the duct increases as the tissues move apart. The price of this procedure is small, but it has several disadvantages: there are frequent cases of relapse of the disease, after which it is no longer possible to use this type of intervention, since the tissues will no longer recover. As a result, inflammation may occur.
- Urethrotomy. It is performed using a cystoscope. The problematic part is simply removed. Despite the fact that re-narrowing rarely develops, such an operation cannot be performed again.
- Endoscopy. This method of therapy is prescribed at the initial stage of the disease.
- Urethroplasty. It gives a positive result in 90% of cases and involves the replacement of damaged tissue. If the length of the structure is large, then the victim requires a donor.
- Laser therapy. Areas affected by fibrosis are burned out. After the procedure, a small wound surface remains, for the treatment of which an ointment prescribed by a doctor is used. This operation is relatively new and, despite the high cost, has mostly positive reviews. The use of laser is characterized by certain contraindications. It should not be prescribed to people with an increased level of tissue epithelialization.
After surgery, rehabilitation is required. It involves taking medications prescribed by a specialist, a balanced diet, caring for the catheter (if installed), and avoiding intense physical activity. It is also necessary to consume enough liquid.
It is important to know! Some hospitals provide a quota for surgical treatment of the disease, but this information must be obtained individually at the selected institution. For urethral stricture, surgery is the only possible method of getting rid of the problem.
Rehabilitation after illness
Since stricture therapy is performed surgically, you need to carefully monitor the condition of the wound and avoid urine leakage into the area of the postoperative suture. Therefore, patients are fitted with a catheter, which facilitates the removal of fluid.
However, this method also provokes complications, for example, cystitis. To prevent an inflammatory process from developing, you need to change the tube at least once every 7 days, treat the bladder with antiseptic solutions, which are infused directly through the catheter.
Physiotherapy is also indicated for quick recovery - galvanization, diathermy, magnetic therapy. The procedures promote healing and increase the flow of oxygen to tissues by normalizing blood circulation.
Features of nutrition and lifestyle
Urethral strictures and surgical treatment provoke the formation of sand and stones. Therefore, patients should adhere to dietary table No. 7 in preparation for surgery and during the recovery period.
Basic recommendations:
- Minimize the number of dishes and foods that can increase the volume of daily urine.
- Avoid alcoholic drinks.
- Completely avoid seasonings, marinades, hot spices, fatty and fried foods that increase thirst.
Physical activity is limited at first, but as rehabilitation progresses, sports activities are encouraged.
Disease prevention
To prevent urethral stricture from developing, you need to take care of your health. Recommended:
- If inflammatory processes occur in the genitourinary system, begin treatment without delay.
- In case of injury, it is important to immediately consult a doctor and, if necessary, agree to surgery.
- Avoid inserting foreign objects into the urethra.
- Observe personal hygiene rules.
- Strengthen your immune system and lead a healthy lifestyle.
If you suspect the development of the disease, it is important to immediately consult a urologist for an examination.
Prognosis and prevention
There are several rules that you can follow to reduce the risk of pathology.
- To avoid treatment of urethral stricture in men and women, you should protect yourself during sexual intercourse and avoid casual relationships. Sexually transmitted diseases are one of the reasons for the development of the defect.
- Use personal towels for genital hygiene.
- It is advisable to perform medical procedures involving catheterization with caution.
- Do not expose the lower abdomen to risk of injury.
- Undergo preventive examinations.
- Treat diseases of the genitourinary system in a timely manner.
- In the autumn-winter period of the year, avoid hypothermia.
The prognosis for early detection of the problem is favorable. Therefore, at the first warning signs, you should visit a doctor. The more you start the process, the less chance of complete healing.
Types of disease
The disease occurs more often in men, which is due to the more complicated structure of the ureteric passage. Based on the nature of its appearance, stricture can be congenital or acquired. For etiological reasons, this disease is classified into:
- traumatic, received at birth;
- inflammatory;
- idiopathic.
The last option is mentioned if it is not possible to detect the cause of the disease. Taking into account the characteristic features of the deviation, the disease is divided into primary, relapse and complex. Taking into account the pathologies found, several types have been identified:
- prostatic;
- membranous, bulbar;
- penile;
- capitate.
Diagnosis of pathology
For both sexes, diagnosis of pathology involves a number of the following studies:
- Ultrasound of the urethra and empty bladder. Allows you to clarify the localization of the narrowed area, the cause, and determine the amount of residual urine;
- CT, MRI with contrast agent. Allows you to determine the size and type, localization of the narrowing of the urethra;
- urethroscopy. Gives an idea of the condition of the internal walls of the urethra;
- OAM. Assessment of the functioning of the urinary organs;
- bacterial culture. Urinalysis to rule out infections;
- uroflowmetry. The rate at which the bladder empties is determined.
Ultrasound is one of the methods for diagnosing the disease
For men, palpation examination of the condition of the rectum and prostate area is provided for their damage.