Urethral hypermobility and postcoital cystitis in women
One of the types of inflammation of the bladder is postcoital cystitis (that is, cystitis that occurs after sexual intercourse). In these cases, bladder inflammation that occurs after sexual intercourse is facilitated by abnormal anatomical features of the woman's urethra, such as a low position or hypermobility of the urethra (excessive mobility of the distal urethra). The consequence of this is that during sexual intercourse the urethra moves into the vagina, and due to friction (the process of the penis entering the vagina), flora unusual for the urinary system penetrates through the urethra into the bladder, causing inflammation.
The clinical picture of such inflammation is practically no different from the usual manifestations of cystitis. Unlike cystitis, the trigger for which is hypothermia, postcoital cystitis appears after each sexual intercourse. This forces a woman to limit or avoid sexual relations. A false idea about the true causes of the disease may suggest that the husband has other sexual partners. There may be discord and breakdown in the relationship between spouses.
Treatment for this abnormal location of the urethra is mainly surgical. Urethral transposition is an operation in which the external opening of the urethra is moved upward by 1.5-2 cm from its original position. The operation is performed in a hospital setting, where the stay takes no more than 1-2 days. In the postoperative period, the patient is not recommended to have sexual activity, usually for 4 weeks, during which complete healing of the postoperative wound occurs. The positive effect of this operation, performed with absolute indications and technically correct, is about 90%. Transposition of the distal urethra is an effective surgical treatment for hypermobility and vaginal ectopic urethra in women. This operation allows the patient to be relieved of postcoital cystitis.
chelnyclinic.ru
Disease prevention
In order to prevent narrowing of the urethra in men, you must adhere to the following rules:
- Avoid casual sex.
- Use condoms during sexual intercourse with new or unreliable partners.
- If you experience symptoms such as pain during urination, rash or discharge, consult your doctor immediately.
- When treating urological or sexually transmitted diseases, follow all doctor's instructions.
- Avoid injury to the genitals.
- You should not abuse solutions of Miramistin and Chlorhexidine, which are used for the prevention of sexually transmitted diseases and are injected directly into the urethra. If you are hypersensitive to such drugs, even a small concentration of substances can cause a burn to the mucous membrane.
If you have problems with urination, you cannot self-medicate, but you must seek help from a urologist. In the early stages, the disease can be quickly cured. Lack of timely treatment may result in the need for several major surgeries.
Hypermobility of internal organs
Hypermobility is a state of increased mobility and flexibility of joints or other internal organs. This is one of the most common pathologies of the musculoskeletal system, which forces patients to consult a doctor for immediate treatment.
Urethral hypermobility in women
With urethral hypermobility, urinary incontinence is often observed. The pathogenesis is based on a violation of the ligamentous and supporting apparatus of the upper half of the urethra. As a result, a displacement of the urethra occurs, in which it moves beyond the manometric cavity.
The clinical picture is represented by hydrocele. Moreover, in most cases, the hydrocele is quite isolated. The severity of this pathology can vary from mild to severe. The main symptom is urinary incontinence. The pathology is especially aggravated by tension. In order to assess the severity of the pathology, a parametric characteristic is used. Usually it is in the range from 6 to 7 points. The presence of a pronounced hydrocele directly or indirectly indicates a severe stage of the disease, in which the motor function of the detrusor is impaired.
The pathophysiology is based on a violation of the transmission mechanism. It should be noted that in most patients, the indicators of hypermobility of the sphincter apparatus are within the age norm. In this case, the most effective treatment method will be surgery. In this case, the main purpose of such an operation is to fix the upper part of the urethra in the area of the manomatric cavity. Theoretically, this could be any of the options for urethropexy.
Most experts are inclined to believe that surgical intervention is required if the parametric indicators of the symptom of urinary incontinence exceed 6 points. Also, an indication for surgical intervention is combined damage to the obturator mechanism of the sphincter apparatus and the urethra. In this case, preliminary drug treatment is usually required.
Biochemists have found that disruption of normal urethral mobility is caused by disruption of normal hormonal levels in women. Typically, the development of this pathology is facilitated by a decrease in estrogen levels in the body. It is logical that the pathology most often occurs in postmenopausal women. It was also found that in most cases these processes are interrelated. Thus, the development of hypermobility also entails hormonal imbalance.
Most experts believe that if urinary incontinence is 5 points or less, it is advisable to carry out complex drug therapy. You can try using physiological methods of influence. Diadynamic methods are the optimal method of treatment. The surgical method is used when other methods are ineffective.
Vaginal cones have proven themselves well as a physiotherapeutic method, which can simultaneously act as a diagnostic factor that allows diagnosing the condition of the vagina and urogenital diaphragm.
You should start with a cone of minimum mass. In this case, the cone must be held in the vagina while in a vertical position. The training can be carried out during the day at any convenient time; no special preparation or training is required. Promotes training and development of the pelvic floor muscles. At the same time, the amount of fluid involuntarily flowing from the urethra is sharply reduced. This training allows you to normalize transmission performance by approximately 5-10%. A woman's ability to hold a cone weighing 50-60 grams for several hours is considered a complete cure.
It is also necessary to take into account that urethral hypermobility is associated with a lack of estrogen hormones; accordingly, hormone replacement therapy is recommended, which can also demonstrate very good results. Teflon ointment has proven itself well, used for mild and moderate stages of pathology.
Testicular hypermobility
In men, testicular hypermobility is often accompanied by postcoidal cystitis that occurs after sexual intercourse. The disease is accompanied by pain, discomfort, a feeling of pressure, heaviness, and cramping. In this case, the pathogenesis is usually based on pathologies of the urethra, a violation of the normal anatomical features of the urethra and urethra. Also, the pathology intensifies when microflora enters the urogenital tract.
Moreover, the clinical picture differs from typical cystitis with its standard manifestations. The trigger for the development of inflammation is physical activity, sexual intercourse, and overexertion. Inflammation develops especially intensely after sexual intercourse, which forces a man to avoid sexual intercourse.
The main treatment method for abnormal location of the urethra is surgery. Transposition of the urethra is used, in which the external opening is moved upward a few centimeters. The operation is simple and is performed in a hospital setting. The patient is sent home within a few days. The recovery period does not last long.
Gastric hypermobility
This condition is usually accompanied by pain in the abdomen and constant heartburn. Quite often a concomitant disease is gastritis. This requires immediate diagnosis and treatment.
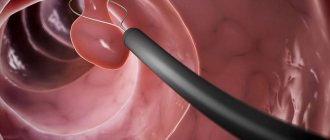
The main diagnostic method is gastroscopy. During this procedure, the membranes and cavity of the esophagus and stomach are examined.
Also often during the study, scrapings are taken from the gastric mucosa. This method allows you to detect bacteria of the Helicobacter genus, which are often the cause of hypermobility, as they cause excessive mobility and swelling of adjacent tissues. Also, the cause of the development of pathology can be the adhesive process.
Hypermobility of the right colon
With increased intestinal motility, motility is impaired, which leads to the development of colitis and various inflammatory diseases of the large and small intestines. In most cases, the pathology is accompanied by constant diarrhea.
The pathogenesis is based on a violation of intestinal motility, in which muscle contractions and peristalsis are significantly accelerated. As a result, the movement of food through the canal is accelerated, and the excretion of feces is accelerated. Pathogenesis can also develop at the cellular level. This damages the cells and disrupts the integrity of the cell membrane. This causes fluid to leak out of the intestines and is excreted in the form of severe diarrhea. As a result, the muscles reflexively contract, causing hypermobility syndrome and constant inflammatory processes.
Itching, burning, and irritation in the anus also develop. Weakness, fatigue, and weakened muscles are often observed. Drowsiness appears. In some cases, nausea and vomiting may develop. If an infection occurs, fever, abdominal pain, headache and muscle weakness are observed.
The danger of this condition lies in the fact that an infection quickly sets in and an inflammatory-infectious process develops. This is accompanied by an increase in temperature and a decrease in immunity. Dehydration is also a common complication.
The disease must be differentiated from infectious and inflammatory diseases, irritable bowel syndrome, ulcers, tumors, and chronic appendicitis. Quite often, this condition develops against the background of gastritis with secretory insufficiency, after gastrectomy, and other operations for various intestinal diseases. Almost always, hypermobility is one of the symptoms of chronic cholecystitis, and also manifests itself against the background of liver and kidney failure.
ilive.com.ua
Symptoms of the disease
A narrowing of the urethra is indicated by problems with urination. The disease can be identified by the following signs:
- In order to begin the act of urination, you need to make an effort.
- The stream of urine weakens and splashes, despite the tension of the abdominal muscles.
- After finishing urination, there is a feeling that the bladder is not completely emptied, and new urges appear.
- In some men, the disease is accompanied by urinary incontinence.
Additional symptoms that indicate the disease:
- Aching pain in the lower abdomen and genital area.
- Weak release of sperm during ejaculation.
- Blood appears in semen or urine.
- Mucous discharge appears after urination.
- Pain and burning may occur in the urethra during urination.
- The volume of urine decreases.
- If almost the entire urethra is narrowed, urine is released in drops.
- With obliteration, urine does not leave the bladder. This is a very dangerous condition and without timely assistance, death is possible.
Note! In women, the disease also manifests itself in the form of disturbances in the act of urination, a feeling of incomplete emptying of the bladder, burning and pain in the urethra. But obliteration is very rare.
Transposition of the distal urethra in the treatment of chronic cystitis
For citation: Pushkar D.Yu., Rasner P.I., Gvozdev M.Yu. Transposition of the distal urethra in the treatment of chronic cystitis // Breast Cancer. 2013. No. 34. P. 14
Cystitis is an inflammation of the bladder mucosa. At least once in her life, every woman in one form or another experiences symptoms of the disease. For many women, this becomes a problem for several years or for life. The most common causes of the onset and then exacerbation of chronic cystitis include bacterial, chemical and other toxic effects, autoimmune reactions, nervous and vascular damage. The development of chronic cystitis is based on processes of impaired permeability of the bladder mucosa against the background of various neurovascular disorders, as well as dyshormonal changes.
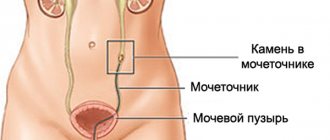
Despite the fact that the cause of chronic cystitis cannot always be determined, most clinicians consider it as a secondary disease, caused primarily by anatomical and pathophysiological changes in the pelvic organs, leading to impaired blood and lymph circulation and supporting chronic inflammation in the bladder. Sexual activity is one of the most important factors in the genesis of inflammatory diseases of the lower urinary tract in women. Moreover, the likelihood of developing the disease largely depends on sexual practice, frequency, regularity and duration of sexual intercourse. There are many similar names that characterize cystitis that occurs after sexual intercourse: “honeymoon” cystitis, “cystitis after sex”, “defloration cystitis”, “genital cystitis”. The term “postcoital cystitis” should be considered the most correct, because it is this name of the inflammatory process in the lower parts of the urinary system in women that is used in special domestic and foreign literature. The ascending route of penetration of microflora into the bladder in women is the main one. The frequent development of cystitis and urethritis is facilitated by the anatomical features of the female urethra: its short length, relatively large diameter and close proximity to the vagina and anus - sources of microorganisms that most often cause the inflammatory process. However, given the same anatomical conditions, the vast majority of women still do not suffer from postcoital cystitis. So what leads to the development of cystitis after sexual intercourse? Among the anatomical causes leading to the development of chronic cystitis and urethritis in women during the sexually active period, the main place is occupied by hypermobility and vaginal ectopia of the external opening of the urethra. Hypermobility is increased mobility of the external opening of the urethra, caused by the presence of adhesions, which are remnants of the hymen. With vaginal ectopia, the external opening of the urethra is located below its usual place - on the border with the entrance to the vagina, and the adhesions are weakly expressed or absent altogether. In both cases, during sexual intercourse, the external opening of the urethra shifts into the vagina with its simultaneous opening, which creates conditions for the penetration of pathogens of the inflammatory process. The penis plays the role of a piston, forcing vaginal contents into the lumen of the urethra. These peculiar anatomical variations in the location of the external urethral opening are one of the most common causes of chronic cystitis. The main symptoms (signs) of cystitis that occurs after sexual intercourse are the appearance of painful, frequent urination, a stinging sensation, a burning sensation several hours (in some cases, a day later) after sexual intercourse. Sometimes these symptoms can occur even after a gynecological examination. The disease debuts from the moment of sexual activity - hence the term “defloration cystitis”. In the future, exacerbations can occur not only after sexual intercourse, but also due to other reasons, such as hypothermia, drinking alcohol or spicy food. Sometimes postcoital cystitis begins with the onset of regular sexual activity or when changing sexual partners. Diagnosis of this condition is not particularly difficult. The anatomical features of the location of the external opening of the urethra are clearly visible during a special examination with a diagnostic Hirschhorn test. However, a significant number of urologists and gynecologists to whom these patients turn are often not informed about this disease, and most urologists do not conduct a special examination of patients in the gynecological chair at all. As a result, treatment is reduced to prescribing courses of antibacterial therapy. The effect of such treatment is extremely temporary. Usually the next sexual intercourse leads to a new exacerbation. The next course of antibiotics, diagnosis of sexually transmitted diseases, unsuccessful examination of the sexual partner, and consultations with related specialists begin. In my practice, I very often encounter similar situations when patients undergo repeated courses of combined treatment and rehabilitation to no avail. All this is accompanied by mental suffering, sexual dysfunction, family problems and significant financial costs. The only pathogenetically substantiated type of treatment for postcoital cystitis is taking an antibacterial or uroantiseptic drug immediately immediately after sexual intercourse. This is the type of treatment recommended by the European Association of Urology. Indeed, there are patients who benefit from this type of treatment. However, many patients are not satisfied with this due to the need for constant use of antibiotics, the presence of side effects and other inconveniences associated with this regimen of taking drugs. If a clear connection between the symptoms of cystitis and sexual activity is identified and there is no effect from drug treatment, surgical correction of the anatomical location of the external opening of the urethra should be used. This operation is called “transposition of the distal urethra” and consists of isolating the final part of the urethra and moving it above the entrance to the vagina (Fig. 1–3). This allows you to remove the external opening of the urethra from the danger zone and, therefore, create conditions for subsequent anti-inflammatory therapy. We have received a patent for this method of surgical treatment, and over the past 15 years this technique has been successfully used in urological practice. It should be especially emphasized that surgical correction should be resorted to only when a clear connection between the symptoms of inflammation of the lower urinary tract and sexual activity is identified and there is no effect from conservative treatment. Currently, this operation has taken a strong place among the surgical techniques used in urogynecology. Like most operations, urethral transposition has a number of features, knowledge of which largely helps to avoid possible complications and achieve a positive result. Only methodologically correct and regular, and not occasional, implementation of this operation guarantees a positive result in the range of 70–75%.
Share the article on social networks
Previous article
Next article
www.rmj.ru
Urethral dystopia in women and its treatment
One of the most common diseases affecting the fair sex is cystitis, an inflammatory lesion of the mucous membrane of the bladder. It is associated both with the negative influence of external factors, for example, prolonged exposure to low temperatures, and is caused by internal problems. A common cause of a chronic recurrent process is urethral dystopia in women. This is a disorder that is an incorrect location of the urethral outlet on the anterior wall of the vagina.
This pathology is an anomaly of intrauterine development. The exact reasons for its occurrence are currently unclear. Women whose urethra opens into the vagina constantly suffer from cystitis after coitus, as the urinary tract becomes infected. In addition, the inflammatory process also affects the reproductive system. Conservative methods in the treatment of urethral dystopia in women do not give the desired result, since they do not eliminate the main cause of the symptoms of the lesion. The most effective are radical surgical techniques that allow you to restore the natural location of the external opening of the urethra.
Causes of pathology
This problem relates to congenital anomalies and is formed in utero. To date, the factors causing the occurrence of this disease are unknown. In many cases, dystopia of the external urethral opening remains undiagnosed until adulthood or before the onset of active sexual life, since it is intimate intimacy that most often provokes the appearance of the clinical picture. There is an assumption about the genetic component of the disease, but there is no evidence for this hypothesis yet.
Main features
In many cases, only one symptom of abnormal urethral location is detected - cystitis. Inflammatory damage to the mucous membrane of the bladder is often initiated by sexual intercourse. During sex, the incorrectly located end of the urethra is mechanically injured, which leads to the development of an ascending infection. The most characteristic clinical signs of this lesion are:
- Frequent urination, which causes significant discomfort to the woman. In this case, the bubble does not fill properly. The urge to go to the toilet occurs due to irritation of the mucous membrane.
- Painful urination is a key symptom with which representatives of the fair sex consult a doctor.
- In some cases, general weakness and a rise in body temperature are noted.
Along with cystitis, urethritis often occurs, as well as inflammatory lesions of the vulva and vagina. Urine is an excellent nutrient substrate for bacteria that normally inhabit a woman's genitals. Taken together, these symptoms significantly reduce the patient’s quality of life.
Diagnostics
Determining the presence of urethral dystopia using modern visual methods is not difficult. The process of confirming the disease begins with collecting an anamnesis, which contains complaints characteristic of the disease. To make a diagnosis, they also resort to a special O'Donnell-Hirschhorn palpation technique. It allows you to determine the exact location of the external urethral opening.
To exclude other concomitant ailments, blood tests and bacteriological tests are used. X-rays with contrast are also indicative. It is carried out using special agents introduced into the bladder through the urethra. With its help, unique photos are obtained, which also help in determining localization. In some cases, an endoscopic examination of the vagina is required, and a computed tomography scan is also performed.
Treatment
Conservative methods of combating urethral dystopia in women do not give lasting results. Even while taking anti-inflammatory and antibacterial drugs, cystitis and vulvovaginitis recur, especially if the patient has an active sex life. The most effective treatment is surgery. It allows you to completely get rid of the problem and prevent the constant occurrence of post-coital inflammation of the bladder mucosa. There are a number of contraindications to the procedure, but it is actively used to combat dystopia.
Preparation and performance of the operation
Before surgery, preliminary antibiotic therapy will be required. It allows you to reduce the possible risk of complications associated with infection of the urogenital tract. An important condition for a successful operation is the use of anti-inflammatory drugs. They help combat swelling of the external opening of the urethra and vagina, which greatly facilitates the surgeon’s work.
Preparation also depends on the presence of other concomitant diseases in the patient. Since various anesthesia protocols are used to carry out the manipulation, from local to general, it will be necessary to undergo a number of examinations, as well as correct the violations identified during the diagnosis.
Surgical treatment of dystopia is reduced to raising the external opening of the urethra. To do this, the patient is placed on her back. The bladder is pre-catheterized, which greatly facilitates the surgeon’s further work. The operation is called transposition of the distal urethra. A small incision is made 1 cm above the existing urethra, after which it is transferred to a physiological position. The remaining wound is closed with stitches. If there are urethrogeminal adhesions, they are dissected during the operation, since they cause significant discomfort to the woman during intimacy and contribute to the development of vaginitis.
Indications and contraindications for surgery
The operation is performed in the presence of dystopia, accompanied by recurrent postcoital inflammation of the mucous membrane of the bladder. This type of treatment is the most effective.
Like any other surgical intervention, manipulation has contraindications. They are associated with exacerbation of chronic processes in the body and the presence of significant infection of the genitourinary tract. In such cases, preoperative examination is required, as well as antibacterial and anti-inflammatory therapy. Transposition of the distal urethra is not recommended for nulliparous women. This is due to the characteristics of the reproductive system and its proximity to the urethra. As a result of surgical treatment, the elasticity of adjacent tissues decreases. Such changes increase the risk of developing pathology during childbirth, as the mobility of the urethra decreases and the likelihood of injury increases.
There are even newer methods of treating dystopia of the external opening of the urethra. They allow not only to give the structure a physiological position, but also to cope with associated defects. For example, with hypermobility of the urethra, which causes injury, and in some cases even partial obstruction, the structure is sutured to the pubic bone. For this purpose, a special technique of applying a ligature is used. This procedure is not used very often, although it has obvious advantages.
When serious contraindications to full-fledged surgery are identified, injections of a biodegradable gel are practiced. The use of preparations based on hyaluronic acid is widespread. The substance is used in cosmetology and minimally invasive surgery because it is well tolerated by patients. By introducing the gel into certain points, a kind of plastic surgery of the urethral outlet is performed, due to which it rises. This manipulation is carried out under local anesthesia, and the drugs used for the procedure also include an anesthetic component. The disadvantages of the technique include a temporary effect, and its duration varies due to the individual characteristics of the patient’s body. In some cases, hyaluronic acid injections are used as a “trial” treatment.
Reviews
Margarita, 26 years old, Astrakhan
She suffered from constant chronic cystitis, which worsened every time after sex, which made sexual life significantly more difficult. I went to see a doctor who diagnosed urethral dystopia. The decision was made to carry out the operation. After a comprehensive examination, surgery was performed and the symptoms disappeared.
Anastasia, 22 years old, St. Petersburg
Since the beginning of sexual activity, cases of cystitis have become more frequent. It was difficult to go to the toilet, and there was nothing to say about intimacy. I decided to see a doctor. I was diagnosed with urethral dystopia. The doctor prescribed antibiotics, anti-inflammatory drugs, and hyaluronic acid injections. Transposition surgery was recommended to be performed after the birth of the child.
prosindrom.ru
Diagnostics
In order to diagnose the disease, the doctor collects anamnesis, finding out how long ago the problems began and what exactly preceded it. The patient may be asked to keep a diary in which he will have to record the frequency of urination, the volume of urine, urge intolerance, and possible urine leaks. You will also need to record the amount of fluid you drink.
Additionally, examinations are carried out:
- General blood and urine analysis.
- Bacteriological study of prostate secretion and urine.
- Comprehensive ultrasound examination of the genitourinary organs.
- Uroflowmetry (determining the amount of urine excreted, the duration of the act and the rate of urine flow).
- Urethrography (x-ray examination of the urethra with contrast).
- Tomography of the pelvic organs (if necessary).
- Endoscopy (examination of the affected area using an endoscope).
Urethral hypermobility and postcoital cystitis in women
One of the types of inflammation of the bladder is postcoital cystitis (that is, cystitis that occurs after sexual intercourse). In these cases, bladder inflammation that occurs after sexual intercourse is facilitated by abnormal anatomical features of the woman's urethra, such as a low position or hypermobility of the urethra (excessive mobility of the distal urethra). The consequence of this is that during sexual intercourse the urethra moves into the vagina, and due to friction (the process of the penis entering the vagina), flora unusual for the urinary system penetrates through the urethra into the bladder, causing inflammation.
The clinical picture of such inflammation is practically no different from the usual manifestations of cystitis. Unlike cystitis, the trigger for which is hypothermia, postcoital cystitis appears after each sexual intercourse. This forces a woman to limit or avoid sexual relations. A false idea about the true causes of the disease may suggest that the husband has other sexual partners. There may be discord and breakdown in the relationship between spouses.
Treatment for this abnormal location of the urethra is mainly surgical. Urethral transposition is an operation in which the external opening of the urethra is moved upward by 1.5-2 cm from its original position. The operation is performed in a hospital setting, where the stay takes no more than 1-2 days. In the postoperative period, the patient is not recommended to have sexual activity, usually for 4 weeks, during which complete healing of the postoperative wound occurs. The positive effect of this operation, performed with absolute indications and technically correct, is about 90%. Transposition of the distal urethra is an effective surgical treatment for hypermobility and vaginal ectopic urethra in women. This operation allows the patient to be relieved of postcoital cystitis.
chelnyclinic.ru
Operation methods
The operation begins with the patient being put under anesthesia. Since this is not an ordinary case, but a complex therapeutic manipulation, the duration of the intervention varies from 2 to 5 hours and requires a lot of experience on the part of the doctor. Usually 2 teams of surgeons take part in the operation at once.
There are at least two main ways of performing surgical treatment:
- Anastomotic urethroplasty. Involves excision and removal of the affected area of the urethra. The remaining ends of the urethra are sutured. This technique is considered outdated because it is “famous” for complications: possible shortening of the penis, its curvature.
- Buccal urethroplasty. The most modern technique involving transplantation of tissue from the cheek, tongue, lips or scrotum instead of stenotic urethral epithelium.
This operation involves several steps:
- Excision of cheek tissue to harvest a mucosal flap. This stage, along with the fifth step, requires pinpoint precision from the surgeon.
- Cheek suturing.
- Dissection of the perineum (incision length varies from 2 to 7 cm).
- Removal of stenotic tissue of the urethra.
- Sewing in a mucous flap from the cheek.
There are other modifications of urethroplasty, but the buccal technique is considered the “gold standard” of urology.
Dystopia of the external urethral meatus
Postcoital cystitis is a recurrent ascending inflammatory process (cystitis, urethritis) in the lower urinary tract in women that occurs after sex.
The cause of postcoital cystitis is the pulling of the external opening of the urethra (urethra) to the entrance to the vagina (urethral hypermobility) due to urethro-hymenal adhesions or its screwing into the vagina (vaginal dystopia of the urethra). In both cases, during sexual intercourse, a huge amount of microflora is thrown from the vestibule of the vagina and genital tract into the urethra and higher into the bladder, causing acute inflammation.
The problem arises some time (usually 1-3 years) after the onset of sexual activity due to the formation of urethro-hymenal adhesions, that is, fusion of the remnants of the hymen with the external opening of the urethra. In some cases, postcoital cystitis occurs after childbirth, accompanied by ruptures followed by the formation of adhesions.
The manifestations of postcoital cystitis are no different from banal acute cystitis, with the only difference being that they occur several hours (usually about a day) after each sexual intercourse.
The problem of postcoital cystitis is, in essence, the problem of the impossibility of normal sexual life. Indeed, no sexual intercourse means no problem of postcoital cystitis! However, looking at the young and sexually active women who come to me with this problem, you understand the tragedy and insidiousness of this disease! There are simple and ineffective “folk” remedies for preventing postcoital cystitis, for example, urinating before and after sexual intercourse (obviously, drinking a lot of water beforehand). There are also more complex, but equally ridiculous methods, such as taking prophylactic antibiotics with every sexual intercourse (and at the same time, not a drop of alcohol and chronic dysbiosis).
Urologists dealing with the problem of treating postcoital cystitis have long come to the conclusion that the only effective and reliable method is surgical - urethral transposition. A simple and atraumatic, but requiring delicate technique, the operation consists of moving the external opening of the urethra further from the entrance to the vagina, closer to the clitoris. Thus, the problem of postcoital cystitis is solved once and for all. My experience in the surgical treatment of postcoital cystitis - urethral transposition - allows me to guarantee that the result will meet your expectations!
dr-rotov.ru
Preparation
First of all, if a narrowing of the urethra is suspected, a number of diagnostic and mandatory procedures are prescribed, which include:
- Ultrasound examination of the urethra, which allows you to diagnose the location and cause of the stricture.
- Ultrasound examination of the bladder, which is performed after it has been emptied. As a result of this, the amount of residual urine in the bladder can be determined.
- Conducting an MRI or CT scan using a contrast agent. Using these procedures, you can diagnose the location of the stricture and its size.
- Urethroscopy will allow you to see the condition of the inner walls of the urethra.
- OAM will assess the overall functioning of the entire urinary system.
- Bacteriological culture of urine will show the presence of an inflammatory process.
see also
- Signs of lupus erythematosus in women
- Prevention of urolithiasis in women
- Latex wipes for women
- How to treat high blood cholesterol in women
- Why do women's knees burn?
- What a woman's small lips should look like
- Drugs for planning pregnancy for women
- The best gift for a woman
- What is good for the thyroid gland in women?
- Why do feet get cold when warm and what should women do?
- Temperature 37 without symptoms in a woman before menstruation
Complications
Impaired urine outflow leads to the ring-shaped muscle at the outlet of the bladder becoming overstrained and subsequently atrophying. As a result, its contractility decreases. The bladder stops emptying completely, and residual urine accumulates in its lumen. If its volume is more than 100 ml, this is a serious pathology and can lead to diseases such as:
- Pyelonephritis.
- Cystitis.
- Orchitis.
- Prostatitis.
- Urolithiasis disease.
- Kidney failure.
- Diverticulitis.
- Hydronephrosis.