Features of the anomaly
As a rule, the disease is classified as a congenital anomaly, although acquired forms are often observed.
Megaureter is often found in pediatric urology; the disease is mainly detected in newborns and children aged 6-10 years.
The disease also affects adults; in women, neuromuscular dysplasia occurs 4 times more often than in the stronger sex.
Experts say that bilateral dysplasia is observed much more often. With unilateral pathology, in most cases the disease is located on the right.
Often the disease develops along with other pathologies, such as dysplasia of the renal parenchyma, posterior urethral valve, etc.
Stage of development
Taking into account the course of the disease, three main stages are noted:
- The first stage is the initial stage of the development of the disease, as a rule, it is called hidden. This stage is almost always asymptomatic, the patient does not feel any disturbances or pain, pathology can only be detected during examination. There is a slight expansion in the lower parts of the ureter.
- Second stage . The first symptoms appear, a feeling of weakness, pain in the lower abdomen and lower back, and fatigue. Enlargement develops in all parts of the ureters.
- Third stage . The most severe form of the disease, muscle tone is completely lost, an increase in urea is observed in the blood, the ureters become greatly enlarged, and their length increases. The patient's condition worsens significantly, the disease actively progresses.
Causes and pathogenesis
There are congenital and secondary ureteroceles, that is, the origins of the development of the disease can be diametrically different.
Statistically, the majority of diagnosed ureteroceles are caused by congenital characteristics of the body. With a deficiency of muscle fibers, the ureter, that is, the hollow tube through which fluid filtered from the blood with waste products leaves the body, is formed narrower than it is necessary to remove urine from the body. Urine puts pressure on the walls of the ureters, deforming them, causing inflammation, metabolic disorders and ureterocele.
There are 3 stages of the disease:
- at stage I, changes in the organs responsible for the removal of fluid and decay products are insignificant;
- at stage II, the cystic formation prevents urine from entering the bladder, so urine goes back to the kidney, this process is called hydronephrosis;
- at stage III, hydronephrosis is accompanied by tissue disorders and, accordingly, bladder activity.
Secondary ureterocele is fixed against the background of the existing pathology – ICD: urolithiasis.
A stone or calculus coming out of the kidneys can block the duct, after which the pathogenesis develops according to the same scenario as with a primary ureterocele.
Considering the development mechanism, we can highlight the structure:
- the emergence of education;
- disruption of urine outflow;
- protrusion of ureterocele into the body of the bladder;
- the appearance of inflammation, including purulent ones.
Due to the inflammation included in the symptomatic picture of ureterocele, the pathology is accompanied by cystitis and pyelonephritis. If the disease is not treated, kidney failure is highly likely to develop.
Reasons for the occurrence of the violation
The causes of the disease are still not fully understood; scientists claim that the disease is congenital.
This is facilitated by many infectious pathologies of the expectant mother, alcohol consumption and smoking on the part of both parents, as well as poor nutrition and poor environment, which together cause megaureter in the fetus.
As for the acquired form, the main factors are:
- tumors of the bladder and kidneys;
- urolithiasis disease;
- inflammatory kidney diseases;
- ureteral injuries;
- serious stressful situations.
Diagnostics
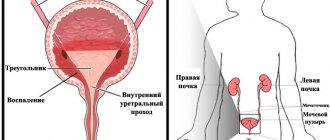
First of all, you need to undergo a gynecological examination. The specialist must take a smear for subsequent cytological examination. After this, an ultrasound examination of the pelvic organs and cystoscopy with collection of biological material for histology are performed.
As an additional diagnosis, it is important to identify or exclude other infectious pathologies and undergo an immunogram. If there is inflammation, a general blood test will show a high level of SOE and leukocytosis.
In the biochemical study of blood, special attention should be paid to renal, liver tests, and the amount of glucose. With leukoplakia, a general urine test will show changes in color, transparency, protein, epithelial cells, and leukocytes. It is important to conduct a culture to identify the pathogen and check the sensitivity of the pathogenic microorganism to antibiotics.
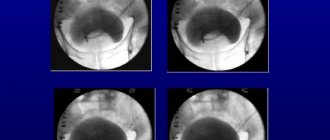
The main method for diagnosing bladder dysplasia is cystoscopy with collection of material for histological examination. Unlike cystitis, with this disease the replacement of the transition layer with squamous epithelium is detected.
Symptoms of the disease
The clinical picture largely depends on the stage of the disease.
At the beginning of the development of dysplasia, the symptoms of the disease do not appear in any way, the patient feels quite normal, and the pathology is mainly detected during examination. With the development of neuromuscular dysplasia of the ureter, the following symptoms emerge:
- general fatigue;
- frequent headaches;
- pale skin;
- swelling under the eyes;
- bad breath;
- pain in the lower abdomen and lower back.
In the case of a severe form, when a ureteral rupture is possible, patients complain of severe pain occurring in the lumbar back. In this case, the patient requires immediate medical assistance.
Types of bladder cancer
Bladder cancer is divided into well-differentiated bladder cancer and poorly differentiated bladder cancer. This division helps determine the rate of growth and spread of a malignant bladder tumor. Even when the stage and extent of bladder cancer have been determined, it is necessary to know the depth of the lesion, since this will determine the choice of treatment methods or combination of methods that will give the best result for the patient.
Superficial bladder cancer
Superficial bladder cancer is bladder cancer that does not grow into the muscle layer.
The most common type of bladder cancer is superficial bladder cancer, which responds well to treatment. In this case, the tumor is located on the surface of the mucous membrane of the bladder and does not grow into the submucosal plate.
Superficial bladder cancer.
When treating superficial bladder cancer, organ-preserving but radical surgery is possible. If bladder cancer is small, the tumor is superficial and highly differentiated, then conservative treatment is possible.
Invasive bladder cancer
Invasive bladder cancer is bladder cancer that grows into the muscle layer.
Invasive bladder cancer is a tumor that grows into the wall of the bladder, and when the tumor grows through the submucosal layer to the muscle layer. In this case, as a rule, radical surgery is required.
Invasive bladder cancer.
Bladder cancer can spread beyond the bladder to nearby lymph nodes and possibly to other organs such as the liver, lungs, or bones.
The best treatment in this situation is removal of the bladder, sometimes in combination with radiation and chemotherapy. In very rare cases, when there is no previous history of bladder cancer and the tumor is in an isolated area, it may be possible to remove only the affected segment of the bladder.
However, most often a radical operation to remove the bladder is necessary.
There are three main types of bladder tumor:
- transitional cell carcinoma of the bladder, which begins in the cells lining the bladder
- squamous cell carcinoma of the bladder, which arises from the flat cells of the epithelium of the bladder,
- adenocarcinoma of the bladder, which begins in the glandular cells of the bladder.
Transitional cell carcinoma of the bladder is the most common bladder tumor.
Bladder dysplasia
Bladder dysplasia is a precancerous condition in which the cells become cancer-like, but they have not yet acquired the ability to grow into tissue or spread to organs distant from the primary lesion. At this stage, a complete cure for bladder dysplasia is possible.
Bladder metaplasia
Metaplasia of the bladder is the transition of one type of tissue to another within the same germ layer. Most often found in epithelium.
In smokers, the transitional epithelium of the bladder mucosa may be replaced by cells that are normally found in the oral cavity (squamous epithelium), a phenomenon called squamous metaplasia.
In patients with recurrent infections, chronic catheterization, or chronic bladder irritation, the normal urothelium (bladder lining) may change to cells characteristic of the intestinal lining (intestinal metaplasia).
Carcinoma in situ (CIS)
Carcinoma in situ (CIS) is an aggressive form of bladder cancer, but it has not yet invaded the bladder wall or metastasized. This type of bladder cancer is most often treated with intravesical immunotherapy or photodynamic therapy of the bladder. Intravesical immunotherapy involves injecting drugs into the bladder. This stimulates the immune system to fight cancer cells.
The most effective and frequently used drug in this treatment method is BCG. BCG is a vaccine containing weakened forms of Mycobacterium tuberculosis. Most patients undergo treatment for 6 weeks, which is followed by cystoscopy and urine cytology to ensure that bladder cancer does not recur.
Patients who have had bladder cancer removed undergo preventive courses of immunotherapy for three weeks every six months for three years.
If the bladder tumor recurs, a repeat six-week course of intravesical BCG is administered. or photodynamic therapy (PDT) for bladder cancer.
Photodynamic therapy (PDT) for bladder cancer is local activation by light of the photosensitizer accumulated in the tumor, which leads to the development of a photochemical reaction that destroys tumor cells, i.e. Photodynamic therapy for bladder cancer selectively destroys tumor cells without damaging normal healthy tissue.
Over 75% of patients with carcinoma in situ are cured after BCG therapy. However, if two courses of BCG therapy and a combination of different methods do not provide a positive effect or tumor recurrence occurs, then radical surgery to remove the bladder or systemic chemotherapy is necessary to prevent metastasis of bladder cancer.
Rare types of bladder cancer include: small cell carcinoma, carcinosarcoma, primary lymphoma and sarcoma.
Rare forms of bladder cancer are squamous cell carcinoma of the bladder, which accounts for about 8% of all bladder tumors, and 1-2% of cases are adenocarcinomas (they account for over 90-95% of all cases of colorectal cancer). Naturally, different forms of bladder cancer respond differently to treatment. Thus, the choice of treatment will differ from patient to patient.
Urologist Altunin Denis Valerievich (Research Institute of Urology, Moscow)
The article is for informational purposes only. For any health problems, do not self-diagnose and consult a doctor!
Author:
V.A. Shaderkina is a urologist, oncologist, scientific editor of Uroweb.ru. Chairman of the Association of Medical Journalists.
03uro.ru
Correct diagnosis is the basis for successful treatment
In order to begin treatment for megaureter on time, it is necessary to make a correct diagnosis.
The most accurate diagnostic method for this pathology is excretory urography; ultrasound is also often used.
These methods make it possible to detect dilation of the ureter and make a diagnosis with accuracy.
Chromociscopy is considered an additional diagnostic method, and a clinical analysis of urine and blood is also taken.
Classification
Depending on the severity of the clinical picture, mild, moderate and severe bladder dysplasia is divided. The latter type of disease is extremely dangerous, as the risk of malignant cell transformation significantly increases.
On this topic
- urinary system
Adenoma and carcinoma
- Natalya Gennadievna Butsyk
- December 9, 2020
However, the disrupted development of tissue structures can be returned to normal and the appearance of a cancerous tumor can be avoided. To do this, you need to promptly seek help from a specialist and begin proper treatment. Even severe leukoplakia can be completely eliminated.
Dysplasia differs from the usual inflammatory process by the presence of focal changes at the tissue level. As the pathology progresses, the walls of the bladder lose elasticity, as a result of which the stretching of the organ worsens. All this leads to a frequent urge to urinate.
Therapy methods
Most urologists are inclined to believe that drug therapy in the treatment of neuromuscular dysplasia of the ureter brings virtually no results.
The only correct solution is considered to be surgical intervention, which involves resection of the distal ureter.
After the operation, antibacterial therapy is required to avoid secondary infection. For this purpose, broad-spectrum antibacterial agents are used.
Also, with megaureter, in some cases, physiotherapy using magnetic therapy is prescribed in the postoperative period.
In addition, all patients must adhere to a certain diet, eliminating spicy, sour, salty and fried foods.
You also need to refrain from heavy physical activity and sports for 2-3 months.
Neuromuscular dysplasia of the ureter
Neuromuscular dysplasia of the ureter is one of the most common and severe anomalies of the upper urinary tract. Despite the large number of works devoted to the study of this anomaly, there is still no consensus regarding the etiology, pathogenesis and its treatment. The difference in views of the authors on these issues is evidenced by the various names of the anomaly: atony, dilatation, dilation of the ureter, giant ureter, dysplasia, megaureter, megadolihoureter, hydroureter, achalasia of the ureter, forced ureter, etc.
The etiology and pathogenesis of this congenital disease are explained in different ways. Some authors believe that congenital dilation of the ureter is based on insufficient development of the neuromuscular apparatus of the ureter, while others associate the development of megaureter with a functional or organic obstacle localized at the level of the prevesical, juxtavesical or intramural parts of the ureter. Recently, neuromuscular dysplasia is understood as a combination of congenital narrowing of the ureter and its intramural part with neuromuscular dysplasia of the lower cystoid.
Information about the prevalence of this disease is contradictory. To study the frequency of neuromuscular dysplasia of the ureters, we (N. A. Lopatkin, A. Yu. Svidler, 1971) analyzed the protocols of 30,000 autopsies. Megaureter was detected in 0.7% of people with diseases of the urinary organs. Comparing the number of patients suffering from this malformation of the ureters identified in the clinic with the number of patients being treated in the clinic, it was noted that ureteral dysplasia would have been detected much more often if this category of patients had been subjected to a urological examination.
Most often, early-stage ureteral dysplasia is detected between the ages of 3 and 15 years, mainly at the age of 6-10 years. In adults, ureteral dysplasia is more often observed in the later stages of development, complicated by pyelonephritis and renal failure. Females are more likely to suffer from this malformation (the ratio of women to men is 1.5: 1). Bilateral ureteral dysplasia is more common than unilateral ureteral dysplasia. The defect is localized on the right almost 2 times more often than on the left.
Literature data (Ludwig, 1950; Oliver, Pinean, 1958, etc.) indicate that the proximal tubules of the human fetal kidney are capable of functioning at 3.5 months of intrauterine life. The ureters appear at earlier stages (fetal length is 4-6 mm). The free end of the ureter grows and divides towards the nephroblastoma. With the progressive ingrowth of the duct of the primary kidney into the sinus, the lower part of the ureter approaches the latter. The ureter begins to separate from the duct and connect to the sinus separately. At the moment when the ureter is separated from the duct of the primary kidney, the opening of the ureter in the sinus is closed by an epithelial membrane (R. Chwalla, 1927). During this period, the length of the fetus is 10-12 mm. The dimensions of the ureteral membrane correspond to the diameter of the ureter. It is very thin and contains two layers of cells: one layer consists of the ureteral epithelium, the other - from the sinus epithelium. The membrane disappears when the length of the fetus reaches 28-36 mm. Typically, the ureteral orifices are open in embryos that are 32 mm long. This stage corresponds to the end of the 2nd month of embryonic development. Ludwig (1950) believes that the renal pelvis, due to the mechanical obstruction created by the membrane, prevents the flow of urine secreted by the primary functioning glomeruli. The author explains the increasing dilatation of the pelvis by the lower density of the surrounding mesenchymal tissue.
According to G. Lauret (1956), at the 2nd month of intrauterine life of the fetus, mesenchymal tissue surrounds the lower end of the ureter and gives rise to several loose muscle fibers. This shell develops slowly from bottom to top. Its development ends in a fetus 150 mm long, that is, at 5 months. As a result, the upper part of the urinary system is less resistant than the lower part to increased intraureteric pressure that can cause dilatation. Roux (1961) noted that in experimental animals the preservation of this membrane is accompanied by the formation of dilated ureters. He also established the presence of a persistent membrane with ectatic ureters in a fetus older than 2 months.