What is kidney hydronephrosis
Hydronephrosis of the left right kidney is a disease that occurs for many reasons. This may be a congenital anomaly of the ureteropelvic segment, narrowing of the ureter (stricture), compression of the ureter from the outside (for example, by a tumor or an enlarged lymph node), obstruction of the lumen of the ureter with a stone.
Physically, all these processes lead to an increase in urine pressure inside the kidney and a gradual stretching of the elements of the collecting system. Due to impaired urine outflow, the excretory function of the kidney suffers, and a gradual thinning of the functionally active layer - the parenchyma - occurs.
Preparing for surgery
Before surgery, it is necessary to eliminate all kinds of urinary tract infections. Using radioisotope techniques, the doctor confirms the presence of obstruction, determines its extent and evaluates kidney function.
Ultrasound with water loading is mandatory. If during the examination the picture remains unclear, then urethrography is used for visualization. If the data is questionable, doctors perform the Whitaker test directly during surgery. To exclude the presence of a pathology such as vesicoureteral reflux, the patient is prescribed voiding cystourethrography.
Before the operation, it is necessary to carry out a set of preparatory measures. First, the doctor examines you and prescribes the necessary tests.
During the operation, the patient lies on his side. The surgeon makes three small incisions (0.5 - 1 cm) in the anterior wall of the abdominal cavity. Through the holes located near the navel, the peritoneum is filled with carbon dioxide using a special needle. Using special instruments, part of the ureter and pelvis is resected.
This technique has some advantages over abdominal surgery:
- no open bleeding;
- the development of infection is excluded;
- damage to nearby internal organs is excluded;
- the development of a postoperative hernia is excluded;
- low-injury;
- no need for blood transfusion;
- minimal rehabilitation period - the length of hospital stay is significantly reduced compared to abdominal surgery.
If nothing bothers the patient, then after 3-4 days he can be discharged. Restoration of the body and work activity occurs in 2-3 weeks. The main disadvantage is a wide range of contraindications.
Diagnosis and treatment of hydronephrosis
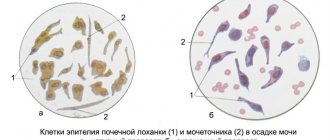
Diagnosis of renal hydronephrosis begins with ultrasound. It is this study that often makes it possible for the first time to diagnose hydronephrosis and refer the patient to a urologist. Further examination should identify the cause of hydronephrosis and determine the functional state of the kidney.
Spiral computed tomography with intravenous enhancement and 3D reconstruction provides extremely important information. To accurately assess kidney function, dynamic nephroscintigraphy is prescribed (sometimes with functional tests, for example with Furosemide).
Hydronephrosis treatment
It is quite obvious that the goal of treating hydronephrosis is to eliminate the cause that caused it. Given the variety of possible reasons described above,
You can imagine the current abundance of treatments for hydronephrosis.
All methods of treating hydronephrosis have one thing in common - they are all surgical. In other words, it is impossible to restore the impaired outflow of urine with the help of medications.
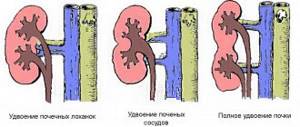
One of the most common forms of hydronephrosis is caused by a congenital anomaly (narrowing or stricture) of the ureteropelvic segment. Despite the fact that this type of hydronephrosis develops in childhood, it can be encountered at any age.
Of course, the most severe forms are identified and operated on in childhood, but often the diagnosis is established only by the age of 20-30.
Postoperative period
The postoperative period passes, as a rule, without complications if the patient follows the doctors’ recommendations. If the surgical method was chosen correctly, then recovery occurs quite quickly, but, of course, this also depends on what stage the disease was at. It is very important to follow all doctor's recommendations. Rehabilitation takes place in the hospital for another two weeks, the patient regularly has stitches treated and bandages changed.
All necessary tests will also be taken from the patient again. Bad urine tests after surgery do not mean that anything was done wrong. After all, the operated person continues to receive drug treatment for several days. Bacteria in the urine after surgery are well destroyed with the help of antibiotics, and the patient is also given antiviral drugs.
Kidney hydronephrosis treatment
The most modern method of surgical treatment of this form of hydronephrosis is laparoscopic plastic surgery of the ureteropelvic segment (laparoscopic plastic hydronephrosis) . This operation not only provides an excellent functional and aesthetic result, but also has a short hospitalization period and a rapid recovery period.
If the cause of hydronephrosis is a short narrowing of the ureter, then transurethral (through the urethra) endoscopic dissection gives good results.
The outflow of urine from the kidney can be temporarily restored (until the cause is eliminated) by installing an internal ureteral stent or nephrostomy.
When you contact me with such a serious problem as hydronephrosis, you can be sure that you will receive first-class help and an individual approach!
Advantages and disadvantages of laparoscopy
Their advantage is:
- Good visualization of the operated area, achieved using magnifying equipment.
- Convenient access to the application site.
- Satisfactory space for surgical intervention.
- Possibility of mobilization of the ureters in any necessary place.
- Reduction of pain in the postoperative period.
- No scar.
- Fast recovery after intervention.
Relative disadvantages:
- Some difficulties in endocorporeal anostomosis.
- Highly qualified specialists involved in the operation.
- The need for expensive equipment.
All difficulties associated with such manipulation are not permanent and tend to be gradually resolved. And the merits of this method are not even questioned. Moreover, they have been proven in practice with good results.
The essence of such surgical intervention as kidney plastic surgery for hydronephrosis is to excise the narrowed segment and suturing the remaining part of the ureter to the renal pelvis.
Questions about the article
Nikitin Igor Alexandrovich
October 24, 2020 at 10:26 pm
Hello! Plastic surgery of the ureteropelvic segment of the right kidney was performed. After 4 weeks, the stent was removed. Naturally (through the urethra) urine is released three times less than through the nephrostomy of the right kidney. This is fine?
drrotov
October 25, 2020 at 10:11 pm
This doesn't mean anything. It is necessary to gradually close the nephrostomy and “train” the pelvis
Anastasia Alekseevna
January 30, 2020 at 05:53 pm
10 days ago, an operation was performed to eliminate the causes of hydronephrosis: laparoscopic LMS plastic surgery, the kidney was sutured, a stent was installed in the ureter. Upon discharge on the 7th day, the tests were normal. Now the pressing pain in the kidney area persists, when pressing on the side, when changing position. Should the pain persist and for how long? What examinations should be performed after surgery?
drrotov
February 1, 2020 at 07:55 pm
Typically, such recommendations are given by the operating urologist before discharge. Pain may persist until the stent is removed. After 6-12 months (depending on the degree of hydronephrosis), a control ultrasound or CT scan is recommended
Tatiana
October 30, 2020 at 10:02 pm
Hello! My daughter (17 years old) was diagnosed with grade 2 hydronephrosis caused by pyelonephritis in May last year and underwent plastic surgery, but in September 2020 it became grade 3, a nephrostomy was installed, in January 2020 a radionuclide examination was performed, the function of the left kidney was reduced by 80%, in August it gave birth, in October during examination the function decreased by 85%. Now no more than 150 ml flows out of her nephrostomy tube. Is it possible to save the kidney or does it require removal, as the attending physician recommends?
drrotov
November 1, 2020 at 10:05 am
Preserving the kidney, unfortunately, does not make sense, since it practically does not function
Oksana 34 years old
May 27, 2020 at 17:03
Good afternoon 1.5 years ago, there was abdominal surgery to repair the ureter, which was compressed by an additional vessel (hydronephrosis). Now I have done an ultrasound, the abdominal system is expanded 33*25 mm, the pelvis is 18*16 mm, the calyx is up to 11 mm, the parenchyma is up to 18.5. Could these ultrasound data indicate a relapse of hydronephrosis?
drrotov
May 28, 2020 at 17:05
You need to know the preoperative picture. Even a successfully performed operation does not always lead to complete restoration of the normal dimensions of the renal cavity system.
Ekaterina 31 years old
May 7, 2020 at 00:12
Good afternoon, there was a 12 mm stone in the H3 ureter, they crushed the stump and installed a stent in February, in April the stent was removed and after a couple of days sharp pain began, they did a CT scan, it turned out that three large fragments were in the H3 ureter, two of 7 mm and one of 6 We did re-crushing. Two weeks later the pain began, now the pelvis is again dilated to 20 mm. Tell me whether the kidney suffers greatly from such an increase, all tests are good. But pain and a feeling of numbness are present. And which doctor should I go to to understand whether there are still stones left and where the hydronephrosis comes from?
drrotov
May 8, 2020 at 10:15 am
Stones (or their fragments) in the ureter always create unfavorable conditions for the kidney and the threat of complications (primarily pyelonephritis). Of course, a urologist will help you get rid of them.
Surgery for hydronephrosis
Surgery for hydronephrosis is a common solution to the problem. Before surgery, examination and preparation are carried out. It is necessary to take a urine test, blood test, ECG test, sanitize the oral cavity, and obtain permission for surgery from a therapist. If the blood test shows azotemia, then the operation cannot be performed until the parameters normalize. Normalization is achieved through hemodialysis. For adults with hydronephrosis of the kidney, the diseased organ is drained before intervention.
Pyeloplasty for hydronephrosis is an operation aimed at eliminating morphological changes in the renal pelvis. Hydronephrosis plastic surgery is performed using open, endoscopic or laparoscopic surgical treatment methods.
Public method
The peculiarity of the open surgical method is to access the kidney through an incision, which is made on the back in the projection of the affected kidney. The length of the cut is about fifteen centimeters. During the operation, the kidney is opened and the affected part is removed along with the pelvis. The kidney is then sutured. It is necessary to make sure that the seam is tight. If the seam has leaks, then the occurrence of fistulas is possible in the future.
The organ may be affected in its thickness, in which case the operation is complicated by access to the part that needs to be removed. In this case, the doctor performs plastic surgery of the ureter and, if necessary, in the vessels of the kidney. To prevent a stricture from forming again, a tube is inserted into the ureter, which must be removed several weeks after the surgical field has healed.
Endoscopic methods
A feature of these methods is access by introducing instruments through the urethra. In the same way, after the instruments, a camera is introduced, under the control of which the intervention is carried out. The advantage of these techniques is their low invasiveness, which makes the patient’s rehabilitation much faster.
Types of endoscopic methods:
- Balloon dilatation is a technique developed to eliminate stenosis in the ureter, which can form as a result of injury or inflammation of its walls. A balloon is inserted into the ureter, which, having reached the desired location, expands under the control of the operating specialist. In this way, the stenosis is eliminated. X-ray control of expansion is carried out. The balloon is then removed;
- Endotomy is a technique that involves laser removal of the affected part of the kidney. After the operation, a tube is temporarily inserted into the ureter, which must be removed during the rehabilitation process;
- Bougienage - the procedure is performed through a cystoscope, through which a bougie is inserted into the ureter;
- Stenting is a method in which a stent is inserted into the kidney and ureter, eliminating the narrowing without making any cuts to the patient's own tissue.
Laparoscopic method
A minimally invasive method that involves inserting instruments through small incisions in the area where the kidneys are projected. This technique does not require sutures due to the size of the incisions made.
Nephrectomy is the complete removal of a kidney. This method is used only when there is too much damaged tissue for the kidney to continue functioning. As a rule, an open method is used for this, because a large incision is required.
When is surgery necessary?
More often, the disease develops in children; one of the kidneys is affected, rarely both. In adults from 20 to 60 years of age, kidney pathology is predominantly registered in women, which is associated with childbearing age, pregnancy and gynecological diseases. Men with prostate adenoma and cancer after 60 years are also at risk.
Hydronephrosis develops due to prolonged congestion.
An increase in urine volume leads to compression of the kidney tissue and its vessels. Pressure increases inside the pelvis and ureter, and glomerular filtration is disrupted. Over time, complications arise, the renal tubules and organ cells atrophy, and necrosis occurs.
Surgery for hydronephrosis is indicated if the benefit from it is greater than the risk of surgery itself. In most patients, surgery can restore function and save the kidney. Removal of an organ is resorted to only as a last resort. Conservative treatment is used as an auxiliary treatment - this is antibacterial therapy and symptomatic care.