Nephrosis or nephrotic syndrome is kidney dystrophy, characterized by chronic degenerative lesions of the renal tubules with simultaneous disruption of water-salt, protein and fat metabolism in the body. The disease is rare. It is based on allergic and autoimmune processes caused by a variety of reasons. The group of nephrosis includes simple and necrotic nephrosis (necronephrosis). Simple ones are lipoid and amyloid-lipoid, and necronephrosis can develop due to toxic and infectious kidney damage, with nephropathy in pregnant women and as a result of blood transfusion.
Nephrosis itself is rarely the primary disease. Most often it develops as a complication of certain chronic diseases: tuberculosis, syphilis, long-term suppurative processes in the lungs, bones and other organs. These diseases lead to severe metabolic disorders and determine the course of nephrosis itself. The main manifestations of nephrosis are swelling, the release of large amounts of protein in the urine and an increase in the amount of lipoids, primarily cholesterol in the blood. Often the swelling reaches enormous proportions and is usually pronounced in the lower part of the body: in the lower back, abdomen, external genitalia and legs. Often, edematous fluid accumulates not only in the subcutaneous tissue, but also in the abdominal cavity and in the pleural cavity. Swelling of the larynx, which makes breathing difficult, or swelling of the intestinal walls, which causes very persistent diarrhea, may occur.
A significant difference between nephrosis and nephritis is the preservation of the function of the kidneys to excrete waste from the body. Therefore, patients with nephrosis very rarely have renal failure or uremia. Their blood pressure also does not increase, as a result of which they are not at risk of heart failure.
Nephrosis is a long-term disease, often completely curable. In this case, the swelling subsides, the general condition improves and the ability to work is restored. However, it must be remembered that patients with nephrosis have reduced resistance to infections, and in severe and protracted cases of the disease, the kidneys may shrink, which can result in uremia.
What it is?
Nephrosis is a secondary lesion of the renal tubules. Nephrosis can be characterized as follows:
- basic renal functions are not impaired;
- Only disturbances in the functioning of the glomeruli may be observed;
- normal blood pressure readings.
Due to this, the pathological process in the kidneys in this disease does not contribute to the development of renal failure. And there is practically no heart failure. The course of the disease is long.
Improvement in the patient's condition is usually observed with a decrease in acute symptoms. For example, eliminating swelling. After all, it is swelling that leads to various adverse consequences. They also have a negative impact on the functioning of other organs and systems.
go to top
Clinical picture
Symptoms of the disease in its chronic form (lipoid or amyloid type of nephrosis) may not manifest themselves for a long time. This is due to the fact that the remaining active and functioning nephrons, for a certain period of time, are able to compensate for the work of the organ. At the same time, there are changes in laboratory tests indicating the presence of a pathological process.
If we are talking about acute forms of the disease, then clinical manifestations appear suddenly and have a steady progression. Often this condition leads to the death of the patient within a few days or hours.
In order to determine which morphological type the disease belongs to (necrotizing, lipoid nephrosis, etc.), it is necessary to conduct a histological examination of the renal tissue, which is obtained by biopsy. Any of these forms of the process is characterized by symptoms associated with disruption of the excretory, filtration and other functions of the organ.
Common manifestations of nephrosis are:
- Varying degrees of tissue swelling, which depends on the severity of the disease. It is customary to distinguish several degrees of spread of the process: 1st degree - swelling does not extend beyond the lower extremities; 2nd degree - the edematous component extends to the labia, lower abdomen and lower back; 3rd degree - swelling affects the patient’s neck and face; 4th degree – anasarca and congestion occur.
- The volume of urine excreted per day gradually decreases, subject to normal fluid intake.
- Weakness and unmotivated fatigue appear, and the efficiency factor decreases.
- Musculoskeletal pain is a common occurrence.
- As a rule, the liver and spleen become enlarged, which is associated with stagnant processes in the body.
- When examining urinary sediment, there are always indicators indicating a disturbance in the functioning of the kidneys (increased protein excretion, lipiduria, casts and other components). In biochemical blood tests, on the contrary, the protein concentration decreases and dysproteinemia occurs.
Distinctive signs of the acute form of nephrosis are:
- A sudden deterioration in the patient’s well-being, which begins with a rise in temperature, shaking chills and profuse cold sweats.
- The act of breathing is disrupted, attacks of suffocation and spasms appear in the bronchial tree.
- The skin changes its natural color: at first there is a sharp redness, and then there is pronounced pallor.
- Muscle-joint fights can be unbearable.
- The condition of patients approaches shock: blood pressure decreases, oliguria or complete urinary retention occurs.
Causes
The etiology of nephrosis is most often associated with various infectious diseases. The most common diseases causing nephrosis include:
- tuberculosis;
- syphilis;
- abscess;
- gangrene.
It is known that purulent processes in the body contribute to the development of negative consequences. This especially affects the cardiovascular system and the renal system. The localization of the purulent process is different.
The purulent process can be localized in bones and other organs. For example, with osteomyelitis. This is predominantly a purulent bone lesion. This is not limited localization.
The purulent process can also occur in the lungs. For example, with pneumonia. Or in the liver and stomach. In this case, localization is not important, since the process is serious and poses a danger to the entire organism as a whole.
go to top
Process options
Kidney nephrosis in its development can occur in acute or chronic form. This directly depends on the causes and factors that led to the activation of the pathological process.
The acute variant of the disease includes the following forms.
Necrotic nephrosis - has a direct connection with disturbances in the processes of blood circulation and nutrition of the tubular apparatus, as a result of which massive death of epithelial structures occurs. Its cause is the toxic effect of a number of toxic substances, drugs or poisons, transfusion of the wrong blood type, extremely severe infections leading to multiple organ failure. A state of acute renal failure occurs, in which the filtration function of the kidneys is disrupted and the volume of urine they secrete sharply decreases. Changes in the tissues of the organ are irreversible and pose a real threat to the patient’s life. The outcome is shrinkage of both kidneys.
Considering the necrotic form of the disease, it is worth mentioning a condition such as neomycin nephrosis. It is caused by the use of a medication, Neomycin, which can accumulate and have a destructive effect on the structures of the kidneys (in patients with impaired functioning of the organ). Many studies have proven the pronounced nephrotoxicity of this group of antibacterial drugs. The clinic of neomycin nephrosis develops suddenly and has typical manifestations of the acute form of the process.
Post-transfusion nephrosis is a kind of necrotic form of the disease, in which the leading element of pathogenesis is the release into the bloodstream of an excessive amount of inflammatory mediators (prostaglandins, tumor necrosis factor, histamine and others). Very often a complication such as a “shock kidney” occurs, in which the organ is almost completely disabled from functioning.
Febrile nephrosis - occurs during acute infectious processes, when the body does not have enough of its own strength to fight the disease, and, to a certain extent, kidney function suffers. The pathological condition of the kidneys may not manifest itself in any way and may be accidentally discovered during an extended examination of the urinary sediment (protein, renal epithelial cells and casts appear). As a rule, this type of nephrosis is completely relieved with proper treatment of the underlying disease.
The chronic version of the disease can occur in several morphological forms.
Lipoid nephrosis (another name for the process is glomerulonephritis with minimal changes) is characterized by severe degeneration of the proximal tubules and the deposition of lipid components in them. In this case, the glomerular apparatus remains unchanged. The changes are usually reversible and tend to spontaneous remission. Their development is facilitated by existing infectious or autoimmune diseases, in which nephrosis acts as a secondary condition.
Amyloid nephrosis is a manifestation of a severe and irreversible disease, namely renal amyloidosis. The pathogenetic basis of the process is the production and accumulation of amyloid in the body of the diseased substance. It is formed due to disturbances in protein metabolism; it cannot be detected in an absolutely healthy person. Active production of antibodies to amyloid begins, which are capable of attacking the kidney’s own tissues, namely the glomeruli, in which the pathological substrate is localized.
Lipoid amyloid nephrosis occurs many times more often than the isolated lipoid form. There are disturbances in both lipid and protein metabolism. The changes affect the tubules and glomerular structures in both kidneys.
Myoglobinuric nephrosis - occurs when myoglobin, a substance formed during the pathological breakdown of proteins of muscle origin, accumulates in the glomeruli and tubular apparatus of the kidneys. As a rule, this form of the disease occurs among people suffering from chronic alcoholism or heroin addiction. Gradually, muscle fiber cells undergo decay, and myoglobin settles in the kidney tissue.
Hydropic nephrosis is associated with processes such as tuberculosis, prolonged fasting, endocrine pathologies, malabsorption, or occurs during massive infusion therapy in a patient with intoxication. There is an increase in kidney cells due to the appearance of vacuoles in them. This condition can only be detected microscopically, since visually the organ remains unchanged.
Symptoms
Nephrosis is characterized by various symptoms. Edema is directly distinguished. Protein is released in the urine. Which indicates a violation of protein and fat metabolism.
The swelling is quite extensive. In this case, the swelling reaches enormous proportions. In what parts of the body is swelling most noticeable? The most common swellings are:
- lower body;
- small of the back;
- abdominal walls;
- external genitalia.
Swelling can also be observed in the lower extremities. The most severe signs of the disease are swelling of the mucous membrane. This may include swelling of the larynx. As well as swelling of the intestinal walls.
Swelling in the larynx makes breathing difficult. The patient may experience asphyxia. Swelling in the intestines can contribute to dyspepsia. Daily diuresis allows you to determine the decrease in the amount of urine. That is, swelling and dropsy directly occur.
A complication of nephrosis is kidney deformity. In this case, the kidney is characterized by wrinkling. In some cases, the disease can take on a necrotic form.
The necrotic form is fatal. This form of necrosis is quite rare. It is usually associated with various poisonings. Including intoxication due to exposure to poisons.
More details on the website: bolit.info
Specialist consultation required!
go to top
Etiology of acute nephrosis and nephritis
Despite the fact that the distinction between nephrosis and nephritis may be justified to a certain extent, we still consider it advisable for practical reasons to consider them simultaneously. At the same time, it is possible to more clearly note what their differences are and, on the other hand, point out the impossibility of making a strict distinction between these pathologies. Certain particularly characteristic and clinically important forms of acute renal diseases will be highlighted.
Toxic jades
In practical terms, it is primarily important that the kidneys often suffer from chemicals introduced into the body (toxic nephritis). Particular attention should be paid to this - not poisons in the proper sense of the word, but taken medicinal substances with their undesirable side effects.
Sometimes even some food and flavoring agents can be harmful to the kidneys. There is no way to list all the substances harmful to the kidneys, so we will limit ourselves to indicating only the most important in practical terms.
List of chemicals harmful to the kidney
Among the real poisons are:
- mineral acids (sulfuric, hydrochloric, nitric),
- oxalic acid
- phosphorus
- lead
- arsenic
- mercury (and above all sublimate)
- chromium (potassium chromate), etc.
List of medicinal substances that have a detrimental effect on the kidney
Of the internal medicines that can lead to kidney disease if taken carelessly or with unusual individual hypersensitivity to them, we will name:
- balsamic substances (copai balsam, turpentine)
- salicylic acid
- bertholet salt (hemoglobinuria), etc.
It is very important to know that many medicinal substances, when rubbed into the skin or applied externally, are absorbed by the skin or through small abrasions, pustules, etc. and can cause severe changes in the kidneys. These include: cantharidin patch, tar preparations, petroleum, resin, naphthol, pyrogallic acid, etc.
And it is here that we need to pay attention to the considerable danger that can threaten the kidneys during prolonged or too vigorous courses of rubbing in gray mercury ointment. Finally, salvarsan nephrosis, which develops after intravenous infusions of salvarsan.
List of nutrients harmful to the kidney
Of the food and flavoring substances that, in some cases, if consumed excessively, can damage the kidneys, we will name:
- spicy seasonings
- mustard
- radish
- alcohol, etc.
Effect of poison on the kidney
As for the very interesting question of the relationship of various poisons to individual areas of the kidney tissue, we will limit ourselves here to only brief comments. When kidneys are damaged by toxic substances, purely degenerative and necrotic changes in the epithelium (nephrosis) generally predominate.
The kidney in case of sublimate poisoning is one of the most striking examples of severe damage to the tubules with almost unchanged glomeruli. However, with many other poisonings it is not possible to make such a sharp distinction. With cantharidin nephritis and, further, with uranium and chromium poisoning, we find changes mainly in the glomeruli.
Diagnostics
In diagnosing the disease, taking an anamnesis is of great importance. Taking an anamnesis involves examining the underlying causes of the disease. Namely, the presence of infectious diseases. Let's say tuberculosis.
Hereditary predisposition is practically not the cause of the disease. But sometimes a hereditary history is required. Diagnosis of nephrosis is based on laboratory tests.
Among other things, the collection of a general blood and urine test is of great importance. Protein is often detected. Albumin is found in blood plasma. The amount of protein in the blood decreases markedly.
Indicators of protein in the blood are the following values: 3.5 – 5.5%. Edema is diagnosed by direct examination of the patient. Sometimes more detailed diagnostics are required.
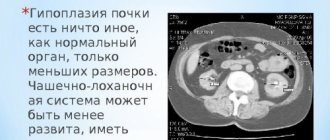
Ultrasound examination can detect various disorders. These violations also affect other organs. The radiographic method is very appropriate.
X-ray technique allows you to detect a suppurative process in the lungs. In some cases, a kidney biopsy is required. In this case, this makes it possible to determine pathological changes in the renal apparatus.
Clinical examination is important in the diagnosis of nephrosis. That is, the examination suggests the ability to diagnose the disease at an early stage of the disease. In some cases, an MRI of the kidneys is required.
go to top
Cardiovascular system in acute kidney diseases
After dropsy, first of all, the condition of acute kidney diseases of the circulatory system deserves the keenest attention. The main difference between degenerative nephrosis and true nephritis is manifested in the characteristics of pulse and blood pressure.
In general, with nephrosis, blood pressure and pulse tension remain unchanged, and with acute nephritis, often just a few days after the onset of the disease, symptoms of the participation of the circulatory organs in the process are detected: the pulse becomes increasingly tense, the second sound of the aorta intensifies, and the blood pressure is above 150 mm Hg, at the beginning of the disease the pulse is often somewhat slow, but then for the most part it increases.
The developing hypertrophy of the left ventricle can, according to my observations, be clinically proven in severe cases of acute nephritis, often after 4-6 weeks, mainly by the apical impulse of the heart, increased arterial tension, which probably depends on the nosebleeds that sometimes occur.
As a manifestation of the above-mentioned general effect of diseased kidneys on the circulatory organs, serous-fibrinous pericarditis occasionally develops in acute nephritis. They are usually considered uremic pericarditis, caused by metabolic products accumulated in the blood. In the same way, pleurisy and, in rare cases, peritonitis can occur.
Prevention
Nephrosis can be prevented using various techniques. Prevention mainly involves eliminating the underlying disease. If the underlying disease is cured, then nephrosis does not occur.
However, external factors can also have an influence. For example, toxic substances. Intoxication of the body mainly occurs. As a result, a severe form of nephrosis may develop.
It is also necessary to adhere to a certain diet to prevent nephrosis. Nutrition should be complete. It is necessary to exclude salt from the diet. And also do not abuse alcoholic beverages.
Diseases of the renal system can be affected by simple hypothermia. However, hypothermia is a consequence of decreased body reactivity. Reduced immunity is also more susceptible to infections.
Prevention will be aimed at strengthening the body's immune response. Immunity is affected by lifestyle, nutrition, and physical activity. However, if you have kidney disease, physical activity should be moderate.
Any purulent diseases must be predetermined. After all, any purulent infection is a consequence of an exacerbation of other diseases. Pus is the penetration of pathological microorganisms. But this penetration can also be prevented!
go to top
Main reasons
There are enough etiological factors for this pathology, but experts identify a group of main causes that most often act as a provocateur of nephrosis:
- Intestinal obstruction;
- Genetically determined disorders of protein metabolism;
- Extensive burn lesions and traumatic complications;
- Infectious pathologies occurring in a chronic or severe form with complications;
- Systemic disorders such as rheumatism or amyloidosis;
- Blood transfusion of the wrong type, which caused a complication;
- Acute toxic poisoning;
- Oncopathology;
- Long-term wearing of compression garments that put pressure on the kidney area.
In women, renal nephrosis can develop against the background of aseptic necrosis during the postpartum recovery period. A hereditary factor should not be excluded, because the presence of nephrosis in parents increases the risk of its occurrence in the child. In a significant number of patients, poisoning with ethylene glycol vapors was noted, which provoked nephrosis. These substances are present in antifreeze fluid used in automobile cooling systems. There have been cases when the disease developed against the background of complications of bacterial origin, characteristic of such pathologies as malaria, cholera, plague, etc.
Treatment
Nephrosis is treated with symptomatic therapy. It is necessary to eliminate the main symptoms of the disease. And also reduce swelling and restore protein and fat metabolism.
Detoxification therapy is of great importance in medical therapy. That is, the direct elimination of toxic factors. Which is poisoning with toxic substances.
When the disease is infectious, antibacterial therapy is crucial. That is, the use of antibiotics depending on the lesion. It is aimed at eliminating the immediate pathogen.
The treatment is quite long. Additionally, dietary nutrition is prescribed. Also additional treatment methods are:
- blood transfusion;
- diuretics.
Diuretics should be used to relieve swelling. In some cases, an albumin preparation is required. A salt-free diet is also used. At the same time, the flow of fluid into the body is limited.
What drugs are used in the treatment of nephrosis? It is preferable to use the following drugs:
- Novazurol;
- salirgan;
- lasix;
- Novurin.
Transfusion of blood products is appropriate in the acute course of the disease with massive edema. The diet must contain vitamins and definitely protein. Protein foods are necessary to maintain metabolism and replenish lost substances.
go to top
Post-transfusion necronephrosis
Post-transfusion necronephrosis occurs during blood transfusion if the blood groups and Rh factor of the donor and recipient were incorrectly determined. When blood incompatible with ABO group factors or Rh antigens enters a patient’s body, he or she develops immunological complications, hemolysis and hemolytic shock occur, resulting in pronounced hemodynamic changes. These phenomena are also observed with an excess of natural or immune agglutinins anti-A or anti-B.
Impaired renal hemodynamics is one of the reasons for the formation of the so-called hemolytic kidney and the development of acute renal failure. In addition, blood transfusion with incorrectly determined parameters causes damage to the tubular epithelium and blockage of them with hemoglobin casts.
In adults
Nephrosis in adults develops due to metabolic disorders. In this case, the disease is more often observed in women, less often in men. There are no age restrictions. From middle to old age.
In adults, the disease is more severe than in children. This is due to the accumulation of nitrogenous compounds. Blood pressure also increases. The concentrating ability of the kidneys also decreases.
Why is nephrosis more common in women? This is primarily due to the peculiarities of the physiological structure of the body. Including the most common hormonal pathologies.
Women are one hundred percent susceptible to these pathologies. But, if the process develops in men, then this is most often associated with the presence of a severe infectious process. For example, with pulmonary tuberculosis.
What are the main symptoms of the disease in adults? The main clinical signs of the disease include:
- swelling;
- weakness;
- decreased performance;
- decreased amount of urine;
- functional disorders of various organs.
All these symptoms are most typical for adults. It is urgent to carry out appropriate diagnostics. Treatment must be prescribed immediately!
go to top
Necrotizing nephrosis
Necrotizing nephrosis or necronephrosis of the kidneys is an acute shockogenic, infectious or toxic damage to the kidneys, accompanied by impaired blood supply, renal ischemia with subsequent necrosis of the epithelium of the renal tubules and the development of acute renal failure. A special group consists of necronephrosis caused by acute intravascular hemolysis - the destruction of red blood cells with the release of hemoglobin into the environment, resulting from the transfusion of incompatible blood.
During the illness, the so-called shock kidney develops, in which blood circulation is disrupted and water filtration in the renal tubules decreases, which leads to oliguria and anuria, and subsequently to uremia.
The causes of shock kidney can be burns, severe injuries, intestinal obstruction, septic condition after childbirth or abortion, as well as severe infectious diseases such as malaria, cholera, toxic dysentery, leptospirosis, diphtheria and others. Regardless of the cause of necronephrosis, it is characterized by the development of acute renal failure.
Symptoms and course of necrotic nephrosis
In the first two days of the disease with necrotizing nephrosis, the patient is dominated by symptoms of poisoning and shock, urination disorders quickly develop: oliguria up to 300-400 ml of urine per day and anuria, which can last up to 6 days. Mild proteinuria is also possible, and the urine sediment may contain hyaline and granular casts, a moderate number of red blood cells, an abundance of epithelial cells and single white blood cells. The relative density of urine is below normal.
As the pathological process increases, renal failure rapidly develops. The phase of azotemic uremia begins with an increase in the amount of nitrogenous wastes and minerals in the blood and the formation of acidosis. During this period, the patient experiences regular bouts of vomiting, he experiences general weakness, apathy, stupor, and develops uremic coma and hypothermia. Following this, the work of the heart is disrupted, pericarditis, pleurisy, and Kussmaul respiration may begin - pathological breathing, characterized by uniform, rare respiratory cycles, deep noisy inhalation and increased exhalation. Sometimes blood pressure rises and slight swelling appears.
The next stage of the disease is hyperkalemia (potassium retention occurs in the blood). At a norm of 16-22 mg% it reaches 30-45 mg%. When taking an electrocardiogram, its characteristic signs are also noted. This leads to severe intoxication of the nervous system, manifested in the form of paresthesia, decreased tendon reflexes, paralysis of the limbs, bradycardia, and arrhythmia.
After a period of oliguria and anuria, polyuria begins, lasting about 2 weeks. The patient’s urine at this time is light, with low relative density, and contains a small amount of protein. Its amount per day can reach up to 3 liters.
If there are no complications, then after some time the kidney functions gradually begin to recover: the amount of urine excreted returns to normal, the concentrating ability of the kidneys improves, and azotemia decreases. Then the blood composition normalizes, the ESR decreases, and all signs of necrotic nephrosis disappear. However, the recovery period can drag on for several months, and in severe cases of the disease, death from uremia is possible.
Diagnosis and treatment of necrotizing nephrosis
In children
Nephrosis in children develops due to unknown reasons. However, sometimes genetic predisposition plays a role. Therefore, a hereditary history is being collected.
In children, the disease is divided into several stages. The increase in symptoms in children is gradual. Most often, the disease can develop as a result of an infectious process.
In children, diphtheria is often a concomitant disease. In some cases, the cause of illness in children is poisoning. Due to intoxication of the body, nephrosis develops.
Symptoms in children vary. At the initial stage of the disease, swelling of the face is noted. Then the body temperature rises. Protein is found in the urine.
The second, third and fourth stages of the disease in children are characterized as follows:
- swelling and protein in the urine;
- disappearance of edema, release of protein;
- nephrotic manifestations (rare).
A secondary pathological process may join the disease. For example, pneumonia. In this case, deaths are possible.
That is why it is necessary to treat the disease at the initial stage. Otherwise the disease becomes more complicated. And in the presence of a weakened immune system, it becomes fatal!
go to top
Amyloid nephrosis
Amyloid nephrosis is one of the manifestations of a common disease: amyloid disease or amyloidosis (synonyms are renal amyloidosis and amyloid renal dystrophy). This pathology is based on a disorder of protein metabolism, leading to the formation of a special substance - amyloid, which does not occur in healthy people and is a glucoprotein. Up to 96-98% of amyloid is a protein component, in which gamma globulin predominates. Amyloidosis occurs more often in middle-aged men.
Amyloidosis is distinguished between genetic or hereditary, primary and secondary. Genetic occurs due to hereditary changes in enzyme systems involved in protein synthesis. This form of the disease is most widespread in the countries of the Mediterranean basin. In our country there are isolated cases of this disease.
The cause of primary amyloidosis has not yet been established; it is recorded very rarely. Secondary amyloidosis is more common and occurs against the background of protein metabolism disorders, often as a result of chronic infections such as tuberculosis, syphilis, malaria, prolonged inflammatory processes in the lungs, and osteomyelitis. Less common with polyarthritis deformans, lymphogranulomatosis, actinomycosis, multiple myeloma.
According to the frequency of amyloid damage, the organs and systems of the body can be arranged in the following order: spleen, kidneys, adrenal glands, liver, gastrointestinal tract, lymph nodes, pancreas, prostate gland.
Symptoms and course of amyloid nephrosis
Under the influence of infection and toxic substances, the process of protein synthesis changes - modified proteins appear. The body responds by turning on autoimmune mechanisms and begins to produce antibodies to these modified proteins. As a result, a special dense amyloid substance is formed, consisting of antigen + antibody complexes, which is deposited in various organs. In primary amyloidosis - around collagen fibers, in secondary - perireticularly. In this regard, in the first case, the tonsils, digestive tract, skin, striated muscles, heart, nerves, large vessels are more often affected, and in the second case, parenchymal organs (liver, spleen, lungs, etc., having small vessels) are more often affected.
The development of genetic amyloidosis occurs in the first 2-3 decades of the patient’s life. In the clinical picture, three syndromes are distinguished: nephropathic, occurring with kidney damage, neuropathic, characterized by predominant damage to the nervous system, and cardiopathic, manifested by changes in the activity of the heart.
Symptoms of genetic amyloidosis are fever, edema, proteinuria, anemia, joint and skin changes, myalgia (muscle pain), damage to the gastrointestinal tract. They may be preceded by urinary syndrome (however, it can develop much later).
Blood pressure in patients is usually normal and does not increase even in the stage of chronic renal failure. However, dysproteinemia is observed - a violation of the normal ratio between different fractions of blood proteins and an increase in ESR. There is also a relatively early decrease in renal blood flow and glomerular filtration rate. In many patients, due to the deposition of amyloid substance, enlargement of the liver and spleen and impaired liver function are detected.
Primary amyloidosis manifests itself in the form of localization of amyloid deposits, as well as functional disorders and vascular thrombosis that occur in the corresponding organs. Its initial stages may be similar to malignant neoplasms, liver cirrhosis, cardiovascular failure and other diseases. All this makes diagnosing the disease very difficult. Primary amyloidosis in the early stages of the disease is not characterized by amyloid deposition in the kidneys. Their defeat does not occur at the beginning of the disease, but later. Because of this, intravital diagnosis of primary renal amyloidosis is complex and requires extensive physician experience and all available diagnostic tools.
Secondary renal amyloidosis can be divided into 3 stages: initial, nephrotic and azotemic. At the initial stage, the patient does not have any complaints or signs characteristic of kidney damage. At least they are not found during physical examination of patients. The main symptoms during this period are the symptoms of the underlying disease, and changes in the kidneys do not have a significant impact on the general condition of the person.
However, urine examination reveals slight proteinuria, periodic erythrocyturia, single casts and leukocytes. Sometimes renal plasma flow and glomerular filtration decrease slightly, which can also be increased and combined with polyuria - an increased amount of urine excreted. In this case, nighttime diuresis consistently exceeds daytime diuresis. In addition, as a result of the predominance of the globulin fraction in the blood, a moderate increase in ESR is noted.
The initial stage can last a long time: from 6 months to 5 years. The timing depends on the nature of the underlying disease. Their reduction occurs during tuberculosis, and their lengthening occurs during inflammatory and suppurative processes.
At the nephrotic stage, the symptoms of the underlying disease no longer play a major role. The clinical picture is dominated by proteinuria, edema, hypoteinemia, dysproteinemia and hyperlipidemia. Albuminuria increases, and the amount of protein in the urine fluctuates significantly throughout the day. Among the proteins in the urine, globulins predominate, especially their coarse fractions. In addition, a large amount of cholesterol esters is noted in the urine sediment, which indicates the addition of secondary lipoid nephrotic syndrome to amyloidosis.
During this period, the patient experiences oliguria - a decrease in the daily amount of urine and a stable predominance of nighttime diuresis over daytime. Due to hypotension caused by damage to the adrenal glands, the filtration function of the kidneys decreases. Sometimes an increased level of cholesterol and a moderate increase in creatinine, the end product of the metabolism of proteins, urea and residual nitrogen, may be observed in the blood. Mild anemia and neutrophilic leukocytosis are also possible. ESR is always increased.
The azotemic or third period of secondary renal amyloidosis is characterized by chronic renal failure that develops as a result of glomerular shrinkage. At this stage of the disease, the patient's concentration and filtration-reabsorption functions of the kidneys decrease and the disorder of the gastrointestinal tract increases. Nausea, vomiting, diarrhea are common, polyuria and hypoisosthenuria are observed - a decrease in the specific gravity of urine.
Examinations of the patient show that residual nitrogen does not exceed 100 mg, and blood pressure is normal or slightly elevated. Cholesterol levels return to normal, anemia increases, swelling remains only in the legs and ankles. Due to the accumulation of globulins and fibrinogen in the glomeruli against the background of slowing renal blood flow, a complication may develop in the form of renal vein thrombosis. At the same time, diuresis quickly decreases, hematuria increases, and hypertension and azotemia develop acutely. At the third stage of secondary amyloidosis of the kidneys, due to azotemic uremia, purulent-septic processes, pneumonia, purulent peritonitis, renal vein thrombosis, erysipelas, lung abscess or other complications, the patient’s death may occur.
Diagnosis and treatment of amyloid nephrosis
Forecast
With nephrosis, the prognosis directly depends on the course of the disease. And also on the stage of the disease, the characteristics of treatment and the presence of reactivity of the body. If the underlying disease is cured, the prognosis is favorable.
If the disease is aggravated by an infectious lesion, then the prognosis is negative. This is especially true for tuberculosis. Diphtheria has the best prognosis.
The prognosis also depends on the characteristics of the treatment. Complex therapy must be selected. This allows not only to improve the prognosis, but also the possible outcome.
go to top
Lipoid nephrosis
Lipoid nephrosis is a rare disease. This is one of the forms of nephrotic syndrome, in which kidney damage occurs, predominantly of a dystrophic nature. Previously, lipoid nephrosis was considered an independent disease, but later it turned out that its cause is almost always some general disease (tuberculosis, osteomyelitis, syphilis, malaria, diphtheria, dysentery, chronic enterocolitis, polyarthritis, lymphogranulomatosis, lead and mercury intoxication, etc.). d.). In cases where the cause of dystrophic changes in the kidneys cannot be identified, the disease is designated as lipoid nephrosis.
It is believed that its causes are severe metabolic disorders in the body, mainly fat and protein. As a result, the processes of cellular nutrition and the permeability of the walls of the capillaries of the renal glomeruli are disrupted. Protein particles and lipoids, contained in large quantities in the primary urine of patients, penetrate the wall of the tubules, causing severe dystrophic changes in the epithelial cells. In addition, recently a great influence on the development of this kidney pathology of the autoimmune mechanism has been revealed.
Exodus
It should be remembered that the process is degenerative. However, the functional features of the kidney are not affected. Therefore, the outcome may end in recovery.
With the development of necrotic nephrosis, the outcome is definitely not favorable. In the presence of suppurative processes, the outcome is fatal. Especially with an abscess and other lesions.
If the functions of other organs are noticeably impaired, then a negative outcome can be expected. Recovery occurs at the initial stage of treatment. Especially when the process of damage to the glomeruli of the kidney has just developed.
go to top
Kidney nephrosis - what is it?
Nephrosis refers to dystrophic processes in the renal parenchyma, accompanied by degeneration of the tubules and connective tissue structures of the kidney. As a result of such a disease, nephrotic syndrome, nephropathy and impaired filtration function of the tubules, oliguria develop. Another name for nephrosis is toxic-infectious kidney, which clearly reflects the specificity of the disease associated with intoxication damage. Pathology develops in acute and chronic forms, with many common manifestations.
Dystrophic nephrotic changes lead to thinning of the tubular tissue, which causes the release of blood proteins in the urine. This factor causes a decrease in renal volume and disruption of protein metabolism, which immediately affects the entire body. Nephrosis is diagnosed more often in patients of childhood and adolescence, which experts explain by the weakness of the abdominal cavity of a growing organism, especially at 2-6 years of age.
Lifespan
In any case, your life expectancy depends on the condition of your body. The state of the body is influenced by lifestyle, nutrition, the presence of stress or lack thereof. Life expectancy is higher if medical prescriptions are followed.
However, if the form of the underlying disease is not cured, the patient’s quality of life decreases. Due to decreased performance and other unpleasant symptoms. Therefore, life expectancy is reduced.
The more seriously the patient takes the disease, the better the treatment will work on him. If the patient follows all medical instructions, then life expectancy increases. Take care of your health and be healthy!
Symptoms and signs
The clinical picture of nephrosis often has a weak degree of severity, so it is quite difficult to diagnose the pathology in the early stages. At first, patients may experience minor swelling in the legs and abdomen. In the later stages, swelling becomes pronounced, so it is difficult not to notice it.
Lipoid nephrosis is characterized by symptoms such as:
- Lack of appetite;
- Fatigue;
- Increased weakness;
- Pastosity on the limbs and face;
- Increasing swelling, spreading to the genitals and lower back;
- Hydrothorax and ascites;
- hypopolyvitaminosis;
- Tachycardic manifestations;
- Oliguria with high urine density.
Necrotic nephrosis is characterized by an acute onset; in the first 48 hours, the patient experiences pronounced symptoms of intoxication and shock with oliguria, which can last up to a week. As the pathology progresses, kidney failure develops.
The amyloid nephrotic type of lesion is accompanied by edema and fever, anemia and proteinuria, muscle pain and gastrointestinal lesions, changes in the skin surface and joint structures. The spleen and liver may become enlarged, and liver functions may be impaired.
Post-transfusion nephrosis has a rapid onset. Signs like:
- Chest, headache and lumbar pain;
- Severe, literally shaking chills;
- Bronchospasms;
- Nausea;
- Redness and then paleness of the skin with sweat;
- Severe hyperthermia;
- Breathing difficulties;
- Rapid decrease in blood pressure;
- Convulsive attack with involuntary urination or defecation.
Urine with post-transfusion nephrosis becomes red-brown. When the patient is brought out of shock, oliguria and jaundice begin to develop. They progress, and the liver and spleen become enlarged.
Nephrosis treatment prognosis, surgery
How much does a kidney cost? Only specialists can answer this question. As a rule, they are asked only to those people who develop a serious pathology that causes complete failure of the renal system. In this case, a surgical intervention is performed, during which the diseased organ is replaced with a donor one. Unfortunately, the survival rate of the transplanted kidney in this case is no more than 75%.
According to doctors, the prognosis for recovery from nephrosis is questionable. It depends on the specific clinical form of the disease. Timely initiation and proper treatment of necrotizing nephrosis usually leads to complete recovery of the patient. It should be noted that in the amyloid form of the disease, the prognosis for its therapy remains unfavorable.
In order not to be interested in how much a kidney costs, people with chronic types of nephrosis should undergo regular spa treatment. At the same time, we can talk about a person’s ability to work only during the period of remission.
According to experts, any kidney nephrosis requires immediate consultation with a doctor. Diagnosis of this disease does not present any difficulties. But this is not enough for his successful therapy.
Causes of nephrotic syndrome
- Incorrect blood transfusion (Rh factor or group mismatch);
- Severe poisoning from dangerous chemicals (concentrated acids, heavy metals, antifreeze or neosalvarsan);
- The person has a severe infectious disease or typhoid fever;
- Intoxication with biological poison (snake bite, eating poisonous mushrooms);
All these and some other reasons can ultimately provoke the development of one or another form of nephrosis in a person.
Prevention and treatment of the disease
Kidney bruises and other injuries very often cause the development of nephrosis. Therefore, you should be extremely careful during dangerous work and sports.
To prevent kidney diseases and diseases of the urinary system, experts recommend adhering to a salt-free diet and limiting fluid intake. This will significantly reduce swelling. For the same purpose, diuretics such as Lasix, Novazurol and Novurit can be used. They help remove salts and excess fluid.
In patients with lipoid disorder, positive changes are observed after the administration of immunosuppressants and corticosteroid drugs. This happens due to the restoration of the structure of the glomeruli of the kidneys. The use of such medications eliminates swelling and promotes remission.
As is known, nephrotic syndrome is accompanied by significant protein loss. In this regard, treatment of such a disease should be aimed at replenishing this loss. In acute conditions with severe edema, a similar effect is achieved through blood transfusions and diuretics. To restore protein reserves, special nutrition is prescribed. The patient's diet should contain predominantly protein products.
If a protein diet is contraindicated for a patient, then he is prescribed a high-calorie diet with the optimal amount of carbohydrates and fats. However, the amount of protein in food should be slightly greater than its loss through urine.
Thus, there are several approaches to the treatment of renal interstitial lesions. Powerful drug therapy during periods of exacerbation should reduce swelling and normalize the patient's condition. As for remission, in this case, a diet should serve as maintenance treatment, which consists of the following:
- reducing salt intake;
- reducing fluid intake;
- consuming enough protein;
- consuming enough vitamins.
It should also be noted that in the chronic form of the disease, the diet should not be followed constantly, but at certain intervals, so that other complications do not arise.
Treatment and prevention of lipoid nephrosis
A patient with lipoid nephrosis is prescribed a protein diet (at the rate of 2-2.5 g of protein per 1 kg of his body weight, excluding edema) and vitamins. The amount of table salt is reduced to 1.5-2.5 g per day, and the amount of liquid consumed is moderately limited. Antibiotics are also used to actively treat foci of infection.
To combat edema, the patient is prescribed bed rest and diuretics : Lasix, hypothiazide, Novurit and others. Recently, corticosteroid drugs and immunosuppressants . Taking corticosteroids usually leads to long-term remission, subsidence of edema, normalization of the structure of the walls of the glomerular capillaries with a decrease in their permeability and a decrease in protein excretion by the kidneys. The administration of polyglucin is recommended as a means of increasing plasma colloid osmotic pressure. After swelling disappears, steroid hormones can be used to improve protein synthesis. During all periods of the disease, it is necessary to use replacement therapy : vitamins and enzymes.
As for the prevention of the disease, as already noted, lipoid nephrosis develops very rarely as an independent disease. Therefore, all its prevention comes down to prevention and timely disposal of the diseases that cause it, as well as treatment of focal or chronic infection. In addition, during the period of relative remission, sanatorium-resort treatment in places with a dry climate, like Bayram-Ali in Central Asia, is recommended.
Causes and types
There are several factors that provoke the development of kidney nephrosis.
10 main reasons:
- intestinal obstruction;
- injuries;
- burns;
- infectious process;
- heavy metal poisoning;
- chemical intoxication, for example, due to antifreeze poisoning;
- violation of blood transfusion rules;
- trauma accompanied by tissue compression;
- development of aseptic necrosis after labor;
- genetic factor.
General signs of the disease
The Institute of Urology, which has been treating the disease in question for many years, has identified common symptoms that are characteristic of all types of nephrosis.
According to experts, any type of kidney damage is accompanied by dystrophic disorders in its tubules. At the same time, their permeability to proteins increases significantly, which causes serious metabolic disruptions in the body. The protein content in the blood in this condition drops to 3.2%. Normally, they provide plasma pressure (oncotic) and prevent liquid substances from entering the intercellular space from the vessels. In the absence of such a process, the patient develops persistent swelling. Also, as the disease progresses, there is a decrease in the volume of urine, which becomes dark in color. This symptom is important for timely detection of the disorder.