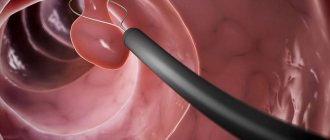
Bladder and urethral instillation is a procedure for introducing liquid medications into the bladder and urethra. The method is used to treat diseases of the bladder, urethra, prostate, and inflammation of the seminal tubercle. Instillation is carried out with antibacterial drugs, antibiotic solutions, ozonated solutions. The purpose of instillation is to restore the damaged mucous membrane of the bladder and destroy malignant cells.
Currently, work is underway on the website to change the price list; for current information, please call: 640-55-25 or leave a request, and an operator will contact you.
Prices for servicesServices
The information and prices presented on the website are for reference only and do not constitute a public offer.
What is the urinary system and how does it work?
The urinary tract is a continuous system of hollow organs whose main function is the production, collection, transportation, storage and excretion of urine.
The urinary system is divided into upper and lower sections. The upper urinary system consists of the kidneys and a tube called the ureter, which transports urine from the kidney to the bladder.
The lower urinary system consists of the bladder and another tube called the urethra, which ends the urinary system and transports urine from the bladder to the outside.
The function of the urinary system is to ensure the removal of metabolic products from the human body, regulate water-salt balance, and also store and transport urine.
The urinary system works in conjunction with the lungs, skin and intestines to maintain the balance of chemicals and water in the body. Adults excrete from 800 to 2000 milliliters of urine per day with normal drinking water consumption per day, which is 1.5-2 liters. Several factors influence the increase in urine production in the body. For example, certain types of medications, such as diuretics (water medications), are sometimes used to treat high blood pressure. Drinks such as coffee and alcohol can also cause an increase in the amount of urine produced in some people.
Treatment approach
Until recently, it was not possible to provide people suffering from urethral stricture with anything other than surgical intervention, which consists of performing anastomotic urethroplasty. For the first time such an operation was performed in 1912 by the famous Russian surgeon B.N. Kholtsov. During the operation, an incision is made in the skin and soft tissues in the affected area, after which the narrowed area of the urethra is removed, and its healthy parts are stitched together. Consequently, it can be stated that the longer the stricture, the larger the urethral element has to be removed, and therefore the length of the urethra must be reduced, which for men faces a very unpleasant consequence - deformation of the penis. Nowadays such surgery is used less and less often.
Currently, medical technologies have stepped far forward, so each individual case of the disease is characterized by a special approach, depending on the location, extent and length of the affected area, as well as contraindications. For simple types of strictures of short length,
bougienage of the urethra is used, during which bougies (dilators) are used that differ from each other in shape and diameter. The disadvantage of this method is the relatively high rate of recurrence of urethral strictures.
To avoid secondary formation of urethral stricture, a urethral stent is installed, which helps maintain the necessary lumen of a certain area of the urethra. Unfortunately, such implants often become dislodged, which limits their use. For short urethral strictures (when the length of the lesion is less than 0.5 centimeters), cutting the stenotic area is sometimes performed (the so-called internal urethrotomy under visual endoscopic control of the surgeon). Modern treatment, namely a laser urethral correction procedure (known as anastomosis without cutting the corpus spongiosum) is gaining increasing popularity.
For urethral stricture with a length of 1-2 centimeters, it is recommended to perform resection of the urethra followed by urethroplasty strictly along the boundaries of the incision. When the length of the damaged area of the urethra exceeds 2 centimeters, urethroplasty is necessary, followed by transplantation of the patient’s own integument (foreskin or buccal mucosa).
Upper urinary system
Kidneys
The kidneys are a paired organ, they are located on both sides of the spine in the retroperitoneal space just above the lumbar region and have the appearance of a large bean and are approximately the size of a fist. The right kidney is located slightly lower than the left due to the position of the liver. In an adult, the average kidney is 10 cm long, 6 cm wide and 3 cm thick, and weighs about 120-200 g. The left one is usually slightly larger than the right kidney.
Each kidney is covered by a fibrous capsule that protects the kidney from injury. All pain sensations are associated with this capsule: the organ itself has no pain receptors. When the capsule is damaged or stretched, pain of varying nature and intensity appears.
Kidney tissue or parenchyma consists of outer (cortical) and inner (medullary) layers.
Blood enters the kidney through the renal artery (a branch of the aorta) and is filtered through the microscopic structural working units of the kidney, the nephrons. Each kidney contains about a million nephrons. Their job is to filter blood and produce urine. Each nephron consists of a ball formed by small blood capillaries (the glomerulus), surrounded by a dome-shaped structure, the glomerular capsule (or Bowman's capsule), and a small tube called the renal tubule. Here, the blood plasma is filtered, which leads to the formation of urine.
The urine storage system consists of small renal calyces, which, merging with each other in 2-3 groups, form a large renal calyx, and these in turn form the renal pelvis. The renal pelvis passes directly into the ureter.
All functions normally performed by two kidneys can be adequately performed by one healthy kidney. Some people are born with only one kidney, while others choose to donate one kidney for transplantation into a person with kidney failure.
Basic kidney function
is to maintain the correct balance of water and minerals (including electrolytes) in the body.
An important function of the kidneys is to regulate fluid balance by excreting excess water in the form of urine while maintaining the required amount of water in the body, which is necessary for life. When the kidneys lose their ability to remove excess water, edema appears.
The kidneys regulate the balance of minerals and substances such as sodium, potassium, calcium, phosphorus, magnesium and bicarbonate and maintain normal blood composition. Changes in sodium levels can affect a person's mental state, while changes in potassium levels can have serious adverse effects and cause problems with the heart and muscle function. Maintaining normal levels of calcium and phosphorus is essential for healthy bones and teeth.
Additional functions of the kidneys include:
- Filtration and removal from the body of food processing waste, medications and harmful substances (toxins).
- Creatinine and urea are two important byproducts of kidney function that can be easily measured in the blood. Their values in blood tests reflect kidney function. When kidney problems occur, creatinine and urea levels increase.
- Regulate Blood Pressure – The kidneys produce various hormones (renin, angiotensin, aldosterone, prostaglandins, etc.) that help regulate the amount of water and salt, the levels of which play a vital role in maintaining blood pressure. Impaired hormone production and salt and water regulation in a patient with, for example, kidney failure can lead to high blood pressure.
- Blood volume regulation
- Regulating blood pH
- Converts vitamin D into its active form, which is necessary for the absorption of calcium from food, growth of bones and teeth, and maintenance of their health. Decreased levels of active vitamin D lead to decreased bone growth rates. Slow growth may be a sign of kidney disease in children.
Erythropoietin
is a hormone produced in the kidneys and plays an important role in the production of red blood cells. With kidney failure, the production of erythropoietin decreases, which in turn leads to a decrease in hemoglobin levels (anemia). This is the reason why the hemoglobin count does not improve in patients with kidney failure despite taking iron supplements and vitamins.
Ureters
These are fibromuscular tubes that drain urine from the renal pelvis to the bladder and are about 25-30 cm long and 6-8 mm wide. They enter the bladder from behind and at an angle, ending in the lumen of the bladder in the form of holes - the mouth of the ureters. The lower ureter is compressed by the bladder wall passively during urine storage and dynamically during voiding. Essentially, it is a valve that prevents vesicoureteral reflux (i.e., stops urine from flowing back into the kidneys). The wall of the ureter is made up of three layers, including a layer of muscle that helps it contract and move urine from the kidney to the bladder. Small portions of urine enter the bladder from the ureters approximately every 10-15 seconds.
Along the length of the ureter there are three physiological narrowings: at the level of the transition of the pelvis to the ureter, the place of intersection with the common iliac vessels and in the thickness of the bladder wall. With urolithiasis, stones can get stuck in places where the ureters are narrowed, causing renal colic.
Preparation
The most important part of preparing for the procedure is identifying the nature and extent of the structure and calculating the diameter of the excretory canal.
Analyzes help determine the exact picture:
- Ultrasound;
- retrograde radiography;
- multislice computed tomography (MSCT).
In addition, it is necessary to undergo general urine and blood tests and bacterial culture tests.
A few hours before bougienage, the patient should stop drinking. This will help to avoid severe pain during the intervention.
How is blood purified and urine formed?
Healthy kidneys filter about 100 ml of blood every minute, removing waste and extra water to eventually form urine.
There are three main stages of urine formation:
- filtration
- reabsorption
- secretion
In the process of purifying the blood, the kidneys retain all the necessary substances and selectively remove excess fluid and waste from the body.
- per day, the kidneys produce 140-180 liters of primary urine; in 24 hours, all circulating blood is cleansed several times; with age, these processes slow down
- the purification process takes place in small filter units known as nephrons.
- each kidney contains about a million nephrons, and each nephron consists of glomeruli and tubules.
- glomeruli are filters with very small pores, characteristic of selective filtration. Water and small substances are easily filtered through them. But larger red blood cells, white blood cells, platelets, protein, etc. cannot pass through these pores. Therefore, such cells are usually not visible in the urine of healthy people.
- The first stage of urine formation occurs in the glomeruli, where urine is filtered in an amount of 100-125 ml per minute, thus 140-180 liters of primary urine are formed in 24 hours. It contains not only industrial waste and toxic substances, but glucose and other useful substances.
- Each kidney performs the process of reabsorption (reabsorption). Of the fluid entering the tubules, 99% of the fluid is selectively reabsorbed and only the remaining 1% of the fluid is excreted as secondary urine. Thanks to this process, all the necessary substances are reabsorbed in the tubules, while 1-2 liters of fluid containing waste and other harmful substances are excreted from the body in the form of secondary urine.
Thus, the kidneys have filtration and concentration abilities.
Can there be a change in urine volume in a person with healthy kidneys?
YES. The amount of water consumed and atmospheric temperature are the main factors that determine the volume of urine that a normal person excretes.
Depending on the amount of fluid consumed, the amount of urine excreted changes: the more fluid enters the body, the more it is excreted and the less concentrated the urine, its color becomes light, even transparent. If the amount of fluid decreases, then the amount of urine excreted becomes less, it will be more concentrated, and the color will be dark straw.
During the summer months, sweating caused by high ambient temperatures causes urine volume to decrease. During the winter months the opposite is true - low temperatures, lack of sweating and more urine.
In a person with normal water intake, if the urine volume is less than 500 ml or more than 3000 ml, this may indicate that the kidneys need more attention and additional examination.
Make an appointment
Make an appointment with a gynecologist by calling 8(812)952-99-95 or filling out the online form - the administrator will contact you to confirm your appointment
guarantees complete confidentiality
Diagnosis confirmation
Diagnosis is carried out by the method of primary examination of the patient. A visual examination and palpation is carried out, if possible. Tests and procedures prescribed:
- Ultrasound;
- MRI;
- blood and urine tests.
If basic examination methods are not informative, urethrocystoscopy is prescribed.
If these procedures do not give an unambiguous result, urethrocytoscopy and uroflowmetry are prescribed. This makes it possible to visually examine the formation and find out its nature of origin. After collecting all the necessary data, treatment measures are prescribed, which depend on the factors and characteristics of the disease.
Lower urinary system
Bladder
The bladder is a hollow muscular organ that serves as a reservoir for urine, located just behind the pubic bone. In men, the seminal vesicles, vas deferens, ureters and rectum are adjacent to the bladder at the back. In women, the uterus and proximal vagina are located between the bladder and rectum.
The volume of the bladder can vary significantly depending on how full it is. The physiological capacity of the bladder is on average 250–350 ml, the anatomical capacity is up to 1000 ml.
The wall of the bladder is represented by: mucosa, submucosa, muscular and outer adventitia. The serous membrane lines only the bottom of the bladder.
The mucous membrane of the bladder has the ability to remain intact in the presence of urine, a rather aggressive liquid, in the bladder.
The bladder consists of an apex, body, bottom and lower narrow part - the neck. At the bottom of the bladder is a triangular area known as the vesical triangle or Lieto's triangle. Urine enters the bladder from the ureters at the very top of the triangle and leaves the bladder through the urethra at the very bottom.
The bladder neck is a funnel-shaped extension at the bottom of the bladder, which then connects to the urethra. It is 2-3 cm long and forms a muscular band around the urethra known as the internal sphincter. The sphincter is usually tightly closed and prevents urine from leaking from the bladder. When a person decides to release urine, the sphincter relaxes and urine flows from the bladder into the urethra.
Male urethra
In men, the urethra is a tube 15–22 cm long, starting from the neck of the bladder and ending with the external opening on the head of the penis (meatus). The urethra in men has the function of transporting urine and releasing ejaculate, which enters through the vas deferens.
The male urinary canal consists of several sections:
- The prostatic part passes through the prostate gland, its length is 3–4 cm, in this part of the urethra the seminal tubercle is located, the vas deferens and the prostate ducts open.
- The membranous (membranous) part of the urethra is a section from the apex of the prostate gland to the bulb of the penis, its length is 1.5–2 cm. The membranous part of the urethra is surrounded by striated muscle bundles of the sphincter.
- The spongy or penile part of the urethra passes inside the spongy body of the penis, opens at the head with an external opening, its length is about 15 cm.
The mechanism of urinary continence involves two sphincters: internal (1) and external (2). The internal sphincter is located on the border between the neck of the bladder and the beginning of the prostatic urethra, the external sphincter is located in front of the seminal tubercle.
Female urethra
The female urethra is much shorter than the male urethra and is only 4 cm in length. Urine leaves the body through the opening in the urethra, which is located above the opening of the vagina.
Danger of disease
Cystic formation in the urethra is an unpleasant disease, and the success of its treatment depends on the stage of development. If the tumor has reached a large size and has a secondary infection, even after surgery, unpleasant symptoms may remain:
- recurrent infectious diseases;
- opening of bleeding;
- neuralgic pain in the area of education;
- urethral stricture;
- hematoma formation.
Forecast
All types of internal urethrotomy show long-term results (up to 2 years) with short (up to 5–10 mm) primary strictures in the bulbous urethra without pronounced scar growths in the spongy tissue adjacent to the area of narrowing.
If the narrowed area is longer than 20 mm, then, according to statistics, repeated strictures in the first year after urethrotomy occur in 30–40 patients out of a hundred operated on; in the second year, relapses occur in almost 85% of patients.
Experts categorically do not recommend repeating urethrotomy, since with almost 100% probability a new relapse and the formation of a more extensive and dense stricture will occur after the operation. In this case, the best option is qualified open reconstructive surgery on the urethra.